Abstract
Overactive bladder (OAB) significantly affects places a considerable economic strain and individuals’ quality of life on global healthcare resources.The ratio of red cell distribution width to albumin (RAR) is a novel inflammatory marker, yet its association with the prevalence of OAB among adults in the U.S. remains unclear. This nationally representative cross-sectional study utilized data derived from the 2005–2020 National Health and Nutrition Examination Survey (NHANES), focusing primarily on individuals aged 20 and older with complete information on red cell distribution width (RDW) and albumin. Subgroup analyses, multivariate logistic regression, and restricted cubic spline (RCS) models were employed to investigate the association of the risk of OAB and the levels of RAR. Additionally, receiver operating characteristic (ROC) curves were used to evaluate the predictive performance of RAR levels for OAB.An overall of 26,987 participants aged over 20 years were included in the analysis, of whom 4,943 were diagnosed with OAB. Both before and after adjusting for potential confounders, the results consistently indicated a significant positive correlation of RAR with the risk of OAB. Using the first quartile (Q1) of RAR as the reference, people in the highest quartile (Q4) had a 41% increased risk of OAB relative to those in Q1 after adjusting for all covariates. The RCS curve revealed a nonlinear relationship between RAR and OAB. Furthermore, interaction tests and subgroup analyses indicated that age modified the positive correlation between OAB and RAR. ROC curve analysis revealed that the cutoff value for predicting OAB with RAR was 3.07 (specificity: 57.70%, sensitivity: 64.64%, AUC: 0.649).In U.S. adults, elevated levels of RAR are related to an increased risk of OAB. RAR levels may serve as a potential marker for the development of OAB.
Similar content being viewed by others
Introduction
OAB is described as a condition marked by urinary urgency, frequently accompanied by increased frequency and nocturia, with or without urge urinary incontinence. This condition occurs in the absence of urinary tract infections or other obvious pathological causes1.The prevalence of OAB in adults in the U.S. is 16.0% in men and 16.9% in women, with Urgency Urinary Incontinence (UUI) occurring more frequently in women and becoming notably more prevalent with age, especially after middle age2.OAB is a prevalent and disruptive chronic condition that profoundly affects daily living and creates considerable economic strain3.Reports indicate that in the U.S., the economic impact of UUI related to OAB totaled $82.6 billion in 20204.Research suggests that the development of OAB may be linked to various contributing factors, including psychological issues such as anxiety, depression, and suicidal thoughts5,6,7.
RDW is a widely employed laboratory measure that indicates systemic inflammation and is linked to several conditions, such as pneumonia, cancer, and chronic obstructive pulmonary disease (COPD)8. Serum albumin, the predominant circulating protein in the blood, serves as a crucial indicator of both nutritional status and inflammatory response9.RAR, recognized as an emerging marker for assessing nutritional status and inflammation, has been previously utilized to predict outcomes in patients with heart failure and chronic kidney disease10,11.Nevertheless, no studies have yet explored the association of RAR with OAB. Thus, this cross-sectional study utilizes data collected during the 2005–2020 NHANES to investigate the relationship of RAR with OAB risk. This research may contribute to advancing further studies on interventions and prevention strategies for OAB, while also providing insights into its underlying pathophysiological mechanisms.
Methods
Study population
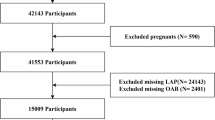
In this nationally representative cross-sectional study, the data were sourced from the NHANES datasets covering the period from 2005 to 2020.All participants provided written informed consent, and the study protocol was authorized by the Institutional Review Board (IRB) of the National Center for Health Statistics.Based on the questionnaire surveys and laboratory tests from the NHANES database, this study focuses on exploring the relationship of the red cell distribution width to albumin ratio (RAR) with overactive bladder (OAB). A total of 76,496 NHANES participants were initially included in the study, with the inclusion criteria being: age 20 years or older, comprehensive data on RDW, nocturia frequency, albumin, and urgency urinary incontinence, as well as other relevant covariates. After screening, a final sample of 26,987 participants was selected for analysis;Exclusion criteria: age < 20 years, cancer, or incomplete data. The process is comprehensively outlined in Fig. 1.
Assessment of OAB and RAR
RAR is calculated as the ratio of RDW to serum albumin levels, both derived from standardized laboratory measurements of participant blood samples12.OAB is a symptomatic syndrome characterized by urinary urgency, often accompanied by nocturia and frequency, with or without urgency urinary incontinence1.The presence of the above symptoms was determined through a questionnaire survey, followed by a comprehensive scoring system. According to previous research,OAB is diagnosed with the help of the Overactive Bladder Symptom Score (OABSS), where a score of 3 or higher is defined as indicative of OAB(Table S1)7,13,14.Due to limited diagnostic granularity in the database, we were unable to exclude patients with conditions that may be similar to OAB symptoms (e.g., interstitial cystitis, chronic cystitis).
Assessment of covariates
The covariates for this research were derived from the NHANES data and included marital status, alcohol consumption,hypertension, sex, age, diabetes, body mass index, cardiovascular disease, race, smoking status, family poverty income ratio,SII,PLR,NLR and symptoms of depression. Based on these variables, participants were further stratified to analyze their clinical characteristics. This analytical approach enables evaluation of potential confounding effects from these variables on the RAR-OAB association, thereby strengthening the validity of our model in detecting clinically relevant relationships.
Statistical analysis
The participants’ baseline characteristics were described according to different RAR levels and the presence of OAB. Continuous variables were reported as weighted means with standard errors, while categorical variables were expressed as weighted percentages. Differences between RAR level quartiles and OAB groups were compared employing the Kruskal–Wallis H test or the Chi-squared test, as appropriate. The non-linear association of OAB with RAR levels was assessed with RCS curves. Logistic regression was employed to analyze the association of OAB with RAR levels, with odds ratios (OR) and 95% confidence intervals (CI) calculated. Three analytical models were applied: an unadjusted crude model, Model 1 adjusted for sex,age, and race, and Model 2 adjusted for sex, age,race,diabetes mellitus, marital status, hypertension, alcohol consumption, family poverty income ratio, SII,PLR,NLR,smoking status, cardiovascular disease, depression and body mass index.Subgroup analyses were carried out to examine the consistency of this relationship across various groups.All analyses were carried out utilizing R software (version 4.3.2), and a P-value of less than 0.05 deemed statistically meaningful.
Results
Baseline characteristics of participants
This study involved a total of 26,987 adults aged 20 and above, with a prevalence of overactive bladder (OAB) of 18.32% (n = 4,943). the average BMI of the participants was 29.12 ± 0.08 kg/m2, and The average age was 45.56 ± 0.24 years. Among the participants, 49.62% (n = 13,391) were female, 41.93% (n = 11,316) were non-Hispanic white,31.09% (n = 8,390) had a family poverty income ratio of 1.3 or less, and 59.99% (n = 16,189) were married or living with a partner.Regarding personal lifestyle factors, 72.08% (n = 19,453) reported a history of alcohol consumption, while only 21.27% (n = 5,741) were current smokers. In terms of clinical comorbidities, the prevalence rates were as follows: 40.18% (n = 10,843) had hypertension, 9.34% (n = 2,520) had cardiovascular disease, and 17.47% (n = 4,715) had diabetes. Table 1 summarizes the detailed characteristics based on participants’ OAB status. The findings indicate that people with OAB tended to be older, female, married or living with a partner, Non-Hispanic White, lower family poverty income ratios, report alcohol consumption, be never-smokers, and present with comorbidities including obesity and hypertension. Furthermore, OAB patients exhibited higher RAR levels, elevated RDW, and lower albumin levels compared to those without OAB.
The association between OAB and RAR
The results in Table 2 demonstrate a positive correlation between RAR as a continuous variable and the likelihood of OAB. In the crude model, without accounting for any covariates, each one-unit rise in RAR was linked to a 1.48-fold higher likelihood of OAB (95% CI(2.27,2.70), P < 0.0001). This relationship continued to be significant in Model 2, which adjusted for all covariates(OR: 1.22, 95% CI(1.10,1.36), P < 0.001). Furthermore,in the fully adjusted model based on RAR quartiles, higher levels, such as Q4, were linked to a 41% greater likelihood of OAB compared to the lowest quartile (Q1) (95% CI:(1.17,1.70), P < 0.001).Then, we examined the nonlinear correlation between RAR and OAB using RCS curves (Fig. 2). The analysis revealed a potential dose–response relationship, with a turning point at an RAR value of 3.07. The odds ratio for OAB prevalence increased rapidly with rising RAR levels, and after reaching the turning point, the rate of increase slowed, exhibiting a saturation effect. To further evaluate the ability of RAR to predict OAB, we performed a ROC curve analysis (Fig. 3). The findings revealed that the optimal cutoff value for identifying OAB using RAR was 3.07, with a specificity of 57.70%, sensitivity of 64.64%, and an AUC of 0.649.
Subgroup analysis
To further investigate the correlation of OAB risk with RAR levels, this study conducted interaction tests and subgroup analyses based on sex,age, race , depression,smoking status , body mass index, diabetes mellitus, marital status, alcohol consumption, cardiovascular disease, and hypertension (Table 3). The results revealed that the positive correlation of elevated RAR levels with increased OAB risk remained consistent across various subgroups, including race, sex, family poverty income ratio, marital status, cardiovascular disease, depression,body mass index , diabetes mellitus, alcohol consumption, hypertension, and smoking status. However, the study adjusts for multiple confounding factors such as age, sex, and BMI, but there remains the potential for residual confounding, particularly with age and alcohol consumption.
Discussion
In this cross-sectional study of 26,987 U.S. adults, we identified a robust association between elevated RAR levels and increased OAB risk, which persisted after full adjustment for all included covariates. Additionally, subgroup analyses suggested that age and drinking status are the factor influencing the association between RAR levels and OAB. As an excellent marker of inflammation risk, this research is the first to explore the connection of RAR levels with OAB. Our findings reveal that RAR exhibited higher AUC values than the remaining inflammatory biomarkers, highlighting its superior performance inpredicting OAB.These findings highlight the important clinical significance of monitoring and intervening in RAR levels to potentially reduce the incidence of OAB.
Substantial evidence has established inflammation as a critical contributor to both the initiation and progression of overactive bladder (OAB). Chronic inflammatory stimulation induces functional modifications in bladder physiology, particularly heightened sensory sensitivity, which ultimately manifests as characteristic OAB symptoms15.In OAB patients, various inflammatory cells infiltrate the bladder, and substances such as IL-5 and macrophage inflammatory protein are also detected in their urine16.Furthermore, studies have revealed an increase in the number and activity of mast cells, T-lymphocytes, and B-lymphocytes within the detrusor muscle of OAB patients17,18,19.
RDW has emerged as a significant prognostic biomarker across various pathophysiological states, particularly in chronic kidney disease and inflammatory conditions, while also demonstrating an independent association with sepsis outcomes20,21.Serum albumin is a well-known negative acute-phase reactant, with its levels declining during inflammation as a result of enhanced microvascular permeability and subsequent albumin leakage22.Earlier research has highlighted a robust link between RAR levels and the likelihood of developing acute kidney injury (AKI) in septic patients23.Additionally, Shan et al. identified RAR as a standalone predictor of septic shock and mortality in severely patients with community-acquired bacteremia24.RAR, the ratio of RDW to albumin, provides a deeper and detailed evaluation of inflammation in contrast to the use of each marker separately25.
Previous studies have demonstrated that in patients with liver cirrhosis, impaired hepatic albumin synthesis leads to reduced serum albumin levels and compromised albumin function, which may disrupt both antioxidant defense mechanisms and immune regulation, potentially exacerbating bladder inflammation26,27.Chung et al. have demonstrated that male gender, a higher serum albumin and hemoglobin levels were linked to a reduced likelihood of nocturia28.Moreover, Lin et al. showed that low-intensity extracorporeal shock wave therapy (LI-ESWT) can alleviate inflammation, promote cell differentiation and stimulate cell proliferation, diminish urinary incontinence, and attenuate OAB manifestations29.Based on the calculation formula for RAR,these findings indicate a possible connection between RAR levels and the likelihood of developing OAB.Potts et al. discovered that the occurrence of overactive bladder rises notably in both men and women with age30.Although age is adjusted in three groups (20–39, 40–59, and ≥ 60), this may still not fully capture the impact of age on OAB symptoms. Interestingly, the subgroup analysis shows significantly high odds ratios (OR) in the 20–39 age group for Q4 (OR 1.91), which suggests a strong correlation between RAR and OAB in younger, otherwise healthy individuals.In younger, the stress and psychological distress associated with career development may increase susceptibility to OAB31. Salaffi et al. alrevealed a positive relationship between sexual dysfunction and variables of OAB burden32.This could have important implications for future diagnostic and therapeutic approaches for young OAB patients. Alcohol consumption can negatively affect OAB through multiple mechanisms. Acetaldehyde, a toxic byproduct of alcohol metabolism, contributes to tissue damage via oxidative stress, inflammation, and DNA adduct formation. Additionally, alcohol’s diuretic effect reduces fluid intake and causes dehydration, leading to concentrated urine33. This irritates the bladder wall, increasing the risk of OAB and urge incontinence.
Our research presents several strengths.This research utilized the robust NHANES database, which features a nationally representative sample and rigorous data collection techniques.RAR, evaluated via laboratory tests, could serve as an effective marker. Its ease of use and consistency make it an important resource for recognizing individuals at elevated risk for OAB in clinical settings.The cross-sectional design, however, constrains the potential to infer a causal connection of RAR with OAB risk.While our study identifies a significant correlation between RAR and OAB symptoms, the clinical applicability of RAR as a biomarker requires further validation through longitudinal or interventional studies to assess its utility in diagnostic or therapeutic decision-making.Additionally, the use of questionnaires may introduce recall bias, particularly regarding information on OAB symptoms.Therefore, future prospective studies are essential to examine the longitudinal correlation link of RAR levels with OAB. Future research should investigate whether RAR levels are associated with OAB symptom severity, treatment response, or OAB subtypes, as this may further elucidate its clinical relevance.
Conclusion
In conclusion, elevated levels of RAR are linked to a higher likelihood of OAB in U.S. adults. RAR might potentially serve as a predictive factor in OAB development, with further prospective studies needed to validate its role as a biomarker.
Data availability
The datasets generated and analysed during the current study are available in the NHANES.If you want to request the data from this study,please contact with corresponding author or direct link to dataset used.(https://wwwn.cdc.gov/Nchs/Nhanes/).
References
Henderson, E. & Drake, M. Overactive bladder. Maturitas 66(3), 257–262. https://doi.org/10.1016/j.maturitas.2010.03.010 (2010).
Stewart, W. F. et al. Prevalence and burden of overactive bladder in the United States. World J. Urol. 20(6), 327–336. https://doi.org/10.1007/s00345-002-0301-4 (2003).
Gibson, S. & Ellsworth, P. Emerging therapies for overactive bladder: preclinical, phase I and phase II studies. Expert Opin. Investig. Drugs. 33(6), 601–612. https://doi.org/10.1080/13543784.2024.2349285 (2024).
Funada, S. et al. Multicomponent intervention for overactive bladder in women: a randomized clinical trial. JAMA Netw Open. 7(3), e241784. https://doi.org/10.1001/jamanetworkopen.2024.1784 (2024).
Zhang, Y. et al. Association between overactive bladder and depression in American adults: A cross-sectional study from NHANES 2005–2018. J. Affect Disord. 1(356), 545–553. https://doi.org/10.1016/j.jad.2024.04.030 (2024).
Vrijens, D. et al. Affective symptoms and the overactive bladder - a systematic review. J. Psychosom. Res. 78(2), 95–108. https://doi.org/10.1016/j.jpsychores.2014.11.019 (2015).
Gong, H. & Huang, S. Associations of overactive bladder (OAB) with suicidal ideation incidence and all-cause mortality among the U.S. population. BMC Psychiatry 24(1), 641. https://doi.org/10.1186/s12888-024-06107-1 (2024).
Tan, Y. et al. The ratio of red blood cell distribution width to albumin as a predictor for rehospitalization risk and rehospitalization all-cause mortality in middle-aged and elderly survivors with sepsis: an ambispective icu cohort study. J. Inflamm. Res. 22(17), 1227–1240. https://doi.org/10.2147/JIR.S451769 (2024).
Masenga, S. K., Kabwe, L. S., Chakulya, M. & Kirabo, A. Mechanisms of oxidative stress in metabolic syndrome. Int. J. Mol. Sci. 24(9), 7898. https://doi.org/10.3390/ijms24097898 (2023).
Kimura, H. et al. Impact of red blood cell distribution width-albumin ratio on prognosis of patients with CKD. Sci Rep. 13(1), 15774. https://doi.org/10.1038/s41598-023-42986-2 (2023).
Ni, Q., Wang, X., Wang, J. & Chen, P. The red blood cell distribution width-albumin ratio: A promising predictor of mortality in heart failure patients - A cohort study. Clin. Chim. Acta. 15(527), 38–46. https://doi.org/10.1016/j.cca.2021.12.027 (2022).
Guo, H., Wang, Y., Miao, Y. & Lin, Q. Red cell distribution width/albumin ratio as a marker for metabolic syndrome: findings from a cross-sectional study. BMC Endocr. Disord. 24(1), 227. https://doi.org/10.1186/s12902-024-01762-7 (2024).
Du, Y. Z. et al. The relationship between dietary live microbe intake and overactive bladder among American adults: a cross-sectional study from NHANES 2007–2018. J. Health Popul. Nutr. 43(1), 120. https://doi.org/10.1186/s41043-024-00612-5 (2024).
Lin, W. et al. Association of socioeconomic status and overactive bladder in US adults: a cross-sectional analysis of nationally representative data. Front Public Health. 26(12), 1345866. https://doi.org/10.3389/fpubh.2024.1345866 (2024).
Hsu, L. N., Hu, J. C., Chen, P. Y., Lee, W. C. & Chuang, Y. C. Metabolic syndrome and overactive bladder syndrome may share common pathophysiologies. Biomedicines. 10(8), 1957. https://doi.org/10.3390/biomedicines10081957 (2022).
Tyagi, P. et al. Urine cytokines suggest an inflammatory response in the overactive bladder: a pilot study. Int. Urol. Nephrol. 42(3), 629–635. https://doi.org/10.1007/s11255-009-9647-5 (2010).
Zhang, N. Z., Ma, L., Jun, C., Guo, Y. X. & Yuan, H. Q. Changes in mast cell infiltration: a possible mechanism in detrusor overactivity induced by visceral hypersensitivity. Int. Braz. J. Urol. 42(2), 373–382. https://doi.org/10.1590/S1677-5538.IBJU.2015.0025 (2016).
Liu, H. T., Shie, J. H., Chen, S. H., Wang, Y. S. & Kuo, H. C. Differences in mast cell infiltration, E-cadherin, and zonula occludens-1 expression between patients with overactive bladder and interstitial cystitis/bladder pain syndrome. Urology 80(1), 225.e13–8. https://doi.org/10.1016/j.urology.2012.01.047 (2012).
Gamper, M. et al. Local immune response in bladder pain syndrome/interstitial cystitis ESSIC type 3C. Int. Urogynecol. J. 24(12), 2049–2057. https://doi.org/10.1007/s00192-013-2112-0 (2013).
Saito, H. et al. Hematological parameters of anemia and prognosis of non-dialysis-dependent chronic kidney disease: the Fukushima CKD cohort study. Clin. Exp. Nephrol. 27(1), 55–65. https://doi.org/10.1007/s10157-022-02282-1 (2023).
Wu, H. et al. Diagnostic value of RDW for the prediction of mortality in adult sepsis patients: A systematic review and meta-analysis. Front. Immunol. 17(13), 997853. https://doi.org/10.3389/fimmu.2022.997853 (2022).
Soeters, P. B., Wolfe, R. R. & Shenkin, A. Hypoalbuminemia: Pathogenesis and Clinical Significance. JPEN J. Parenter. Enteral. Nutr. 43(2), 181–193. https://doi.org/10.1002/jpen.1451 (2019).
Xu, Y. & Qi, W. Association between red cell distribution width to albumin ratio and acute kidney injury in patients with sepsis: a MIMIC population-based study. Int. Urol. Nephrol. 55(11), 2943–2950. https://doi.org/10.1007/s11255-023-03572-7 (2023).
Shan, X., Jiang, J., Li, W. & Dong, L. Red blood cell distribution width to albumin ratio as a predictor of mortality in ICU patients with community acquired bacteremia. Sci. Rep. 14(1), 28596. https://doi.org/10.1038/s41598-024-80017-w (2024).
Long, J. et al. Association between red blood cell distribution width-to-albumin ratio and prognosis of patients with aortic aneurysms. Int. J. Gen. Med. 1(14), 6287–6294. https://doi.org/10.2147/IJGM.S328035 (2021).
Garcia-Martinez, R. et al. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology 58(5), 1836–1846. https://doi.org/10.1002/hep.26338 (2013).
Taverna, M., Marie, A. L., Mira, J. P. & Guidet, B. Specific antioxidant properties of human serum albumin. Ann. Intensive Care. 3(1), 4. https://doi.org/10.1186/2110-5820-3-4 (2013).
Chung, M. S. et al. Prevalence and associated risk factors of nocturia and subsequent mortality in 1,301 patients with type 2 diabetes. Int. Urol. Nephrol. 46(7), 1269–1275. https://doi.org/10.1007/s11255-014-0669-2 (2014).
Lin, K. L. et al. Low-Intensity Extracorporeal Shock Wave Therapy Promotes Bladder Regeneration and Improves Overactive Bladder Induced by Ovarian Hormone Deficiency from Rat Animal Model to Human Clinical Trial. Int J Mol Sci. 22(17), 9296. https://doi.org/10.3390/ijms22179296.PMID:34502202;PMCID:PMC8431217 (2021).
Potts, J. M. & Payne, C. K. Urinary Urgency in the Elderly. Gerontology 64(6), 541–550. https://doi.org/10.1159/000492330 (2018) (Epub 2018 Aug 29 PMID: 30157480).
Kim, S. Y., Bang, W. & Choi, H. G. Analysis of the prevalence and associated factors of overactive bladder in adult Korean men. PLoS ONE 12(4), e0175641. https://doi.org/10.1371/journal.pone.0175641 (2017).
Salaffi, F. et al. Overactive bladder syndrome and sexual dysfunction in women with fibromyalgia and their relationship with disease severity. Clin. Exp. Rheumatol. 40(6), 1091–1101. https://doi.org/10.55563/clinexprheumatol/9mbbpb (2022).
Wallner, M. & Olsen, R. W. Physiology and pharmacology of alcohol: the imidazobenzodiazepine alcohol antagonist site on subtypes of GABAA receptors as an opportunity for drug development?. Br. J. Pharmacol. 154(2), 288–298. https://doi.org/10.1038/bjp.2008.32 (2008).
Acknowledgements
We would like to express our gratitude to the participants and researchers of NHANES.
Funding
This research is supported by the National Natural Science Foundation (82160474) ,Provincial Chinese Medicine Science and Technology Program(2021B686) and Provincial Health Commission Science and Technology Program Project(202210401).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the work:K.Z.,Z.R.,X.C.,ZG,JL conceived this study;KZ,ZR and XC completed the data collection and data analysis.ZG and JL participated in the collating of the results.KZ completed the manuscript.YZ supervised the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The ethical review board of the National Center for Health Statistics granted approval to the NHANES protocols, and ethical approval was exempted in this study.The National Institutes of Health obtained written consent from subjects for the collection and utility data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, K., Rao, Z., Chen, i. et al. Association of overactive bladder with red cell distribution width to albumin ratio in American. Sci Rep 15, 27395 (2025). https://doi.org/10.1038/s41598-025-13129-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13129-6