Abstract
Recent studies have considered pancreatectomy combined with synchronous metastasectomy as a potential treatment option for patients with metastatic pancreatic ductal adenocarcinoma (PDAC). This study aimed to evaluate the role of surgery in PDAC patients with hepatic metastases and to identify the prognostic factors. PubMed, Embase, and Cochrane Library databases were searched and the hazard ratio (HR) with 95% confidence interval (CI) was extracted from eligible studies. Pooled HR with 95% CI were used to reveal the association between synchronous surgery and overall survival (OS). Thirteen studies with 1107 patients were included. The results (pooled HR 0.496, 95% CI 0.414–0.594, I2 = 0, p = 0.531) indicated that simultaneous resection could prolong the survival of PDAC patients with hepatic metastases. Moreover, patients who underwent synchronous surgery plus preoperative chemotherapy had better OS than those who received synchronous surgery alone (HR 0.579, 95% CI 0.473–0.709, I2 = 0, p = 0.418). Preoperative chemotherapy, resection of the primary tumor, R0 resection margin status at pancreatic resection and postoperative chemotherapy were the prognostic factors in PDAC patients with liver metastasis. Synchronous resection of primary tumors and metastases could prolong the survival of PDAC patients with hepatic metastases, and adjuvant chemotherapy played a crucial role in the perioperative period of metastatic PDAC patients.
Similar content being viewed by others
Introduction
Pancreatic ductal adenocarcinoma (PDAC), arising from the pancreatic ductal epithelium, is one of the most aggressive malignant digestive system tumors, with a 5-year survival rate of less than 10%1. Surgical resection is taken as the only curative therapy for PDAC, and the 5-year survival rate after radical resection is approximately 20%2,3. Unfortunately, more than half of the patients present with distant metastases and are considered an absolute contraindication for surgical resection4,5. Additionally, even among PDAC patients evaluated as resectable, there are 14%-30% of patients have abdominal metastasis (such as liver metastasis, mesenteric metastasis, or peritoneal implant metastasis) during open surgery or laparoscopic exploration without any positive signs on preoperative imaging examination, which is also known as occult metastasis6. The most common site of metastasis is the liver, which accounts for approximately 80% of PDAC cases with distant metastases7.
Palliative chemotherapy is the standard therapeutic strategy for the treatment of unresectable metastatic PDAC (UR-M PDAC). Gemcitabine plus nab-paclitaxel (GA) and FOLFIRINOX (fluorouracil, irinotecan, oxaliplatin, and calcium folinate) have become the first-line medications for UR-M PDAC, which could prolong overall survival (OS)8,9. Historically, resection of recurrent or metastatic pancreatic cancer seemed to be inconceivable. However, in recent years, pancreatectomy combined with synchronous or metachronous metastasectomy has been considered for selected patients with UR-M PDAC. Synchronous resection of primary tumors and metastases in PDAC may provide survival benefits without compromising safety and quality of life in a highly selected group of patients10,11,12.
In this context, our aim is to evaluate the clinical value of surgical resection of PDAC with synchronous metastases and to confirm the prognostic factors of PDAC patients with simultaneous liver metastasis.
Materials and methods
The systematic review and meta-analysis were done according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement13. This systematic review and meta-analysis was also conducted following the recommendations of the AMSTAR (Assessing the methodological quality of systematic reviews) guidelines14.
Search strategies
The PubMed, Embase, and Cochrane Library databases were searched for eligible articles up to September 1, 2024. The search was conducted using medical subject headings (MeSH) in combination with free-text words. The following search headings were used: “pancreatic cancer”, “liver”, “metastasis”, “resection”, and “hepatectomy”, and we used “AND”,“OR”,“NOT”for combination of these headings to avoid missing and wrong articles. The search strategy is described in the Supplementary Materials. Our protocol was registered on the International Platform of Registered Systematic Review and Meta-analysis Protocols database (INPLASY2024100064).
Inclusion and exclusion criteria
All studies included in the meta-analysis were selected according to the following inclusion criteria: (1) all patients were diagnosed with PDAC with synchronous liver metastases; (2) primary tumor and metastases were simultaneously resected with or without preoperative chemotherapy; (3) survival data can be collected in the literature; (4) Newcastle–Ottawa Quality Assessment Scale (NOS) score ≥ 6. The exclusion criteria were as follows: (1) neuroendocrine tumor and other pathological types; (2) metachronous liver metastasis; (3) studies with incomplete survival data; (4) abstracts, case reports, editorials, letters, systematic reviews, and comments; (5) studies that enrolled the overlapped or same population; and (6) duplicate studies.
Data extraction
Two investigators (PCZ and ZHW) independently extracted the necessary data from the included studies, and any disagreements were resolved by discussion until a consensus was reached. The following data were extracted from each study: first author, publication year, country, study design, number of patients, follow-up duration, tumor site, number of liver metastases, median survival time, and overall survival.
Quality assessment
The Newcastle–Ottawa Quality Assessment Scale (NOS) was used to evaluate the quality of the included studies. NOS consists of three aspects: selection, comparability, and outcomes. Studies with a score of six or higher were considered high-quality studies15. This work was also performed independently by two investigators (PCZ and ZHW). (Supplementary Table S1).
Statistical analysis
Meta-analysis was conducted using Stata 14.0 software, following the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines. The heterogeneity of the pooled effect was assessed using Cochran’s Q test and the Higgins I2 statistic. Q test p value < 0.1 or I2 > 50% was considered significant heterogeneity, and a random-effect model was applied to estimate the pooled HR. While heterogeneity was not significant (Q test p value > 0.1 or I2 < 50%), a fixed-effect model was used. Sensitivity analysis was applied to reduce and explain heterogeneity among the studies. Furthermore, publication bias was visually checked through a funnel plot and then quantitatively analyzed using Begg’s and Egger’s tests. All statistical tests were two-sided, and a p value less than 0.05 were defined as statistically significant.
Results
Study selection
We searched the PubMed, Embase, and Cochrane Library databases, and 6560 articles were initially retrieved. After removing 363 duplicates, 6197 articles remained. After screening the titles and abstracts, 6127 articles were excluded for being irrelevant topics, reviews or meta-analysis, conference abstracts, letters, case reports, case series, or comments. Finally, 14 articles met our inclusion criteria, and 1107 patients had UR-M PDAC with synchronous hepatic metastasis16,17,18,19,20,21,22,23,24,25,26,27,28,29. Among the 1107 patients, 553 patients who underwent synchronous resection of the primary tumor and metastases were included in this meta-analysis, while 554 patients received palliative chemotherapy and constituted the non-surgical group. The detailed selection process was illustrated in Fig. 1.
Clinical characteristic of enrolled studies
All included studies were retrospective and were mainly published in the past ten years. Among the 553 patients who underwent surgery, 185 underwent preoperative chemotherapy, while the others underwent upfront surgery. Palliative chemotherapy was administered to the rest 554 patients. The scores of study quality assessed by the NOS ranged from 6 to 8. The main characteristics of the surgical and the non-surgical populations were presented in Tables 1 and 2.
Clinical benefits of curative surgery in PDAC patients with liver metastases
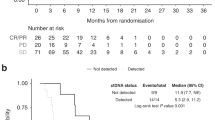
Seven studies investigated patients who underwent synchronous resection of primary tumors and liver metastases16,18,22,23,26,27,29. There were 553 patients in surgical group, whereas the non-surgical group included 554patients. The pooled HR was 0.496 with 95% CI: 0.414–0.594 (I2 = 0, p = 0.531). It revealed that simultaneous resection could prolong the survival of PDAC patients with hepatic metastases. (Fig. 2).
Clinical values of preoperative chemotherapy in PDAC patients with liver metastases
Four studies reported the survival data of PDAC patients with liver metastases underwent preoperative chemotherapy16,17,18,19. A total of 107 patients who underwent synchronous resection of the primary tumor and liver metastases with preoperative chemotherapy were enrolled, while 72 patients underwent upfront surgery without chemotherapy. The characteristics of patients who underwent preoperative chemotherapy were reported in Table 3. According to the pooled results (HR = 0.579, 95% CI: 0.473–0.709, I2 = 0, p = 0.418), patients performed preoperative chemotherapy had better OS. Forest plot was illustrated in Fig. 3.
Subgroup analyses and meta regression analyses
To explore and explain the heterogeneity, meta regression analyses were performed for the number of patients in the surgical group, the use of propensity score matching (PSM), and the administration of preoperative chemotherapy, yielding p-values of 0.825, 0.848, and 0.785, respectively. In addition, we performed subgroup analyses according to the aforementioned three factors, setting a cut-off value of 20 for the number of patients in the surgical group; the results were illustrated in Fig. 4A–C.
Sensitivity analysis and publication bias
Sensitivity analysis was conducted to assess the effect of individual studies on the pooled HR of OS in studies that included synchronous surgery, and the results suggested that omitting any individual studies had no significant effect on the pooled HR (Fig. 5). Furthermore, publication bias was investigated, and there was no obvious asymmetry in the funnel plot upon visual inspection (Fig. 6), then Begg’s and Egger’s tests yielded p-values of 0.035 and 0.072, respectively, which also indicated that there was some extent of publication bias among the included studies.
Prognostic factors in PDAC patients with liver metastasis
Clinicopathological variables were analyzed to identify the risk factors associated with prognosis and survival in PDAC patients with liver metastasis. Finally, preoperative chemotherapy, resection of the primary tumor, R0 resection margin status at pancreatic resection, and postoperative chemotherapy could be considered as independent prognostic factors in PDAC patients with liver metastasis,and the results were presented in Table 4.
Discussion
Synchronous resection the primary and metastatic tumors has gained wide acceptance as a curative treatment in colorectal cancer patients with liver metastases30,31. The role of synchronous surgery for hepatic metastases from pancreatic neuroendocrine tumors on long-term outcomes has also been well-documented32,33,34. Nonetheless, radical surgery was used to be heresy in most instances for PDAC patients with liver metastases, and palliative chemotherapy seemed to be the only option. With advances in systemic treatment and surgical techniques, synchronous resection has been introduced in recent years for PDAC patients with liver metastasis. Some studies reported that radical surgery was valuable and could prolong survival35, whereas some articles were discouraged because it did not improve survival36.
To clarify the controversy regarding synchronous resection, we collected relevant studies and conducted a meta-analysis. In our study, 14 articles with 1107 PDAC patients with synchronous hepatic metastases were enrolled16,17,18,19,20,21,22,23,24,25,26,27,28,29. Our pooled analysis showed that simultaneous resection could significantly improve overall survival of PDAC patients with hepatic metastases compared to those who did not undergo surgery (HR = 0.496, 95% CI: 0.414–0.594, I2 = 0, p = 0.531). Furthermore, according to our further study, PDAC patients with hepatic metastases who received preoperative chemotherapy had better survival than those who underwent upfront surgery (HR = 0.579, 95% CI: 0.473–0.709, I2 = 0, p = 0.418). We also confirmed several risk factors associated with the prognosis of liver metastases. These included preoperative chemotherapy, resection of the primary tumor, and resection margin status et al.
Chemotherapy, especially preoperative chemotherapy, played a crucial role in the management of PDAC patients with liver metastases. For metastatic patients, GA, FOLFIRINOX, and modified FOLFIRINOX (m-FOLFIRINOX) were the standard regimens. The results of a phase III clinical trial showed that the median OS of the FOLFIRINOX regimen for the treatment of UR-M PDAC was 11.1 months, which was significantly longer than that of the gemcitabine single-agent group at 6.8 months (p < 0.01). The progression-free survival (PFS) was also significantly prolonged (6.4 months vs. 3.3 months, p < 0.001)37,38,39. A phase II clinical trial also investigated m-FOLFIRINOX, which revealed that m-FOLFIRINOX prolonged survival, reduced the incidence of side effects, and improved chemotherapy tolerance40. Recently, NALIFIROX (liposome irinotecan, 5-fluorouracil, leucovorin, and oxaliplatin) has been introduced as a novel reference regimen for the treatment of metastatic patients. The OS and progression-free survival (PFS) of the NALIFIROX group were 11.1 months and 7.4 months, respectively, which were superior to the 9.2 months and 5.6 months in the GA group (P values were 0.036 and < 0.001, respectively)41. In our study, preoperative chemotherapy ( pooled HR: 0.307, 95% CI: 0.219–0.433) was an independent risk factor associated with survival. According to Crippa et al., the median OS of 11 metastatic patients with partial or complete response after preoperative chemotherapy was obviously longer than that of the remaining 116 patients who did not undergo surgery (median OS: 39 vs 11 months, p < 0.0001)27. Preoperative chemotherapy was helpful in assessing tumor biological behavior, screening potential patients for surgery, and eliminating or controlling liver metastases. Therefore, compared to upfront surgery (surgery-first), conversion surgery (chemotherapy-first) had significantly better median survival in PDAC patients with synchronous hepatic metastases.
The optimal duration of preoperative chemotherapy is still debated. In the current studies, the median duration of preoperative chemotherapy for PDAC patients with liver metastases was 6.2 to 12 months. Ushida et al. believed that a duration of preoperative chemotherapy ≥ 8 months was an independent protective factor and could improve the prognosis of patients42. Conversely, in accordance with Hank’s study, a time interval from initial diagnosis to surgery of < 5 months or ≥ 9 months was an independent risk factor and was associated with poor prognosis43. The criteria for conversion surgery are also debatable. Ushida et al. proposed that the indications for conversion surgery for UR-M PDAC were serum CA19-9 level within the normal range, imaging examination results showing tumor shrinkage, progression-free survival of 8 months or more, and disappearance of metastatic lesions42. In addition, Hank et al. defined a relatively lax indication: the primary lesion was evaluated as stable or improved according to the Response Evaluation Criteria in Solid Tumors (RECIST) standard, the metastatic lesion was partially responded to or better, and the tumor marker level was reduced. More clinical trials were required to determine the best surgical indication43.
The role of postoperative chemotherapy in patients with metastasis was also unclear. Nagal et al. showed that postoperative chemotherapy had little impact on the median OS after surgical resection of UR-M PDAC with liver metastases17. The main reasons why patients did not undergo postoperative chemotherapy were poor physical condition, severe complications, older age, and patient unwillingness44. In our study, we enrolled three articles, and the pooled results (HR = 0.430, 95% CI: 0.283–0.653) indicated that postoperative chemotherapy was associated with better OS19,20,23.
This meta-analysis has several limitations. Firstly, all the included studies were retrospective, so the overall level of clinical evidence was relatively low, and potential selection bias was inevitable. Secondly, the survival data of the studies were estimated from the survival curve and survival time, which might not be very accurate. Thirdly, the sample size was relatively small. Therefore, caution should be exercised in the pooled results of the meta-analysis.
Conclusion
In summary, our meta-analysis revealed that preoperative chemotherapy combined with simultaneous resection of both primary and metastatic tumors was able to prolong the survival of PDAC patients with synchronous liver metastases and that these patients could also benefit from postoperative chemotherapy. Moreover, owing to the existing limitations, large, multicenter RCTs are urgently needed.
Data availability
The original contributions of the study are included in the article/supplementary materials.
References
Siegel, R. L., Miller, K. D., Wagle, N. S. & Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 73, 17–48. https://doi.org/10.3322/caac.21763 (2023).
Strobel, O., Neoptolemos, J., Jäger, D. & Büchler, M. W. Optimizing the outcomes of pancreatic cancer surgery. Nat. Rev. Clin. Oncol. 16, 11–26. https://doi.org/10.1038/s41571-018-0112-1 (2019).
Liu, C. et al. Association between preoperative sarcopenia and prognosis of pancreatic cancer after curative-intent surgery: A updated systematic review and meta-analysis. World J. Surg. Oncol. 22, 38. https://doi.org/10.1186/s12957-024-03310-y (2024).
Park, W., Chawla, A. & O’Reilly, E. M. Pancreatic cancer: A review. JAMA 326, 851–862. https://doi.org/10.1001/jama.2021.13027 (2021).
Mizrahi, J. D., Surana, R., Valle, J. W. & Shroff, R. T. Pancreatic cancer. Lancet 395, 2008–2020. https://doi.org/10.1016/s0140-6736(20)30974-0 (2020).
Sakaguchi, T. et al. A simple risk score for detecting radiological occult metastasis in patients with resectable or borderline resectable pancreatic ductal adenocarcinoma. J. Hepatobiliary Pancreat. Sci. 29, 262–270. https://doi.org/10.1002/jhbp.1026 (2022).
Noda, Y., Tochigi, T., Baliyan, V., Kordbacheh, H. & Kambadakone, A. Hepatobiliary contrast uptake patterns on gadoxetic acid-enhanced MRI in liver metastases from pancreatic ductal adenocarcinoma: Can it predict prognosis?. Eur. Radiol. 31, 276–282. https://doi.org/10.1007/s00330-020-07115-x (2021).
Ay, S. et al. FOLFIRINOX versus gemcitabine plus nab-paclitaxel as the first-line chemotherapy in metastatic pancreatic cancer. J. Chemother. 34, 465–471. https://doi.org/10.1080/1120009x.2022.2026125 (2022).
Di Costanzo, F., Di Costanzo, F., Antonuzzo, L., Mazza, E. & Giommoni, E. Optimizing first-line chemotherapy in metastatic pancreatic cancer: Efficacy of FOLFIRINOX versus nab-paclitaxel plus gemcitabine. Cancers https://doi.org/10.3390/cancers15020416 (2023).
Crippa, S. et al. A systematic review of surgical resection of liver-only synchronous metastases from pancreatic cancer in the era of multiagent chemotherapy. Updates Surg. 72, 39–45. https://doi.org/10.1007/s13304-020-00710-z (2020).
De Simoni, O. et al. Oligometastatic pancreatic cancer to the liver in the era of neoadjuvant chemotherapy: Which role for conversion surgery? A systematic review and meta-analysis. Cancers https://doi.org/10.3390/cancers12113402 (2020).
Sakaguchi, T., Valente, R., Tanaka, K., Satoi, S. & Del Chiaro, M. Surgical treatment of metastatic pancreatic ductal adenocarcinoma: A review of current literature. Pancreatology 19, 672–680. https://doi.org/10.1016/j.pan.2019.05.466 (2019).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 88, 105906. https://doi.org/10.1016/j.ijsu.2021.105906 (2021).
Shea, B. J. et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358, j4008. https://doi.org/10.1136/bmj.j4008 (2017).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012. https://doi.org/10.1001/jama.283.15.2008 (2000).
Satoi, S. et al. Oncological role of surgical resection in patients with pancreatic ductal adenocarcinoma with liver-only synchronous metastases in a single-center retrospective study. J. Gastrointest. Oncol. 14, 2587–2599. https://doi.org/10.21037/jgo-23-655 (2023).
Nagai, M. et al. Oncologic resection of pancreatic cancer with isolated liver metastasis: Favorable outcomes in select patients. J. Hepatobiliary Pancreat. Sci. 30, 1025–1035. https://doi.org/10.1002/jhbp.1303 (2023).
Yun, W. G. et al. The role of local treatment including pancreatectomy for pancreatic ductal adenocarcinoma patients with isolated synchronous liver metastasis: Propensity score-matched analyses. J. Hepatobiliary Pancreat. Sci. 30, 1036–1045. https://doi.org/10.1002/jhbp.1313 (2023).
Bachellier, P., Addeo, P., Averous, G. & Dufour, P. Resection of pancreatic adenocarcinomas with synchronous liver metastases: A retrospective study of prognostic factors for survival. Surgery 172, 1245–1250. https://doi.org/10.1016/j.surg.2022.03.003 (2022).
Jin, T., Dai, C. & Xu, F. Clinical effect of simultaneous surgical resection of hepatic and pancreatic lesions versus systemic chemotherapy in treatment of resectable pancreatic cancer with liver metastasis. J. Clin. Hepatol. 38(3), 622–628 (2022).
Safi, S. A. et al. Surgical margin clearance and extended chemotherapy defines survival for synchronous oligometastatic liver lesions of the ductal adenocarcinoma of the pancreas. Int. J. Clin. Oncol. 26, 1911–1921. https://doi.org/10.1007/s10147-021-01961-5 (2021).
Shao, Y. et al. Feasibility of pancreaticoduodenectomy with synchronous liver metastasectomy for oligometastatic pancreatic ductal adenocarcinoma: A case-control study. Ann. Med. Surg. 62, 490–494. https://doi.org/10.1016/j.amsu.2020.11.037 (2021).
Yang, J. et al. Patients with hepatic oligometastatic pancreatic body/tail ductal adenocarcinoma may benefit from synchronous resection. HPB 22, 91–101. https://doi.org/10.1016/j.hpb.2019.05.015 (2020).
Andreou, A. et al. The role of hepatectomy for synchronous liver metastases from pancreatic adenocarcinoma. Surg. Oncol. 27, 688–694. https://doi.org/10.1016/j.suronc.2018.09.004 (2018).
Hackert, T. et al. Radical surgery of oligometastatic pancreatic cancer. Eur. J. Surg. Oncol. 43, 358–363. https://doi.org/10.1016/j.ejso.2016.10.023 (2017).
Tachezy, M. et al. Synchronous resections of hepatic oligometastatic pancreatic cancer: Disputing a principle in a time of safe pancreatic operations in a retrospective multicenter analysis. Surgery 160, 136–144. https://doi.org/10.1016/j.surg.2016.02.019 (2016).
Crippa, S. et al. Is there a role for surgical resection in patients with pancreatic cancer with liver metastases responding to chemotherapy?. Eur. J. Surg. Oncol. 42, 1533–1539. https://doi.org/10.1016/j.ejso.2016.06.398 (2016).
Gleisner, A. L. et al. Is resection of periampullary or pancreatic adenocarcinoma with synchronous hepatic metastasis justified?. Cancer 110, 2484–2492. https://doi.org/10.1002/cncr.23074 (2007).
Shrikhande, S. V. et al. Pancreatic resection for M1 pancreatic ductal adenocarcinoma. Ann. Surg. Oncol. 14, 118–127. https://doi.org/10.1245/s10434-006-9131-8 (2007).
Tepelenis, K. et al. The role of preoperative chemotherapy in the management of synchronous resectable colorectal liver metastases: A meta-analysis. Curr. Oncol. 30, 4499–4511. https://doi.org/10.3390/curroncol30050340 (2023).
Wang, S. H., Song, L., Tang, J. Y., Sun, W. P. & Li, Z. Safety and long-term prognosis of simultaneous versus staged resection in synchronous colorectal cancer with liver metastasis: A systematic review and meta-analysis. Eur. J. Med. Res. 27, 297. https://doi.org/10.1186/s40001-022-00937-z (2022).
Wu, Z., Qiu, X., Zhi, Y., Shi, X. & Lv, G. The risk and prognostic factors for G1 pancreatic neuroendocrine tumors: A retrospective analysis of the SEER database. Front. Oncol. 12, 993524. https://doi.org/10.3389/fonc.2022.993524 (2022).
Yang, Z., Liang, J., Leng, K. & Shi, G. Survival benefit of surgical resection for pancreatic neuroendocrine tumors with oligometastatic liver metastasis: A retrospective and propensity score-matching analysis. Front. Oncol. 12, 903560. https://doi.org/10.3389/fonc.2022.903560 (2022).
Zheng, M., Li, Y., Li, T., Zhang, L. & Zhou, L. Resection of the primary tumor improves survival in patients with gastro-entero-pancreatic neuroendocrine neoplasms with liver metastases: A SEER-based analysis. Cancer Med. 8, 5128–5136. https://doi.org/10.1002/cam4.2431 (2019).
Takeda, T. et al. Outcomes of pancreatic cancer with liver oligometastasis. J. Hepatobiliary Pancreat. Sci. 30, 229–239. https://doi.org/10.1002/jhbp.1184 (2023).
Takada, T., Yasuda, H., Amano, H., Yoshida, M. & Uchida, T. Simultaneous hepatic resection with pancreato-duodenectomy for metastatic pancreatic head carcinoma: does it improve survival?. Hepatogastroenterology 44, 567–573 (1997).
Gunturu, K. S., Jarboe, J. & Saif, M. W. Highlights on the first line treatment of metastatic pancreatic cancer. Jop 13, 361–367. https://doi.org/10.6092/1590-8577/963 (2012).
Von Hoff, D. D. et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 369, 1691–1703. https://doi.org/10.1056/NEJMoa1304369 (2013).
Conroy, T. et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 364, 1817–1825. https://doi.org/10.1056/NEJMoa1011923 (2011).
Stein, S. M. et al. Final analysis of a phase II study of modified FOLFIRINOX in locally advanced and metastatic pancreatic cancer. Br. J. Cancer 114, 737–743. https://doi.org/10.1038/bjc.2016.45 (2016).
Wainberg, Z. A. et al. NALIRIFOX versus nab-paclitaxel and gemcitabine in treatment-naive patients with metastatic pancreatic ductal adenocarcinoma (NAPOLI 3): A randomised, open-label, phase 3 trial. Lancet 402, 1272–1281. https://doi.org/10.1016/s0140-6736(23)01366-1 (2023).
Ushida, Y. et al. Optimizing indications for conversion surgery based on analysis of 454 consecutive Japanese cases with unresectable pancreatic cancer who received modified FOLFIRINOX or gemcitabine plus nab-paclitaxel: A single-center retrospective study. Ann. Surg. Oncol. 29, 5038–5050. https://doi.org/10.1245/s10434-022-11503-6 (2022).
Hank, T. et al. Oncological outcome of conversion surgery after preoperative chemotherapy for metastatic pancreatic cancer. Ann. Surg. 277, e1089–e1098. https://doi.org/10.1097/sla.0000000000005481 (2023).
Mataki, Y. et al. Clinical benefits of conversion surgery for unresectable pancreatic ductal adenocarcinoma: A single-institution retrospective analysis. Cancers https://doi.org/10.3390/cancers13051057 (2021).
Acknowledgements
The authors thank all medical staff who contributed to the maintenance of the medical record database.
Author information
Authors and Affiliations
Contributions
PCZ, ZHW, and BLT conceived of and designed the study. PCZ, ZHW, and KX were responsible for the collection and assembly of the data, data analysis, and interpretation. PCZ and ZHW were involved in writing the manuscript. PCZ, ZHW and BLT revised the manuscript accordingly. All authors have contributed to the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This meta-analysis or review article is not applicable to this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, P., Wang, Z., Xue, K. et al. Synchronous surgery combined preoperative chemotherapy benefits patients suffering pancreatic ductal adenocarcinoma with liver metastases: a systematic review and meta-analysis. Sci Rep 15, 28403 (2025). https://doi.org/10.1038/s41598-025-13811-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13811-9