Abstract
The monolayer of approximately 300,000 human corneal endothelial cells (hCECs) on the posterior surface of the cornea is essential to maintain transparency but is non-self-regenerative. Corneal blindness can currently only be treated by corneal transplantation, hindered by a global donor shortage, highlighting the need for developing tissue and/or cell therapy. The mass production of these advanced therapy medicinal products requires obtaining high-yield, high-quality endothelial cell cultures characterized by hexagonal shape, low size variability, and high endothelial cell density (ECD). Among the usual critical quality attributes which combine the expression of differentiation markers, ECD and cell morphological parameters, the latter are not optimally measured in vitro by conventional image analysis which poorly recognizes adherent cultured cells. We developed a high-performance automated segmentation using Cellpose algorithm and an original analysis method, improving the calculation of classical morphological parameters (coefficient of variation of cell area and hexagonality) and introducing new parameters specific to hCECs culture in vitro. Considering the importance of the extracellular matrix in vivo, and the panel of molecules available for coating cell culture plastics, we used these new tools to perform a comprehensive comparison of 13 molecules (laminins and collagens). We demonstrated their ability to discriminate subtle differences between cultures.
Similar content being viewed by others
Introduction
Human Corneal Endothelial Cells (hCECs) form a monolayer of hexagonal cells at the inner part of the cornea, resting on the Descemet’s membrane (DM). They have a crucial barrier and ion pump functions, ensuring deswelling of the hydrophilic stroma. This function is essential for maintaining corneal thickness and transparency. Corneal endothelial dysfunction is the major cause of corneal low vision worldwide1,2. The only treatment for these diseases is corneal transplantation with around 185,000 keratoplasties per year worldwide. However, the global chronic and severe shortage of donors highlights the importance of developing alternative solutions3. Cell therapy is now a reality in Japan, where it has been approved by health authorities, and may soon be in the United States of America. Complementary approaches, such as tissue engineering, could also be useful to meet this growing demand4,5,6. For both advanced therapy medicinal products (ATMPs), the production of high-quality clinical grade hCECs in vitro (small, hexagonal and cohesive) is essential and particularly challenging because of the low regenerative capacity already mentioned7. So far, all clinical-grade hCECs cultures have been exclusively performed using donors under the age of 35, as their cells are more numerous and exhibit significantly higher proliferative capacities compared to older donors8,9,10. However, these young donors are extremely rare due to a very high refusal rate for pediatric donations, and the (fortunately) low mortality among young adults.
A persistent challenge is therefore to establish high-yield cultures of hCECs sourced from older donors using innovative methods to increase hCECs density in vitro while avoiding phenotypic changes such as endothelial mesenchymal transition (EndoMT)11,12,13,14. In EndoMT, cells lose their hexagonal shape and intercellular junctions, increase their production of extracellular matrix (ECM), change their gene expression and, hypothetically, their functionality (such as pump function), although this aspect is rarely investigated in most research studies. To obtain an optimal cell culture, two parameters can be improved: the culture medium and the molecular coating of culture plastics, which enhances cell adherence and differentiation. The present study is focused on molecular coating.
The three main coating proteins used in hCECs culture are collagens, fibronectin and laminins15,16. In Japan, the Laminin-511 E8 protein fragment has been selected as an ideal xeno-free defined substrate to produce clinical-grade hCECs. For evaluating hCECs quality in adherent culture conditions, morphometric analysis has multiple advantages. The monolayer arrangement facilitates imaging, allowing for clearer observation and analysis of cellular characteristics. These culture conditions closely mimic the native tissue environment, providing a better simulation of the physiological conditions of hCECs. Therefore, in vitro cell morphology might be a good predictor of what will be observed in the recipient of ATMPs. In addition, it will likely be challenging to gain approval from health authorities for clinical batch release criteria if the cultured cells do not sufficiently resemble native corneal endothelium, as morphological conformity is expected to be a key indicator of the viability and effectiveness of cells prepared for transplantation.
Understanding cell morphology in adherent culture conditions, particularly in response to different coating molecules, could provide new insights for optimizing cell selection and improving transplantation outcomes. We hypothesize that in primary culture, a characterization based on cell morphology could potentially be used to select high-quality cells, particularly when using donors over the age of 30, who are significantly more frequent but whose hCECs are fewer in number, less proliferative and more prone to EndoMT.
In the present study, we performed a screening of several laminins and collagens to optimize hCECs quality and maximize the culture yield. Morphometry and ECD were quantified using an artificial intelligence (AI) driven segmentation tool, specifically designed, trained and tuned for hCECs analysis and initially validated on cultures with defined phenotypes.
Materials and methods
Donor tissue and ethical statement
hCECs used in this study were obtained from primary cell cultures derived from organ-cultured human corneas. They were sourced from corneal donations for scientific purposes (Laboratory of Anatomy of the Faculty of Medicine of Saint-Étienne) or from three French eye banks (Besançon, Saint-Étienne, and Nantes). All corneas were unsuitable for transplantation because their parameters did not meet the required standards for clinical use. All experimental protocols were approved by a designated institutional and/or licensing committee and informed consent were obtained from all subjects and/or their legal guardian(s). The BiiO laboratory, authorized by the Ministry of Higher Education, Research, and Innovation of France (Ministère de l’Enseignement Supérieur, de la Recherche et de l’Innovation, MESRI) under the number DC-2023-5458, conducted this research on these human corneas without the need for additional ethical approval. They were handled in accordance with the principles of the Declaration of Helsinki, bioethics laws, and French and European regulations regarding tissue donations.
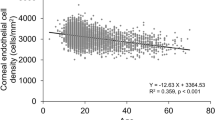
For AI fine-tuning, we used 15 immunofluorescence-labeled images from 3 different cultures (see and S13 and data in the supplementary section). For AI segmentation and criteria validation, we used 4 other different endothelial cell cultures (listed in Table 1) which had varying quality, ranging from a culture undergoing endothelial-mesenchymal transition to an endothelial culture from a very young donor (2 years old, characterized by high ECD and excellent morphology). For the comparison of coating molecules, eight cultures from eight donors were used. The donors ages ranged from 55 to 85 years, with a mean ± standard deviation of 71 ± 11 years (sex ratio = 1 (4 males, 4 females)) and corneas were stored at 31 °C in organ culture medium (CorneaMax, Eurobio, Les Ulis, France) during 25 ± 22 days (min = 4; max = 72) before use. The initial ECD, measured within 5 days after retrieval, was 2390 ± 559 (1287–3233) cells/mm2. Donors and cultures characteristics were detailed in Table 1.
Cell culture media
Three different media were used: 1/The DM digestion medium consisted of Opti-MEM (11058021, Gibco, Grand Island, NY, USA) supplemented with 200 µg/mL CaCl2 (C5670, Sigma-Aldrich, St. Louis, MO, USA); 20 µg/mL ascorbic acid (A5960, Sigma-Aldrich) and 2 mg/mL collagenase A (10103586001, Roche, Basel, Switzerland). 2/The basic medium consisted of Opti-MEM supplemented with antibiotic–antimycotic (152 − 062, Gibco) at 1/200, 8% of fetal bovine serum (S-1860-500, Eurobio), 0.1% of CaCl2, 0.08% of chondroitin sulfate (034-1462, FUJIFILM Wako Pure Chemical Corporation, San Diego, CA, USA), 10 µM of SB203580 (3.8 µg/mL) (S1076, SelleckChem, Houston, TX, USA) and 1 µM of SB431542 (S1067, SelleckChem) (where SB203580 was an inhibitor of the p38 MAPK pathway and SB431542 an inhibitor of the TGF-β receptor; both involved in the limitation of EndoMT in cell culture), 20 µg/mL of ascorbic acid and 5ng/mL of Epidermal Growth Factor (EGF) (PHG0311, Gibco, Grand Island, NY, USA). 3/The medium for the initiation of primary cell culture and for cell passaging was the basic medium with the addition of a ROCK inhibitor (RI), Y-27,632 (S1049, SelleckChem) to promote cell adherence, proliferation and survival17,18,19.
Primary culture of hCECs
hCECs were cultivated using a protocol derived from the standard peel and digest method, also used by the team which selected the coating with iMatrix-511 (892012, Nippi, Incorporated, Tokyo, Japan)20. We increased the digestion time from 12 to 16 h and used a higher collagenase concentration (from 1 mg/mL to 2 mg/mL) to enhance cell dissociation, as previously described21. To isolate hCECs, DM was mechanically peeled from donor corneas, ensuring maximum peripheral coverage. The membranes were then incubated at 37 °C in a humidified 5% CO₂ atmosphere for 16 h with 0.5 mL of digestion medium in 48-well plates (3548, Corning, Kennebunk, ME, USA). After digestion, released hCECs were centrifuged at 200 g for 5 min in conical-bottom tubes (641997, Dutscher, Caplugs Evergreen, CA, USA). The cells were then seeded in 24-well plates (3524, Corning) pre-coated with iMatrix-511 according to the manufacturer’s instructions. hCECs were cultured in a humidified 5% CO2 atmosphere at 37 °C. The basic medium was changed the day after seeding and then weekly until confluence, which took about a month.
For cell passage, hCECs cultures were first rinsed in Ca2+ and Mg2+-free phosphate buffered saline (PBS) (SH30256.02, Cytiva, MA, USA), then incubated in TrypLE Select Enzyme 5X (A1217701, Gibco) for 15 min at 37 °C until cell detachment. Cells were detached mechanically by aspirating and dispensing the liquid in the well and chemically using TrypLE solution. Cells were then transferred in conical-bottom tubes containing basic medium supplemented with RI. The complete detachment of cells was confirmed using a phase-contrast microscope (CKX41, Olympus, Tokyo, Japan). Viable cells were counted using Trypan blue staining and an automatic cell counter (TC10, Bio-Rad, Hercules, CA, USA). Counting was performed twice to ensure repeatability and to calculate the average cell number. Passage followed a defined scaling ratio: P1 (1 well of a 24-well plate into 1 well of a 12-well plate), and P2 (1 well of a 12-well plate into 1 well of a 6-well plate), with subsequent passages at a 1:2 ratio. Throughout all stages, cells used for experiments were cultured on plates coated with the reference molecule, iMatrix-511 until experiment with the different molecular coatings. Cultured hCECs at passages 4 through 9 were used for these experiments. After the last cell counting, hCECs were centrifuged at 200 g for 5 min. The supernatant was removed and hCECs were resuspended in the medium previously described and seeded, this time, at 500 cells/mm² in 384-well plates (353961, Falcon, MA, USA) for experiments with the different molecular coatings.
To validate our AI image analysis method, we selected four cultures with very different phenotypes based on conventional naked-eye microscopy observations, representative of the various endothelial qualities, ranging from the poorest (non-transplantable) to the best (the desired goal, i.e. deemed suitable for clinical application), as illustrated in Fig. 1. Culture 1 underwent EndoMT. Culture 2 was typical of a double population of normal and likely senescent cells. Culture 3 and 4 both were clinically acceptable compared to the initial clinical trial9. For this step, each of the 4 cultures was cultured on plates coated with iMatrix-511 (the reference coating) in 384 wells with 16 replicates per culture.
In a second step, we used this validated AI image analysis method to evaluate 13 coating molecules on 8 different cultures. The diversity of the parameters involved, particularly the inter-donor variability and the variability associated with the coating molecules, made it impossible to subjectively discriminate by the naked eye, which justified the use of an automated analysis method. The 8 cultures were selected based on their ECD higher than 1000 cells/mm². This rather low threshold (by reference to the usual eye bank lower threshold of 2000 cells/mm2 for transplantation) was chosen because the aim of this work was to screen for conditions likely to increase final ECD.
For the screening of molecular coating, for each coating condition tested, 8 replicates were performed for each of the 8 different corneal donors (1 coating molecule, 1 donor, 8 repetitions). We selected 9 laminin isoforms (all from BioLamina, Sundbyberg, Sweden) as well as iMatrix-511 (Nippi) and 3 types of collagens (all from Sigma Aldrich) (Table 2). Laminins differed in their chain composition, tissue localization, and biological functions, making them of interest for specific applications in regenerative medicine and tissue engineering. These 13 molecules were compared to a negative control (uncoated well). The coating with the ten laminin molecules, including the control, was performed overnight at 4 °C, as recommended by the supplier, with all at 1 µg/cm² except for iMatrix-511, which was coated at 0.5 µg/cm². For the three collagen molecules, incubation time was done at 37 °C until complete drying of the well. Collagens I and IV were performed at 6 µg/cm² and collagen II at 2 µg/cm².
Immunocytochemistry
At confluence, after approximately 3 weeks of culture, immunocytochemistry (ICC) was performed on hCECs directly in culture plates. The ICC protocol was previously described21,33. Briefly, cells were rinsed in Ca2+ and Mg2+ DPBS (SH30028.FS, Cytiva, Saint-Germain-en-Laye, France) and then fixed in pure methanol for 15 min at room temperature (RT). After three rinses, with Ca2+ and Mg2+ DPBS, cells were incubated in saturation buffer composed of 2% bovine serum albumin (A3059-100G, Sigma-Aldrich) and 2% goat serum (191356, MP Biomedicals, Irvine, CA, USA) for 30 min at 37 °C. The hCECs were incubated with the primary antibody for 1 h at 37˚C: NCAM (1:400, MAB24081, R&D Systems, Minneapolis, MN, USA). After three rinses in PBS, the highly cross-absorbed secondary antibodies (Alexa Fluor 488-conjugated goat anti-rabbit IgG (A11034, Invitrogen, Carlsbad, CA, USA)), diluted to 1/800, and DAPI diluted at 2 µg/mL in blocking buffer were incubated for one hour at 37 °C under gentle agitation. After rinsing three times, Fluoromount-G mounting medium (00-4958-02, Invitrogen) was added to each well.
Images acquisition
The samples were observed with an inverted fluorescence microscope IX81 (Olympus), equipped with CellSens Dimension software V2.3 (Olympus). Images were taken at x10 and x40 magnification at the center of each well. Images were obtained using a FITC and DAPI filters, using optimized parameters for each image (intensity of light source, exposure time, contrast, resolution) and a CMOS camera with 2024 × 2048 pixels resolution (Orcas-Flash4.0 LT+, C11440-42U30, Hamamatsu Photonics K.K., Hamamatsu city, Japan).
Endothelial cell density measurement
After staining, 8 replicate images per molecular coating were taken for each donor, to measure ECD. For this, we automated the counting of each cell nucleus (DAPI-stained) with a macro using the “Stardist” plugin (https://github.com/stardist/stardist) on Fiji Software (V2.9.0/1.53t https://fiji.sc/) using x10 magnification images34,35. The software segmented each stained nucleus and calculated the ECD according to the pixel ratio. We performed a visual inspection to ensure proper nuclear recognition and corrected any possible errors.
Cellular segmentation and morphological analysis using AI and mathematical algorithms
To characterize hCECs morphology, we developed a high-performance AI-based automatic segmentation and analysis solution for cells labeled with a lateral membrane marker (here NCAM) and a nucleus marker (DAPI). For morphological analysis, 2 images were taken per molecular coating and for each donor.
Segmentation using AI
We used Cellpose, an open-source generalist deep learning algorithm for cell and nucleus segmentation (https://github.com/MouseLand/cellpose) that can be tuned for optimizing results with the users’ data (Fig. 1)36. We selected the cyto3 model because of its versatility and better efficacy than other available pretrained models37. We first verified if it was efficient with our images. We then tuned the “cyto3” Cellpose model with hCECs images labeled with NCAM and DAPI (Model in supplementary section). We manually segmented 15 images of different cell culture quality directly on the Cellpose Graphical User Interface (GUI) which allowed the extraction of the result of the segmentation on a separate image as well as the regions of interest (ROI) of each image (S13 and data in supplementary section). Manual segmentation took approximately 4–8 h per image, depending on image complexity and ECD.
We then performed a 4-fold cross-validation on the Python version of Cellpose based on the 15 manually segmented images (2048 × 2048 pixel for 1330 × 1330 μm, 16 bits) coupled with the fluorescence images (membranes and nuclei in two different image channels). Data were divided into 60% training set, 20% test set and 20% validation set, data augmentation was performed with a factor of 4 by horizontally and vertically flipping images. As there were approximately 1500 cells per image, the training set was thus constituted of around 54,000 cells. For each fold, we optimized epochs (number of training cycles the AI went through to learn/correct the weights of the model) using the validation set (800 was the best epochs per fold). Cross-validation was done by comparing manually segmented images with Cellpose segmentation using a published dissimilarity criterion and the 6 parameters described hereafter : Endothelial Cell Density (ECD), Coefficient of variation of cell area (CV), Adjusted CV, hexagonality (HEX), quality of HEX (HEX-Q) and Filimorphism38.
Cell segmentation and AI training steps using Cellpose. (A) Steps for image segmentation with Cellpose which used an U-net model pre-trained on different cell types (Cyto3 model). The initial segmentation was not efficient on NCAM-labeled cultured corneal endothelial cells. Cell areas were coded by colors. (B) Steps for training a new model consisted in the selection of NCAM-labeled image of various quality (n = 15 images), followed by manual labeling and then a 4-fold cross validation training to optimize epochs and control segmentation quality of the newly trained model (tuned model). (C) Comparison of the same image segmented with the pre-trained Cyto3 model and with our tuned model. Scale bar = 500 μm on each image.
Morphometric analysis
We developed a custom script in Python language (V3.11.4, https://www.python.org/downloads/release/python-3114/), interpreted with Spyder IDE (V5.4.3) to measure 5 parameters on segmented images and to conduct a comprehensive analysis of cell polymegathism and pleomorphism (Fig. 2):
1/ CV of cell area: the conventional parameter for polymegathism already mentioned. The lower the value, the more homogeneous the mosaic. It was calculated by the formula \(\:{CV}_{area}=\frac{{SD}_{area}}{{Mean}_{area}}\). The CV of a healthy endothelium ranged from 26 to 35%, depending on the patient’s age39,40,41,42,43; 2/ Adjusted CV was specifically designed for this study to assess cell cultures containing several cell populations in terms of area. This adjusted CV allowed studying the CV of the majority population within the culture by replacing the mean with the median and the standard deviation with one calculated from median absolute deviation (see Supplementary methods); 3/ HEX for polymorphism. The HEX of a healthy endothelium ranged from 45 to 70% depending on the patient’s age39,40,41,42,43; 4/ Quality of hexagonality (HEX-Q) was also specifically designed for this study: among hexagonal cells (with 6 neighbors), it measured their proximity to a perfect hexagon based on the HEXADEV criterion44. HEX-Q calculation took into account the convexity of the cell as well as the length of the sides and the angle of each side of the hexagonal cell (see Supplementary methods); 5/ Filimorphism: this parameter, specifically designed for this study assessed cell elongation by modifying the aspect ratio formula (depending on definitions, aspect ratio in the literature is calculated either 1- as the ratio between the length of the major axis and the minor axis of the cell’s fitting ellipse or 2- as the ratio between the maximal and minimal Feret diameter of a cell) adapting it even for extremely concave (U-shaped) cells (see Supplementary methods).
Establishment of endothelial quality score
To comprehensively evaluate the different parameters, a score was established, hereafter referred to as the Endothelial Quality Score (EQS). This scoring system assigned 50% weight to ECD, as it is the primary criterion used in clinical practice (eye banking), and 50% to morphology, considering that both were equally important. Morphology evaluation was based on the five parameters previously described: HEX, HEX-Q, CV, adjusted CV and filimorphism, each contributing 1/10 of the EQS. The EQS was derived from Z-scores, which were calculated by the following formula: \(\:{Z}_{i}=\:\frac{{X}_{i}-\mu\:}{\sigma\:}\:\); where \(\:{Z}_{i}\) was the score value, Xi the raw value, µ the population mean for the given criterion, and σ the standard deviation of the referred population. The higher the EQS, the better the endothelial quality.
Statistical analysis
To analyze the results of the algorithm using the AI model, the GraphPad Prism software was used. Initially, the normality of each culture for each parameter was tested using three different tests (Kolmogorov-Smirnov test, Agostino and Pearson omnibus normality test, and Shapiro-Wilk normality test). If one of these three tests indicated normality for the four cultures, a repeated Measures ANOVA followed by Bonferroni’s multiple comparison test was performed as a post-hoc analysis. If none of the normality tests showed a normal distribution, a Friedman test was used, followed by Dunn’s multiple comparison post-hoc test.
To evaluate the relationship between coating molecules and ECD or morphology, a linear mixed-effect model was used. ECD values and other positive criteria were log-transformed before the mixed effect analysis. This model accounted for both fixed effects, such as factors of interest (coating molecule), and random effects (donor, replicate ID), to account for inter-individual variations and correlations between observations. Statistical analyses were performed using R software (version 4.4.1), with the “lme4” and “lmerTest” packages to fit a linear mixed-effects model. Results were expressed as the ratios of the ECD effect relative to the reference molecule with the corresponding 95% confidence intervals.
Results
Efficiency validation of the morphological analysis
For the 4 cultures selected for validation, the 6 parameters successfully differentiated them as anticipated (Fig. 3). Culture 1 (EndoMT) had a low ECD with very low hexagonality and resembled fibroblasts, with high polymegathism. Culture 2 (double population) had an acceptable hexagonal pattern (HEX-Q) but significant pleomorphism (high CV and high filimorphism). For the last two cultures: culture 3 had a high ECD and low polymegathism; however, it exhibited higher pleomorphism than culture 4. Culture 4 had a slightly lower ECD, but this pleomorphism was minimal (HEX, HEX-Q, filimorphism).
The EQS significantly discriminated the two cultures with a good phenotype by assigning a significantly higher EQS to the culture with the highest ECD (culture 3), despite having slightly higher pleomorphism (Fig. 4). In contrast, the first two cultures were not significantly different. However, these two cultures appeared visually different with NCAM staining, with a complete absence of hexagonal shaped cells resembling hCECs in culture 1. In culture 2, some cells exhibited a hexagonal shape similar to those observed in cultures 3 and 4.
Validation of the AI-based method for quantifying the various hCECs morphological parameters. (A) Endothelial cell cultures of highly variable quality used for AI algorithm validation. Cell lateral membranes were labeled with anti-NCAM (in green) and the nuclei were counterstained using DAPI (in blue). The images were taken in the center of each well at x10 magnification with a zoom x6 in the center of the image. Image scale bar = 300 μm, zoom scale bar = 50 μm. (B) Evaluation of 6 parameters across 4 different culture qualities. Graph illustrating 6 objective evaluation parameters across 4 culture qualities: (1) EndoMT cells at passage 7; (2) Mixed population quality at passage 5; (3) High quality – young donor (below 30 yo) at passage 4; (4) High quality – aged donor (over 30 yo), at passage 11. ns = non-significant = p-value > 0.05, *p-value < 0.05, **p-value < 0.01, ***p-value < 0.001.
Endothelial quality score (EQS) for evaluating cell culture quality based on morphological and ECD criteria. EQS was calculated from the z-score of each of the 6 chosen parameters (ECD, Hexagonality, Quality of Hexagonality, CV, Adjusted CV, Filimorphism). Graph illustrating 6 objective evaluation parameters across 4 culture qualities: (1) EndoMT cells at passage 7; (2) Mixed population quality at passage 5; (3) High quality – young donor (below 30 yo) at passage 4; (4) High quality – aged donor (over 30 yo), at passage 11. *=p-value < 0.05, **=p-value < 0.01, ***=p-value < 0.001).
Coating and donor impact on morphological and density parameters
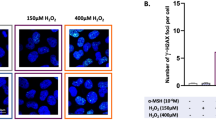
Cell cultures from the 8 donors exhibited highly variable quality (Fig. S12 in the supplementary data), which complicates the interpretation of coating effects using visual inspection and conventional statistical methods. An automated analysis system would greatly simplify and accelerate this evaluation. The mixed model allowed us to assess their impact while considering multiple variables, including both intrinsic and extrinsic donor-related factors. An example of cell response to the different coatings was shown in Fig. 5. For ECD, no molecule had a significantly lower value compared to the uncoated control, while eight molecules exhibited significantly better results (Fig. 6A). For iMatrix-511, although ECD was not significantly higher than in the uncoated control, it demonstrated reduced cell size variability (adjusted CV), fewer filiform cells, and a higher proportion of cells appeared hexagonal in shape (HEX-Q). Only HEX did not allow for differentiating the different coating molecules. On the contrary, HEX-Q was able to discriminate between cultures (for instance, B121, B332, and iMatrix-511 had higher HEX-Q than the control) (Fig. 6B).
EQS differentiated the efficacy of coating molecules on cell culture quality. Only B332 did not have a significantly better EQS than the uncoated control, while all other coating molecules showed an improved one. The coating that achieved the highest score was collagen IV (Col IV). iMatrix-511 also improved cellular quality, but to a lesser extent (Fig. 6C).
Representative example of the effects of coating molecules on hCECs cultured in vitro. Molecular names were expressed on the top left of each image. Images were taken in the center of each well at x40 magnification. The control represented a well without coating. Cell lateral membranes were stained with anti-NCAM (green) and the nuclei were counterstained using DAPI (blue). The donor used for this example was “c” in Table 1. Scale bars are placed in the bottom-right images of columns IV and CTRL (100 μm).
Summary of the mixed model analysis for coating molecules. (A) The table presented the ratio, p-value, and confidence interval, highlighting significant differences between the tested coating molecules and the control. The color scale indicates the level of significance, with darker green representing higher significance and lighter green representing lower significance. (B) Forest plot of molecule expression ratios according to the evaluated criterion. This forest plot illustrated the expression ratios of different coating molecules based on the evaluated criterion. Each point represents the mean ratio value, while the vertical bars indicate the corresponding confidence intervals (lower and upper bounds). The vertical line at y = 1 served as the reference value compared to the uncoated control. A ratio greater than 1 suggested superiority compared to the control, whereas a ratio lower than 1 indicated inferiority compared to the control. If the ratio of the parameters ECD, Hexagonality, and HEX-Q is greater than that of the control, the culture quality is better (green zone); otherwise, it is worse (red zone). If the ratio of the parameters CV, Adjusted CV, and Filimorphism is greater than that of the control, the culture quality is worse (red zone); otherwise, it is better (green zone). (C) Forest plot of molecule expression ratios (compared to the uncoated control) according to the endothelial quality score (EQS) (including all 6 evaluations parameters). Each point represented the mean ratio value, while the horizontal bars indicated the corresponding confidence intervals (lower and upper bounds).
Discussion
Corneal endothelial diseases are the leading indication for corneal transplantation worldwide. Two ATMPs are or will soon be able to compensate for the shortage of donors: cell therapy (available in Japan), and tissue therapy (in development)45,46. To ensure their large-scale production, both techniques require the culture of clinical grade hCECs, that is with the correct phenotype and obtained in large quantities according to pharmaceutical standards.
To draw a parallel with donor corneas, ECD is the main release criterion by corneal banks, and the decision threshold varies depending on the surgical technique considered. The threshold of 2000 cells/mm² is consensual for penetrating grafts, and a higher value is required for endothelial grafts, as the surgery itself causes additional cell loss. Some banks add criteria for cell mortality, but these are not consensual. There are two historical morphometric parameters, used for 50 years to qualify the endothelium in vivo in patients and ex vivo in eye banks: the percentage of hexagonal cells (HEX) to evaluate polymorphism, and the coefficient of variation of cell surface (CV) for pleomorphism. HEX and CV are provided by eye banks but rarely serve as non-compliance criteria due to a lack of data on their postoperative impact47. Until recently, they were not used for the selection of in vitro cell cultures. Okumura et al. developed software called the Corneal Endothelial Cell Analyzer to assess the transformation of hCECs into fibroblasts, based on cell density, percentage of hexagonal cells (HEX), and the variation coefficient based on the aspect ratio (ratio of height to width). This software follows four processing steps: (1) noise reduction, (2) contour enhancement, (3) binarization, and (4) skeletonization31.
Cellpose is an open-source software for segmenting cells in culture. Pre-trained models available did not correspond to our needs, but the tuning of our own model was very efficient. The dissimilarity criterion c, evaluated with a tolerance margin of 3 pixels (c = 0 in the ideal case and c > 1 for poor segmentation) was 0.034 ± 0.010 when the model segmentation was compared to the ideal manual segmentation38. Additionally, we proposed several metrics to refine the assessment of hCECs cultures, as morphometric analysis (limited to HEX and CV) was initially developed for in vivo specular microscopy images, where endothelial cells exhibit a more regular morphology than in vitro: 1/the adjusted CV is more suitable than CV in the context of cultured hCEC likely to contain double or triple populations of normal, senescent and/or fibroblastic cells; 2/ HEX-Q is a sensitive criterion to evaluate the similarity of the cell contour to a regular hexagon; 3/ filimorphism, as a robust metric to study cell elongation. Further studies are now needed to establish a relationship between our proposed metrics (considered as new image biomarkers of cell quality) and conventional biological biomarkers (such as pump function, gene expression) already used in hCEC production. Several possibilities could be considered, such as the development of a robust imaging-based method for functional assessment (as Na+/K+ATPase labeling), potentially by adding a specific fluorescence channel or by correlating functionality with morphological features. Our team was also working on the development of non-imaging-based functional tests. These were to be implemented first in vitro, and eventually ex vivo using bioreactor models — which would have represented the gold standard of functional validation, although technically challenging given the large cohorts under investigation48,49,50,51.
To obtain a clinical-grade endothelial cell culture, several difficulties must be overcome. In some cultures, several different cell populations are observable, with varying phenotypes ranging from typical endothelial cells to senescent or even fibroblastic cells (undergoing an EndoMT)11,14,32,52. To approximate physiological conditions, the use of coating molecules on plastic culture plates is widely referenced16,20,23,25,28,30,32. The DM is composed of collagen types IV and VIII, laminin, fibronectin, and other extracellular matrix (ECM) proteins that provide structural support and influence cellular behavior28,53,54,55,56,57. These proteins play a critical role in regulating fundamental cellular processes such as cell adherence, proliferation, polarity, morphogenesis, and function, particularly the integrin/laminin complexes58. Okumura et al. identified 2 laminin isoforms present in DM and demonstrated their positive effect, as well as that of the recombinant E8 fragment of laminin 511, on endothelial culture yield, in comparison with laminin 211, fibronectin, collagen I, FNC Coating mix (Athena Environmental Sciences, Inc., Baltimore, MD, USA) and no coating. Morphometric parameters were not used for their selection, which was based on adhesion tests, proliferation and flow cytometric analysis of endothelial marker expression20,59.
In our screening study, we compared a wide range of coating molecules: 9 laminins and 3 collagens selected from the known composition of DM60,61. The use of NCAM labeling, employed for cell segmentation, relies on its ability to reveal lateral membrane expansions. Although ZO-1 is more commonly used, NCAM appears to be linked to activity and differentiation levels62,63. Our team had previously reported the use of NCAM as a reliable biomarker to assess EndoMT induction evidenced by changes in fluorescence intensity. This technique indicates a reduction in protein expression when fluorescence intensity declines. As a limitation, it is widely recognized that quantitative analyses using microscopy are influenced by numerous variables. To overcome this limitation, we developed the morphometric analysis presented in this article to automatically, robustly, and rapidly analyze a high number of cells.
Indeed, cultures 1 and 2 were challenging to statistically differentiate by our analysis, particularly because the cultures do not present hexagonal cells, giving two criteria with values close to zero and thus a score whose interpretation must be nuanced. The use of a segmentation based on two markers, one endothelial and one fibroblastic, could be interesting to complement the analysis and allow the discrimination of two cell populations in the same culture. In that case, the AI will need to be retrained on this other marker.
To allow a global interpretation, we grouped the 6 morphometric parameters and ECD into an endothelial quality score, giving equal weight to both the quantity and quality of the cells. This score, which allowed the discrimination of cultures that were not very different, could be used during the production of endothelial ATMPs and compared to other critical quality attributes. The weighting of each parameter depends on the results of future studies (preclinical and clinical) and can be adjusted if necessary.
One limitation of this work is the use of 384-well plates. Although these plates offer the advantage of minimizing cell consumption, they are associated with greater inter-well variability due to their small volume, which amplifies the effects of slight variations in the number of seeded cells. For culture qualification during production, larger surface areas will likely be more appropriate. Additionally, phase contrast imaging can be employed to analyze cell morphology in unfixed cells.
Given the scarcity of corneal endothelial cells, it’s important to maximize their amplification. Most research groups working on this subject use passage 2 or 3 cells, considering them suitable for clinical use and ensuring sufficient expansion while preserving the phenotype. Amplification is limited by the onset of the EndoMT phenomenon. To counteract this transition, we evaluated improvements in cell adhesion through various coating molecules. The feasibility of ex vivo expansion methods for clinical application depends not only on morphological quality but also on the capacity to obtain sufficient numbers of functional cells. While our study primarily focused on early morphological criteria, we acknowledge that parameters such as total yield and the proportion of high-quality cells are equally important. In this regard, the robustness of our results relies on the use of several cultures with significant variability (extreme ages, passage, quality, initial DCE) and statistical analysis through a mixed model.
Conclusions
In conclusion, we demonstrated that our morphological analysis tool allows the discrimination of quality variations between very similar cultures. We then used this tool to identify a coating molecule capable of improving the in vitro culture of hCECs. To account for all the parameters of cell quality, we developed a score that provides an overall assessment of the culture quality, highlighting that the coating has a positive effect on the cultures, regardless of the laminin used. Using a complex statistical model, we were able to identify coating molecules that show better morphology or density compared to the uncoated control. Collagen IV appears to be the best coating molecule for improving hCECs culture in this context and, based on this analysis, even superior than iMatrix-511.
Data availability
The database for training and AI model weights used during the current study are available on the supplementary section.
References
Liu, C., Gao, Z. Q., Li, J. & Zhou, Q. et « Identification of novel therapeutic targets for Fuchs’ endothelial corneal dystrophy based on gene bioinformatics analysis », PLOS ONE, vol. 17, no 3, p. e0264018, mars (2022). https://doi.org/10.1371/journal.pone.0264018
Chen, X., Xu, J. & Chen, X. Yao, « cataract: advances in surgery and whether surgery remains the only treatment in future ». Adv. Ophthalmol. Pract. Res. 1, 100008. https://doi.org/10.1016/j.aopr.2021.100008 (nov. 2021). no 1.
Gain, P. et al. « Global Survey of Corneal Transplantation and Eye Banking », JAMA Ophthalmol, vol. 134, no 2, pp. 167–173, févr. (2016). https://doi.org/10.1001/jamaophthalmol.2015.4776
Crouzet, E. et al. « Tissue engineered endothelial keratoplasty in rabbit: tips and tricks », Acta Ophthalmologica, vol. 100, no 6, pp. 690–699, (2022). https://doi.org/10.1111/aos.15081
Parekh, M. et al. « Biomaterials for corneal endothelial cell culture and tissue engineering », J Tissue Eng, vol. 12, p. 2041731421990536, janv. (2021). https://doi.org/10.1177/2041731421990536
Teichmann, J. et al. « Tissue Engineering of the Corneal Endothelium: A Review of Carrier Materials », Journal of Functional Biomaterials, vol. 4, no 4, Art. no 4, déc. (2013). https://doi.org/10.3390/jfb4040178
Wongvisavavit, R., Parekh, M., Ahmad, S. & Daniels, J. T. et « Challenges in corneal endothelial cell culture », Regen Med, vol. 16, no 9, pp. 871–891. https://doi.org/10.2217/rme-2020-0202
Senoo, T. & Joyce, N. C. et « Cell cycle kinetics in corneal endothelium from old and young donors », Invest Ophthalmol Vis Sci, vol. 41, no 3, pp. 660–667, mars (2000).
Kinoshita, S. et al. « Injection of Cultured Cells with a ROCK Inhibitor for Bullous Keratopathy », N Engl J Med, vol. 378, no 11, pp. 995–1003, mars., (2018). https://doi.org/10.1056/NEJMoa1712770
Toda, M. et al. « Production of Homogeneous Cultured Human Corneal Endothelial Cells Indispensable for Innovative Cell Therapy », Invest Ophthalmol Vis Sci, vol. 58, no 4, pp. 2011–2020, avr. (2017). https://doi.org/10.1167/iovs.16-20703
Spinozzi, D. et al. « Improving the success rate of human corneal endothelial cell cultures from single donor corneas with stabilization medium », Cell Tissue Bank, vol. 19, no 1, pp. 9–17, mars., (2018). https://doi.org/10.1007/s10561-017-9665-y
Parekh, M. et al. « Passaging capability of human corneal endothelial cells derived from old donors with and without accelerating cell attachment », Exp Eye Res, vol. 189, p. 107814, déc. (2019). https://doi.org/10.1016/j.exer.2019.107814
Peh, G. S. L. et al. « propagation of human corneal endothelial cells: a novel dual media approach ». Cell. Transpl. 24, 287–304. https://doi.org/10.3727/096368913X675719 (2015). no 2.
Roy, O., Beaulieu Leclerc, V., Bourget, J. M., Thériault, M. & Proulx, S. et « Understanding the Process of Corneal Endothelial Morphological Change In Vitro », Investigative Ophthalmology & Visual Science, vol. 56, no 2, pp. 1228–1237, févr. (2015). https://doi.org/10.1167/iovs.14-16166
Liu, Y. et al. « human corneal endothelial cells expanded in vitro are a powerful resource for tissue engineering ». Int. J. Med. Sci. 14, 128–135. https://doi.org/10.7150/ijms.17624 (2017). no 2.
Palchesko, R. N., Lathrop, K. L. & Funderburgh, J. L. et A. W. Feinberg, « In vitro expansion of corneal endothelial cells on biomimetic substrates », Sci Rep, vol. 5, p. 7955, janv. (2015). https://doi.org/10.1038/srep07955
Okumura, N. et al. « Enhancement on primate corneal endothelial cell survival in vitro by a ROCK inhibitor », Invest Ophthalmol Vis Sci, vol. 50, no 8, pp. 3680–3687, août., (2009). https://doi.org/10.1167/iovs.08-2634
Koizumi, N., Okumura, N. & Kinoshita, S. et « Development of new therapeutic modalities for corneal endothelial disease focused on the proliferation of corneal endothelial cells using animal models », Experimental Eye Research, vol. 95, no 1, pp. 60–67, févr. (2012). https://doi.org/10.1016/j.exer.2011.10.014
Okumura, N. et al. « Activation of the Rho/Rho Kinase Signaling Pathway Is Involved in Cell Death of Corneal Endothelium », Invest Ophthalmol Vis Sci, vol. 57, no 15, pp. 6843–6851, déc. (2016). https://doi.org/10.1167/iovs.16-20123
Okumura, N. et al. « Laminin-511 and – 521 enable efficient in vitro expansion of human corneal endothelial cells », Invest Ophthalmol Vis Sci, vol. 56, no 5, pp. 2933–2942, mai., (2015). https://doi.org/10.1167/iovs.14-15163
He, Z. et al. « Corneal endothelial cell therapy: feasibility of cell culture from corneas stored in organ culture », Cell Tissue Bank, vol. 22, no 4, pp. 551–562, déc. (2021). https://doi.org/10.1007/s10561-021-09918-8
Nishiuchi, R. et al. « Ligand-binding specificities of laminin-binding integrins: a comprehensive survey of laminin-integrin interactions using recombinant alpha3beta1, alpha6beta1, alpha7beta1 and alpha6beta4 integrins », Matrix Biol, vol. 25, no 3, pp. 189–197, avr. (2006). https://doi.org/10.1016/j.matbio.2005.12.001
Watanabe, M. et al. « Maintenance of Hepatic Functions in Primary Human Hepatocytes Cultured on Xeno-Free and Chemical Defined Human Recombinant Laminins », PLoS One, vol. 11, no 9, p. e0161383, (2016). https://doi.org/10.1371/journal.pone.0161383
Sasaki, T. et al. « Laminin-121–recombinant expression and interactions with integrins », Matrix Biol, vol. 29, no 6, pp. 484–493, juill. (2010). https://doi.org/10.1016/j.matbio.2010.05.004
Hagbard, L. et al. « Developing defined substrates for stem cell culture and differentiation », Philos Trans R Soc Lond B Biol Sci, vol. 373, no 1750, p. 20170230, juill. (2018). https://doi.org/10.1098/rstb.2017.0230
Ishikawa, T. et al. sept., « Laminins 411 and 421 differentially promote tumor cell migration via α6β1 integrin and MCAM (CD146) », Matrix Biol, vol. 38, pp. 69–83, (2014). https://doi.org/10.1016/j.matbio.2014.06.002
Jokinen, J. et al. « Integrin-mediated cell adhesion to type I collagen fibrils », J Biol Chem, vol. 279, no 30, pp. 31956–31963, juill. (2004). https://doi.org/10.1074/jbc.M401409200
Choi, J. S. et al. « in vitro evaluation of the interactions between human corneal endothelial cells and extracellular matrix proteins ». Biomed Mater, (2013).
Delco, M. L. et al. « Integrin α10β1-Selected Mesenchymal Stem Cells Mitigate the Progression of Osteoarthritis in an Equine Talar Impact Model », Am J Sports Med, vol. 48, no 3, pp. 612–623, mars., (2020). https://doi.org/10.1177/0363546519899087
Rutgers, M. et al. « Effect of collagen type I or type II on chondrogenesis by cultured human articular chondrocytes », Tissue Eng Part A, vol. 19, no 1–2, pp. 59–65, janv. (2013). https://doi.org/10.1089/ten.TEA.2011.0416
Kern, A., Eble, J., Golbik, R. & Kühn, K. et « Interaction of type IV collagen with the isolated integrins alpha 1 beta 1 and alpha 2 beta 1 », Eur J Biochem, vol. 215, no 1, pp. 151–159, juill. (1993). https://doi.org/10.1111/j.1432-1033.1993.tb18017.x
Chen, S. et al. « Advances in culture, expansion and mechanistic studies of corneal endothelial cells: a systematic review », J Biomed Sci, vol. 26, no 1, p. 2, janv. (2019). https://doi.org/10.1186/s12929-018-0492-7
He, Z. et al. « optimization of immunolocalization of cell cycle proteins in human corneal endothelial cells ». Mol. Vis. 17, 3494–3511 (2011).
Weigert, M., Schmidt, U., Haase, R., Sugawara, K. & Myers, G. et « Star-convex Polyhedra for 3D Object Detection and Segmentation in Microscopy », in IEEE Winter Conference on Applications of Computer Vision (WACV), mars 2020, pp. 3655–3662., mars 2020, pp. 3655–3662. (2020). https://doi.org/10.1109/WACV45572.2020.9093435
Frangi, A. F., Schnabel, J. A., Davatzikos, C., Alberola-López, C. & Fichtinger, G. et Éd., Medical Image Computing and Computer Assisted Intervention – MICCAI : 21st International Conference, Granada, Spain, September 16–20, 2018, Proceedings, Part IV, vol. 11073. in Lecture Notes in Computer Science, vol. 11073. Cham: Springer International Publishing, 2018. (2018). https://doi.org/10.1007/978-3-030-00937-3
Stringer, C., Wang, T., Michaelos, M. & Pachitariu, M. « Cellpose: a generalist algorithm for cellular segmentation », Nat Methods, vol. 18, no 1, pp. 100–106, janv. (2021). https://doi.org/10.1038/s41592-020-01018-x
Pachitariu, M. & Stringer, C. et « Cellpose 2.0: how to train your own model », Nat Methods, vol. 19, no 12, pp. 1634–1641, déc. (2022). https://doi.org/10.1038/s41592-022-01663-4
Gavet, Y., Pinoli, J. C. & Geometric Dissimilarity Criterion Between Jordan Spatial Mosaics. et « A. Theoretical Aspects and Application to Segmentation Evaluation », J Math Imaging Vis, vol. 42, no 1, pp. 25–49, janv. (2012). https://doi.org/10.1007/s10851-011-0272-4
Ono, T. et al. « corneal endothelial cell density and morphology in ophthalmologically healthy young individuals in japan: an observational study of 16842 eyes ». Sci. Rep. 11, 18224. https://doi.org/10.1038/s41598-021-97776-5 (sept. 2021).
Bourne, W. M., Nelson, L. R. & Hodge, D. O. et « Central corneal endothelial cell changes over a ten-year period », Invest Ophthalmol Vis Sci, vol. 38, no 3, pp. 779–782, mars (1997).
Duman, R., Tok Çevik, M., Görkem Çevik, S., Duman, R. & Perente, İ. et « Corneal endothelial cell density in healthy Caucasian population », Saudi J Ophthalmol, vol. 30, no 4, pp. 236–239, (2016). https://doi.org/10.1016/j.sjopt.2016.10.003
Abdellah, M. M. et al. « Corneal Endothelial Cell Density and Morphology in Healthy Egyptian Eyes », J Ophthalmol, vol. p. 6370241, 2019, (2019). https://doi.org/10.1155/2019/6370241
Arıcı, C., Arslan, O. S. & Dikkaya, F. et « Corneal endothelial cell density and morphology in healthy Turkish eyes », J Ophthalmol, vol. p. 852624, 2014, (2014). https://doi.org/10.1155/2014/852624
« Microcomputer analysis for corneal endothelial cell morphology - Alanko – 1983 - Acta Ophthalmologica - Wiley Online Library ».
Català, P. et al. « Approaches for corneal endothelium regenerative medicine », Progress in Retinal and Eye Research, vol. 87, p. 100987, mars., (2022). https://doi.org/10.1016/j.preteyeres.2021.100987
Ben Moussa, O. et al. « Femtosecond Laser Cutting of Human Crystalline Lens Capsule and Decellularization for Corneal Endothelial Bioengineering », Bioengineering (Basel), vol. 11, no 3, p. 255, mars., (2024). https://doi.org/10.3390/bioengineering11030255
Acquart, S. et al. « Endothelial morphometry by image analysis of corneas organ cultured at 31 degrees C », Invest Ophthalmol Vis Sci, vol. 51, no 3, pp. 1356–1364, mars., (2010). https://doi.org/10.1167/iovs.08-3103
Garcin, T. et al. « Preclinical validation of an innovative corneal bioreactor versus organ culture for long term storage: a randomized controled study », Acta Ophthalmologica, vol. 95, no S259, (2017). https://doi.org/10.1111/j.1755-3768.2017.01544
Guindolet, D. et al. « storage of Porcine cornea in an innovative bioreactor ». Invest. Ophthalmol. Vis. Sci. 58, 5907–5917. https://doi.org/10.1167/iovs.17-22218 (nov. 2017). no 13.
Garcin, T. et al. « Innovative corneal active storage machine for long-term eye banking », American Journal of Transplantation, vol. 19, no 6, pp. 1641–1651, juin., (2019). https://doi.org/10.1111/ajt.15238
Garcin, T. et al. « Three-month Storage of Human Corneas in an Active Storage Machine », Transplantation, vol. 104, no 6, pp. 1159–1165, juin., (2020). https://doi.org/10.1097/TP.0000000000003109
Mimura, T. & Joyce, N. C. et « Replication competence and senescence in central and peripheral human corneal endothelium », Invest Ophthalmol Vis Sci, vol. 47, no 4, pp. 1387–1396, avr. (2006). https://doi.org/10.1167/iovs.05-1199
Sabet, M. D. & Gordon, S. R. et « Ultrastructural immunocytochemical localization of fibronectin deposition during corneal endothelial wound repair. Evidence for cytoskeletal involvement », Biol Cell, vol. 65, no 2, pp. 171–179, (1989).
Nakayasu, K., Tanaka, M., Konomi, H. & Hayashi, T. et « Distribution of types I, II, III, IV and V collagen in normal and keratoconus corneas », Ophthalmic Res, vol. 18, no 1, pp. 1–10, (1986). https://doi.org/10.1159/000265406
Numata, R. et al. « Cultivation of corneal endothelial cells on a pericellular matrix prepared from human decidua-derived mesenchymal cells », PLoS One, vol. 9, no 2, p. e88169, (2014). https://doi.org/10.1371/journal.pone.0088169
Yamaguchi, M. et al. « Adhesion, migration, and proliferation of cultured human corneal endothelial cells by laminin-5 », Invest Ophthalmol Vis Sci, vol. 52, no 2, pp. 679–684, févr. (2011). https://doi.org/10.1167/iovs.10-5555
de Oliveira, R. C. & Wilson, S. E. et « Descemet’s membrane development, structure, function and regeneration », Exp Eye Res, vol. 197, p. 108090, août (2020). https://doi.org/10.1016/j.exer.2020.108090
McKay, T. B., Schlötzer-Schrehardt, U., Pal-Ghosh, S., Stepp, M. A. & et « integrin: basement membrane adhesion by corneal epithelial and endothelial cells ». Exp. Eye Res. 198, 108138. https://doi.org/10.1016/j.exer.2020.108138 (sept. 2020).
Koizumi, N., Okumura, N., Kinoshita, S. & Kruse, F. E. et U. Schloetzer-Schrehardt, « application of laminin to corneal endothelial cell culture », 4 juin 2015.
Saikia, P., Medeiros, C. S., Thangavadivel, S. & Wilson, S. E. et « Basement membranes in the cornea and other organs that commonly develop fibrosis », Cell Tissue Res, vol. 374, no 3, pp. 439–453, déc. (2018). https://doi.org/10.1007/s00441-018-2934-7
Eghrari, A. O., Riazuddin, S. A., Gottsch, J. D. & et « overview of the cornea: structure, function, and development ». Prog Mol. Biol. Transl Sci. 134, 7–23. https://doi.org/10.1016/bs.pmbts.2015.04.001 (2015).
Aouimeur, I. et al. « Investigating the Role of TGF-β Signaling Pathways in Human Corneal Endothelial Cell Primary Culture », Cells, vol. 12, no 12, p. 1624, juin., (2023). https://doi.org/10.3390/cells12121624
He, Z. et al. « 3D map of the human corneal endothelial cell », Sci Rep, vol. 6, p. 29047, juill. (2016). https://doi.org/10.1038/srep29047
Acknowledgements
We extend our sincere gratitude to the cornea donors and their families for their generous and invaluable contributions to medical and scientific advancement. We also wish to sin-cerely thank the Eye Banks of Saint-Étienne, Besançon, and Nantes for their crucial support in providing corneas for research purposes. We also thank the transplant coordination of the CHU of Saint-Étienne and Paris Robert Debré as well as the laboratory of anatomy of the Faculty of Medicine of Saint-Étienne.
Funding
None.
Author information
Authors and Affiliations
Contributions
G.Tr., L.C., Z.H., P.G., G.Th., C.M., took part in the concept and design of the study. G.Tr., L.C., I.A., C.M., G.B., E.O., C.M., performed experiments, collected and analyzed data. G.B., Y.G. and C.M., trained the AI. G.Tr., L.C., Z.H., E.O., P.G., G.Th., C.M. wrote-original draft preparation, G.Tr., L.C., Z.H., E.O., Y.G., A.M., P.G., G.Th., C.M. wrote-review and edited. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Travers, G., Coulomb, L., Aouimeur, I. et al. Investigating the role of molecular coating in human corneal endothelial cell primary culture using artificial intelligence-driven image analysis. Sci Rep 15, 31301 (2025). https://doi.org/10.1038/s41598-025-14367-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-14367-4