Abstract
To analyze the incidence and progression rates of myopia among children aged 6–8 years in Chengdu, and to evaluate the influence of baseline parameters and dynamic changes in ocular biometric parameters on new-onset myopia risk. A total of 26,169 students aged 6–8 years from eight administrative districts in Chengdu were followed annually for 4 years. All students underwent uncorrected distance visual acuity testing, non-cycloplegic autorefraction, and ocular biometric parameters. Potential risk factors for myopia onset were screened through multivariate logistic regression analysis. The influence of each factor was evaluated using the area under the curve (AUC). Results showed that the baseline prevalence of myopia was 17.8%. The cumulative incidence rates of myopia were 8.1–13.4% (2nd year), 8.6–12.2% (3rd year), and 11.5–16.2% (4th year) across different age groups, with higher rates in older children and females. The mean myopia progression rate was − 0.45 ± 0.32 D/year in the persistent myopia (PM) group. The annual growth rates of axial length(AL) and axial length/corneal radius (AL/CR) ratio in both the new-onset myopia (NOM) group and PM group were higher than those in the persistent non-myopia (PNM) group. The NOM showed significantly higher annual reduction rates in lens thickness and lens power(LP), and higher annual increase rate in anterior chamber depth compared to both PNM and PM. Both baseline parameters (e.g., AL, LP) and their changes 1–3 years before myopia onset significantly influenced the risk of myopia onset (all P < 0.001). The model combining baseline values and annual changes demonstrated good performance with cross-validated AUC values of 0.853. The study demonstrates that baseline values and changes 1–3 years before myopia onset in ocular biometric parameters have important influence on myopia onset, suggesting their incorporation into comprehensive myopia prevention and control systems for children.
Similar content being viewed by others
There is a global trend among children and adolescents toward earlier onset of myopia, faster progression, and an increasing proportion of high myopia(HM), with East Asian populations showing significantly higher myopia rates than those in Europe and the Americas1,2. By 2050, the estimated prevalence of myopia among children and adolescents in China is projected to reach approximately 84%3. Approximately 50% of the world’s population will experience varying degrees of myopia, with a global HM prevalence rate of around 9.8%4. HM can lead to fundus changes, such as tessellated fundus, optic disc tilt, and posterior scleral staphyloma5,6,7. HM may also result in serious complications, including cataracts, glaucoma, myopic macular degeneration, and retinal detachment8. Further progression to pathological myopia can cause irreversible vision impairment and blindness, making it one of the leading causes of blindness worldwide9.
To address this challenge, multiple countries have employed cohort studies to investigate factors influencing childhood myopia. Research has been extensively conducted in countries such as the United States10,11Singapore12,13Australia14and China, with a particular focus on the onset and progression of childhood myopia. Several Chinese cities, including Anyang, Shandong, and Guangzhou, have conducted cohort studies examining childhood myopia incidence and progression rates, yielding significant findings. For instance, the Anyang Childhood Eye Study (ACES) revealed that myopia prevalence among seventh-grade students increased from 67.3 to 82.7%, while HM prevalence rose from 2.7 to 7.1%15. Wang et al.16 conducted a two-year follow-up study of 123,535 students aged 6–13 years in Feicheng, Shandong, and found that myopia prevalence in 2020 had increased by 1.4-3 times compared to the previous five years. In a five-year follow-up study of 4,645 students aged 7–14 years in Guangzhou, Wang et al.17 discovered that the annual myopia incidence consistently ranged between 20 and 30%. The research team led by He Xiangui at the Shanghai Eye Disease Prevention and Treatment Center conducted a survey and follow-up study of 1,856 first-, second-, and third-grade students from six primary schools in Shanghai’s Baoshan district. They found that over a two-year period, the average progression of myopic refraction was 0.91, 0.91, and 1.11D respectively, while axial length (AL) increases were 0.70, 0.64, and 0.71 mm respectively, with refractive error showing a positive correlation with myopia progression18.
Research has shown that baseline ocular biometric parameters (such as spherical equivalent(SE), AL, etc.) serve as objective indicators with significant predictive value for myopia onset10. Ma et al. found that prediction models incorporating baseline parameters such as SE and AL can achieve high accuracy (AUC = 0.880)18. Similarly, Zhang et al. developed prediction models based on indicators including AL, anterior chamber depth(ACD), and lens thickness(LT), achieving AUC values of 0.815–0.974, demonstrating that ocular biometric parameters can effectively predict myopia onset19. Notably, additional myopia predictors such as lower positive relative accommodation (PRA), less hyperopic SE, longer AL, and female gender have also been identified as key risk factors20. With the advancement of machine learning technologies, the accuracy of prediction models has further improved. For instance, the Time-aware Long Short-Term Memory (T-LSTM) model developed by Huang et al.21through analyzing large-scale population data, reduced the mean absolute prediction error to 0.103 ± 0.140D.
In terms of machine learning applications, Du et al. constructed efficient models for predicting children’s SE progression based on up to 33 parameters, including visual acuity, ocular biometric parameters, intraocular pressure, and accommodative function, achieving mean errors of 0.372-0.43622. Lin et al. successfully developed machine learning algorithms using large-scale data on age, SE, and annual progression rates from populations aged 6–20 years, accurately predicting SE values for future years with mean absolute errors of 0.253–0.395 for 3-year predictions and 0.503–0.799 for 8-year predictions23. Additionally, Huang et al. developed a T-LSTM model utilizing multiple refractive screening results, including uncorrected visual acuity, SE, keratometry(K), and AL, which can accurately process long-term sequential data to further improve prediction accuracy21.
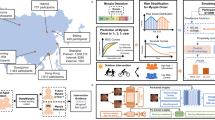
Myopia screening is the crucial first step in childhood myopia prevention and control. Currently, although cycloplegic refraction is the gold standard for childhood myopia screening, its limited accessibility and utilization are attributed to insufficient public awareness (e.g., parental concerns about side effects of cycloplegic agents) and the lack of qualifications for performing cycloplegic refraction in some optical facilities. This study determines the annual incidence and progression rates of myopia among 6-8-year-olds in Chengdu, China, while assessing the predictive role of baseline and dynamic ocular biometric parameters changes in identifying myopia onset risk.
Method
Study design and population
This was a prospective cohort study conducted from December 2019 to December 2023 in Chengdu, China, involving students aged 6–8 years. This study adopted a stratified random cluster sampling method: eight districts were randomly selected from the 23 districts/counties in Chengdu, and a census was conducted on all primary schools within them (totaling 281). The study adhered to the principles of the Declaration of Helsinki and received ethical approval from the Ethics Committee of Ineye hospital of Chengdu university of TCM (2019yh-007). In collaboration with the Chengdu Education Bureau, an online parents’ meeting was held prior to the school screenings to explain the study’s purpose, methods, and relevant precautions. Informed consent was obtained from the parents. During the survey, a total of 342,566 person-times were conducted, and 107,505 individuals were screened. After applying inclusion and exclusion criteria, 26,169 individuals were included in the baseline study (Fig. 1).
Inclusion Criteria: (1) Students enrolled in primary schools in Chengdu; (2) Aged 6–8 years; (3) Individuals who completed four consecutive ocular biometric parameters.
Exclusion Criteria: (1) Patients with various types of glaucoma, corneal diseases, lens diseases, retinal diseases, optic nerve diseases, etc.; (2) Patients with amblyopia, strabismus, anisometropia, or severe visual dysfunction; (3) Patients with entropion, severe conjunctivitis, etc.; (4) Individuals with poor compliance, mental disorders, or cognitive impairments.
The research team consisted of ophthalmologists, optometrists, and ophthalmic nurses, all of whom received standardized training. All participants underwent a comprehensive ophthalmic examination, including uncorrected and corrected visual acuity tests, non-cycloplegic autorefraction, and measurements of ocular biometric parameters. Visual acuity was measured using the International E-chart, which complies with GB11533-2011 standards, with uncorrected distance visual acuity tested for all students and corrected visual acuity for those wearing glasses. Refractive error was assessed using a Topcon RM-800 autorefraction from Japan. Three consecutive measurements were taken for each eye, with the requirement that the difference in spherical power between any two measurements be less than 0.5D. If the difference exceeded this threshold, additional measurements were performed, and the final result was the average of all valid measurements. Ocular biometric parameters was performed using a Tianjin Suowei SW-9000 optical biometer, with measurements taken in a non-cycloplegic state. Three measurements per eye were taken, and the instrument performed automatic quality control. If a measurement was deemed invalid, it was repeated. The final data for each eye were the average values of valid measurements.
Relevant definition
Myopia definition: Myopia is defined as a SE ≤ − 0.50 D in non-cycloplegic refraction and uncorrected visual acuity (UCVA) > 0 logMAR24,25. Persistent myopia (PM) Group: Children who demonstrated myopia consistently across all four data collection time points. Persistent non-myopia (PNM) group: Children who remained non-myopic throughout all four data collection time points.New-onset myopia (NOM) group: Children who were initially non-myopic at the first information collection and subsequently developed myopia in subsequent information collections.The rates of NOM is defined as the number of new-onset myopia cases divided by the number of individuals who were not myopic in the previous year. Annual change calculation for parameters: To account for the differences in follow-up intervals between individuals and to accurately reflect the temporal changes in parameters, the annual change for each parameter is calculated by subtracting the baseline value from each follow-up measurement and dividing the difference by the follow-up interval (in years). The average of the annual changes across all follow-up points is then taken as the final annual change.
Calculation of lens power
This study employed the method proposed by Bennett for calculating lens power (LP)26,27. This method is based on ocular optical principles and assumes the positions of the principal points of the crystalline lens, requiring only the subject’s refractive error, corneal curvature values, and relevant ocular biometric measurements (AL, ACD, LT) to complete the calculation.
The Bennett formula used in this study is as follows:
LP= -[1000nx(Scv + Km)]/[1000n-(ACD + C1xLT)x(Scv + Km)] + 1000n/(-C2xLT + Vd), and Scv = SE/(1-0.014xSE), C1 = 0.596, C2=−0.358, n = 1.336, Vd = AL-ACD-LT.
In the formula, LP represents lens power, SE is the spherical equivalent, Km is corneal power, ACD is anterior chamber depth, LT is lens thickness, AL is axial length, Vd is vitreous depth, n is the refractive index of aqueous and vitreous humors, and C1 and C2 are estimated parameters based on the Gullstrand-Emsley eye model. This formula, based on ray tracing principles, eliminates the need for direct measurement of crystalline lens surface curvature, providing a convenient method for lens power assessment in clinical practice and research.
Data analysis methods
Data analysis was performed using multiple Python libraries (version 3.11.7) including Pandas, NumPy, SciPy, Statsmodels, and Scikit-learn. For normally distributed quantitative data, results were expressed as mean ± standard deviation. Independent samples t-tests were used for comparisons between two groups (gender), while one-way analysis of variance (ANOVA) was employed for multiple group comparisons (age, refractive status). When data did not follow a normal distribution, Mann-Whitney tests were conducted. Categorical data were presented as n (%) with 95% confidence intervals. Fisher’s exact test was used for nominal categorical variables (such as gender, myopia status) comparisons between groups. Kruskal-Wallis H tests were used for comparing ordinal data across multiple groups, while Wilcoxon rank-sum tests were applied for two-group comparisons of ordinal data. Variables were standardized to eliminate dimensional effects, and extreme outliers were removed using the three-sigma method. All statistical tests were two-sided, with P < 0.05 considered statistically significant. Considering that the relationship between most ocular biometric parameters and the risk of myopia onset may not be completely linear, we stratified both baseline values and annual change rates into tertiles. This approach, consistent with similar ophthalmic studies28,29,30allowed us to evaluate threshold effects while maintaining statistical robustness. Logistic regression models were then applied to assess the impact of these stratified parameters on NOM. Annual change rates were calculated using data from examinations in years 1–3 as predictors, while using myopia status at the fourth examination as the outcome measure. This temporal separation between predictors and outcome reduced the risk of circular reasoning. To account for the hierarchical data structure, we applied cluster-robust standard errors with schools as the clustering unit, with Tertile 1 serving as the reference group and adjusting for age and gender. Model performance was assessed using 5-fold cross-validation, with AUC values reported as mean ± standard deviation.
Results
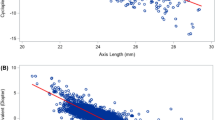
A total of 26,169 subjects were included in the study, of whom 13,155 (50.27%) were male. No significant differences were found between males and females in terms of proportion, age distribution, and SE (all P > 0.05). Overall ocular biometric parameters, the mean values (± SD) for the total sample were: AL, 23.06 ± 0.79 mm; K, 43.31 ± 1.49D; axial length/corneal radius (AL/CR) ratio,2.96 ± 0.09; LT, 3.67 ± 0.24 mm; ACD, 2.94 ± 0.27 mm; central corneal thickness(CCT), 541.68 ± 31.98 μm and LP 23.56 ± 2.15D, and males showed significantly higher values in AL, ACD, CCT, and AL/CR ratio compared to females, while females demonstrated significantly higher values in LT, LP, and K (Table 1). The overall myopia prevalence among children aged 6–8 years was 17.8%, showing an increasing trend with age (9.2% vs. 16.1% vs. 26.5%). No statistical differences in myopia prevalence were found between genders in the 6- and 7-year-old groups. However, in the 8-year-old group, females showed a higher prevalence of myopia compared to males (27.3% vs. 25.7%, P < 0.001). With increasing age, AL, AL/CR ratio, ACD, and CCT showed continuous growth across all age groups (P < 0.001;Table 2; Fig. 2).
Subjects were stratified into PNM, NOM, and PM groups based on refractive status during follow-up. Annual AL growth ranked as follows: PM (0.436 ± 0.193 mm/year) was greater than NOM (0.428 ± 0.190 mm/year), which was greater than PNM (0.211 ± 0.126 mm/year) (P < 0.001). For LT reduction and ACD increase rates, NOM showed greater changes than PNM, which showed greater changes than PM (both P < 0.001). AL/CR ratio growth was higher in NOM/PM than PNM (P < 0.001). LP decreased faster in NOM vs. PNM/PM (P < 0.001). Minor CCT changes followed the pattern: PNM was greater than NOM, which was greater than PM (P < 0.001), while K reduction ranked as NOM was greater than PM, which was greater than PNM (P < 0.001) (Table 3).Age-stratified analyses (6-, 7-, 8-year-olds) are detailed in Supplemental Table 1.
The incidence rates of myopia in the 6-year-old group were 8.1%, 8.6%, and 11.5% in the second, third, and fourth years, respectively. For the 7-year-old group, the new-onset myopia rates were 9.9%, 9.9%, and 14.6%, while the 8-year-old group showed rates of 13.4%, 12.2%, and 16.2%. The rates of NOM demonstrated an increasing trend with both age and follow-up duration. Although girls generally showed higher incidence rates of myopia than boys, the gender difference in the 6-year-old group was not statistically significant during the follow-up period. However, in the 8-year-old group, girls exhibited significantly higher incidence rates of myopia than boys, indicating that gender differences in incidence rates of myopia became more apparent with increasing age and were more pronounced in older age groups and longer follow-up periods. (Table 4; Fig. 3)
Excluding the confounding effects of multicollinearity among the parameters in each model, Table 5 presents multivariate logistic regression analysis for NOM at year 4 follow-up, adjusted for age, gender, and baseline ocular parameters (AL, K, LP). Each additional year of age (OR = 1.05, P = 0.011) and female gender (OR = 1.35, P < 0.001) were associated with increased NOM risk. Longer baseline AL showed a dose-dependent relationship with NOM risk (middle tertile: OR = 1.49; highest tertile: OR = 2.31, both P < 0.001), as did steeper K values (middle tertile: OR = 1.28; highest tertile: OR = 1.75, both P < 0.001). Conversely, higher LP values demonstrated a protective effect (highest tertile: OR = 0.79, P < 0.001).
Table 6 analyzed the impact of annual changes in ocular biometric parameters (years 1–3) on NOM at year 4. Age (OR = 1.63, P < 0.001) and female gender (OR = 1.07, P < 0.001) remained significant risk factors. Most notably, rapid axial elongation strongly predicted myopia onset, with children in the highest AL change tertile showing over five-fold increased risk (OR = 5.62, P < 0.001) compared to the lowest tertile. For annual K change, both middle tertile (−0.14 to −0.07 D/y) and highest tertile (>−0.07 D/y) demonstrated significant increased risk (OR = 1.14, 95% CI: 1.09–1.19; OR = 1.28, 95% CI: 1.23–1.34; both P < 0.001). Similarly, for annual LP change, both middle tertile (−1.19 to −0.33 D/y) and highest tertile (>−0.33 D/y) exhibited significant risk (OR = 1.15, 95% CI: 1.10–1.19; OR = 1.12, 95% CI: 1.07–1.17; both P < 0.001).
The analytical results for Model-3 (adjusted for age, gender, and baseline ocular biometric parameters: AL, ACD, LT, CCT, and K) and Model-4 (adjusted for age, gender, and annual changes in the aforementioned parameters from years 1–3) are presented in the supplementary materials (Supplementary Tables 2 and 3).
Comparative analysis of predictive efficacy demonstrated that Model-2 (incorporating annual changes in AL, K, and LP) exhibited superior predictive performance (AUC = 0.842, CV-AUC = 0.842 ± 0.004) compared to Model-1 (including baseline parameters AL, K, and LP; AUC = 0.685, CV-AUC = 0.684 ± 0.010). The integration of Models 1 + 2 (combining baseline parameters and annual changes) enhanced the AUC to 0.853 (CV-AUC = 0.853 ± 0.006). Similarly, Model-4 (annual changes in AL, ACD, LT, CCT, and K) demonstrated improved predictive efficacy over Model-3 (baseline AL, ACD, LT, CCT, and K), with AUC values of 0.842 versus 0.697, respectively. The combined application of Models 3 + 4 achieved an AUC of 0.856 (CV-AUC = 0.856 ± 0.005) (Figs. 4 and 5). These results suggest that dynamic ocular biometric parameter changes hold significantly greater predictive value than static baseline parameters, while the combination of baseline and change data achieves optimal prediction performance. Notably, models based on parameters (AL, K, LP) performed similarly to those using parameters (AL, ACD, LT, CCT, K).
Discussion
In this 4-year cohort study of children aged 6–8 years in Chengdu, we found that the baseline myopia prevalence was 17.8%, with cumulative incidence rates ranging from 8.1 to 16.2% across different age groups and follow-up years. The myopia progression rate in the PM group averaged − 0.45 ± 0.32 D/year, demonstrating significant progression during early school years. In this 4-year cohort study of children aged 6–8 years in Chengdu, we found that the baseline myopia prevalence was 17.8%, with cumulative incidence rates ranging from 8.1 to 16.2% across different age groups and follow-up years. The myopia progression rate in the PM group averaged − 0.45 ± 0.32 D/year, demonstrating significant progression during early school years.
We also explored the influence of baseline and dynamic changes in ocular biometric parameters, such as AL, K, and LP, on the onset and development of myopia in children in Chengdu. The results indicated that children with higher baseline AL and AL/CR ratio, steeper K, stronger LP, and greater annual changes in AL, AL/CR, and LP had a significantly increased risk of myopia onset. In conclusion, both baseline and dynamic changes in ocular biometric parameters significantly influence the risk of myopia onset. These findings provide important insights for prospective screening and early intervention, offering a new approach to precision prevention of myopia.
In this study, the overall myopia prevalence among children aged 6–8 years was 17.84%. Compared to other regions in China, this prevalence was higher than Wenzhou (14.21% for grades 1–3)31 but lower than Shanghai (25.6% for ages 7–9)32and significantly lower than the comprehensive survey results across various Chinese regions (35.8% for ages 6–8)33. The myopia prevalence for children aged 6, 7, and 8 years in this study were 9.2%, 16.1%, and 26.5% respectively, which were lower than those in Hong Kong (17.0% for below 7 years, 28.9% for 7 years, and 37.5% for 8 years)34. In comparison with other countries worldwide, these prevalence were substantially higher than Australia (7.6% at age 6)35the United States (6.1% for ages 5–8)36and various European countries such as Poland (4.0% at age 7)37Ireland (3.3% for ages 6–7)38the Aston Eye Study (AES) in the UK (5.7% for ages 6–7)28Bulgaria (14.2% for ages 6–10)39and Meta-analysis of myopia prevalence in African countries (3.4% for ages 5–11)40. The high prevalence of myopia among school-age children in China is likely attributable to multiple factors, including intense educational competition, limited outdoor activities, prolonged screen time, home confinement during COVID-19, and genetic factors16,41,42.
Previous studies have shown that new-onset myopia develops rapidly during childhood and adolescence before stabilizing in young adulthood43. In this study, we found that the incidence of myopia among children in Chengdu, increased rapidly from 9.2% at age 6 to 26.5% at age 8. Similar to our findings, studies in Weifang (China)44Chongqing (China)45and Hong Kong (China)34 also observed rapid increases in new-onset myopia among school-age children. In other countries, such as Spain, surveys of childhood myopia prevalence found rapid increases among children aged 5–7 years46while studies of Caucasian children in the United Kingdom also found higher rates of myopia onset during the school-age period compared to adolescence47. In our study, the rapid increase in new-onset myopia rate among children aged 6–8 years reflects that early school age was a critical period for myopia onset and progression, likely associated with gradually increasing academic demands and decreasing outdoor activity time.
AL growth is strongly associated with myopia progression48. The Guangzhou Twin Registry study of twins aged 7–15 years revealed accelerated AL growth during myopia onset (0.43 mm/year) compared to pre-onset (0.20 mm/year) and post-onset phases (0.21 mm/year)49. Consistent with the European Eye Study50 and the Northern Ireland Childhood Errors of Refraction (NICER) study51our findings demonstrated faster AL growth in the NOM group than in the PNM group. The AL/CR ratio further serves as a critical biomarker for myopia assessment. While an AL/CR ratio > 3 was historically used as a diagnostic threshold52recent evidence highlights age- and sex-dependent critical thresholds, increasing from 2.93 to 2.96 (age 6) to 3.07 (age 18) in girl and boy, reflecting ocular developmental dynamics aligned with somatic growth53.
The overall refractive status of the eye is determined by three key parameters: AL, K, and the LP. Among these, the K value was relatively stable54 and was consistent with the results of this study. This study further revealed that the NOM group exhibited greater annual reductions in LP and increases in AL compared to the PM and PNM groups. And based on the current analysis of annual parameter changes, we observed that AL change demonstrated the strongest association with myopia onset, both K and LP changes also showed significant associations with myopia development, though with smaller effect sizes than AL change (Table 6). Our findings on AL growth and LP changes align with previous studies49,55,56,57though conflicting evidence exists, such as Xiong et al. found no significant LP loss differences between persistent emmetropia and NOM groups58. AL growth and LP loss coordinate to maintain refractive homeostasis in children through dynamic balance, however, the dynamic relationship between them requires further systematic research to confirm.
This study enhances myopia prediction by integrating baseline ocular biometric parameters with their annual rate of change 1–3 years pre-onset, significantly improving accuracy compared to single-parameter models. However a key limitation of our study was the exclusion of environmental and genetic factors, which were well-established determinants of myopia onset and progression59,60,61. Chua et al. proposed that factors such as age of onset, gender, ethnicity, and AL can effectively predict HM (AUC = 0.85)62. Yang et al. also found that factors such as wearing spectacle frames and lifestyle factors (e.g., outdoor activities, diet, and behavior) were associated with the new-onset myopia, with an AUC of 0.9863. Regarding genetic factors, especially parental myopia status, it has been established as a high-risk predictor for myopia64reflecting the interaction between genetics and environment. In recent years, there have been significant advances in the application of single nucleotide polymorphisms (SNPs) and polygenic risk scores (PRS) from genome-wide association studies (GWAS) in myopia prediction. Ghorbani Mojarrad et al. optimized myopia prediction by integrating PRS into the Cox proportional hazards model, achieving an AUC of 0.67-0.7565. A GWAS study also found that a model incorporating 890 significant SNPs effectively predicted low, moderate, and high myopia (AUCs of 0.67, 0.74, and 0.75, respectively)66. Overall, this study improves the prediction model for new-onset myopia by combining baseline ocular biometric parameters and their annual rate of change, significantly enhancing its accuracy.
This study’s strengths include a large-scale cohort of children aged 6–8 in Chengdu, China, and a four-year longitudinal follow-up systematically tracking refractive and ocular biometric parameters. Limitations: Non-cycloplegic measurements may still overestimate myopia incidence, potentially resulting in slightly higher estimates of actual myopia prevalence due to the influence of pseudomyopia cases. The decision not to perform cycloplegic refraction in this study was based on the following considerations: (1) ethical approval and parental consent challenges for using cycloplegic agents on students in a large-scale study; (2) temporary blurred vision after cycloplegia potentially affecting students’ learning activities on the same day; and (3) as pointed out in Chen et al.‘s24 study, using automated refraction under non-cycloplegic conditions ensured higher participation rates and visual status under natural accommodation. Given that the focus of this study was to analyze the relationship patterns between ocular biometric parameters and myopia development, this limitation has minimal impact on our main conclusions. We also referred to similar large-scale screening studies24,25,67ensuring adequate sample size and research feasibility while maintaining rigorous procedures for non-cycloplegic refraction. However, this study cannot substitute the accuracy of cycloplegic refraction. Therefore, in future research, we suggest conducting both cycloplegic and non-cycloplegic measurements to verify whether the biometric parameter measurement results maintain consistency under different conditions. Absence of environmental (e.g., outdoor activity) and genetic data (e.g., parental myopia) limits predictive model completeness. Future work should: incorporate cycloplegic refraction, expand data collection to environmental/genetic factors, and develop comprehensive models for improved myopia control strategies.
This study, based on four-year cohort data of children aged 6–8 years in Chengdu, confirmed that baseline values, as well as annual changes in these parameters 1–3 years prior to myopia onset, serve as critical predictive factors for myopia development. These findings highlight the importance of monitoring ocular biometric parameters and their dynamic changes before myopia onset in providing a theoretical basis for predicting myopia onset.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions as they contain information that could compromise the privacy of research participants.
References
Grzybowski, A., Kanclerz, P., Tsubota, K., Lanca, C. & Saw, S. M. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 20, 27. https://doi.org/10.1186/s12886-019-1220-0 (2020). PMID:31937276.
Ezegwui, I. R. et al. Prevalence of refractive errors and visual impairment in school children in Enugu South-East Nigeria. Niger J. Clin. Pract. 24, 380–386. https://doi.org/10.4103/njcp.njcp_521_19 (2021). .PMID:33723112.
Dong, L. et al. A systemic review and Meta-Analysis. Retina 40, 399–411. https://doi.org/10.1097/iae.0000000000002590 (2020). .PMID:31259808.
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042. https://doi.org/10.1016/j.ophtha.2016.01.006 (2016). .PMID:26875007.
Chang, L. et al. Myopia-related fundus changes in Singapore adults with high myopia. Am. J. Ophthalmol. 155, 991–999e991. https://doi.org/10.1016/j.ajo.2013.01.016 (2013). .PMID:23499368.
Flores-Moreno, I., Lugo, F., Duker, J. S. & Ruiz-Moreno, J. M. The relationship between axial length and choroidal thickness in eyes with high myopia. Am. J. Ophthalmol. 155, 314–319e311. https://doi.org/10.1016/j.ajo.2012.07.015 (2013). .PMID:23036569.
Yan, Y. N. et al. Ten-Year progression of myopic maculopathy: the Beijing eye study 2001–2011. Ophthalmology 125, 1253–1263. https://doi.org/10.1016/j.ophtha.2018.01.035 (2018). .PMID:29602569.
Ikuno, Y. & OVERVIEW OF THE COMPLICATIONS OF HIGH MYOPIA Retina 37, 2347–2351, https://doi.org/10.1097/iae.0000000000001489 (2017). .PMID:28590964.
Wong, T. Y., Ferreira, A., Hughes, R., Carter, G. & Mitchell, P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am. J. Ophthalmol. 157, 9–25e12. https://doi.org/10.1016/j.ajo.2013.08.010 (2014). .PMID:24099276.
Zadnik, K. et al. Prediction of Juvenile-Onset myopia. JAMA Ophthalmol. 133, 683–689. https://doi.org/10.1001/jamaophthalmol.2015.0471 (2015). .PMID:25837970.
Mutti, D. O. et al. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Invest. Ophthalmol. Vis. Sci. 52, 199–205. https://doi.org/10.1167/iovs.09-4826 (2011). .PMID:20739476.
Saw, S. M. et al. Y. A cohort study of incident myopia in Singaporean children. Invest. Ophthalmol. Vis. Sci. 47, 1839–1844. https://doi.org/10.1167/iovs.05-1081 (2006). .PMID:16638989.
Tong, L., Chan, Y. H., Gazzard, G., Tan, D. & Saw, S. M. Longitudinal study of anisometropia in Singaporean school children. Invest. Ophthalmol. Vis. Sci. 47, 3247–3252. https://doi.org/10.1167/iovs.05-0906 (2006). .PMID:16877388.
Ojaimi, E. et al. Methods for a population-based study of myopia and other eye conditions in school children: the Sydney myopia study. Ophthalmic Epidemiol. 12, 59–69. https://doi.org/10.1080/09286580490921296 (2005). .PMID:15848921.
Li, S. M. et al. Time outdoors and myopia progression over 2 years in Chinese children: the Anyang childhood eye study. Invest. Ophthalmol. Vis. Sci. 56, 4734–4740. https://doi.org/10.1167/iovs.14-15474 (2015). PMID:26207310.
Wang, J. et al. Progression of myopia in School-Aged children after COVID-19 home confinement. JAMA Ophthalmol. 139, 293–300. https://doi.org/10.1001/jamaophthalmol.2020.6239 (2021). .PMID:33443542.
Wang, S. K. et al. Incidence of and factors associated with myopia and high myopia in Chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. 136, 1017–1024. https://doi.org/10.1001/jamaophthalmol.2018.2658 (2018). .PMID:29978185.
Ma, Y. et al. Cohort study with 4-year follow-up of myopia and refractive parameters in primary schoolchildren in Baoshan district, Shanghai. Clin. Exp. Ophthalmol. 46, 861–872. https://doi.org/10.1111/ceo.13195 (2018). .PMID:29577563.
Zhang, M. et al. Validating the accuracy of a model to predict the onset of myopia in children. Invest. Ophthalmol. Vis. Sci. 52, 5836–5841. https://doi.org/10.1167/iovs.10-5592 (2011). .PMID:21330664.
Wong, Y. L. et al. Prediction of myopia onset with refractive error measured using non-cycloplegic subjective refraction: the WEPrOM study. BMJ Open. Ophthalmol. 6, e000628. https://doi.org/10.1136/bmjophth-2020-000628 (2021). .PMID:34179509.
Huang, J., Ma, W., Li, R., Zhao, N. & Zhou, T. Myopia prediction for children and adolescents via time-aware deep learning. Sci. Rep. 13, 5430. https://doi.org/10.1038/s41598-023-32367-0 (2023). PMID:37012269.
Du, B. et al. Prediction of spherical equivalent difference before and after cycloplegia in school-age children with machine learning algorithms. Front. Public. Health. 11, 1096330. https://doi.org/10.3389/fpubh.2023.1096330 (2023). .PMID:37113174.
Lin, H. et al. Prediction of myopia development among Chinese school-aged children using refraction data from electronic medical records: A retrospective, multicentre machine learning study. PLoS Med. 15, e1002674. https://doi.org/10.1371/journal.pmed.1002674 (2018). .PMID:30399150.
Thorn, F. et al. Refractive status and prevalence of myopia among Chinese primary school students. Clin. Experimental Optometry. 103, 177–183. https://doi.org/10.1111/cxo.12980 (2020). .PMID:31674055.
Wang, J. et al. Prevalence of myopia in 3-14-year-old Chinese children: a school-based cross-sectional study in Chengdu. BMC Ophthalmol. 21, 318. https://doi.org/10.1186/s12886-021-02071-6 (2021). .PMID:34470605.
Cheng, T. et al. Crystalline lens power and associated factors in highly myopic children and adolescents aged 4 to 19 years. Am. J. Ophthalmol. 223, 169–177. https://doi.org/10.1016/j.ajo.2020.07.007 (2021). .PMID:32681906.
Bennett, A. G. A method of determining the equivalent powers of the eye and its crystalline lens without resort to phakometry. Ophthalmic Physiological Optics: J. Br. Coll. Ophthalmic Opticians (Optometrists). 8, 53–59. https://doi.org/10.1016/0275-5408(88)90089-0 (1988). .PMID:3047630.
Li, S. M. et al. Annual incidences and progressions of myopia and high myopia in Chinese schoolchildren based on a 5-Year cohort study. Invest. Ophthalmol. Vis. Sci. 63, 8. https://doi.org/10.1167/iovs.63.1.8 (2022). .PMID:34989760.
Saw, S. M. et al. Incidence and progression of myopia in Singaporean school children. Invest. Ophthalmol. Vis. Sci. 46, 51–57. https://doi.org/10.1167/iovs.04-0565 (2005). .PMID:15623754.
He, X. et al. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS One. 10, e0111766. https://doi.org/10.1371/journal.pone.0111766 (2015). .PMID:25693186.
Jiang, D. et al. Longitudinal association between myopia and parental myopia and outdoor time among students in wenzhou: a 2.5-year longitudinal cohort study. BMC Ophthalmol. 21, 11. https://doi.org/10.1186/s12886-020-01763-9 (2021). PMID:33407251.
Cheng, P. et al. Prevalence and related factors of children myopia in Pudong new area, shanghai: a cross-sectional study. BMJ Open. 13, e079330. https://doi.org/10.1136/bmjopen-2023-079330 (2023). .PMID:38070885.
Zhou, J. et al. [Prevalence of myopia and influencing factors among primary and middle school students in 6 provinces of china]. Zhonghua Liu Xing Bing Xue Za Zhi. 37, 29–34. https://doi.org/10.3760/cma.j.issn.0254-6450.2016.01.006 (2016). .PMID:26822639.
Fan, D. S. et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest. Ophthalmol. Vis. Sci. 45, 1071–1075. https://doi.org/10.1167/iovs.03-1151 (2004). PMID:15037570.
Robaei, D., Rose, K., Kifley, A. & Mitchell, P. Patterns of spectacle use in young Australian school children: findings from a population-based study. J. Aapos. 9, 579–583. https://doi.org/10.1016/j.jaapos.2005.07.005 (2005). .PMID:16414527.
Theophanous, C. et al. Myopia prevalence and risk factors in children. Clin. Ophthalmol. 12, 1581–1587. https://doi.org/10.2147/opth.S164641 (2018). PMID:30214142.
Czepita, D., Zejmo, M. & Mojsa, A. Prevalence of myopia and hyperopia in a population of Polish schoolchildren. Ophthalmic Physiol. Opt. 27, 60–65. https://doi.org/10.1111/j.1475-1313.2006.00419.x (2007). .PMID:17239191.
Harrington, S. C., Stack, J., Saunders, K. & O’Dwyer, V. Refractive error and visual impairment in Ireland schoolchildren. Br. J. Ophthalmol. 103, 1112–1118. https://doi.org/10.1136/bjophthalmol-2018-312573 (2019). .PMID:30315130.
Dragomirova, M., Antonova, A., Stoykova, S., Mihova, G. & Grigorova, D. Myopia in Bulgarian school children: prevalence, risk factors, and health care coverage. BMC Ophthalmol. 22, 248. https://doi.org/10.1186/s12886-022-02471-2 (2022). .PMID:35658918.
Ovenseri-Ogbomo, G. et al. Systematic review and meta-analysis of myopia prevalence in African school children. PLoS One. 17, e0263335. https://doi.org/10.1371/journal.pone.0263335 (2022). .PMID:35113922.
Lyu, F. [Educational environment: the most powerful factor for the onset and development of myopia among students]. Sichuan Da Xue Xue Bao Yi Xue Ban. 52, 895–900. https://doi.org/10.12182/20211160301 (2021). .PMID:34841750.
Yu, M. et al. Global risk factor analysis of myopia onset in children: A systematic review and meta-analysis. PLoS One. 18, e0291470. https://doi.org/10.1371/journal.pone.0291470 (2023). .PMID:37729320.
Bullimore, M. A. et al. IMI-Onset and progression of myopia in young adults. Invest. Ophthalmol. Vis. Sci. 64, 2. https://doi.org/10.1167/iovs.64.6.2 (2023). .PMID:37126362.
Zhang, J. et al. Prevalence of myopia: A large-scale population-based study among children and adolescents in weifang, China. Front. Public. Health. 10, 924566. https://doi.org/10.3389/fpubh.2022.924566 (2022). .PMID:35958863.
Zhou, W. J. et al. Five-Year progression of refractive errors and incidence of myopia in School-Aged children in Western China. J. Epidemiol. 26, 386–395. https://doi.org/10.2188/jea.JE20140258 (2016). PMID:26875599.
Alvarez-Peregrina, C. et al. On behalf of grupo de investigación alain, A. The prevalence of myopia in children in spain: an updated study in 2020. Int. J. Environ. Res. Public. Health. 18 https://doi.org/10.3390/ijerph182312375 (2021). PMID:34886101.
McCullough, S. J., O’Donoghue, L. & Saunders, K. J. Six year refractive change among white children and young adults: evidence for significant increase in myopia among white UK children. PLoS One. 11, e0146332. https://doi.org/10.1371/journal.pone.0146332 (2016). .PMID:26783753.
Saw, S. M. et al. Eye growth changes in myopic children in Singapore. Br. J. Ophthalmol. 89, 1489–1494. https://doi.org/10.1136/bjo.2005.071118 (2005). .PMID:16234459.
Xiang, F., He, M. & Morgan, I. G. Annual changes in refractive errors and ocular components before and after the onset of myopia in Chinese children. Ophthalmology 119, 1478–1484. https://doi.org/10.1016/j.ophtha.2012.01.017 (2012). .PMID:22578257.
Tideman, J. W. L. et al. W. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 96, 301–309. https://doi.org/10.1111/aos.13603 (2018). PMID:29265742.
Breslin, K. M., O’Donoghue, L. & Saunders, K. J. A prospective study of spherical refractive error and ocular components among Northern Irish schoolchildren (the NICER study). Invest. Ophthalmol. Vis. Sci. 54, 4843–4850. https://doi.org/10.1167/iovs.13-11813 (2013). .PMID:23745004.
Yebra-Pimentel, E. et al. [Changes in axial length/corneal radius ratio (AL/CR) according to refractive state of the eye. Relationship with ocular components]. Arch. De La. Sociedad Esp. De Oftalmologia. 79, 317–324. https://doi.org/10.4321/s0365-66912004000700004 (2004). PMID:15286900.
Liu, S. et al. Cutoff values of axial length/corneal radius ratio for determining myopia vary with age among 3–18 years old children and adolescents. Graefe’s Archive Clin. Experimental Ophthalmol. = Albrecht Von Graefes Archiv Fur Klinische Und Experimentelle Ophthalmologie. 262, 651–661. https://doi.org/10.1007/s00417-023-06176-0 (2024). .PMID:37578514.
Li, S. M. et al. Distribution of ocular biometry in 7- and 14-year-old Chinese children. Optom. Vis. Sci. 92, 566–572. https://doi.org/10.1097/opx.0000000000000570 (2015). .PMID:25875684.
Zhang, J. et al. Changes in lens thickness and power before and after myopia onset. Invest. Ophthalmol. Vis. Sci. 66, 36. https://doi.org/10.1167/iovs.66.3.36 (2025). .PMID:40100202.
Han, X. et al. Longitudinal changes in lens thickness and lens power among persistent Non-Myopic and myopic children. Invest. Ophthalmol. Vis. Sci. 63, 10. https://doi.org/10.1167/iovs.63.10.10 (2022). .PMID:36107112.
Rozema, J., Dankert, S., Iribarren, R., Lanca, C. & Saw, S. M. Axial growth and lens power loss at myopia onset in Singaporean children. Invest. Ophthalmol. Vis. Sci. 60, 3091–3099. https://doi.org/10.1167/iovs.18-26247 (2019). .PMID:31323091.
Xiong, S. et al. Accelerated loss of crystalline lens power initiating from emmetropia among young school children: a 2-year longitudinal study. Acta Ophthalmol. 100, e968–e976. https://doi.org/10.1111/aos.15002 (2022). .PMID:34411434.
Yue, Y. et al. High prevalence of myopia and low hyperopia reserve in 4411 Chinese primary school students and associated risk factors. BMC Ophthalmol. 22 https://doi.org/10.1186/s12886-022-02436-5 (2022). PMID:WOS:000793842400001.
Mountjoy, E. et al. Education and myopia: assessing the direction of causality by mendelian randomisation. Bmj 361, k (2022). https://doi.org/10.1136/bmj.k2022 (2018).PMID:29875094.
Mutti, D. O. Hereditary and environmental contributions to emmetropization and myopia. Optom. Vis. Sci. 87, 255–259. https://doi.org/10.1097/OPX.0b013e3181c95a24 (2010). .PMID:20019643.
Chua, S. Y. et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 36, 388–394. https://doi.org/10.1111/opo.12305 (2016). .PMID:27350183.
Yang, X. et al. Prediction of myopia in adolescents through machine learning methods. Int. J. Environ. Res. Public. Health. 17 https://doi.org/10.3390/ijerph17020463 (2020). PMID:31936770.
Lee, S. S. & Mackey, D. A. Prevalence and risk factors of myopia in young adults: review of findings from the raine study. Front. Public. Health. 10, 861044. https://doi.org/10.3389/fpubh.2022.861044 (2022). .PMID:35570945.
Ghorbani Mojarrad, N., Plotnikov, D., Williams, C. & Guggenheim, J. A. Association between polygenic risk score and risk of myopia. JAMA Ophthalmol. 138, 7–13. https://doi.org/10.1001/jamaophthalmol.2019.4421 (2020). .PMID:31670792.
Hysi, P. G. et al. Meta-analysis of 542,934 subjects of European ancestry identifies new genes and mechanisms predisposing to refractive error and myopia. Nat. Genet. 52, 401–407. https://doi.org/10.1038/s41588-020-0599-0 (2020). PMID:32231278.
Wilson, S., Ctori, I., Shah, R., Suttle, C. & Conway, M. L. Systematic review and meta-analysis on the agreement of non-cycloplegic and cycloplegic refraction in children. Ophthalmic Physiol. Opt. 42, 1276–1288. https://doi.org/10.1111/opo.13022 (2022). .PMID:35913773.
Acknowledgements
We thank the Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Key Laboratory of Sichuan Province Ophthalmopathy Prevention & Cure and Visual Function Protection with TCM Laboratory and Retinal Image Technology and Chronic Vascular Disease Prevention&Control and Collaborative Innovation Center for its technical support.
Funding
1.Sichuan Provincial Science and Technology Plan “Unveiling and Leading” Project (2023YFS0506);2.National Natural Science Foundation of China (62175022);3.Chengdu University of Traditional Chinese Medicine“Xinglin Scholars” Discipline Talent Research Enhancement Plan (ZDZX2022004);4.Sichuan Natural Science Foundation (2022NSFSC0803).
Author information
Authors and Affiliations
Contributions
Zengrui Zhang and Jingyu Mu contributed to the design and conduct of the study, results interpretation and wrote the whole paper. Yanrong Yang contributed to the design and conduct of the study. Junguo Duan and Yun Dai contributed to the results interpretation and critically revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study received approval from the Ethics Committee of Chengdu University of Traditional Chinese Medicine Ineye Hospital(2019yh-007). All research methods adhered to the principles outlined in the “Declaration of Helsinki”. Prior to conducting the study, the objectives and methods were presented to the principals, teachers, and parents of the participating schools to obtain informed consent, and signatures were obtained accordingly. Informed consent to participate in the study was obtained from students parents.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Z., Mu, J., Yang, Y. et al. Influence of dynamic changes of ocular biometric parameters on new-onset myopia in Chinese children: a 4-year cohort study. Sci Rep 15, 28474 (2025). https://doi.org/10.1038/s41598-025-14453-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-14453-7