Abstract
Electrochemotherapy (ECT) presents an effective alternative for local tumor management, particularly valuable when surgery is not feasible. The side effects are generally mild, including local inflammation, edema, and changes in pigmentation or alopecia. However, severe side effects such as necrosis, dehiscence, or fistula formation may occur if the tumor involves the full tissue thickness. This study aims to evaluate the efficacy of gabapentin in managing pain in cats with facial squamous cell carcinoma (SCC) staged T2–T4 (N0M0) treated with ECT. A subjective survey outlining typical quality of life measures was given to owners and compared to the veterinarian’s assessment of reaction to palpation of the tumor affected area. Pain assessment was conducted based on a questionnaire provided to the owner and during clinical examination at several time points: before the first ECT treatment (D0), seven days after (D1), at 14 days after and just prior to the administration of the second session (D2) and finally, 28 days after the first session (14 days after second ECT session) (D3). Cats were randomly divided in two groups: a control group (CG) composed of cats that received only NSAID’s for analgesic protocol in the post-ECT for acute pain management, and gabapentin group (GG) composed of cats that, in addition to NSAID’s, received gabapentin for long-term pain management. Statistical analyses showed that patients treated with gabapentin had better quality of life (QoL) and pain assessment scores than those in the control group at various observation times. In cats with advanced stages of facial SCC, the disease is associated with pain, which may be exacerbated by ECT, requiring close monitoring both immediately after treatment and in the long term. Furthermore, ECT is an effective treatment for cats with facial SCC.
Similar content being viewed by others
Introduction
Feline facial squamous cell carcinoma (SCC) is a malignant tumor arising from epidermal cells that differentiate into keratinocytes. It accounts for approximately 10.4% of feline skin tumors, especially in older cats, with white-haired cats having a 13.4-fold higher risk than those with other coat colors1,2,3,4. Chronic exposure to ultraviolet (UV) light is considered the primary cause of feline facial SCC, with lesions typically occurring in the nasal planum (80–90%), pinnae (50%), eyelids (20%) and lips1. Clinically, feline facial SCC appears as ulcerated, erythematous, and crusted lesions, rarely metastasizing but often progressing into painful ulcers5,6. When metastasis occurs, it generally affects the draining lymph nodes and lungs; staging should include lymph node cytology and chest radiographs, following the World Health Organization TNM system (Tumor, Nodes, Metastasis-TNM)7,8.
The success of SCC treatment in cats depends on clinical stage, invasiveness, and lesion location, with early intervention improving outcomes1,4. Surgical excision is the standard approach, offering the longest disease-free intervals6. Advanced SCC (T2–T4) may require a highly aggressive surgical approach to achieve clear surgical margins, which can result in significant aesthetic impact and loss of function, often not accepted by the owner7. Less invasive treatments, like cryosurgery and photodynamic therapy, are also used, while chemotherapy has limited efficacy9.
Electrochemotherapy (ECT) presents an effective alternative for local tumor management, particularly valuable when surgery is not feasible. Over the past years, ECT has become a valuable supplementary treatment for solid tumors, including feline SCC, due to high response rates, ease of use, low side effects, and affordability10. For facial SCC in cats, response rates can reach up to 77%, with some protocols achieving complete responses in 87.5% of cases1,11. The side effects are generally mild, including local inflammation, edema, and changes in pigmentation or alopecia12,13. However, severe side effects such as necrosis, dehiscence, or fistula formation may occur if the tumor involves the full tissue thickness12. In advanced stage SCC of the nasal planum in cats, scar tissue can develop, potentially leading to complications like anosmia10.
Gabapentin is an anticonvulsant drug with well-established clinical efficacy in human patients for managing refractory partial seizures, secondarily generalized tonic-clonic seizures, and chronic neuropathic pain. In veterinary medicine, it is used off-label in combination with other treatments to control seizures, manage neuropathic pain, and alleviate anxiety14. Gabapentin is a lipophilic structural analogue of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). While its exact mechanism of action is not fully understood, it is known to interact with voltage-gated calcium channels by binding to the alpha-2-delta subunit15,16. Various studies in feline patients have demonstrated gabapentin’s efficacy in managing hyperalgesia and allodynia17 neuropathic pain18,19, acute perioperative pain20, and anxiety control21,22,23.
Based on the available veterinary literature, ECT is considered a safe therapeutic treatment, typically associated with mild side effects, with pain rarely mentioned. While references are made to pain experienced during the treatment and in the immediate post-treatment period, there is no significant mention of long-term pain12,24.
We hypothesized that in cats with facial SCC at stages T2, T3, and T4, due to the extent of the lesion and, at times, the involvement of bone and cartilage tissue especially in T4 stage, the painful component was already present in the pre-treatment phase, and that the administration of ECT exacerbated this pain condition. We also hypothesized that chronic pain develops following ECT, necessitating analgesic therapy.
For these reasons, in our study we evaluated the efficacy of gabapentin for managing pain in cats with facial SCC T2–T4 (N0M0) following ECT. Also, we evaluated the impact of gabapentin administration on the quality of life (QoL) in the enrolled cats and investigated whether statistically significant differences in QoL existed between gabapentin-treated and untreated patients, along with an assessment of any associated side effects and those related to ECT administration. Lastly, a comparison was made between the owners’ pain assessments and the veterinarians’ findings to determine any correlations. Additionally, we investigated whether there was a relationship between tumor stage and response to treatment.
Materials and methods
Patients
In this randomized prospective study, 42 owned cats with diagnosis of facial SCC at stages T2–T3-T4 N0M0 according to the WHO System for SCC staging in cat8 (Table 1), treated with ECT, were included. The cats were referred to the Cancer Unit of the Department of Veterinary Medicine-University of Bari between January 2022 and October 2024. The study was approved by the “Ethics Committee for Animal Experimentation” (CESA-DIMEV “Animal Welfare Body”) with protocol n. 38/24 and methods involving animals were performed in accordance with the relevant guidelines and regulations (ARRIVE guidelines).
The inclusion criteria required a confirmed cytological/histological diagnosis of SCC, lymph node cytology, chest X-ray or CT scan, evaluation of the hematobiochemical profile and serological evaluation of infectious diseases such as FIV/FeLV tests. Patients with comorbidities, lymph node involvement, those who discontinued gabapentin therapy for management reasons, those requiring more than two sessions of ECT in order to achieve disease control, and those who underwent additional treatments (e.g. surgery) besides ECT were excluded from the study.
The enrolled patients were randomized into two groups using Microsoft Excel: the control group (CG) composed of cats that received only NSAID’s for analgesic protocol in the post-ECT for acute pain management, and gabapentin group (GG) composed of cats that, in addition to NSAID’s, received gabapentin for long-term pain management.
Electrochemotherapy treatment procedures
The ECT treatment was performed with Onkodisruptor® (Biopulse, Rome, Italy), an electric pulse generator, under general anesthesia. The anesthetic protocol included premedication with dexmedetomidine 10 µg/kg (Cepedex®; p.h. farmaceutici) and ketamine 2 mg/kg (Ketabel®; p.h. farmaceutici) administered intramuscularly; induction with fentanyl 2 µg/kg (Fentadon®; Dechra) and propofol 2–4 mg/kg (PROPOMITOR®; Ecuphar) administered intravenously, followed by patient intubation. Anesthesia maintenance was achieved through the administration of isoflurane (IsoFlo®, Zoetis, Italy).
The treatment area was shaved, and any scabs and necrotic tissue were removed. Then, it was cleaned with sterile gauze soaked in saline solution.
The ECT protocol included the administration of bleomycin (Bleoprim 15,000 UI®; Sanofi, Italy) at a dose of 15 mg/m2 as a bolus via intravenous injection. Eight minutes after the administration of bleomycin, biphasic pulses were applied to the tumor area at a voltage of 1100 V/cm, a frequency of 1 Hz, and a duration of 100 µs, using plate and needle electrodes in all cats (Onkodisruptor®). The protocol involved two sessions conducted 14 days apart.
Post-ECT treatment
In the 3 days following the ECT treatment, all patients from CG received analgesic therapy with oral meloxicam 0.05 mg/kg/day (Metacam®; Boehringer Ingelheim). Additionally, the cats included in GG received gabapentin 10 mg/kg twice daily (Gabapentin®; DOC generic Srl, Italy) for 28 days following ECT treatment. If the cats showed a lack of appetite reported by the owner, it was necessary to introduce an orexigenic therapy based on mirtazapine (Mirataz® Dechra).
QoL and pain assessment
Owners were provided with a questionnaire to assess the QoL and their evaluation of the cat’s pain (variable “pain owner”) assigning a score between 1 and 5 to each variable. During the clinical examination, pain assessment was conducted by the veterinarian (variable “pain vet”) through palpation of the affected area, with responses scored on a scale from 1 to 5 (Table 2).
The assessments were conducted at the following timepoints: before the first ECT treatment (D0), seven days after (D1),14 days after and just prior to the administration of the second session (D2) and finally, 28 days after the first session (14 days after second ECT session) (D3).
ECT toxicity
Adverse events of ECT were assessed according to the VCOG-Common Terminology Criteria for Adverse Events (VCOG-CTCAE, version 2). Pruritus, alopecia, erythema, skin ulcerations, and tissue necrosis were assessed25. Mild adverse events were classified as grade ≤ 2, while severe adverse events were classified as grade > 2. The assessment of adverse effects was conducted at 7 days after the first ECT treatment (D1) and 14 days after the second ECT session (D3) through clinical evaluation.
Gabapentin toxicity
The assessment of adverse events secondary to gabapentin administration was collected during clinical follow-ups based on the owners’ reports.
Figure 1 summarizes the time points for data collection from the owner’s questionnaire, the veterinarian pain assessment and the evaluation of adverse events related to ECT.
Statistical analysis
All the data set were tested for normal distribution and variance homogeneity using Shapiro–Wilk’s test. Then, they were subjected to analysis of variance (ANOVA), using the General Linear Model (GLM) software by SAS (2018) (version 9.3, SAS Institute Inc., Cary, NC, USA).
All scores data were subjected to ANOVA according to the following model: yijk = µ + αi + Gj + Tk + (G × T) jk + εijkl, where yijk represents all parameters as dependent variables; µ is the mean; αi is the random aninal effect, G represents the effect of the jth group (j = 1, 2), T represents the effect of the kth treatment time (k = 1, …, 4), G × T represents the effect of the binary interaction between the two independent variables (jk = 1,…, 8) and εijkl is the error. Subsequently, a Tukey test for repeated measures was carried out to evaluate the differences among the means during the time. The data were analyzed using Spearman’s correlation coefficient to assess the strength and direction of the linear relationship between the variables. The pain score dataset of both owner and vet, for each time point, were subjected to ANOVA according to the following model: yijk = µ + αi + Sj + Ek + (S × E) jk + εijkl, where yijk represents all parameters as dependent variables; µ is the mean; αi is the random aninal effect, S represents the effect of the jth stage (j = 1, …, 3), E represents the effect of the kth evaluator (k = 1, 2), S × E represents the effect of the binary interaction between the two independent variables (jk = 1,…, 6) and εijkl is the error. All means were expressed as square means and mean standard error. The significance level was set to P < 0.05.
Descriptive analysis was applied to evaluate the side effects related to gabapentin administration and adverse events from ECT.
Results
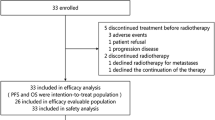
Out of 42 animals enrolled, 12 patients were excluded from the study for several reasons: five cats due to discontinuous administration of gabapentin by the owner (n = 5), four cats due to concurrent diagnosis of FIV or FeLV or other comorbidities (hyperthyroidism, Chronic Kidney Disease, cardiomyopathy or other metabolic, infectious disorders) or lymph node involvement (n = 4), three cats who required a third electrochemotherapy session for tumor control or that underwent surgery or other treatments (n = 3).A total of 30 owned cats met the inclusion criteria and were enrolled in the study. All 30 cats were domestic shorthair with diagnosis of squamous cell carcinoma, of which 8 cases were diagnosed through biopsy and 22 cases through cytology. There were 17 females and 13 males, all neutered. Ages ranged from 8 to 17 years (mean ± SD: 11.9 ± 2.86). Only three cats underwent head, neck and chest CT scan; the remaining cats were staged using chest x ray (DV, LL left and right).
Of the 30 cats recruited who met the inclusion criteria, 10 belonged to the CG and 20 to the GG. Tumor locations in the CG were distributed as follows: nasal planum (n = 5), temporal region (n = 1), periocular region (n = 1), nasal planum and upper lip (n = 1), nasal planum and infraorbital region (n = 1), and upper lip and cheek region (n = 1). Six were T2N0M0 (n = 6), two T3N0M0 (n = 2), and two T4N0M0 (n = 2). In the GG, tumor locations included nasal planum (n = 8), temporal region (n = 1), periocular region (n = 2), nasal planum and upper lip (n = 3), nasal planum and infraorbital region (n = 2), and upper lip and cheek region (n = 4). Six were T2N0M0 (n = 6), nine were T3N0M0 (n = 10), and four were T4N0M0 (n = 4).
QoL and pain assessment
The results obtained from the questionnaire administered to the owner and the veterinarian’s evaluation at D0 (day 1), D1 (day 7), D2 (day 14), and D3 (day 28) in the two groups were statistically analyzed. In both cases, the assessment was always carried out by the same person. The comparison between the CG and the GG over the course of 28 days is reported in Table 3.
The scores for happiness, mobility, appetite, hygiene, and general health showed significant differences between the two groups (P < 0.0001) and underwent significant changes over time, independent of group assignment (P < 0.0001). Additionally, their temporal trends differed significantly between the groups (p < 0.05). The owner pain score exhibited significant changes within groups regardless of time (P < 0.0001). The veterinarian pain score demonstrated significant differences between the groups (P < 0.0001) and underwent significant temporal changes irrespective of group assignment (P < 0.0001).
In the GG, the scores for happiness, appetite, hygiene, general health and owner pain showed an increasing trend starting from D2 (P < 0.01); the mobility score decreased at D1 (P < 0.01), followed by an increase at D3 (P < 0.01), and the vet pain score exhibited a decreasing trend at D1 (P < 0.01), followed by an increase starting from D2 (P < 0.01).
In the CG, the scores for happiness, mobility, and owner pain did not show significant changes over time (P > 0.05). The appetite score showed a decrease from D0 to D2 (P < 0.01), the hygiene score decreased at D1 (P < 0.01), the general health score showed a reduction at D2 (P < 0.01), and finally, the vet pain score increased at D3 (P < 0.01).
At D1, appetite and hygiene scores were significantly higher in the GG compared to the CG (P < 0.01). At D2, happiness, appetite, hygiene, general health, and vet pain scores were significantly higher in the GG compared to the CG (P < 0.01). At D3 happiness, mobility, appetite, hygiene, general health, and vet pain scores were all significantly higher in the GG compared to the CG (P < 0.01).
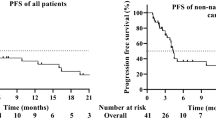
The results of Spearman’s correlation showed significant associations between all parameters (P < 0.0001), with coefficients ranging from 0.47 (owner pain and hygiene) to 0.84 (mobility and general health). Data were summarized in Fig. 2.
Effects of stage and evaluators (veterinarian and owner) on pain score in CG and GG are reported in Fig. 3.
Effects of stage and evaluators (veterinarian and owner) on pain score in CG and GG. CG = control group, GG = gabapentin group, T2 = T2N0M0 T3 = T3N0M0 T4 = T4N0M0, World Health Organization (WHO) TNM (tumor, node, metastasis) classification system for feline epidermal origin tumors. Different letters of the same color show statistical differences among stages within the same day of the same scorer: A, B = P < 0.01; a, b = P < 0.05. Statistical differences between scorers at the same stage in the same day are shown: * = P < 0.05.
At D0, pain scores in CG patients showed significant differences based on stage (P < 0.0001) and evaluator (P < 0.05), while the correlation between stage and evaluator was not statistically significant (P > 0.05). For T3 and T4, for both evaluators, pain scores were lower compared to T2 (P < 0.01).
At D1, stage had a significant effect on pain scores (P < 0.0001), with lower scores at T4 compared to T2 for the owner’s assessment only (P < 0.05). At D2, pain scores were significantly affected only by stage (P < 0.01), while at D3, significant differences were observed based on both stage and evaluator (P < 0.05), without a significant interaction (P > 0.05).
In GG animals, only stage significantly affected the score at D1 (P < 0.0001), D2 (P < 0.01), and D3 (P < 0.05). At D1 owner score for T2 was higher than T3 (P < 0.05) and T4 (P < 0.01), vet score for T2 was higher than T3 and T4 (P < 0.01).
After D2 and D3, owner scores at T4 showed lower values than T2 (P < 0.05). Moreover, at D3 of treatment at T3 the vet score was higher than the owner one (P < 0.05).
ECT toxicity
None of the patients showed adverse effects related to the administration of bleomycin according to the VCOG criteria25.
Regarding ECT-related toxicity, at D1 in GG, alopecia grade I was observed in 3.3% (n = 1), erythema grade I in 56.7% (n = 17), pruritus grade I in 13.3% (n = 4) and grade II in 6.7% (n = 2), skin ulceration grade I in 6.7% (n = 2) and grade II in 3.3% (n = 1). No tissue necrosis was reported.
At D3, alopecia grade I was seen in 3.3% (n = 1), erythema grade I in 30% (n = 9), and pruritus grade I in 10% (n = 3). No skin ulceration or tissue necrosis occurred.
In CG at D1, alopecia grade I was found in 10% (n = 1), erythema grade I in 80% (n = 8), skin ulceration grade II in 20% (n = 2), and pruritus grade I in 10% (n = 1) and grade II in 20% (n = 2). No tissue necrosis was noted. At D3, alopecia grade I was observed in 10% (n = 1), erythema grade I in 50% (n = 5) and pruritus grade I in 10% (n = 1) and grade II in 20% (n = 2). No skin ulceration or tissue necrosis occurred. Data were summarized in Fig. 4.
Gabapentin toxicity
In 3 out of the 20 cats in the GG, owners reported mild sedation in the hours following administration.
Other therapy
Mirtazapine was administered due to observed lack of appetite in 4 cats with T4 stage, 2 cats of the CG and 2 cats of the GC.
Discussion
This study suggests that gabapentin is effective in managing pain in cats with advanced stage (T2–T4) facial SCC treated with ECT. To evaluate the relationship between disease progression and pain, as well as the potential role of ECT in intensifying it, only cats with advanced-stage disease who received ECT as their only treatment were included.
From the veterinary literature, we know that ECT is an effective procedure with limited side effects10. To the best of our knowledge, no studies have explored the potential for chronic pain associated with this treatment. While references are made to pain experienced during the treatment and in the immediate post-treatment period, there is no significant mention of long-term pain12,24. In human medicine, ECT has become an increasingly popular treatment for cutaneous metastases, offering pain relief in cases of skin metastases26. However, it has also been associated with post-treatment pain, including severe or neuropathic pain in some patients, such as those with breast cancer27.
Similarly, clinical experience and reports from owners of cats undergoing ECT, particularly for advanced stage facial SCC, indicate discomfort and clinical signs associated with pain. This pain, which can primarily be attributed to the local invasiveness of the disease, may also be exacerbated by the ECT treatment itself.
In our study, to objectively assess pain, we created a scale that could be statistically compared with the pain evaluations provided by the owners. We believe that comparing our assessment with the owners’ is essential as they know their pets well and can recognize often subtle and subjective signs of pain. Furthermore, since tumor stage may affect pain score, we also considered this variable, to allow a more thorough evaluation of its potential impact.
Based on our results, the evaluations by cat owners did not always align with the veterinarians’ assessments. Therefore, we cannot draw a definitive conclusion on which evaluator is more likely to underestimate or overestimate pain. A factor that may have contributed to these differences in evaluations is that, although data from both assessments were collected at the same time points, the owner’s evaluation was based on a longer observation period (up to two weeks between D2 and D3) in a familiar environment, allowing the cat to express its behavior more naturally. In contrast, the veterinarian’s assessment was limited to the time of the visit, and it is well established that cats are typically stressed or uncomfortable in a veterinary setting.
However, at D0, both veterinarians and owners consistently attributed higher pain scores to advanced stages of the disease (T3–T4). This finding was expected, as it aligns with the WHO classification, which links advanced disease stages with the progressive involvement of surrounding structures, including muscles, cartilage, and bones in T4, ultimately leading to increased pain2.
Furthermore, higher pain scores in stages T3 and T4 were observed at later timepoints in both groups. Although no direct statistical comparison was made between the two groups concerning disease stage, our data suggest that, while gabapentin is effective in pain management, in patients with advanced stage disease, prolonged analgesic therapy beyond 28 days may be necessary to achieve adequate pain relief.
Pain assessment showed significant differences between the groups with noticeable temporal variations.
In GG, pain score initially decreased ad D1, but increased from D2 onward, a trend observed by both veterinarians and owners. Additionally, the higher pain level recorded by the veterinarian at D1 suggests that gabapentin may not have fully reached its analgesic effect, which is consistent with the seven days treatment duration. This finding aligns with prior studies that highlight gabapentin’s limited efficacy in managing acute pain14.
In CG, the owners’ evaluations showed no significant changes over time. In contrast, the veterinarian observed a significant reduction in pain only at D3, suggesting a delayed improvement compared to the treated group.
A key consideration is that all cats received NSAIDs for three days following each ECT session. This finding is particularly relevant, as it suggests that NSAIDs administration alone was insufficient to provide adequate pain control in the control group, whereas the addition of gabapentin contributed to improved pain management in the treated group.
When comparing the two groups, owners did not report statistically significant differences in pain levels, but their assessment showed a trend toward higher scores in GG, suggesting a perceived benefit of gabapentin. In contrast, from D2 onward, veterinarians consistently recorded lower pain levels in the GG compared to the CG, highlighting a significant effect of the analgesic treatment.
These findings confirm that ECT induces pain, as shown by the temporal changes in pain scores and the differences observed between groups. However, gabapentin effectively managed this pain, with a stronger effect noted in the veterinarian’s assessment. These results underscore the importance of a multimodal pain management approach for patients receiving ECT. Given the complex nature of pain associated with both the disease and the treatment, it is crucial to integrate various therapeutic strategies. Moreover, the results support the efficacy of gabapentin in providing additional analgesia, showing its potential to improve patient well-being beyond NSAIDs alone.
Quality of life (QoL) parameters, including happiness, appetite, hygiene, and general health, showed significant improvement over time in the GG, with substantial increases starting at D2. In contrast, the CG exhibited a decline in QoL at D1 and D2. Cats of GG showed increased appetite, likely due to the appetite-stimulating effects of gabapentin, which have been documented in both human and veterinary medicine28,29. The improved appetite could also be related to pain relief, which may have facilitated increased food intake, as seen in other parameters.
However, two cats with T4 stage disease in both groups experienced a reduction in appetite, which requiring the addition of mirtazapine to stimulate food intake30. This was likely due to severe tissue loss in the nasal planum region, which led to anosmia, skin irritation, and crusting, all of which contributed to a decreased appetite.
Spearman’s correlation results reveal strong associations among various health parameters, indicating that changes in one aspect of a cat’s health related to the others. These findings underscore the necessity of a holistic approach when evaluating and managing pain.
Veterinary literature has consistently reported that ECT is well tolerated, with no significant side effects13. However, recent studies suggest that in cases of advanced-stage SCC (T3–T4), severe side effects occur in 62% of cats31. In our study, while the primary focus was on pain evaluation, we also assessed other side effects in both groups, including pruritus, alopecia, erythema, skin ulcerations, and tissue necrosis. Overall, these side effects were generally mild and transient, with most resolving without lasting consequences. A distinct response pattern emerged between the two groups. In the GG the lower frequency and resolution of erythema and pruritus suggest good long-term tolerability further indicating that gabapentin may have played a role in a more favorable side effect profile. Although the CC group experienced a higher incidence of erythema, pruritus, and skin ulcerations, these effects did not result in irreversible damage. Furthermore, tissue necrosis was not observed in either group. These findings align with those of previous studies, reinforcing the overall safety and low toxicity of ECT5,10,11,13.
Gabapentin was generally well tolerated, according to the owners. However, in three treated cats, owners reported noticeable weakness following the morning doses of gabapentin, along with a reduction in the cats’ usual nighttime activity. These observations align with the known sedative properties of gabapentin32. However, these effects could not be statistically quantified, as most owners administered gabapentin in the morning before leaving for work and in the evening, which may have led to an underreporting of its sedative effects.
Although the sedative effect was not quantitatively assessed, it seemed to be mild, as it was not frequently reported by the owners. This mild sedation likely contributed to a more favorable response to stimulation during the pain assessment by the veterinarian, as more relaxed cats may experience less discomfort or stress. Furthermore, gabapentin’s sedative properties may have played a role in alleviating certain side effects of ECT, such as pruritus. In summary, while the sedative effect was subtle, it may have had a beneficial impact on both pain management and the resolution of side effects.
Although it was not the primary focus of our study, in agreement with the literature, our results also demonstrated that ECT is an effective therapeutic approach for achieving local control of facial SCC in cats1,11,31,33, even in advanced stages.
The study has several limitations. Firstly, the follow-up period was relatively short, particularly for assessing outcomes in advanced-stage patients, where longer treatment durations may be required. Additionally, although the sedative effect of gabapentin was observed in only four cats, it may have influenced pain and quality of life assessments, potentially introducing a confounding factor. To ensure consistency across all patients, the same ECT protocol was applied using both needle and plate electrodes. Consequently, it was not possible to determine whether the type of electrode used had any impact on the pain caused by the treatment. Another limitation was the difference in group sizes; although a statistically significant comparison was made between the two groups, the imbalance in patient distribution across stages and different tumor localization could have influenced the overall results. Furthermore, the assessments provided by owners and veterinarians were based on different methodologies, which may have introduced variability in the evaluation of outcomes. Although the two approaches were aligned by including the animal’s response to palpation of the tumour-affected area in both evaluations, this methodological difference remains a limitation. Finally, for ethical reasons, a placebo was not administered to the control group, which may have influenced the subjective perception of treatment efficacy by both owners and veterinarians.
Conclusions
Gabapentin has proven to be a well-tolerated and effective option for pain management. The combined assessment of the cat’s quality of life by both the owner and veterinarian is essential to ensure the animal’s overall well-being throughout the treatment process. In advanced stages, the disease is associated with pain, which may be exacerbated by ECT, requiring close monitoring both immediately after treatment and in the long term. While mild adverse effects are observed, they generally resolve over time.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Tozon, N., Pavlin, D., Sersa, G., Dolinsek, T. & Cemazar, M. Electrochemotherapy with intravenous bleomycin injection: an observational study in superficial squamous cell carcinoma in cats. J. Feline Med. Surg. 16, 291–299 (2014).
Goldschmidt, M. H. & Shofer, F. S. Skin Tumors of the Dog and Cat, 2nd edn. (1998).
Thomson, M. Squamous cell carcinoma of the nasal planum in cats and dogs. Clin. Tech. Small Anim. Pract. 22, 42–45 (2007).
Simčič, P. et al. A retrospective multicentric study of electrochemotherapy in the treatment of feline nasal planum squamous cell carcinoma. Vet. Sci. 8, 53 (2021).
Lana, S., Ogilvie, G., Withrow, S., Straw, R. & Rogers, K. Feline cutaneous squamous cell carcinoma of the nasal planum and the pinnae: 61 cases. J. Am. Anim. Hosp. Assoc. 33, 329–332 (1997).
Vail, D. M., Thamm, D. H. & Lipatk, J. M. Withrow e MacEwen’s Small Animal Clinical Oncology. (2020).
Murphy, S. Cutaneous squamous cell carcinoma in the cat. J. Feline Med. Surg. 15, 401–407 (2013).
Owen, L. N. TNM Classification of Tumours in Domestic Animals. 46–47 (1980).
Dos Anjos, D. S., Sierra, O. R., Spugnini, E. P., De Nardi, A. B. & Fonseca-Alves, C. E. Comparison of two different doses of bleomycin in electrochemotherapy protocols for feline cutaneous squamous cell carcinoma nonsegregated from ultraviolet light exposure. Sci. Rep. 10, 18362 (2020).
Spugnini, E. P. & Baldi, A. Electrochemotherapy in Veterinary Oncology: State-of-the-Art and Perspectives. Vet. Clin. N. Am. Small Anim. Pract. 49, 967–979. https://doi.org/10.1016/j.cvsm.2019.04.006 (2019).
Spugnini, E. P. et al. Electrochemotherapy for the treatment of squamous cell carcinoma in cats: A preliminary report. Vet. J. 179, 117–120 (2009).
Tellado, M., Mir, L. M. & Maglietti, F. Veterinary guidelines for electrochemotherapy of superficial tumors. Front. Vet. Sci. 9, (2022).
Ramos, S. C., Dias-Pereira, P., Luís, A. L., MacFarlane, M. & Santos, A. A. Electrochemotherapy in dogs and cats—A review. Vet. Comp. Oncol. 22, 311–321 (2024).
Di Cesare, F. et al. Gabapentin: clinical use and pharmacokinetics in dogs, cats, and horses. Animals. 13, 2045 (2023).
Kukkar, A., Bali, A., Singh, N. & Jaggi, A. S. Implications and mechanism of action of Gabapentin in neuropathic pain. Arch. Pharm. Res. 36, 237–251 (2013).
Baillie, J. K. & Power, I. The mechanism of action of Gabapentin in neuropathic pain. Curr. Opin. Investig. Drugs. 7, 33–39 (2006).
Vettorato, E. & Corletto, F. Gabapentin as part of multi-modal analgesia in two cats suffering multiple injuries. Vet. Anaesth. Analg. 38, 518–520 (2011).
Lorenz, N. D., Comerford, E. J. & Iff, I. Long-term use of Gabapentin for musculoskeletal disease and trauma in three cats. J. Feline Med. Surg. 15, 507–512 (2013).
Rusbridge, C. Neuropathic pain in cats: mechanisms and multimodal management. J. Feline Med. Surg. 26, (2024).
Steagall, P. V. & Monteiro-Steagall, B. P. Multimodal analgesia for perioperative pain in three cats. J. Feline Med. Surg. 15, 737–743 (2013).
van Haaften, K. A., Forsythe, L. R. E., Stelow, E. A. & Bain, M. J. Effects of a single preappointment dose of Gabapentin on signs of stress in cats during transportation and veterinary examination. J. Am. Vet. Med. Assoc. 251, 1175–1181 (2017).
Erickson, A., Harbin, K., MacPherson, J., Rundle, K. & Overall, K. L. A review of pre-appointment medications to reduce fear and anxiety in dogs and cats at veterinary visits. Can. Vet. J. 62, 952–960 (2021).
Eagan, B. H., van Haaften, K. & Protopopova, A. Daily Gabapentin improved behavior modification progress and decreased stress in shelter cats from hoarding environments in a double-blind randomized placebo-controlled clinical trial. J. Am. Vet. Med. Assoc. 261, 1305–1315 (2023).
Spugnini, E. P. et al. Definition of novel electrochemotherapy parameters and validation of their in vitro and in vivo effectiveness. J. Cell. Physiol. 229, 1177–1181 (2014).
LeBlanc, A. K. et al. Veterinary < scp > Cooperative Oncology Group—Common terminology criteria for adverse events (< scp > VCOG-CTCAE v2) following investigational therapy in dogs and cats. Vet. Comp. Oncol. 19, 311–352 (2021).
Campana, L. G. et al. Bleomycin-based electrochemotherapy: clinical outcome from a single institution’s experience with 52 patients. Ann. Surg. Oncol. 16, 191–199 (2009).
Matthiessen, L. W. et al. Electrochemotherapy for large cutaneous recurrence of breast cancer: A phase II clinical trial. Acta Oncol. (Madr). 51, 713–721 (2012).
DeToledo, J. C., Toledo, C., DeCerce, J. & Ramsay, R. E. Changes in body weight with chronic, high-dose gabapentin therapy. Ther. Drug Monit. 19, 394–396 (1997).
Fantinati, M. et al. Appetite-stimulating effect of Gabapentin vs Mirtazapine in healthy cats post-ovariectomy. J. Feline Med. Surg. 22, 1176–1183 (2020).
Ferro, L. et al. Appetite stimulant and anti-emetic effect of mirtazapine transdermal ointment in cats affected by lymphoma following chemotherapy administration: A Multi-Centre retrospective study. Animals. 12, 155 (2022).
Ferrer-Jorda, E. & Rodríguez-Pizà, I. Description of outcome and adverse events in 21 cats with locally advanced nasal planum squamous cell carcinoma treated with electrochemotherapy. J. Feline Med. Surg 26, (2024).
Tucker, L. E. et al. Evaluation of the sedative properties of oral trazodone, Gabapentin or their combination in healthy cats. J. Feline Med. Surg 26, (2024).
Spugnini, E. P. & Porrello, A. Potentiation of chemotherapy in companion animals with spontaneous large neoplasms by application of biphasic electric pulses. J. Exp. Clin. Cancer Res. 22, 571–580 (2003).
Acknowledgements
The authors thank Prof. Aristide Maggiolino from the Animal Science section of the Department of Veterinary Medicine, University of Bari, for the statistical support in the preparation of this paper.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: S.C. and D.F. Methodology: S.C., A.D.B., C.P. Investigation: S.C., C.P., D.F., Visualization: S.C., D.F. Funding acquisition: not applicable. Project administration: S.C. and D.F. Data analysis: L.F., S.C., C.P. Supervision: S.C. and D.F. Writing—original draft: S.C., C.P. and D.F. Writing—review and editing: D.F. and S.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
All cat owners signed an informed consent form for the administration of electrochemotherapy and intravenous chemotherapy with Bleomycin. Additionally, the owners completed a diary to assess the quality of life (QoL) throughout the entire gabapentin treatment. All procedures were carried out by veterinary personnel for diagnostic purposes, and methods involving animals were performed in accordance with the relevant guidelines and regulations. This study was approved by the Ethics Committee of Department of Veterinary Medicine – University of Bari (Authorization n 38/24).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ciccarelli, S., Perrone, C., Forte, L. et al. Efficacy of gabapentin as pain management of T2–T4 feline facial squamous cell carcinoma treated with electrochemotherapy. Sci Rep 15, 27874 (2025). https://doi.org/10.1038/s41598-025-13767-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13767-w