Abstract
There is a lack of research on hepatitis B virus (HBV) reactivation and prognosis in hepatocellular carcinoma (HCC) patients with undetectable HBV DNA after systemic therapy. This study aims to compare HBV reactivation (HBVr) and prognosis between patients treated with tyrosine kinase inhibitor (TKI) monotherapy and those receiving TKI combined with programmed cell death protein‑1 (PD-1) inhibitors. The retrospective study comprised 877 advanced HCC patients from two medical centers with undetectable HBV DNA, receiving TKI monotherapy (n = 419) or TKI plus PD-1 inhibitors (n = 458). HBVr rates, tumor progression, and overall survival (OS) were analyzed. The HBVr rate markedly higher in the combination cohort compared to the TKI monotherapy cohort (16.6% vs. 12.5%, P = 0.018). Multivariable regression analysis identified the combination therapy (HR 1.295, 95%CI 1.010–1.662, P = 0.042), ALT > 40 U/ml (HR 1.460, 95%CI 1.079–1.978, P = 0.014), Hepatitis B e antigen (HBeAg) positivity (HR 1.570, 95%CI 1.133–2.174, P = 0.007), and tumor size > 5 cm (HR 1.394, 95%CI 1.051–1.848, P = 0.021) as independent predictors of HBVr. Patients receiving antiviral prophylaxis had a lower HBVr rate than those not receiving it (27.4% vs. 33.7%, P = 0.013). Patients with HBVr had shorter progression-free survival (PFS) (P < 0.001) and OS (P < 0.001) compared to those without HBVr. TKI plus PD-1 inhibitors increases the risk of HBVr compared to TKI monotherapy, leading to higher tumor progression and shorter OS. Continuous antiviral therapy can help prevent HBVr after systemic treatment in HCC patients.
Similar content being viewed by others
Introduction
HCC is the third leading cause of cancer-related deaths globally1, with the majority arising from chronic liver disease, and over 50% of HCC cases being HBV-related2. HBV remains lifelong in patients because of covalently closed circular DNA (cccDNA) in the liver, which antiviral therapies cannot fully eradicate, necessitating long-term antiviral treatment to prevent viral replication3. HBVr is a critical issue, as it can interfere with antitumor treatments, accelerate tumor progression, and reduce survival. Common causes of HBVr include viral genome mutations, immunosuppressive therapy, and virus- or drug-induced immune damage. The immune system is crucial in both preventing HBV infection and its reactivation4.When the equilibrium between immune response and viral replication is disrupted, HBVr occurs.
For advanced unresectable hepatocellular carcinoma (uHCC), systemic therapy is crucial and significantly prolongs survival5. Since the introduction of sorafenib in 2007, TKIs have been a powerful tool in uHCC treatment6. Recently, the combination of PD-1 inhibitors and TKIs has gained increasing attention. PD-1 inhibitors can synergize with TKIs, and by combining anti-angiogenic agents with immune checkpoint inhibitors appropriately, tumor vascular normalization can be induced, improving the tumor microenvironment and enhancing antitumor immunity7. However, concerns about HBVr due to immunotherapy persist. Studies, such as by Knolle et, suggest PD-1 inhibitors act as key immunosuppressive mediators, preventing excessive liver damage8. Blocking the PD-1/PD-L1 axis has the potential to disrupt hepatocytes, releasing latent viruses into circulation. Moreover, PD-1 inhibitors can inhibit regulatory T cell proliferation, and blocking PD-1 may enhance Treg cell activity, potentially increasing immunosuppression and leading to HBVr9.
Previous reports have indicated that systemic therapy drugs may lead to HBVr. In a retrospective study of 171 hepatitis B surface antigen (HBsAg) positive non-small cell lung cancer patients treated with TKIs, Yao et al.10 found that 16 cases (9.36%) experienced HBVr. The mechanism by which TKIs cause HBVr might involve immunosuppression11,12. There have been more frequent reports of HBVr caused by immune checkpoint inhibitors (ICIs). A retrospective study by Zhang et al.13 indicated that among 114 HBsAg-positive patients undergoing anti-PD-1/PD-L1 therapy, 6 cases (5.3%) experienced HBVr within 18 weeks of treatment initiation. The mechanism by which anti-PD-1/PD-L1 therapy induces HBVr is not fully understood. The PD-1/PD-L1 pathway is involved not only in cancer immune evasion but also in the process of HBV infection. Inhibiting the PD-1/PD-L1 axis can cause HBVr by damaging hepatocytes, releasing latent viruses, or modulating T cell function, such as promoting Treg proliferation. Despite the immune-enhancing effects of ICIs, HBVr may still occur during treatment.
Studies have typically defined HBVr as either a conversion of HBsAg from negative to positive, or by referencing the American Association for the Study of Liver Diseases (AASLD) 2018 reactivation criteria14: (1) an increase in HBV DNA by ≥ 2 log IU/mL from baseline if HBV DNA was detectable at baseline, (2) HBV DNA ≥ 3 log IU/mL if HBV DNA was undetectable at baseline, or (3) HBV DNA ≥ 4 log IU/mL when baseline levels are unknown. This definition is relatively broad and lacks specific criteria for patients undergoing immunotherapy. Various guidelines have different thresholds for HBV DNA levels to define reactivation, and studies focusing on HBV DNA reactivation, particularly in patients with undetectable HBV DNA, are limited. Additionally, there is a lack of data on the reactivation and survival rates in HCC cases with undetectable HBV DNA, especially in those receiving long-term antiviral therapy or immunotherapy. Previous studies have not standardized baseline HBV DNA levels, leaving the evaluation of reactivation under various therapeutic strategies unclear. Therefore, this study intends to assess HBVr rates among HCC patients with undetectable HBV DNA treated with either TKI monotherapy or in conjunction with TKI and PD-1 inhibitors. We also seek to evaluate whether prophylactic antiviral therapy given before treatment impacts the outcomes of reactivation and assess the effects of HBVr on tumor progression and OS.
Method
Patients
This retrospective cohort study encompassed all HCC patients who visited the Fifth Medical Center of the Chinese PLA General Hospital and the Affiliated Hospital of Guizhou Medical University from January 2019 to January 2024. HCC was diagnosed by pathology or two radiological imaging techniques. Inclusion criteria: (1) Patients over 18 years of age; (2) HBsAg seropositive with undetectable baseline HBV DNA; (3) continuous antiviral therapy after baseline; (4) received at least one month of PD-1 inhibitor plus TKI treatment or TKI monotherapy. Exclusion criteria: (1) history of other malignancies, other viral hepatitis, or HIV infection; (2) incomplete follow-up data for HBV DNA or imaging assessments; (3) follow-up intervals exceeding 5 months or incomplete medical records.
Different guidelines vary slightly in their definitions of HBVr but generally rely on evaluating changes in HBV DNA levels relative to baseline values. For example, reactivation is indicated when HBV DNA becomes detectable in clinically cured patients (HBsAg-negative, HBcAb-positive), when HBsAg converts from negative to positive, or when HBV DNA increases by ≥ 2 log IU/mL. In this study, all participants were HCC patients with undetectable HBV DNA at baseline. According to the 2021 guidelines of the Asian-Pacific Association for the Study of the Liver (APASL)15, two definitions of HBVr were adopted: Definition A, in which undetectable baseline HBV DNA becomes detectable; and Definition B, in which undetectable baseline HBV DNA increases to ≥ 100 IU/mL.
This retrospective study was conducted in accordance with the ethical principles of the Declaration of Helsinki and was approved by the ethics committees of two medical centers, with written informed consent waived. The approving committees were the Ethics Committee of the Fifth Medical Center of Chinese PLA General Hospital (KY-2024-9-149-1) and the Ethics Committee of the Affiliated Hospital of Guizhou Medical University (2023-NO.934). The study has been registered in the Chinese Clinical Trial Registry (ChiCTR2500101601). All methods used followed relevant regulations. TKI or PD-1 inhibitor therapy was administered according to the dosing and administration guidelines specified in the respective drug labels.
Data collection and outcomes
All initial data, including demographic information, liver function, antiviral therapy regimen, and cancer characteristics, were collected. Follow-up visits were conducted every 3 to 5 months after the initiation of treatment, with contrast-enhanced abdominal CT or MRI scans performed during each visit, and HBV DNA levels were measured. HBV DNA levels were measured using an automated nucleic acid extraction system (Natch S Pro) with magnetic bead-based extraction. Quantification was performed with the Roche COBAS Z 480 real-time PCR system using a commercial HBV DNA quantification kit (PCR-fluorescence probe method). The lower limit of detection was 40 IU/mL. The primary endpoint was HBVr. Secondary endpoints included tumor progression (evaluated using RECIST version 1.1) and OS, which was measured from the start of systemic therapy until cancer-related death or the last follow-up.
Statistical analysis
Statistical analyses were conducted using SPSS version 29.0. Continuous variables are presented as mean ± standard deviation or median (interquartile range, IQR). The chi-square test was used to analyze categorical variables. Continuous variables were analyzed using the Student’s t-test or Wilcoxon test. Kaplan-Meier curves were used to assess cumulative probabilities for primary and secondary endpoints, with the log-rank test applied for comparisons. Cox proportional hazards regression analysis was used to calculate adjusted hazard ratios (HR). Statistical significance was defined as a P-value of < 0.05, with all tests being two-tailed.
Results
Patient characteristics and outcomes
A total of 1,822 HCC patients receiving systemic therapy were screened for the study, and 945 were excluded for the following reasons: 725 had detectable HBV DNA, 108 lacked adequate HBV DNA follow-up, 74 were HBsAg-negative, 20 received PD-1 inhibitor monotherapy, 11 had other primary tumors, 5 had other viral hepatitis or HIV infections, and 2 had undergone liver transplantation. Ultimately, 877 HCC patients with undetectable HBV DNA were included, with 419 receiving TKI monotherapy and 458 undergoing TKI combined with PD-1 therapy (Fig. 1).
No significant statistical differences in baseline characteristics were observed between the two cohorts (Table 1). Most patients were male (n = 742, 84.6%), and a large proportion had stage C according to the Barcelona Clinic Liver Cancer (BCLC) staging system (n = 520, 59.2%). Most patients had Child-Pugh A liver function (n = 652, 74.3%). In the TKI monotherapy cohort, lenvatinib (n = 227, 25.8%) and sorafenib (n = 156, 17.7%) were the most commonly used treatments, while in the TKI plus PD-1 cohort, lenvatinib plus sintilimab (n = 163, 18.5%) was the most frequently used regimen.
HBV reactivation
Among the 877 HCC patients with undetectable HBV DNA, 256 patients (29.1%) experienced reactivation according to Definition A (110 patients in the TKI cohorts [12.5%], 146 in the TKI combined with PD-1 cohort [16.6%]), while 181 patients (20.6%) experienced reactivation according to Definition B (74 in the TKI cohort [8.4%], 107 in the TKI plus PD-1 cohort [12.2%]). The reactivation rate in the TKI plus PD-1 cohort was significantly higher than in the TKI monotherapy cohort, under both Definition A (P = 0.018) and Definition B (P = 0.009) (Fig. 2a and b). According to the 2018 AASLD reactivation criteria, HBVr occurred in 13 patients (3.1%) in the TKI group and 33 patients (7.2%) in the TKI + PD-1 group. Given the similar conclusions, no additional figures were generated. A subgroup analysis was performed comparing the most commonly used regimens in both cohorts (lenvatinib/lenvatinib plus sintilimab). Similarly, the lenvatinib plus sintilimab combination had a higher reactivation rate than lenvatinib alone, under both Definition A (P = 0.013) and Definition B (P = 0.043) (Fig. 2c and d).
High viral load of HBV DNA
In this study, four patients experienced reactivation with an HBV DNA viral load greater than 105 IU/mL (Table 2). HBVr occurred at 16 weeks, 36 weeks, 92 weeks, and 120 weeks, respectively. All four patients were male, with three receiving a TKI plus PD-1 inhibitor regimen. Two patients were initially HBeAg-negative but converted to HBeAg-positive after reactivation. None of the patients changed their antiviral medications, and subsequent follow-up showed either a decline or clearance of HBV DNA. None of the four patients exhibited signs of reactivation-associated hepatitis or elevated AFP levels during reactivation. However, three patients experienced tumor progression: one discontinued targeted immunotherapy due to upper gastrointestinal bleeding, while the other two received local treatments. Overall, HBVr was associated with tumor progression and interfered with cancer treatment.
Risk factors for HBV reactivation
Tables 3 and 4 presents the results of univariate and multivariate analyses of risk factors associated with HBVr under two definitions. Univariate analysis indicated that under Definition A, combination therapy (P = 0.015), ALT > 40 U/L (P = 0.006), HBeAg (+) (P = 0.015), AFP ≥ 400 ng/mL (P = 0.017), extrahepatic metastasis (P = 0.041), and tumor size > 5 cm (P = 0.005) were significant risk factors for HBVr. Under Definition B, combination therapy (P = 0.007), ALT > 40 U/L (P = 0.009), HBeAg (+) (P = 0.014), AFP ≥ 400 ng/mL (P = 0.012), extrahepatic metastasis (P = 0.020), tumor size > 5 cm (P = 0.002), and BCLC stage C (P = 0.022) were identified as risk factors for HBVr.
The significant factors potentially influencing HBVr were incorporated into in the multivariate analysis. The results showed that, for both Definition A and Definition B, combination therapy (Definition A: HR 1.295, 95% CI 1.010–1.662, P = 0.042; Definition B: HR 1.426, 95% CI 1.058–1.923, P = 0.020), ALT > 40 (Definition A: HR 1.460, 95% CI 1.079–1.978, P = 0.014; Definition B: HR 1.516, 95% CI 1.060–2.168, P = 0.023), HBeAg (+) (Definition A: HR 1.570, 95% CI 1.133–2.174, P = 0.007; Definition B: HR 1.730, 95% CI 1.185–2.526, P = 0.005), and tumor size > 5 cm (Definition A: HR 1.394, 95% CI 1.051–1.848, P = 0.021; Definition B: HR 1.492, 95% CI 1.070–2.081, P = 0.018) were independent risk factors for HBVr.
Antiviral prophylaxis and HBV reactivation
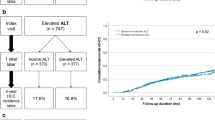
All patients in this study received antiviral therapy with oral nucleos(t)ide analogues (NAs). Entecavir (ETV) (n = 700, 79.8%) was the most commonly used drug, followed by tenofovir disoproxil fumarate (TDF) (n = 96, 10.9%) and tenofovir alafenamide (TAF) (n = 51, 5.8%). Seventy-six patients switched antiviral regimens after reactivation, and 36 patients had undetectable HBV DNA within 3–6 months of follow-up, but 6 patients experienced multiple HBVr. Additionally, 34 patients experienced tumor progression or death after reactivation, with no further follow-up. In our study, only 417 patients (47.5%) were undergoing long-term antiviral therapy prior to tumor diagnosis. In the six months prior to baseline, 243 patients (27.7%) were not consistently receiving antiviral therapy. We grouped patients based on adherence to antiviral therapy in the six months before baseline and found that those who were not consistently treated were more likely to experience reactivation (Fig. 3). This was significant under both Definition A (P = 0.013) and Definition B (P = 0.011).
HBV reactivation and prognosis
In our study, the risk of reactivation remained high, even in patients with undetectable HBV DNA. Among the 256 patients who experienced reactivation under Definition A, 181 (70.7%) had tumor progression, and under Definition B, 131 (72.3%) showed progression. The progression rate was slightly higher under Definition B, which sets a more stringent criterion for HBVr. To assess the effect of reactivation on survival and progression, we grouped patients based on reactivation status and plotted Kaplan-Meier survival curves, using the log-rank test for comparisons. The results (Fig. 4a, b, c and d) showed that under Definition A, the median overall survival (mOS) for the reactivation group was 23 months (95% CI 19–27), compared to 36 months (95% CI 32–45) for the non-reactivation group. Reactivation was linked to markedly poorer OS (P < 0.001) and PFS (P < 0.001). Similarly, under Definition B, the reactivation group had an mOS of 19 months (95% CI 16–25), while the non-reactivation group had an mOS of 36 months (95% CI 32–44). Both OS (P < 0.001) and PFS (P < 0.001) were notably reduced in the reactivation group relative to the non-reactivation group.
To explore whether different viral loads after HBVr affect survival and tumor progression, we divided the reactivated patients into two subgroups based on whether their viral load exceeded 100 IU/mL. We then compared OS and PFS between these groups. The results indicated that patients with viral loads greater than 100 IU/mL had significantly worse OS (P = 0.019) and PFS (P = 0.045) compared to those with lower viral loads (Fig. 5).
Discussion
We were the first to demonstrate HBVr in patients with undetectable HBV DNA. Compared to TKI monotherapy, the combination of TKI and PD-1 inhibitors resulted in a higher reactivation rate. Combination therapy with TKI and PD-1, ALT > 40, HBeAg(+), and tumor size > 5 cm were identified as independent risk factors for HBVr in HCC patients. Additionally, we found that patients undergoing prolonged and consistent antiviral therapy had a lower reactivation rate. Moreover, patients with HBVr experienced significantly lower OS and PFS compared to those without reactivation.
After standardizing baseline HBV DNA levels and increasing the sample size, we reconfirmed that combining TKI with PD-1 inhibitors results in an elevated HBVr rate relative to TKI monotherapy, aligning with the conclusions of our previous research. We further compared the most frequently used TKI regimen, lenvatinib, with the combination therapy of lenvatinib and the PD-1 inhibitor sintilimab, and similarly, the reactivation rate was greater in the combination therapy group relative to the TKI monotherapy group.
There have been prior reports suggesting that receiving TKI treatment may affect HBVr. Yao et al.10 found a clinically significant risk of HBVr (9.36%) in non-small cell lung cancer patients undergoing EGFR TKI treatment. In our study, even under the stricter B definition for reactivation, TKI monotherapy showed a high rate of HBVr (n = 74, 17.6%). The mechanism by which TKIs induce HBVr remains unclear. One hypothesis is that TKI targets key pathways involved in immune activation and cell proliferation, leading to lymphocyte dysfunction and HBVr. Meanwhile, whether ICIs trigger HBVr has been a major concern for clinicians. Despite ICIs enhancing immunity, HBVr can still occur during treatment. In a study by Ng et al.16, 6 out of 114 HCC patients (9.7%) receiving anti-PD-1/PD-L1 treatment experienced HBVr, with 2 (3.2%) developing active hepatitis. In our study, we found that patients undergoing combination therapy of PD-1 inhibitors and TKI were more likely to experience HBVr, suggesting that this regimen may more easily disrupt the immune balance.
We focus on the issue of HBVr in HCC patients not only because chronic HBV infection is prevalent in HCC, but also due to the potential relationship between the tumor environment and HBVr. Tumor-induced immune evasion may increase the risk of replication, dissemination, and proliferation of latent or chronic infectious pathogens. Anti-cancer therapies may disrupt the previous immune balance between the liver and HBV in those infected or carrying the virus, making HBVr more likely17. Chronic hepatitis B (CHB) patients typically exhibit impaired or absent virus-specific T-cell responses, with exhausted T cells showing impaired cytokine production and persistent expression of multiple inhibitory receptors, including PD-1 and CTLA-418. ICIs, by inhibiting the PD-1/PD-L1 axis or CTLA-4, may help reinvigorate the function of these exhausted T cells in CHB patients. In theory, ICIs should enhance the immune system’s ability to fight HBV, thereby inhibiting the virus19,20. However, in CHB patients, ICI treatment may disturb the immune homeostasis of chronic HBV infection, resulting in viral reactivation instead of suppression, creating a paradox that runs counter to the original therapeutic intent. The underlying mechanisms of this phenomenon require further investigation.
Given the paradoxical effects of ICI therapy on HBV patients, which may even increase the risk of HBVr, many guidelines recommend prophylactic antiviral treatment during ICI therapy. It is noteworthy that in this study, more than half of the patients initiated consistent antiviral therapy only after being diagnosed with cancer, as many HCC patients are first diagnosed with HBV infection when they seek treatment for symptoms caused by advanced tumors. A study by Mu-Gen et al.21 found that liver cancer patients who underwent antiviral therapy for over one year before surgery had better survival rates and lower recurrence rates. In our study, we found that HCC patients who underwent antiviral therapy for over six months prior to baseline treatment had a lower HBVr rate, indicating that prolonged antiviral therapy provides some protection for liver cancer patients. Similarly, a large-scale study by Yoo et al.22 on cancer patients receiving ICI treatment found that the HBVr rate was 0.5% for HCC patients and 2.9% for non-HCC patients, while the HBVr rate for those who received prophylactic antiviral treatment was 0.4%, compared to 6.4% for those who did not. This significant difference highlights the importance of prophylactic antiviral therapy. Given the shortened life expectancy of cancer patients and the potential for HBVr, antiviral prophylaxis allows patients to concentrate on cancer therapy, minimizing interruptions caused by HBVr.
We identified four cases of HBVr with HBV DNA levels exceeding 4 log10 IU/mL, in which spontaneous viral decline occurred without adjustment of antiviral therapy. ALT levels remained normal, but three of these patients experienced tumor progression. We speculate that the spontaneous decline in viral load may be associated with tumor control. As tumor burden decreases, the PD-1/PD-L1 axis may be relieved, allowing restoration of HBV-specific CD8+ T cell function23. Additionally, the tumor microenvironment (TME), which is rich in Tregs that suppress antiviral T cell responses, may become less immunosuppressive as Tregs decline, leading to enhanced T cell activity and HBV suppression24. Furthermore, during tumor progression, immunosuppressive M2 macrophages increase, whereas tumor control may favor proinflammatory M1 macrophage polarization, which promotes HBV antigen presentation and T cell activation via cytokines such as IL-12 and TNF-α, thereby inhibiting HBV replication25. These findings suggest that tumor progression can influence HBV DNA dynamics, while tumor control may help restore immune homeostasis and suppress viral replication.
In this study, all included patients were undergoing antiviral therapy and had undetectable baseline HBV DNA. The 2023 AASLD guidelines26 recommend concurrent antiviral therapy during anticancer treatment for HCC patients. One of the study’s focuses was whether consistent antiviral treatment had been initiated within six months prior to baseline. Interestingly, we found that patients who began antiviral therapy six months before baseline experienced a markedly reduced HBVr rate relative to patients who had not. This is a surprising result, as we expected that patients without prior preventive antiviral therapy but with undetectable HBV DNA would be in a well-controlled state. We hypothesized that concurrent antiviral therapy during systemic treatment would not lead to a higher reactivation rate than in those who started preventive antiviral therapy earlier. However, the results contradicted our expectations. We speculate that early preventive antiviral therapy may act as a protective factor, and regardless of antiviral treatment status, systemic therapy can influence HBVr.
We were unable to isolate a group of patients without antiviral therapy for comparison, as the number of such cases was too small to be clinically meaningful and did not align with current guidelines, which recommend the use of NAs to prevent HBVr27. Regarding whether to immediately adjust antiviral therapy after HBVr, in this study, most patients managed to reduce HBV DNA to a controlled or undetectable level following consistent and standard antiviral treatment. A prospective study by Zhong et al.28 found that patients with low viral loads who switched antivirals medications achieved better viral clearance compared to those who continued entecavir. However, due to the limited sample size in this study, we could not confirm whether switching medications after reactivation leads to improved outcomes in terms of tumor progression or survival. Larger studies may be needed to validate this observation.
The 2018 AASLD guidelines on HBVr provide a widely used definition; however, given the time since their release, they do not differentiate between specific patient populations (e.g., the 2021 APASL guidelines provide separate recommendations for patients receiving immunotherapy). In our previous study29, we applied three HBVr definitions to HCC patients undergoing systemic therapy. The findings indicated that, under the AASLD 2018 definition, many patients experienced tumor progression without meeting the criteria for HBVr. Similarly, in this study, the definition of HBVr as detectable HBV DNA (Definition A: 256 cases [29.1%]) identified more reactivation cases compared to the 2018 AASLD definition (46 cases [5.2%]). While stricter criteria result in higher reactivation rates, we consider this approach reasonable for advanced HCC patients, as it aids in exploring the relationship between viral reactivation and tumor progression. The 2021 APASL guidelines suggest that, after initiating immunotherapy, HBVr is defined as detecting HBV DNA levels > 100 IU/mL in patients whose HBV DNA was undetectable at baseline, or as a conversion from undetectable to detectable HBV DNA in HBsAg-negative patients. Our study applied even stricter criteria (Definition A: from undetectable HBV DNA to detectable; Definition B: an increase to > 100 IU/mL from baseline), and we observed differences in survival and tumor progression between patients based on these criteria (Fig. 5). We found that patients with high HBV DNA viral loads after reactivation had shorter survival and higher risks of disease progression. We believe that using a more sensitive definition is more effective for monitoring and guiding treatment.
HBVr affects patient prognosis, as confirmed in this study. The association between HBVr and tumor progression remains unclear, as both can influence the immune environment. The increase in regulatory T cells not only suppresses HBV antigen-specific immune responses but also inhibits immune responses targeting liver cancer antigens30. The relationship between the two is more likely mutually reinforcing, making it challenging to establish a clear cause-and-effect relationship, which requires further experimental validation.
Our study has several limitations. First, to confirm that all participants were HBV patients, we included only those with undetectable HBV DNA and positive HBsAg. While this ensured uniformity in the study population, it may have introduced selection bias, potentially overlooking patients who are HBsAg-negative but HBcAb-positive. Second, although we employed two definitions for HBVr and believe a more sensitive definition is applicable for HCC patients receiving immunotherapy, we did not establish a simple and generalizable definition. Additionally, we did not propose specific antiviral strategies for patients experiencing HBVr or tumor progression, which warrants further investigation. Finally, we did not include patients receiving only PD-1 inhibitors or those with other types of cancer, as such cases are rare at our center, limiting the generalizability of our findings.
In conclusion, we have validated, for the first time, the occurrence of HBVr and its prognostic impact in HCC patients with undetectable HBV DNA. Our findings highlight that even with inactive HBV DNA, these patients still require vigilant monitoring of HBV DNA levels and tumor progression.
Data availability
All our authors promise that the data mentioned in the article are available without any conflict of interest. Correspondence and requests for materials should be addressed to Yinying Lu. This retrospective study was approved by the ethics committees of two medical centers, with informed consent waived. All procedures complied with relevant regulations. The approving ethics committees were the Ethics Committee of the Fifth Medical Center of Chinese PLA General Hospital (KY-2024-9-149-1) and the Ethics Committee of the Affiliated Hospital of Guizhou Medical University (2023-NO.934). The study has been registered in the Chinese Clinical Trial Registry (ChiCTR2500101601).
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for Clinicians. ;71:209–49. (2021).
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, European association for the study of the liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J. Hepatol. 69, 182–236 (2018).
Voican, C. S. et al. Hepatitis B virus reactivation in patients with solid tumors receiving systemic anticancer treatment. Ann. Oncol. 27, 2172–2183 (2016).
Liu, C., Shih, Y-F. & Liu, C-J. Immunopathogenesis of acute flare of chronic hepatitis B: with emphasis on the role of cytokines and chemokines. Int. J. Mol. Sci. 23, 1407 (2022).
Kudo, M. et al. Lenvatinib versus Sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391, 1163–1173 (2018).
Llovet, J. M. et al. Sorafenib Adv. Hepatocellular Carcinoma N Engl. J. Med. 359, 378–390 (2008).
Kikuchi, H. et al. Increased CD8 + T-cell infiltration and efficacy for multikinase inhibitors after PD-1 Blockade in hepatocellular carcinoma. J. Natl. Cancer Inst. 114, 1301–1305 (2022).
Knolle, P. A. & Thimme, R. Hepatic immune regulation and its involvement in viral hepatitis infection. Gastroenterology 146, 1193–1207 (2014).
Franceschini, D. et al. PD-L1 negatively regulates CD4 + CD25 + Foxp3 + Tregs by limiting STAT-5 phosphorylation in patients chronically infected with HCV. J. Clin. Invest. 119, 551–564 (2009).
Yao, Z-H. et al. Incidence of hepatitis B reactivation during epidermal growth factor receptor tyrosine kinase inhibitor treatment in non-small-cell lung cancer patients. Eur. J. Cancer. 117, 107–115 (2019).
Ando, T. et al. Reactivation of resolved infection with the hepatitis B virus immune escape mutant G145R during dasatinib treatment for chronic myeloid leukemia. Int. J. Hematol. 102, 379–382 (2015).
Chang, C-S., Tsai, C-Y. & Yan, S-L. Hepatitis B reactivation in patients receiving targeted therapies. Hematology 22, 592–598 (2017).
Zhang, X. et al. Hepatitis B virus reactivation in cancer patients with positive hepatitis B surface antigen undergoing PD-1 Inhibition. J. Immunother Cancer. 7, 322 (2019).
Terrault, N. A. et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 67, 1560–1599 (2018).
Lau, G. et al. APASL clinical practice guideline on hepatitis B reactivation related to the use of immunosuppressive therapy. Hepatol. Int. 15, 1031–1048 (2021).
Ng, K. Y. Y. et al. Real-world efficacy and safety of immune checkpoint inhibitors in advanced hepatocellular carcinoma: experience of a tertiary Asian center. Asia Pac. J. Clin. Oncol. 17, e249–e261 (2021).
Hwang, J. P., Barbo, A. G. & Perrillo, R. P. Hepatitis B reactivation during cancer chemotherapy: an international survey of the membership of the American association for the study of liver diseases. J. Viral Hepat. 22, 346–352 (2015).
Ye, B. et al. T-cell exhaustion in chronic hepatitis B infection: current knowledge and clinical significance. Cell. Death Dis. 6, e1694 (2015).
Fisicaro, P. et al. Combined Blockade of programmed death-1 and activation of CD137 increase responses of human liver T cells against HBV, but not HCV. Gastroenterology 143, 1576–1585e4 (2012).
Rao, M., Valentini, D., Dodoo, E., Zumla, A. & Maeurer, M. Anti-PD-1/PD-L1 therapy for infectious diseases: learning from the cancer paradigm. Int. J. Infect. Dis. 56, 221–228 (2017).
Dai, M-G. et al. Preoperative antiviral therapy and Long-Term outcomes for hepatitis B Virus-Related hepatocellular carcinoma after curative liver resection: A multicenter analysis. J. Hepatocell Carcinoma. 11, 927–939 (2024).
Yoo, S. et al. Risk of hepatitis B virus reactivation in patients treated with immunotherapy for Anti-cancer treatment. Clin. Gastroenterol. Hepatol. 20, 898–907 (2022).
Tzeng, H-T. et al. (ed Bertoletti, A.) PD-1 blockage reverses immune dysfunction and hepatitis B viral persistence in a mouse animal model. PLoS ONE 7 e39179 (2012).
Liu, L. et al. Single-cell analysis reveals HBV-specific PD-1 + CD8 + TRM cells in tumor borders are associated with HBV-related hepatic damage and fibrosis in HCC patients. J Exp Clin Cancer Res [Internet]. [cited 2025 Jul 7];42. Available from: https://jeccr.biomedcentral.com/articles/ (2023). https://doi.org/10.1186/s13046-023-02710-4
Li, B. et al. Anti–PD-1/PD-L1 Blockade Immunotherapy Employed in Treating Hepatitis B Virus Infection–Related Advanced Hepatocellular Carcinoma: A Literature Review. Front Immunol [Internet]. 2020 [cited 2025 Jul 7];11. Available from: https://www.frontiersin.org/article/https://doi.org/10.3389/fimmu.2020.01037/full
Singal, A. G. et al. AASLD practice guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology 78, 1922–1965 (2023).
Drafting Committee for Hepatitis Management Guidelines, the Japan Society of Hepatology. Japan society of hepatology guidelines for the management of hepatitis C virus infection: 2019 update. Hepatol. Res. 50, 791–816 (2020).
Li, Z. et al. Switching from Entecavir to Tenofovir Alafenamide for chronic hepatitis B patients with low-level viraemia. Liver Int. 41, 1254–1264 (2021).
Lei, J. et al. Comparison of hepatitis B virus reactivation in hepatocellular carcinoma patients who received tyrosine kinase inhibitor alone or together with programmed cell death protein-1 inhibitors. Hepatol. Int. 17, 281–290 (2023).
Zhang, H. H. et al. Regulatory T cells in chronic hepatitis B patients affect the Immunopathogenesis of hepatocellular carcinoma by suppressing the anti-tumour immune responses. J. Viral Hepat. 17 (Suppl 1), 34–43 (2010).
Funding
This study was supported by the National Natural Science Foundation of China (NO. 82272956).
Author information
Authors and Affiliations
Contributions
Z. L, J. L, H. L contributed to the study conception and design, statistical analysis, and drafting of the initial manuscript. H. D, Y. Z, F. W, W. M, H. Y, X. C, and Q. K contributed to data collection and analysis. J. Z and Y. L provided supervision for the study and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics declarations
This study has been approved by the Ethics Committee of the Fifth Medical Center of the PLA General Hospital (KY-2024-9-149-1) and the Ethics Committee of the Affiliated Hospital of Guizhou Medical University (2023-NO.934).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, Z., Lei, J., Li, H. et al. HBV reactivation and prognosis after systemic therapy in HCC with undetectable HBV DNA: a multicenter retrospective study. Sci Rep 15, 30204 (2025). https://doi.org/10.1038/s41598-025-13406-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-13406-4