Abstract
This study aims to establish normative data for the Smoothness Index (SI) of the iris surface using Anterior Segment Optical Coherence Tomography (AS-OCT) in a healthy population. The study included 198 eyes from 99 subjects, 50 female and 49 males. The average age of participants was 46.71 ± 16.25, spanning 18–75 years. AS-OCT imaging was performed on both eyes before and after pupil dilation. The SI was calculated for various meridians of the iris. Participants were healthy individuals with no underlying iris pathologies, normal intraocular pressure, and a refractive error ranging from spherical equivalent (SE) -3.00 to + 3.00 diopters (D). The average SI was found to be 0.812 ± 0.036, with no significant differences between the eyes. The SI increased slightly with age and was higher in undilated pupils compared to dilated pupils. The study found no significant association between sex and the average SI. The normative range of SI across various meridians was established, providing a reference for future research on iris pathologies. This study highlights the SI pattern of normal iris in Iranians, which can be used for comparison in future research on iris pathologies. These findings are to be confirmed in a larger and more heterogeneous population.
Similar content being viewed by others
Introduction
Since optical coherence tomography (OCT) imaging of the anterior segment of the eye (AS-OCT) was introduced in 1994, significant advancements have been made in resolution, tissue penetration, and analytical methodologies1. The images produced by AS-OCT are essential for clinicians and researchers, offering critical insights into the anatomical characteristics of the anterior segment and associated pathologies. Due to the ever-increasing progress of imaging tools and modalities in ophthalmology, researchers’ interest in quantitative studies in this field has increased significantly2,3.
For example, AS-OCT has proposed various quantitative iris parameters to investigate related pathologies. In 2010, Wang and his colleagues investigated iris characteristics such as curvature, area, and thickness using AS-OCT, and its relationship with the susceptibility to Angle Closure Glaucoma (ACG)4. AS-OCT metrics play a significant role in the identification of pigment dispersion syndrome as well5. According to Ozer and his colleagues research, one of the most frequently observed iris characteristics in unilateral herpetic uveitis is the disorganization of the iris layers (DIL), which can be detected through AS-OCT imaging techniques6. Several studies have been conducted to analyze the modifications in iris parameters in the context of Fuchs uveitis (FU), employing AS-OCT7,8,9.
In 2019, Zarei and his colleagues defined a new and practical index called Smoothness index (SI) as the ratio of the length of the straight line from the most peripheral to the most central part of the iris to the actual length of the iris surface. The use of SI allows for a quantitative evaluation of the iris surface smoothness, potentially aiding in the identification of subtle atrophic changes in the iris of eyes impacted by FU, particularly when heterochromia is not present10,11.
Recent studies suggest that SI may serve as a useful biomarker not only in FU but also in other anterior segment conditions where structural iris integrity is altered, thus reinforcing its clinical relevance in detecting early or subclinical pathology12,13. Emerging evidence has further highlighted the diagnostic value of SI in differentiating between forms of anterior uveitis that often share overlapping clinical features. For instance, SI has been applied to distinguish cytomegalovirus (CMV)-related anterior uveitis from rubella virus-associated uveitis, both of which can present with mild inflammation and elevated intraocular pressure. Similarly, SI has demonstrated utility in differentiating FU from Posner-Schlossman syndrome, conditions that share clinical characteristics such as unilateral ocular hypertension and subtle anterior chamber reaction. In both cases, SI provided objective, non-invasive insight into differences in iris surface smoothness, supporting its role as a valuable adjunct in clinical decision-making13,14.
However, the lack of sufficient studies defining the normal range of this novel index to minimize the effect of inter-individual differences and the possible effect of various factors including pupil dilation, sex, and age indicates the necessity and importance of the present study.
This study outlines the normative range of SI across various meridians, taking into account pupil status and gender differences. By establishing this baseline, the findings aim to enhance the interpretability of SI in clinical assessments and future research.
Methods
This observational study was conducted at Farabi Eye Hospital, Tehran, Iran, in accordance with the Declaration of Helsinki and approved by the local Institutional Review Board (IRB). Eligible participants were healthy Iranian adults (≥ 18 years old) with normal intraocular pressure (IOP), no detectable iris abnormalities on ophthalmoscopic examination, and a refractive error within a spherical equivalent (SE) range of -3.00 to + 3.00 diopters (D). Exclusion criteria included history of ocular trauma, laser treatments, intraocular surgeries, intumescent cataracts, or use of topical/systemic ophthalmic medications. Additionally, participants with shallow anterior chamber angles, peripheral iridotomy/iridectomy, or abnormal iris configurations (e.g., plateau iris or anterior bowing) identified on AS-OCT were excluded to ensure population homogeneity.
All anterior segment optical coherence tomography (AS-OCT) imaging was performed in a standardized, windowless room using fixed-intensity LED lighting to eliminate ambient light variability. Imaging was conducted using a Swept Source (SS)-OCT system (CASIA 1 or 2, Tomey, Japan) in both eyes under undilated and pharmacologically dilated conditions, on the same day between 8:00 AM and 12:00 PM. Pupil dilation was achieved by instilling one drop of 1% Tropicamide in each eye, followed by a 30-minute waiting period. Full dilation was defined operationally as the absence of pupillary light reflex. Absolute pupil diameter was not used as a threshold since within-subject comparisons were the focus.
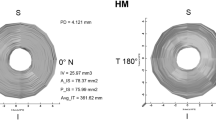
Participants were instructed to maintain wide eye opening and avoid blinking during image capture. During the imaging session, participants were asked to keep their eyes as wide open as possible and to avoid blinking. Imaging was repeated when artifacts were detected until acceptable image quality was obtained. Each eye was imaged along sixteen meridians spaced 11° apart (from 180° to 349°). As a result, each participant provided 64 AS-OCT images (16 from each eye in undilated and dilated stages, respectively).
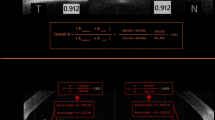
AS-OCT images were processed following protocols described in our previous study11. A brief summary of the key steps is provided here: First, the images were converted to grayscale, followed by initial preprocessing steps, including contrast enhancement and histogram matching. Adaptive K-means clustering was employed to segment the anterior iris border from the background, with manual verification to ensure accurate identification of the true iris edge, defined as the point of attachment to the ciliary body (peripheral) and the pupil margin (central). The basal length was calculated as the straight-line distance between these points, while the actual length followed the natural curvature of the iris surface, as required for the Smoothness Index (SI) calculation. To prevent measurement errors due to tilt, the Swept Source (SS)-OCT system’s automated alignment features were used to maintain a perpendicular imaging plane, and post-acquisition manual checks excluded images with misalignment or unclear iris boundaries. The SI was then computed for each hemi-meridian (Nasal, Temporal, Superior, and Inferior) and the overall SI for each scan using the equations provided.
Statistical analysis
Descriptive statistics were used to characterize the variables, including mean, standard deviation, median, range, frequency, and percentage. To compare subgroups while accounting for the correlation of eyes within a subject, a generalized estimating equation (GEE) was utilized. Iris thickness, estimated through anatomical screening to exclude significant variations (e.g., plateau iris or anteriorly bowed iris), was included as a covariate in the multivariate GEE analysis to account for its potential influence on Smoothness Index (SI) measurements. The Shapiro-Wilk test and Q-Q plots were used to assess data normality. All statistical analyses were conducted using SPSS software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). A p-value of less than 0.05 was considered statistically significant.
Results
A total of 198 eyes from 99 participants, comprising 50 females and 49 males, were included in the study. The mean age of participants was 46.71 ± 16.25, ranging from 18 to 75 years.
The normal range of all determined parameters including SI of hemi-meridians (SI1, SI2) and Overall SI of the sixteen axes is presented separately in Table 1 for females and males, as well as for dilated and undilated pupils in each eye (Table 1). For more detailed analysis refer to the supplementary Table 1.
In order to simplify the comparison, the average SI was determined by taking the mean of the overall SI values from all sixteen axes in each eye in undilated pupil status. The average SI in both eyes of individuals were same and measured 0.812 ± 0.036. Therefore, there was no inter-eye differences.
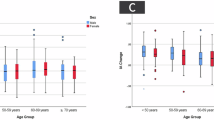
The GEE scatter plot demonstrates a significant association between age and average SI, with a regression coefficient of 0.001. This implies that an increase of one year in age corresponds to an approximate increase of 0.001 in average SI (Fig. 3).
Given that no inter-eye differences were observed in the analysis, all 198 eyes were compared to determine whether variations in pupil status would significantly affect the average SI. The GEE analysis indicates that the Average SI in undilated pupils exceeds that of dilated pupils, a difference that is statistically significant (B = 0.024 ,95%CI [0.019–0.028], P value < 0.001). Supplementary Table 2 provides a detailed comparison of all the sixteen axes overall SI, organized by eye (OD or OS) based on the pupil status. Across all axes, genders, and eyes, the SI was significantly higher in the undilated state compared to the dilated state (P < 0.001).
Multivariate GEE analysis confirmed that the average SI in undilated pupils is significantly greater than in dilated pupils (adjusted P < 0.001), as shown in Table 2. For a more detailed analysis, please refer to Supplementary Table 3.
Sex was not significantly associated with average SI (B = -0.005, 95% CI [-0.015, 0.004], P = 0.274). However, Supplementary Table 4 shows statistically significant sex differences in overall SI for specific axes.
Overall, the mean SI1 values seem marginally elevated compared to SI2 values across the majority of meridians in the right eye (Table 3). This observation aligns with the box plot analysis presented in Fig. 4, which also indicated that SI1 values generally exceed SI2 values. There are minor discrepancies in both mean values and standard deviations among various meridians. For example, SI1 values are significantly elevated at 180T and 270T and 90 S in comparison to other meridians.
Generally, for the left eye, SI2 values are marginally elevated compared to SI1 levels over the majority of meridians (Fig. 5; Table 4). This contrasts with the prior evaluation of the right eye, when SI1 levels were predominantly elevated. SI2 indices for the left eye at 0T and 90 S, in addition to the SI1 index at 270I, are considerably greater than other meridians indices.
The observation indicates that SI2 values are often elevated in the left eye and SI1 values are predominantly greater in the right eye, both suggesting the involvement of temporal hemi-meridians.
Discussion
The rapid development of imaging techniques and modalities in ophthalmology has significantly heightened researchers’ enthusiasm for conducting quantitative research, as the advent of AS-OCT revolutionized the qualitative and quantitative research on the anterior segment of the eye. Thus far, numerous iris parameters have been quantified through AS-OCT, enabling the recognition of iris pathologies in various diseases by comparing these findings against standard normative values in different populations15,16,17.
Since Zarei et al. presented the smoothness index (SI) as a for iris evaluation based on AS-OCT in 2019, a number of studies have been undertaken to assess the amount of this index in patients with various pathologies11,14,18,19,20. However, the absence of a standard range for comparing patient data may result in an incomplete interpretation of the findings. It was also necessary to consider the potential influence of characteristics such as age, gender, race, and the status of the pupil. Consequently, this research was carried out with the objective of augmenting the data associated with this novel index, with the intention of broadening its applicability in diverse iris pathologies. As we pioneered conducting this type of study and given the scarcity of prior research in this area, we do not possess adequate data to juxtapose our results with those of other investigations.
The normative range of average SI in this study was determined to be 0.812 ± 0.036, with no significant differences observed between the eyes.
Our study demonstrates a positive correlation between age and the Smoothness Index (SI) in univariate analysis, with an increase of approximately 0.001 units per year (P < 0.05). This suggests that age may influence iris smoothness, potentially due to physiological aging processes such as age-associated miosis or iris atrophy17. However, this association was not significant in multivariate analysis (P = 0.122) after adjusting for confounders such as pupil status, sex, and iris thickness, possibly due to the influence of these covariates or limited statistical power. Given the absence of ocular pathologies (uveitis, glaucoma, dystrophy, masses) and prior interventions (laser treatment, intraocular surgery) in our subjects, the age-related trend observed in the univariate analysis warrants further investigation. To the best of our knowledge, there are currently no published studies that have directly examined the relationship between age and the SI. This highlights the novelty of our findings and underscores the need for future research with larger sample sizes to confirm the age-SI relationship and explore its clinical significance in detecting early iris changes. Investigating whether this trend is consistent across populations, and whether it holds diagnostic significance in early detection of iris atrophy or other age-related changes, would be particularly valuable.
While no significant overall association was found between sex and average SI, the analysis revealed statistically significant differences between males and females for specific axes. This observation highlights the potential for subtle sex-related variations in SI distribution that require further exploration.
Pupil status emerged as a crucial determinant of SI. The study unequivocally demonstrated that SI values were significantly higher in undilated pupils compared to dilated pupils. This finding is consistent with the SI calculation method, which involves dividing the baseline by a constant actual line. In the non-dilated state, the baseline (numerator) increases, leading to a higher SI value. This relationship remained significant even after controlling for age and gender in multivariate analysis. This finding underscores the importance of standardized pupil conditions when performing SI measurements and emphasizes the need for careful consideration of pupil status in clinical applications.
A noteworthy finding was the observed asymmetry in SI between the left and right eyes. In the right eye, SI1 values generally predominated, whereas in the left eye, SI2 values tended to be higher. It is important to note that both SI1 in the right eye and SI2 in the left eye correspond to the temporal hemi-meridians. There appears to be a symmetrical relationship between the two eyes in terms of iris smoothness, consistent with other previously examined interocular parameters21. This symmetry warrants further investigation to determine its clinical significance and potential underlying causes.
Observations of both eyes at 3 o’clock, 6 o’clock, and 12 o’clock revealed a smoother iris among the normal population. This finding may be significant for the examination of different iris pathologies in these specific regions, potentially aiding in the reduction of false positive outcomes.
A significant limitation of our research is the homogeneity of the participants’ ethnicity as they were all Iranian. Given the variability of iris parameters among various populations and ethnicities22,23,24, it is anticipated that the normal range of iris smoothness will also exhibit differences across these racial groups. Additionally, all participants in this study had dark brown irides, which is typical of the studied population. Lighter eye colors, such as green or blue, were not represented. Therefore, the potential influence of iris pigmentation on SI could not be evaluated. Further investigations comparing SI across diverse eye colors may help determine whether pigmentation-related anatomical differences contribute to variations in iris surface smoothness. Also, the relatively small sample size may have limited the statistical power to detect subtle effects. Additionally, the study did not investigate the impact of potential confounding factors, such as refractive errors, on SI measurements.
As the aim of this study was to establish a normative reference for SI in a healthy population, it is important to place these findings within a clinical context. Previous research has demonstrated higher SI values in pathological conditions. For instance, in a study on Fuchs uveitis, the mean SI in unaffected fellow eyes was reported as 0.841 ± 0.041, which is comparable to our population’s value of 0.812 ± 0.036. However, affected eyes exhibited a significantly higher SI of 0.876 ± 0.030, suggesting increased iris smoothness as a pathological marker. Similarly, another study investigating rubella and CMV-related uveitis reported a mean SI of 0.87 ± 0.04 in healthy controls, slightly higher than that of our cohort. These comparisons reinforce the potential utility of SI as a non-invasive, quantitative biomarker capable of distinguishing between normal and pathological iris conditions. They also underscore the importance of building robust normative databases across different populations and iris characteristics to enable accurate interpretation of clinical deviations10,14.
Future research should focus not only on confirming the age-related findings of this study but also on identifying whether SI can serve as an early biomarker for degenerative or age-related iris changes. Further studies with larger sample sizes are needed to confirm and further investigate the observed asymmetry in SI between the left and right eyes. Additionally, exploring the potential clinical applications of SI measurements in diagnosing and monitoring various ocular conditions is warranted.
The current research may serve as a foundation for subsequent investigations across various ethnic groups and in relation to different diseases affecting the iris. In addition, these data can provide a framework for future investigations that incorporate artificial intelligence.
In conclusion, this study highlights the SI pattern of normal iris in Iranians, which can be used for comparison in future research on iris pathologies. These findings are to be confirmed in a larger and more heterogeneous population. Notably, the study identified a positive correlation between age and SI, with the index increasing by approximately 0.001 units per year. This quantitative observation may reflect physiological aging processes and suggests the potential utility of SI as a non-invasive marker for early iris changes.
Data availability
Data is available from the corresponding author on reasonable request.
References
Izatt, J. A. et al. Micrometer-scale resolution imaging of the anterior eye in vivo with optical coherence tomography. Arch. Ophthalmol. 112(12), 1584–1589 (1994).
Ramos, J. L. B., Li, Y. & Huang, D. Clinical and research applications of anterior segment optical coherence tomography—a review. Clin. Exp. Ophthalmol. 37(1), 81–89 (2009).
Marin, Y. F. G. et al. Anterior segment optical coherence tomography (AS-OCT) image analysis methods and applications: A systematic review. Comput. Biol. Med. 146, 105471 (2022).
Wang, B. et al. Quantitative Iris parameters and association with narrow angles. Ophthalmology 117(1), 11–17 (2010).
Topcu, H. et al. Comparison of corneal, endothelial, and anterior segment parameters in eyes with and without pigment dispersion. Photodiagn. Photodyn. Ther. 40, 103161 (2022).
Ozer, M. D. et al. Vivo analysis and comparison of anterior segment structures of both eyes in unilateral herpetic anterior uveitis. Ocul. Immunol. Inflamm. 29(7–8), 1438–1444 (2021).
Basarir, B. et al. Analysis of Iris structure and iridocorneal angle parameters with anterior segment optical coherence tomography in fuchs’ uveitis syndrome. Int. Ophthalmol. 33, 245–250 (2013).
Invernizzi, A. et al. In vivo analysis of the Iris thickness by spectral domain optical coherence tomography. Br. J. Ophthalmol. 98(9), 1245–1249 (2014).
Ozer, M. D. et al. In vivo analysis and comparison of anterior segment structures of both eyes in unilateral fuchs’ uveitis syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol. 257, 1489–1498 (2019).
Zarei, M. et al. Quantitative analysis of the iris surface smoothness by spectral domain optical coherence tomography in Fuchs uveitis. medRxiv, : p. 2020.05. 06.20093302. (2020).
Zarei, M. et al. Quantitative analysis of the Iris surface smoothness by anterior segment optical coherence tomography in Fuchs uveitis. Ocul. Immunol. Inflamm. 30(3), 697–702 (2022).
Zhang, Z. et al. Investigation of 3D Iris morphology early alteration after implantable collamer lens implantation by using SS-OCT. Heliyon, 11(1) (2025).
López, P. E. & Guijarro, J. J. G. Comparative analysis of iridian anterior segment OCT and microbiological features in Fuchs Uveitis Syndrome and Posner-Schlossman Syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol.
Escribano Lopez, P. & Gonzalez, J. J. Guijarro Iridian anterior segment OCT in rubella uveitis syndrome and cytomegalovirus anterior uveitis: A comparative study. Graefe’s Arch. Clin. Exp. Ophthalmol. 260(11), 3647–3655 (2022).
Huang, W. et al. Anterior and posterior ocular biometry in healthy Chinese subjects: Data based on AS-OCT and SS-OCT. PLoS One 10(3), e0121740 (2015).
Xu, B. Y. et al. Ocular biometric determinants of anterior chamber angle width in Chinese Americans: The Chinese American eye study. Am. J. Ophthalmol. 220, 19–26 (2020).
Tun, T. A. et al. Association of Iris surface features with Iris parameters assessed by swept-source optical coherence tomography in Asian eyes. Br. J. Ophthalmol. 100(12), 1682–1685 (2016).
Cai, Y. et al. Anterior segment structures in dark Iris Chinese patients with unilateral fuchs’ uveitis syndrome. Int. Ophthalmol. 42(9), 2939–2947 (2022).
Zarei, M., Ebrahimiadib, N. & Riazi-Esfahani, H. Using anterior segment optical coherence tomography to compare the smoothness of anterior Iris surface between two eyes in unilateral fuchs’ uveitis syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol. 257, 2799–2800 (2019).
Escribano López, P. & González, J. J. Guijarro Comparative analysis of iridian anterior segment OCT and microbiological features in Fuchs Uveitis Syndrome and Posner-Schlossman Syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol. 1–11 (2025).
Li, Y. & Bao, F. J. Interocular symmetry analysis of bilateral eyes. J. Med. Eng. Technol. 38(4), 179–187 (2014).
Sng, C. C. et al. Associations of Iris structural measurements in a Chinese population: The Singapore Chinese eye study. Investig. Ophthalmol. Vis. Sci. 54(4), 2829–2835 (2013).
Wang, D. et al. Differences in Iris structural measurements among American caucasians, American Chinese and Mainland Chinese. Clin. Exp. Ophthalmol. 40(2), 162–169 (2012).
Lee, R. Y. et al. Differences in Iris thickness among African Americans, Caucasian Americans, Hispanic Americans, Chinese americans, and Filipino-Americans. J. Glaucoma 22(9), 673–678 (2013).
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
H.F. and M.Z. conceptualized and designed the study, collected the data, and drafted the initial manuscript. T.M. and S.N. performed data analysis and contributed to data interpretation. D.A. and M.K assisted in data gathering and data entry. E.K.P. and M.Z. supervised the project, provided critical revision of the manuscript, and served as corresponding authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This manuscript adheres to the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardian(s) prior to participation in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fakhredin, H., Mahmoudi, T., Nohasfarmaniyeh, S. et al. Quantitative analysis of iris surface smoothness in normal population. Sci Rep 15, 28603 (2025). https://doi.org/10.1038/s41598-025-13964-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-13964-7