Abstract
Stroke is a neurological condition characterized by prolonged rehabilitation, requiring long-term patient cooperation for effective recovery. Rehabilitation adherence plays an important role in the prognosis. This study aimed to identify the patient-, doctor-, hospital-, and society-level factors influencing rehabilitation adherence. In this qualitative study, semi-structured interviews were conducted with 25 experts in rehabilitation medicine, cardiovascular medicine, and neurology from six representative cities in China (Beijing, Tianjin, Shanghai, Wuhan, Harbin, and Chengdu) to explore the factors affecting rehabilitation adherence. Transcripts were coded and analyzed using an inductive thematic approach for data analysis. NVivo 14 was used to manage and analyze the textual data. All methods were performed in accordance with relevant guidelines and regulations, specifically the Guidelines for the “Prevention and Treatment of Cerebrovascular Diseases (2024 Edition)” and the “2024 China Stroke Prevention and Treatment Guidelines” issued by the General Office of the National Health Commission of the People’s Republic of China. Regarding in-hospital rehabilitation, medical experts believed that the characteristics of patients who had a stroke directly affected their rehabilitation adherence, including rehabilitation expectations, self-efficacy, economic pressure, family support, and trust in doctors. Additionally, medical experts also believed that various factors at the doctor, hospital, and societal levels influence patient characteristics, such as doctors’ professional skills, collaboration between departments, and social cognition, ultimately affecting rehabilitation adherence. For out-of-hospital rehabilitation, medical experts believed that the key determinants of adherence include accessibility to tele-rehabilitation, tele-medical resources, and active participation of hospital outpatient clinics. Most medical experts believed that it is crucial to focus not only on direct factors, such as rehabilitation expectations and self-efficacy, which influence patients’ subjective intentions, but also on identifying the pathways through which doctors, hospitals, and societal factors impact patient behavior. Attention should be given to in- and out-of-hospital rehabilitation.
Similar content being viewed by others
Introduction
The Global Burden of Disease (GBD) study indicates that in 2019, there were 12.2 million new cases of stroke globally, with 101 million prevalent cases. In China, there were 3.94 million new cases of stroke and 28.76 million prevalent cases in the same year1,2. Stroke is the leading cause of death and disability among adults in China. As of 2019, China had the highest stroke incidence rate worldwide. From 2013 to 2019, the age-weighted prevalence of stroke among residents aged 40 and above in China increased by 13.2%3.
According to the World Health Organization (WHO), rehabilitation is an evidence-based, highly effective intervention for reducing disability rates among patients who have had a stroke4. This not only improves their self-care ability significantly, but also helps in preventing the recurrence of stroke through risk factor management and health education5,6,7. Studies have shown that approximately 90% of patients who have had a stroke can recover walking and self-care abilities if they are actively rehabilitated, and some patients can also undertake light work; contrastingly, without rehabilitation, only 6% of patients regained their self-care and walking abilities8,9,10,11,12.
China has seen some progress in its “three-phase rehabilitation network.” This is a rehabilitation system that includes acute rehabilitation, recovery rehabilitation, and community or home-based rehabilitation designed for patients with conditions such as stroke, aimed at improving rehabilitation outcomes and quality of life. However, a considerable number of patients may not receive adequate rehabilitation after discharge, which poses challenges to their recovery. Low rehabilitation adherence among this demographic is one of the most critical reasons for delayed recovery and poor functional outcomes13,14,15 posing a significant challenge in reducing the disease burden of stroke and improving the quality and effectiveness of rehabilitation treatment.
Research on rehabilitation adherence among patients with a history of stroke in China is relatively limited. Particularly, a comprehensive analysis of the factors influencing rehabilitation adherence among these patients across different hospitals and cities is lacking. Existing studies primarily focus on identifying specific factors influencing rehabilitation adherence without addressing in-hospital and out-of-hospital rehabilitation situations or the relationship between the different influencing factors16,17. For example, a physician’s communication skills can assist patients in developing more targeted rehabilitation plans and facilitate their implementation, thereby improving their adherence to the rehabilitation process. Studies have investigated various factors affecting rehabilitation adherence (such as social support, economic status, and patient self-efficacy); however, there is a lack of research on how these factors impact adherence in China, where rehabilitation resources are limited. The absence of an understanding of patient-, family-, and society-level factors can hinder the clinicians’ ability to develop comprehensive, personalized rehabilitation plans, ultimately affecting patient adherence18,19,20,21,22,23 A greater understanding of the underlying logic and pathways of the influencing factors can elucidate problems within the rehabilitation system and possibilities for improvement in similar settings worldwide.
The importance of rehabilitation medicine, cardiovascular medicine, and neurology in providing effective rehabilitation services was highlighted by the WHO’s “Rehabilitation 2030 Initiative.” They formulate rehabilitation plans, provide medical prescriptions, verbal encouragement, and rehabilitation advice, offering comprehensive consultations considering patients’ complications and comorbidities. This approach leads to a more direct and in-depth understanding of the factors influencing patient rehabilitation adherence. This study aimed to explore the factors influencing rehabilitation adherence from these medical perspectives and identify their effects on the behavior of patients who have had a stroke.
Methods
Study design and participants
In this qualitative study, semi-structured interviews were conducted with 25 experts in rehabilitation medicine, cardiovascular medicine, and neurology from six cities covering major geographic areas in China (Beijing, Tianjin, Shanghai, Wuhan, Harbin, and Chengdu). Here, the inclusion of cardiovascular specialists (n = 4) was intentional to address: (1) the high prevalence of cardiovascular comorbidities in stroke patients that influence rehabilitation planning, and (2) the critical role of cardiovascular risk factor management in secondary stroke prevention during rehabilitation. Their expertise complemented the neurological and rehabilitation perspectives to provide comprehensive insights. This manageable framework allowed for in-depth interviews while balancing practical constraints such as time, resources, and scheduling.
Principles for sampling
We employed purposeful sampling (also called purposive sampling) to select information-rich cases. The sampling strategy was designed to: (1) ensure geographic representation across six major Chinese cities; (2) include diverse hospital tiers (tertiary to community hospitals); (3) achieve balanced representation across specialties (rehabilitation medicine, neurology, cardiology). Purposeful sampling allows researchers to select medical experts with extensive experience in rehabilitation medicine, cardiovascular medicine, and neurology, ensuring that the collected data are highly relevant to the research topic; therefore, we adopted this approach. An important principle of purposeful sampling is achieving data saturation, where sampling is stopped when no new insights emerge.
Participants selection
Expert definition
Medical experts were operationally defined as: (1) board-certified physicians in rehabilitation medicine, neurology or cardiovascular medicine; (2) with ≥ 10 years clinical experience in stroke care; (3) holding associate attending physician rank or higher.
Sampling methodology
We employed purposeful sampling (also called purposive sampling) to select information-rich cases. The sampling strategy was designed to: (1) ensure geographic representation across six major Chinese cities; (2) include diverse hospital tiers (tertiary to community hospitals); (3) achieve balanced representation across specialties (rehabilitation medicine, neurology, cardiology).
Selection process
Participants were identified through: (1) national professional directories; (2) peer recommendations from academic societies; (3) snowball sampling where initial participants suggested additional qualified experts. Recruitment continued until thematic saturation was achieved at 25 interviews.
Finally, twenty-five medical experts were selected based on their expertise, experience, and contributions to stroke treatment and research24. We focused on medical experts because they play a central role in formulating rehabilitation plans, providing medical prescriptions, and offering rehabilitation advice to patients who have had a stroke. Their professional knowledge and clinical experience enable them to have a direct and in—depth understanding of the factors influencing patient rehabilitation adherence.
City selection
The chosen cities have higher stroke incidence rates and significant regional characteristics among all cities in the same area25. These cities were selected for the following reasons:
-
(1)
Stroke incidence rate. These cities have relatively higher stroke incidence rates compared to other areas in China. As of 2019, China had the highest stroke incidence rate worldwide, and these cities are regional economic centers with large populations, where the burden of stroke is significant.
-
(2)
Regional characteristics. They cover major geographic areas in China, including the north, south, east, and central regions. Each city has its own unique regional characteristics in terms of population demographics, economic development, medical resources, and cultural background. By including these cities, we aimed to capture the diversity of stroke care practices and the factors influencing rehabilitation adherence in different regions of China.
-
(3)
Medical resources. These cities are regional economic centers with well—developed medical resources and facilities where rehabilitation services are frequently provided. They have a large number of high—level medical institutions, including tertiary hospitals and specialized rehabilitation centers, which can provide a rich source of expert opinions on stroke rehabilitation.
Although these cities share some similarities in terms of the general principles of stroke care, there are also differences in their medical resource allocation, healthcare policies, and patient populations. For example, the economic development levels of these cities vary, which may affect the accessibility and affordability of rehabilitation services for patients. Additionally, cultural and regional differences may also influence patients’ attitudes towards rehabilitation and their adherence to treatment plans. By studying these cities, we can gain a more comprehensive understanding of the factors influencing rehabilitation adherence in different settings and identify strategies for improving stroke care across the country.
The research team contacted doctors through medical institutions, professional associations, or personal mail. The research team also introduced the overall goals, importance, and specific details of the study to the doctors through phone calls, emails, or face-to-face meetings. The doctors received a comprehensive research plan, including interview requirements, timelines, and expected outcomes. After fully understanding the study, the doctors decided whether to participate. This process ensured that doctors voluntarily participated and had a complete understanding of the content and requirements of the study.
Data collection
This study was approved by the Institute for Global Health and Development at Peking University. The study followed the consolidated criteria for reporting qualitative research (COREQ).
A review meeting was held in June 2023 at the Peking University Institute for Global Health and Development to discuss and refine the interview outline as well as review and provide feedback on the study design. 25 medical experts from the National Health Commission of China, Beijing Neurosurgical Institute, Beijing Rehabilitation Hospital, and Peking University were invited to provide guidance and revisions to the interview outline. We also revised the outline based on feedback from the pilot interviews. The interview guide can be found in Appendix 1.
Prior to the interviews, the researchers read and obtained written informed consent from participants, even though ethical approval was waived due to the study’s non-patient nature. The interviews were performed by two authors (Meng Liu and Ziting Wu) and six research assistants (Luyang Xiao, Shanshan Li, Ya Wang, et al.). Experts chose a setting where they felt comfortable, usually their private office within the hospital. No nonparticipants were present, and interruptions were rare. Semi-structured interviews were conducted to determine factors affecting rehabilitation adherence. To ensure high-quality and credible answers, the interviewers probed extensively for specific and detailed explanations. Interviews were audio-recorded, and notes were obtained with permission from the participants. Names or contact information were not recorded. The interviews lasted 60 to 120 min and were recorded and transcribed in Chinese, with the results translated into English. No repeat interviews were conducted, and the interview transcripts were not returned to the participants for comments.
Data analysis
The interview guide is provided in the Online Appendix.
After the interviews, the researchers translated the recorded interviews into textual data. The text data were managed and analyzed using NVivo 14. Any personal information that could reveal the identities of the participants was removed. Data were analyzed using Braun and Clarke’s inductive thematic analysis. The ground-up approach directly summarizes and refines the code according to the text and then elaborates on the specific data analysis process in combination with this study. Complexity or integration capabilities are gradually added to the base model while ensuring each new level works properly and is compatible with existing parts26. Initially, the researchers categorized the factors influencing rehabilitation adherence into four themes based on literature review: hospital, social, doctor, and patient levels27,28. The research team then independently encoded 25 interview materials based on the literature revealing four secondary and 663 tertiary codes. The process of constructing and refining the code structure included adding and reconstructing codes as new concepts emerged and identifying new relationships within the units of a given category. The research team reviewed the code structure for logic and breadth. We then organized the rest of the interview materials using the code structure line by line, and no new concepts emerged from reviewing the successive data. This meant that our code structure reached the theoretical saturation point and was considered finalized. Using the finalized code structure, Meng Liu and Ziting Wu independently encoded all interview text data. They met as a group to code in several sessions, achieving consensus and assigning codes to observations by an agreed-upon group process. The code reference points are presented in Appendix 1.
Results
Characteristics of the participants
A total of 25 medical experts participated in the interviews. Researchers obtained 25 recordings and translated documents. Among the experts, 9 were female, and 16 were male. These experts came from different hospitals in the six provinces mentioned earlier, with 16 from rehabilitation departments, five from neurology, and four from cardiovascular departments. Twenty experts worked in tertiary hospitals, and five worked in secondary hospitals. Among the 25 experts, there was one professor, three associate professors, 12 chief physicians, eight deputy chief physicians, and one attending physician. The distribution of the 25 medical experts is shown in Appendix 2.
Facilitators and barriers to hospital-based rehabilitation
Based on the qualitative analysis of interview data with medical experts, our study identified distinct categories of facilitators and barriers to stroke rehabilitation adherence across four key levels.
Facilitators
Patients
Rehabilitation expectations
Most medical experts revealed that patients’ health status and the timing of rehabilitation play a crucial role in determining their rehabilitation expectations. If a patient already has an underlying condition or experiences stroke-induced mental or neurological disorders, rehabilitation expectations may be lowered. More than half of the experts noted that patients with higher cognitive abilities had stronger self-management skills, often holding positive expectations for rehabilitation and setting clear, achievable rehabilitation goals.
“Patients with relatively high awareness levels are more likely to come to contact with rehabilitation doctors, experts, or scholars, and are more likely to accept rehabilitation. In my communication with patients, I found that due to the low cognitive level of some patients, their rehabilitation expectations are relatively high, leading to a significant gap between their expectations and reality. This causes a lack of trust in doctors and hinders better acceptance of rehabilitation treatment.” — Associate Professor of Neurology, male, 52 years old.
Self-efficacy
Several experts have highlighted that strong psychological determination indicates an individual’s capacity to maintain strong motivation and mental fortitude, effectively bouncing back from setbacks and persisting through challenges. Highly determined patients are always more willing to face challenges during rehabilitation and are more likely to motivate themselves. Strong psychological determination helps patients cope positively with negative emotions such as anxiety and depression.
“A certain patient underwent three months of rehabilitation treatment in the hospital. After that, I visited his home six times a month to provide rehabilitation therapy, and the patient recovered very well. In my opinion, the key factor that enabled this patient to complete his rehabilitation was his resilience and strong motivation to return to society and work.” —Professor of Rehabilitation Medicine, male, 57 years old.
Trust in doctors
Most experts believe that trust forms the foundation for in-depth communication between doctors and patients who have had a stroke. Based on trust, patients are more willing to share their symptoms, health status, and personal health information. This enables rehabilitation doctors to better understand the patients’ conditions and formulate precise rehabilitation plans. Additionally, trust helps alleviate anxiety and stress in patients.
“Medical staff need to ensure effective communication with patients, letting them know what the staff can do to help. Medical staff should tell patients the ultimate goal of rehabilitation, bridging the gap with patients. Professionalism (e.g., the knowledge structure of rehabilitation doctors, for instance, I developed a mindset for managing patients in my 40 s) and compassionate communication help patients quickly connect and trust. Apart from professionalism, rehabilitation doctors’ psychological and humanistic understanding also helps build trust, enhancing patients’ adherence to rehabilitation.”—Professor of Rehabilitation, female, 54 years old.
Doctors
Communication skills
Most medical experts noted that when patients and doctors establish good communication, patients depend on the doctor. In particular, when patients experience improvements under their doctor’s guidance, patients become more trusting. Research has also indicated that a good rehabilitation plan relies on thorough communication between doctors and patients. Most medical experts also believed that fully understanding the patient’s physiological and psychological status and maintaining adequate communication significantly influences the implementation of the rehabilitation plan.
“Many patients and families don’t know what rehabilitation can do for them. They need to know why they are doing it, how to do it, what they can achieve by doing it, and the consequences of not doing it. Knowing these things helps improve patients’ adherence to rehabilitation. (…) Before starting rehabilitation training, showing patients videos of previous patients’ rehabilitation outcomes can help them accept treatment, as seeing is believing.” — Chief Physician of Rehabilitation Medicine, male, 49 years old.
Attitude towards career
Most medical experts believed doctors’ passion for their work and desire to gain a sense of accomplishment make them more proactive in their rehabilitation efforts, fostering empathy with patients. If doctors complain about low income, they lose the motivation to engage in their work and adopt a negative attitude toward patients. This can cause patients to become wary and resistant, thereby affecting their rehabilitation outcomes and adherence.
“From my first day in medical school, I had the initial intention and responsibility to be a good doctor who’ saves lives and helps the injured, holding a positive view of this noble profession. While receiving social honors, I also have the responsibility to alleviate patients’ suffering, which provides me with comfort. (…).” — Chief Physician of Neurology, female, 61 years old.
Professional competence
Rehabilitation training is a complex task requiring doctors to formulate scientific training plans and be creative. Most medical experts indicated that interesting training programs reduce patient resistance and help them adhere to rehabilitation strategies. Patients are more likely to cooperate in scientific and creative clinical practices.
“Doctors should use different ways to develop rehabilitation training content, making it interesting for patients and preventing their work from becoming tedious or rigid. Additionally, for patients with average cooperation, it is important to provide psychological counseling and, when necessary, coax them through the rehabilitation process without feeling bored, while showing compassion.” — Chief Physician of Rehabilitation Medicine, male, 49 years old.
Society-related factors
Government support
Almost all medical experts advocate for government policy inclinations and financial support to expand the promotion of rehabilitation medicine knowledge and increase public awareness. A higher medical insurance reimbursement rate boosts patients’ enthusiasm for rehabilitation and allows them to actively receive treatment without excessive financial burdens.
“The government should do more publicity to raise the awareness of rehabilitation throughout society. Moreover, the government should correct the professional qualifications of rehabilitation therapists. For example, the Ministry of Human Resources and Social Security recently classified rehabilitation therapists as social service workers, similar to catering service workers. This cannot guarantee the identity and social status of rehabilitation therapists and may negatively affect their work motivation.” — Associate Professor of Rehabilitation Department, Male, 49 years old.
Barriers
Patients
Family cooperation
During interviews, five medical experts mentioned that families are often overly eager, expecting patients to regain mobility, leading to the common occurrence of “over-rehabilitation.” This refers to a situation where patients undergo excessive or intensive rehabilitation efforts, often driven by unrealistic expectations from families or caregivers. They believed that this “over-rehabilitation” not only reduces the patient’s independence, causing excessive reliance on the family and affecting their ability to participate in rehabilitation activities and self-management, but also increases pressure on the patient. This may lead to frustration or an inability to meet high expectations, causing resistance and negative emotions toward the rehabilitation plan.
“The role of family members is twofold. Financial and psychological support can enhance patients’ adherence to rehabilitation, but excessive care can also be a hindrance to rehabilitation. For example, helping patients dress or feed them can create dependency, affecting the patients’ rehabilitation expectations. Allowing patients to do what they can for themselves leads to better rehabilitation outcomes.” — Associate Professor of Rehabilitation Medicine, male, 49 years old.
Economic pressure
Several medical experts have highlighted that a patient’s financial situation significantly affects their rehabilitation adherence. At the individual level, economic pressure can manifest in many forms, such as job loss, financial distress, and difficulty paying bills. With substantial economic pressure, patients may struggle to adhere to planned rehabilitation activities, face challenges in purchasing necessary medications, or have difficulty accessing essential rehabilitation resources (such as physical therapy or rehabilitation equipment). Economic pressure can lead to anxiety and depression, further promoting the development of complications and comorbidities.
“Currently, hyperbaric oxygen therapy, acupuncture, electrotherapy, and physical therapy are the main methods of patient rehabilitation. Hyperbaric oxygen therapy is more effective but more expensive. Patients in Shanghai have agricultural insurance (high reimbursement rate), so most can accept hyperbaric oxygen therapy. However, most patients from other regions, facing economic pressure, do not accept hyperbaric oxygen therapy, making up about 15% of patients.” — Deputy Chief Physician of Neurology, female, 44 years old.
Hospitals
Department collaboration
Most medical experts also believed that when a patient has had a stroke and is admitted to the cerebrovascular or neurology department during the onset period, the involvement of rehabilitation doctors can aid in functional recovery during the treatment of the primary disease. Unfortunately, many rehabilitation medical experts suggest that departmental collaboration is not straightforward and that the involvement of rehabilitation doctors is often not timely.
“It often happens that patients are hospitalized in the neurology department, where they receive clinical treatment from them. At the end of the initial consultation, the neurology department did not notify the rehabilitation doctors for a consultation, so the rehabilitation doctors were not involved in the treatment process. Moreover, the patient went home directly after treatment in the neurology department.” — Deputy Director of Neurology, Chief Physician, Female, 44 years old.
Hospital investment
Most medical experts indicated that most hospitals, especially community hospitals, lack rehabilitation doctors, making it difficult to understand and meet patients’ needs promptly and adequately. This results in poor medical outcomes and patient experiences, leading them to mistakenly believe that rehabilitation has little impact on their health. Furthermore, with the general shortage of beds in rehabilitation departments, patients find it difficult to secure beds and receive timely formal rehabilitation.
“Community professional staff are severely lacking, and many community hospitals do not have rehabilitation doctors. Community hospitals also face the problem of having few and unprofessional therapists.” — Deputy Director of Neurology, Chief Physician, Female, 44 years old.
“I hope that hospitals can improve their ward facilities. Currently, rehabilitation department wards are crowded, with few bathrooms, and overall poor conditions.” — Chief Physician of Rehabilitation Department, Female, 60 years old.
Training of rehabilitation talent
Research found that most hospitals lack adequate training for rehabilitation doctors, and the training content is not standardized. Because few practicing physicians have a degree in rehabilitation medicine, most rehabilitation therapists require professional training to improve their treatment levels to meet the minimum treatment standards.
“The professional level of rehabilitation therapists needs to be improved, especially among young people. Therefore, hospitals should regularly train rehabilitation therapists. Hospitals can set up regular training departments for rehabilitation workers to enhance the professional ability of personnel.” — Chief Physician of Rehabilitation Department, Male, 58 years old.
Society-related factors
Government support
Almost all medical experts advocate for government policy inclinations and financial support to expand the promotion of rehabilitation medicine knowledge and increase public awareness. A higher medical insurance reimbursement rate boosts patients’ enthusiasm for rehabilitation and allows them to actively receive treatment without excessive financial burdens.
“The government should do more publicity to raise the awareness of rehabilitation throughout society. Moreover, the government should correct the professional qualifications of rehabilitation therapists. For example, the Ministry of Human Resources and Social Security recently classified rehabilitation therapists as social service workers, similar to catering service workers. This cannot guarantee the identity and social status of rehabilitation therapists and may negatively affect their work motivation.” — Associate Professor of Rehabilitation Department, Male, 49 years old.
Social awareness
According to medical experts, social awareness impacts rehabilitation compliance in three ways. First, it influences whether patients feel support from family, friends, and the community. Second, it involves interactions between patients and rehabilitation teams. Third, social awareness can shape expectations and attitudes of others toward the rehabilitation of patients who have had a stroke.
“Overall, the social awareness of rehabilitation remains low. Most people mistakenly understand rehabilitation as physical therapy session, a massage, or undergoing some form rehabilitation, thus necessitating publicity and education for the public (including clinical doctors).” — Associate Professor of Rehabilitation Department, Male, 49 years old.
Accessibility of medical resources
Research found that high medical resource accessibility makes it easy for patients to obtain the necessary rehabilitation equipment and receive guidance from healthcare professionals. Continuous rehabilitation encourages patients to actively participate in treatment, thereby enhancing their confidence in the process.
“A 60-year-old aunt with level three hemiplegia was brought to the hospital by her family for rehabilitation. Upon admission, she was only being fed through a nasal tube. Based on the evaluation of her swallowing and limb functions, the prognosis should be good. In about half a month, her condition would significantly improve. However, the patient was discharged after only a week, mainly due to financial conditions and her children’s need to return to work in nearby prefecture-level cities, which lack specialized rehabilitation hospitals.” — Chief Physician of Rehabilitation Medicine, Female, 36 years old.
Establishing a three-tier rehabilitation network
Some medical experts point out that three-tier rehabilitation, such as community and home rehabilitation, can be more effective, where community hospitals can also undertake certain rehabilitation work. Unfortunately, Most medical experts indicated that despite significant improvements in constructing the three-tier rehabilitation system, it falls short of expectations.
“Society lacks barrier-free facilities, so regardless of how well patients rehabilitate, many eventually become disabled. If barrier-free facilities are not increased, these patients’ social participation will be very low. In Japan, there are taxis specifically for disabled people in wheelchairs, allowing them to independently use transportation to visit doctors. These facilities help patients reintegrate into society.” — Deputy Chief Physician of Neurology, Female, 44 years old.
Establishing industry standards and norms
Research found that rehabilitation medicine lacks unified scientific standards in China and globally. As the saying goes, “Three parts treatment, seven parts care,” but regrettably, the current structure of rehabilitation personnel in China cannot meet the standards of a continuous care model. Most medical experts indicated that one of the main reasons for this is the lack of professional certifications and commissioned training in the rehabilitation medical system.
“The rehabilitation treatment system lacks systematic and standardized approaches. The government should establish standardized referral mechanisms (setting corresponding standards), unify personnel requirements, clarify unified management models (such as medical documents), and establish supervision and regulatory mechanisms for the medical process.” — Chief Physician of Rehabilitation Department, Male, 50 years old.
According to the above analysis, the facilitators to hospital-based rehabilitation include key facilitators for stroke rehabilitation adherence include patients’ positive rehabilitation expectations, strong self-efficacy, and trust in doctors. Higher cognitive abilities enable patients to set realistic goals, while psychological resilience helps them overcome challenges. Effective doctor-patient communication and physicians’ professional attitudes enhance treatment plans. Government support through policies and insurance coverage, along with improved social awareness and accessible medical resources, further promote rehabilitation adherence. Meanwhile, the barriers to hospital-based rehabilitation involve patients’ unrealistic expectations due to low cognitive levels, leading to mistrust in doctors. Limited healthcare resources, financial constraints, and lack of standardized rehabilitation protocols hinder treatment continuity. Inadequate social awareness and insufficient barrier-free facilities reduce patients’ social participation. Additionally, the absence of professional certifications and training for rehabilitation staff impacts service quality and motivation.
Home-based rehabilitation
Facilitators
Home rehabilitation programs and rehabilitation systems
Personalized home-based rehabilitation programs are crucial for patient recovery. When investigating user needs for rehabilitation systems, the experts consistently identified exercise selection and quality as core requirements. Forty-four percent (25 medical experts) emphasized the importance of exercise selection (Appendix Fig. 1).
Outpatient participation
Most medical experts believed that outpatient rehabilitation can meet the specific rehabilitation needs of patients who have had a stroke, such as the targeted recovery of language skills and motor functions. Compared with inpatient rehabilitation, outpatient rehabilitation is generally more cost-effective for patients, significantly reducing medical and other related expenses.
“Communities are encouraged to establish outpatient rehabilitation clinics and facilities, as patients have more options and there is less commitment than just having a rehabilitation clinic. There was a grandmother who, due to some dementia and cognitive impairment, was unwilling to be hospitalized, fearing that her family did not like her. Her family left her in the hospital, but she needed a family member to accompany her during hospitalization. Later, the treatment plan was changed to allow for outpatient treatment, and her compliance significantly improved.” — Associate Chief Physician and Associate Professor of Rehabilitation Medicine, Male, 49 years old.
Barriers
Remote rehabilitation and accessibility of medical resources
According to medical experts, if medical resources are not easily accessible, patients may have to wait longer to receive rehabilitation. Moreover, the incompleteness and inadequacy of the three-tier rehabilitation network not only leads to a shortage of rehabilitation resources but also result in patients facing a lack of rehabilitation services. Additionally, a considerable portion of rehabilitation training must be conducted outside the hospital.
“In areas where transportation is convenient and rehabilitation hospitals are accessible, patient compliance is relatively higher. If the community or rehabilitation center does not provide remote rehabilitation services, patients will be unable to access these services. This requires government departments to further improve the construction of the rehabilitation medicine discipline system and continuously enhance the accessibility of community and home rehabilitation.” — Chief Physician of Neurology, Female, 61 years old.
According to the above analysis, key factors promoting stroke rehabilitation adherence to home-based rehabilitation include patients’ recovery expectations, self-efficacy, and positive mental health, supported by adequate economic status. Physicians’ tailored treatment strategies, structured rehabilitation plans, strong family/social support, and effective hospital interdepartmental collaboration further enhance adherence. Obstacles to adherence home-based rehabilitation involve limited accessibility to rehabilitation services due to resource shortages, inadequate three-tier rehabilitation networks, and geographic barriers. Poor mental health, financial constraints, and lack of family/social support also hinder compliance, compounded by insufficient explanations of behavioral change pathways.
Discussion
In this study, we identified facilitators factors to hospital-based rehabilitation include key facilitators for stroke rehabilitation adherence include patients’ positive rehabilitation expectations, strong self-efficacy, and trust in doctors, etc. Meanwhile, we identified barriers factors to hospital-based rehabilitation involve patients’ unrealistic expectations due to low cognitive levels, leading to mistrust in doctors, etc.
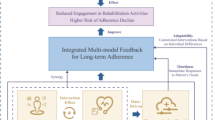
Furthermore, we identified factors such as rehabilitation expectations, family cooperation, economic pressure, self-efficacy, and trust in doctors as major influences on patient rehabilitation adherence.24 Additionally, this study also found various factors at the doctor, hospital, and society level can affect patient characteristics, ultimately impacting rehabilitation adherence (Fig. 1)29.
Research found that rehabilitation expectations, financial pressure, and self-efficacy were the three most crucial factors influencing rehabilitation adherence. Most medical experts indicated that if patients expect significant benefits from rehabilitation, they are more likely to adhere to the treatment plan, exercise, or other rehabilitation measures, and vice versa30,31,32 And they believed that under substantial financial pressure, patients may cut expenses, refuse treatment, or reduce the quantity and quality of necessary rehabilitation medical services33. The findings of this study show that financial pressure can delay the optimal rehabilitation period for patients, thereby reducing their rehabilitation expectations and adherence. A patient’s self-efficacy directly affects their rehabilitation motivation34, self-encouragement, and ability to face setbacks. Surprisingly, no strong correlation was observed between self-efficacy and age. Patients with a higher social status had stronger self-efficacy. Interestingly, most medical experts believed that patients’ trust in their doctor helps establish a long-term stable doctor-patient relationship, supporting long-term rehabilitation efforts35.
According to medical experts, improving professional identity and job satisfaction can enhance the performance of rehabilitation doctors by providing a sense of achievement and reducing work stress36, and vice versa. Most medical experts indicated that when doctors value and love their work, they are more likely to approach it responsibly, actively consider patients’ needs, and avoid medical discrimination37. Communication also helps build trust between doctors and patients and provides information for creating personalized rehabilitation plans.
Most medical experts noted that certain obstacles concerning patient flow between hospital departments, mainly due to the limited number of beds in the neurology and rehabilitation departments and the incomplete tiered rehabilitation network38. Patients hospitalized in tertiary hospitals cannot be effectively referred to lower-level hospitals or community rehabilitation institutions, thereby occupying beds needed by other patients. Almost all medical expertsencouraged eligible community health service institutions to establish stroke clinics, enhance the health management of high-risk stroke populations, and conduct stroke prevention and rehabilitation management for these patients39,40. The study also found that most hospitals, especially community hospitals, lack rehabilitation doctors, necessitating increased investment to actively recruit these professionals Moreover, hospitals should regularly train therapists to improve their rehabilitation treatment levels and meet the minimum treatment standards29.
The study found that government support, social awareness, and the establishment of industry standards and norms were the top three social factors affecting rehabilitation adherence in patients who have had a stroke. Most experts suggest decentralizing government resources and allowing functional departments to delegate power, enabling more rehabilitation professionals to participate in policy formulation and implementation41. Some medical experts emphasized that many patients have never heard of rehabilitation treatment, and some consider it a form of massage, which indicates a considerable lack of accurate understanding of rehabilitation treatment in society, along with existing prejudices42. Furthermore, most medical experts noted that China’s current rehabilitation personnel structure does not meet the standards of the continuous care model, making it hard to achieve patient-centered continuous care or rehabilitation43.
In the out-of-hospital rehabilitation context, this study found that aside from the individual characteristics of the patients, active participation of hospital outpatient clinics and medical resource accessibility (e.g., number of medical professionals, beds, and rehabilitation equipment) affect patient compliance (Fig. 2)43.
According to medical experts, active participation in hospital outpatient clinics can significantly improve rehabilitation compliance by providing personalized rehabilitation programs8, multidisciplinary team collaboration, patient education, psychological support, supervision, follow-up, and utilization of family and community resources44,45 The hospital outpatient department can develop personalized rehabilitation plans based on specific patient conditions. These plans can better meet patient needs and improve rehabilitation compliance46. Hospital clinics often involve multidisciplinary teams, including neurologists, rehabilitation therapists, nurses, and dietitians. Through multidisciplinary collaboration in outpatient departments, patients can receive more comprehensive treatment advice and guidance, reduce treatment inconsistencies, and increase their trust and compliance47.
In this study, we identified facilitators factors to home-based rehabilitation include patients’ recovery expectations, self-efficacy, and positive mental health, supported by adequate economic status, etc. Meanwhile, we identified barriers factors to home-based rehabilitation involve limited accessibility to rehabilitation services due to resource shortages, inadequate three-tier rehabilitation networks, and geographic barriers, etc.
Most medical experts indicated that accessibility to medical resources, including geography48, economy49, information, service supply, community support, and psychological support50, has an important impact on out-of-hospital rehabilitation compliance. They believed that an environment with high access to medical resources can provide patients convenient, economical, and continuous rehabilitation support, significantly improving their rehabilitation compliance. Conversely, in resource-poor areas, patient compliance is often low; therefore, the rehabilitation effect is limited. Moreover, the study found that the accessibility of medical resources for patients who have had a stroke in China is relatively low, especially in rural and remote areas. The reduced accessibility leads to a breakdown in communication between healthcare providers and patients after discharge, resulting in lower rehabilitation adherence29.
This investigation has several limitations that should be acknowledged. This study was conducted in six representative cities in China (Beijing, Tianjin, Shanghai, Wuhan, Harbin, and Chengdu). Although the economic and social conditions in these cities largely represent typical urban areas in the eastern, central, and western regions, they may not represent all areas in China. Urbanization bias might have been present in the sample. These cities are all metropolitan or provincial capitals in China with relatively good medical resources, economic development levels, and social security. Therefore, the findings may not fully apply to small and medium-sized cities or rural areas51, and they could have underestimated the problems of inadequate rehabilitation resources and poor access to medical services in these areas52. Because of the complexity of data collection and possible interview bias, we did not interview patients or their families. This leads to research that might lack a deep understanding of what patients experience during recovery. The personal experiences, feelings, and family support of patients are essential factors that influence rehabilitation adherence29. However, without this information, our findings may not fully reflect patients’ recovery processes and challenges. Relying solely on medical records or doctors’ reports can lead to data being biased toward the perspective of the healthcare system, ignoring the real experiences and needs of patients in their daily lives. We relied on existing large-scale datasets or literature that answered our research questions without the need to gather additional information through interviews. We did not examine issues related to health insurance and healthcare payments. The economic pressures faced by patients with a history of stroke and their underlying causes may differ because of the variations in health insurance policies across different regions. Furthermore, this study did not specifically include rehabilitation specialists from traditional Chinese Medicine hospitals, despite the important role of traditional Chinese Medicine rehabilitation in stroke recovery in China. This represents an important direction for future research.
Conclusions
In this study, we found that the following factors significantly affect rehabilitation adherence: self-efficacy, trust in physicians, family collaboration, rehabilitation expectations, and economic pressure. Furthermore, multiple elements pertaining to physicians, hospitals, and society can have complex effects on patients, ultimately influencing their rehabilitation compliance. According to medical experts, patients should be proactive and upbeat to increase their expectations and self-efficacy toward rehabilitation. Physicians should build strong patient relationships, communicate more with their patients, earn their trust, and create rehabilitation programs that are interesting and evidence-based. Hospitals should self—assess capabilities and patient needs. Tertiary hospitals can focus on advanced rehab tech (e.g., VR, tele—rehab) and collaborate with research. Secondary and grassroots hospitals should prioritize basic patient—management software and staff training. Tertiary hospitals should form formal interdisciplinary teams with regular communication. Secondary and grassroots hospitals can learn from larger ones and set up joint consultations for stroke patients. Hospitals should also optimize resource allocation according to patient volume and case severity. Tertiary hospitals handle complex cases and high—level rehab, while secondary and grassroots hospitals engage in early intervention and community—based rehab for better system efficiency and timely patient care. The government should increase funding support for rehabilitation medical services to create a favorable environment for patients and enhance societal awareness of rehabilitation medicine.
Data availability
The data that support the findings of this study are available from the author (Meng Liu, menglau@pku.edu.cn) but restrictions apply to the availability of these data, which were used under license from the Institute for Global Health and Development, Peking University (Beijing) for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from the Institute for Global Health and Development, Peking University. Website: https://ghd.pku.edu.cn/xygk/lxwm/index.htm.
References
Global Burden of Disease 2019 Study Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet 396(10258), 1204–1222 (2020).
Wu, S. et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 18(4), 394–405 (2019).
Temporal Trend and Attributable Risk Factors of Stroke Burden in China 1990–2019: An Analysis for the Global Burden of Disease Study 2019. https://www.thelancet.com/pdfs/journals/lanpub/PIIS2468-2667(21)00228-0.pdf.
World Health Organization. Rehabilitation. https://www.who.int/news-room/fact-sheets/detail/rehabilitation. (2024).
Davis, S. M. & Donnan, G. A. Secondary prevention after ischemic stroke or transient ischemic attack. N. Engl. J. Med. 366(20), 1914–1922 (2012).
Hankey, G. J. Secondary stroke prevention. Lancet Neurol. 13(2), 178–194 (2014).
Bangad, A., Abbasi, M. & de Havenon, A. Secondary ischemic stroke prevention. Neurotherapeutics 20(3), 721–731 (2023).
Dobkin, B. H. Rehabilitation after stroke. N. Engl. J. Med. 352(16), 1677–1684 (2005).
Winstein, C. J. et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 47(6), e98–e169 (2016).
The Cerebral Vascular Disease Committee of the Chinese Rehabilitation Medical Association 2020 Academic Annual meeting and the 23rd National Cerebral Vascular Disease Rehabilitation Academic Conference. https://www.carm.org.cn/xwzx/fzjgdt/art/2020/art_dfa39bec2b5f4539b198e56acaa690db.html.
Saunders, D. H. et al. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003316.pub6 (2016).
Veerbeek, J. M. et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PloS ONE 9(2), e87987 (2014).
Teasell, R. et al. Evidence-based review of stroke rehabilitation: Executive summary. Top Stroke Rehabil. 16(6), 463–488 (2009).
Duncan, P. W. et al. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke 33(1), 167–178 (2002).
Bissonnette, J. M. Adherence: A concept analysis. J. Adv. Nurs. 63(6), 634–643 (2008).
Dong, X., Jing, R. & Duan, Y. Research status on adherence to rehabilitation training and its influencing factors among stroke patients. J. Yan’an Univ. (Med. Sci. Ed.) 21(1), 85–88+93 (2023).
Sheng, H. et al. A study on the dynamic changes in rehabilitation exercise adherence among stroke patients. Chin. J. Nurs. 51(6), 712–715 (2016).
Liu, Q. et al. Association between self-efficacy and self-management behaviours among individuals at high risk for stroke: Social support acting as a mediator. J. Clin. Nurs. 32(1–2), 71–82 (2023).
Li, Z. et al. Factors impact the adherence rate of prophylaxis for deep venous thrombosis in acute ischaemic stroke patients: An analysis of the China national stroke registry. Neurol. Res. 37(5), 427–433 (2015).
Zhou, B. et al. Caregiver-delivered stroke rehabilitation in rural China: The RECOVER randomized controlled trial. Stroke 50(7), 1825–1830 (2019).
Chen, M. & Che, C. Perceived Social Support, Self-Management, Perceived Stress, and Post-Traumatic Growth in Older Patients Following Stroke: Chain Mediation Analysis. Medicine (Baltimore) 103(29), e38836 (2024).
Wang, Y. et al. Stroke care quality in China: Substantial improvement, and a huge challenge and opportunity. Int. J. Stroke. 12(3), 229–235 (2017).
Yan, L. L. et al. Prevention, management, and rehabilitation of stroke in low-and middle-income countries. Eneurol. Sci. 2, 21–30 (2016).
Macias, V. et al. Interpersonal challenges in surgical care provision in Rural Mexico: A qualitative study. Lancet Reg. Health Am. https://doi.org/10.1016/j.lana.2022.100210 (2022).
GBD 2019 Neurology Collaborators. Global, regional, and national burden of neurological disorders in 2019: A systematic analysis for the global burden of disease study 2019. Lancet Neurol. 20(5), 317–328 (2021).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 3(2), 77–101 (2006).
Pizzari, T. et al. Adherence to anterior cruciate ligament rehabilitation: A qualitative analysis. J. Sport Rehabil. 11(2), 90–102 (2002).
Smith-Forbes, E. V. Exploration of factors associated with patient adherence in upper extremity rehabilitation: A mixed-methods embedded design [dissertation] (University of Kentucky, 2015).
Pishkhani, M. K., Dalvandi, A., Ebadi, A. & Hosseini, M. Factors affecting adherence to rehabilitation in Iranian stroke patients: A qualitative study. J. Vasc. Nurs. 37(4), 264–271 (2019).
Rosewilliam, S., Roskell, C. A. & Pandyan, A. D. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin. Rehabil. 25(6), 501–514 (2011).
Wiles, R. et al. Exploring the impact of stroke on family carers: A qualitative study. Disabil. Rehabil. 24(6), 296–308 (2002).
McCurley, J. L., Funes, C. J. & Zale, E. L. Preventing chronic emotional distress in stroke survivors and their informal caregivers. Neurocrit. Care 30(3), 581–589 (2019).
Pan, S., Sun, X. & Shan, L. The role of telerehabilitation in stroke care: A systematic review and meta-analysis. J. Telemed. Telecare 22(6), 312–319 (2016).
Ishida, A., Yamaguchi, T. & Shibata, M. Long-term outcomes and predictors of stroke recovery in a community-based cohort. Stroke 54(2), 572–580 (2023).
Miller, E. L., Murray, L. L. & Richards, L. G. Comprehensive overview of nursing and interprofessional care of the stroke patient: A scientific statement from the American heart association. Stroke https://doi.org/10.1161/STR.0b013e3181e7512b (2017).
Naess, H., Lunde, L. & Waje-Andreassen, U. Recurrent stroke and its risk factors: A longitudinal study. Eur. Stroke J. 27(3), 123–129 (2012).
Schulman, J. I., Braun, J. & Stone, G. The role of neuroplasticity in recovery after stroke. Stroke 30(3), 713–717 (1999).
O’Shea, E., Rukundo, A., Foley, G., Wilkinson, T. & Timmons, S. Experiences of health service access: A qualitative interview study of people living with Parkinson’s disease in Ireland. Health Expect. 27(1), e13901 (2024).
Dehghan Nayeri, N., Mohammadi, S., Pedram Razi, S. & Kazemnejad, A. Adherence of family caregivers of patients with stroke to rehabilitation regimen. HAYAT 18(1), 30–41 (2012).
Mitchell, K. Assessment of stroke survivors: assisting families of stroke survivors on acute rehabilitation units. Top. Stroke Rehabil. 16(6), 420–424 (2009).
Allarakha, S., Gupta, R. & Patel, N. Telehealth interventions for post-stroke rehabilitation: An updated review. Telemed. E Health 28(4), 545–552 (2022).
Delbari, A. & Roghani, Salman. Stroke rehabilitation: Principles, advances, early experiences, and realities in Iran. J. Sabzevar Univ. Med. Sci. 19(2), 96–108 (1970).
Yin, Y., Gao, W., Cui, X. & Tang, W. Development and validation of the Chinese patient - centered integrated care scale. BMC Health Serv. Res. 24(1), 1668 (2024).
Glass, T. A. et al. Impact of social support on outcome in first stroke. Stroke 24(1), 64–70 (1993).
Outpatient Service Trialists, Cochrane Stroke Group. Therapy-based rehabilitation services for stroke patients at home. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD002925/full (1996).
Wade, D. T. Stroke: Rehabilitation and long-term care. Lancet 339(8796), 791–793 (1992).
Wiles, R. et al. Patients’ expectations of recovery following stroke: A qualitative study. Disabil. Rehabil. 24(16), 841–850 (2002).
Higashida, R. et al. Interactions within stroke systems of care: A policy statement from the American Heart Association/American stroke association. Stroke 44(10), 2961–2984 (2013).
Springer, M. V., Skolarus, L. E. & Patel, M. Food insecurity and perceived financial stress are associated with cost-related medication non-adherence in stroke. J. Health Care Poor Underserved 34(2), 625–639 (2023).
Allen, L. J. A cost-effectiveness study of home-based stroke rehabilitation (Univ Western Ontario (Canada), 2015).
Wang, L. et al. Body - mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004–18. Lancet 398(10294), 53–63 (2021).
Jing, Q. et al. Regional disparities of rehabilitation resources for persons with disabilities in China: data from 2014 to 2019. Int. J. Environ. Res. Public Health 17(19), 7319 (2020).
Acknowledgements
The authors wish to thank all the experts who participated in the interviews and provided valuable insights for this study.
Author information
Authors and Affiliations
Contributions
Meng Liu, Ziting Wu, and Gordon G. Liu contributed equally to the work as joint first authors. Meng Liu and Gordon G. Liu conceived the study, designed the interview process, analyzed the data, and wrote the manuscript. Ziting Wu participated in the interview process, content organization, data sorting, and manuscript writing. Luyang Xiao and Shanshan Li contributed to data collection, the interview process, and manuscript revision. All authors critically reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All authors have consented to the publication of this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, M., Wu, Z., Liu, G.G. et al. Barriers and facilitators for stroke patients’ adherence to rehabilitation in China: a qualitative study based on medical experts. Sci Rep 15, 31525 (2025). https://doi.org/10.1038/s41598-025-12795-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-12795-w