Abstract
Since the COVID-19 pandemic, there is growing evidence that the social epidemiological context may play a crucial role in the adoption of health protective behaviours in response to emerging infectious diseases. Yet, our understanding of how and why these behaviours are influenced by the epidemiological forces remains relatively limited. This repeated, cross-sectional investigation examines the extent to which the association between the socio-epidemiological context and protective behaviour was mediated by a series of common social cognitive factors from leading models of health behaviour during the COVID-19 epidemic in France. Representative samples of the French population completed an online, self-report survey at seventeen intervals (March–November 2020), with approximately 2000 participants in each survey wave. Results indicate that both contextual and social cognitive variables largely drove the adoption of protective behaviours over time. However, social cognitive variables only partially mediated the effect of the epidemiological context on protective behaviour (physical distancing and hygiene measures), suggesting that unknown factors may be operating in addition to those commonly used in these models. These findings highlight the need for future research to consider the epidemiological context, and further possible mediating variables, when modelling determinants of social cognitions and preventive behaviour, and above all, to broaden its focus to include neglected underlying psychological mechanisms involved in the behavioural response to epidemics.
Similar content being viewed by others
Introduction
The COVID-19 pandemic has highlighted the importance of individual and community engagement in and adherence to protective behaviours in reducing disease spread and subsequent health burden1. Understanding the determinants of these protective measures in the context of a constantly evolving epidemic of this novel, infectious virus has since been the focus of much recent research attention. Of necessity, existing theoretical models predicting behavioural response have been applied to the COVID-19 pandemic, with research in this area falling largely into two broad categories: studies from the health psychology field investigating social cognitive determinants of protective behaviour2,3,4,5,6, or those from the human behaviour modelling domain exploring epidemiological determinants of protective measures and their subsequent impact on disease spread7,8,9. Although several authors in the past have insisted upon the need to explore how epidemics influence health and social behaviour10,11,12, little research has focused upon combining these two research fields to investigate how and why the epidemiological context itself might impact protective behaviour – answers to which would represent an important advancement for both fields of research. The current study attempts to bridge this gap in the literature by exploring whether and the extent to which the effect of the epidemiological context on protective behaviour (physical distancing and hygiene measures) is mediated by common social cognitive variables from leading models of health behaviour. It is hoped that this goal of developing a better understanding of the causal or mediating mechanisms that underpin the adoption of preventive behaviours13 will not only enable us to assess the ability of existing theories of health behaviour to account for the effects of unstable epidemic conditions, but that it shall also facilitate the development of public health interventions that can target the appropriate mediators, at the appropriate time, to promote behavioural change and reduce the spread of future emerging infectious diseases.
Theoretical background
Health psychology research into determinants of health protective behaviour has largely focused upon intrapersonal or interpersonal cognitive factors influencing the adoption and maintenance of protective behaviours in response to a public health threat3,14,15,16. From this perspective, a set of social cognitive models of health behaviour, such as the health belief model17, the theory of planned behaviour18, protection motivation theory19 and social cognitive theory20 consistently contend that the behavioural response to a particular disease or health issue arises as a result of social cognitive factors. Grounded in these social cognitive models of health behaviour frequently used in the field of infectious diseases21, the current investigation adopted a “splitting”, or constituent concept approach to theory testing, whereby concepts and hypotheses (and in this instance, social cognitive and epidemiological variables) emanating from often different theories are tested and evaluated22,23. Acknowledging that theory development “is a cyclic process that involves the specification of relations between factors, the testing of those relations, the re-specification or rejection of initially hypothesised principles and the testing of new relations”24 (p 296), we sought to explore the mechanisms underlying the adoption of health behaviours. When using the term “social cognitive variables” in this article, we will refer to these main variables drawn from the afore-mentioned models.
Although developed largely through research into more chronic health issues intrinsically associated with a fairly stable epidemic environment25,26,27, such as that associated with HIV, cancer or cardiovascular disease, these models nonetheless provide a good starting point in any empirical exploration of behaviour change28. The question remains as to whether they apply differently to the unstable, rapidly evolving context inherent to a pandemic of an emerging infectious disease. If we consider for instance perceived risk, observed in the past to drive adoption of protective behaviour16,29,30, it is likely that, when faced with the rapid spread and evolving variants of COVID-19, and resultant extremely unstable volatile epidemic context31, people would react by reappraising the risk and modifying their behaviour over time32. Behavioural modelling applied to the COVID-19 outbreak suggests that people engage in a Bayesian learning process, updating risk appraisal according to newly-acquired relevant information33 and protective behaviours in response to this particular epidemic34. However, research into COVID-19 risk appraisal and protective behaviours has provided varying findings35: a positive correlation36,37, no correlation38,39, or inconsistent results4. Nonetheless, temporal investigations revealed a more consistent trend towards a reduction in risk perception and protective measures over time5,40,41,42, possibly due to risk habituation40 or, having adopted preventive measures, to appraising risk as being reduced43. As was the case with risk perception (measured through perceived severity and perceived vulnerability to infection)4,6,44, other social cognitive factors, such as perceived behavioural control45,46,47, perceived barriers41, response efficacy (the perceived effectiveness of protective measures)35, worry48 and perceived social norms3,4,38,49,50,51 have been found to play a role in people’s decision to adopt protective measures during an epidemic, although not always consistently35,38. To identify the social cognitive determinants of adherence to protective behaviours during the COVID-19 epidemic in France, measures of each of these common constructs were incorporated into the current study.
Epidemic context and protective behaviour
Despite empirical support for people’s updating their beliefs and perceptions during an epidemic, the effect of the epidemic context on social cognitions and subsequent preventive behaviour appears to be underrepresented in the existing health psychology literature regarding infectious diseases. Several investigations have nonetheless responded to calls to address this10,11,12,27,42, lending support for the influential role of the epidemiological context in its influencing the adoption of some protective measures in response to both perceived and actual disease prevalence during a mosquito-borne disease epidemic26, in its association with levels of worry during the H1N1 epidemic in the United Kingdom (number of hospitalisations)48, and with compliance with H1N1 protective recommendations in Malaysia (death incidence)52, as well as its correlation with COVID-19 risk perception (case numbers)42.
Although several investigations have acknowledged the influence of the COVID-19 epidemiological context on people’s compliance with health recommendations5,7,41,53,54, findings from the few relevant studies vary. Whilst government policy stringency scores7,55 and disease incidence (number of hospitalisations)40 were associated with preventive behaviour, these effects diminished over time7,40, and social cognitive factors, rather than incidence (case numbers), were proposed to represent more reliable determinants of protective behaviour5, highlighting the importance of exploring the social cognitive pathways through which the epidemic context might influence behaviour. We define the epidemic context here as encompassing the epidemiological situation and the interrelated, government-regulated social environment56,57. Henceforth, the terms “epidemic context” and “epidemiological context” shall be used interchangeably.
Epidemic context in France
This investigation spanned the first nine months of the COVID-19 epidemic in France. During this time, two national lockdowns were instigated, the first of which began on 17 March 2020, coinciding with the beginning of the data collection period, and finished on 10 May 2020. Throughout this period, schools, universities and all non-essential businesses were closed and the public was asked to stay at home. People were authorised to go out for essential items within one kilometre of their residence, i.e., for essential medical treatment or to their local supermarket. From 11 May, restrictions were lifted progressively, with cafés and leisure centres re-opening with limited capacity. In response to increasing hospital admissions and fatalities, a series of regional and national curfews was imposed, followed by a second lockdown, from 30 October to 15 December 2020, during which non-essential businesses closed but schools and factories remained open58. Data collection concluded in November, during the second lockdown. Considering lockdown in measurement of the epidemic context is important as it is likely that participants’ being authorised to engage in social activities may have an influence upon their adoption or otherwise of other protective behaviours such as hygiene measures.
Research objective
The main objective of the current study is to determine: (1) whether the epidemiological context influences adherence to protective behaviour and its main social cognitive determinants, and (2) whether the effect of the epidemiological context on protective behaviour (physical distancing and hygiene measures) is mediated by social cognitive variables and if so, to what extent. Given the changes, both epidemiological and in terms of government-imposed lockdowns, occurring during the first year of the COVID-19 epidemic in France, it seems reasonable to assume that this epidemiological context might impact the social cognitive variables that, in turn, influence protective behaviour. Thus, the current exploration of the underlying causal mechanisms by which psychosocial factors influence health behaviours may improve our understanding in this area, thereby making a small contribution to moving health behaviour change theory forward13.
Results
Temporal variations in protective behaviours and their determinants
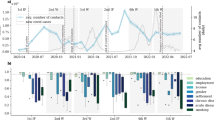
As shown in Fig. 1, the number of health protective behaviours reported by participants varied considerably over time (with a median value = 7 in Week 2, and = 4 in Week 27; Kruskal Wallis’s chi² = 4467.5, df = 16, p < .001, η2 = 0.131). To further examine the distribution of the behavioural data across surveys, a generalised mixed model was used. Based on the Wald Z test, we found that the between-survey variance in protective behaviours was 0.023 (Z = 44.9, p < .001), which indicated a clustering effect in the behavioural data. To assess the level of non-independence in the behavioural variable, we calculated the intraclass correlation coefficient (ICC). The ICC was estimated at 0.117, i.e., a value above the threshold of 0.05, which is commonly considered as evidence of data clustering59. These temporal variations in health protection behaviour made it necessary to use a multilevel model in subsequent multivariate analyses. By contrast, as shown in Fig. 2, the social cognitive factors were prone to significant but smaller variations over time (Kruskal Wallis’s chi² > 73 (16; 34,016), p < .001, 0.002 < η2 < 0.054). With the notable exception of perceived social norms (ICC = 0.073) and, to a smaller degree, worry (ICC = 0.028), the constructs related to the threat and the coping appraisals were surprisingly found to be largely insensitive to the epidemiological context during the first year of the pandemic in France (ICC < 0.020).
Contextual determinants of health protective behaviours
When tested individually, the multilevel Poisson regression analyses showed that adoption of preventive behaviours was significantly influenced by the three contextual variables introduced into the model: time, number of new COVID-19 hospitalisations, and lockdown. However, consistent with previous research40, we found that the incidence–behaviour relationship was moderated to a large extent by time. As shown in Fig. 3, the effect of the incidence of COVID-19 on preventive behaviour was substantially weaker in the second study period than in the first, i.e., the weight of incidence tended to weaken over time. These three variables, as well as one representing the interaction between incidence and time, were then tested simultaneously as potential predictors of the adoption of preventive behaviour. As Table 1A (Step 2) shows, among the Level 2 variables, only the interaction term and the time factor remained significant in predicting preventive behaviour (IRR = 1.006 and 0.986 ; p < .001, respectively), suggesting that the effect of hospitalisation numbers on health behaviours was moderated by time. These results show that one more week was related to 1–2% less self-reported engagement in protective behaviour, while one unit increase in the interaction between incidence and time was positively associated with 0.4–0.8% more adherence to behavioural measures.
Personal determinants of health protective behaviours
Controlling for these four contextual variables, the following sociodemographic variables were introduced into a new generalised linear mixed model: gender, age, occupation and location of dwelling (urban or rural). As shown in Table 1B (Step 5), most of these personal determinants were found to predict the adoption of preventive behaviours (0.971 > IRR > 1.097; p < .01), with women, older people and those in rural areas being significantly more likely to adhere to protective behaviour than men, younger people and urban dwellers over the whole period. This analysis also revealed that the effect of the epidemiological context on the adoption of preventive behaviours remained largely unchanged once the sociodemographic variables were introduced into the model. These results suggest that there was very little association between epidemiological contextual variables and sociodemographic variables.
The seven variables drawn from prominent social cognitive models of health behaviours were then introduced into the model. The results of this final analysis, which explained 27.6% of the variance in the behavioural variable, are shown in Table 1B (Step 7). All the social cognitive variables were significantly associated with adherence to health protective behaviours (p < .001). However, only perceived behavioural control and perceived social norms were found to have large effect sizes (IRR > 1.02): participants with one unit higher in perceived behavioural control and social norms reported adhering on average across the study 5–6% and 7–8% more, respectively, to protective behaviour compared with participants with one unit lower in these constructs.
Mediators of the epidemiological context–behaviour relationship
To investigate the relationship between the epidemiological context and behaviour, we examined whether and to what extent the regression coefficients related to the contextual factors were reduced in this last modelling. Contrary to our expectations, the introduction of the seven social cognitive variables in the GLMM model did not appear to significantly alter the epidemiological context–behaviour relationships. As shown in Table 1B (Step 7), only the IRRs associated with the time factor decreased very slightly from 0.984 (95% CI: 0.979–0.989) to 0.986 (95% CI: 0.981–0.990), suggesting possible interactions with some social cognitive factors. To investigate further the relationship between time and adherence to protective behaviour, we conducted a mediation analysis. Following MacKinnon and Luecken’s13 procedure for modelling of mediated effects, only those social cognitive factors found to be relatively sensitive to the context were included as mediating variables in this analysis (η2 > 0.02). As shown in Table 2, the indirect effect of time on the adherence to preventive behaviours only represented 28.6% of the total effect. This indirect effect was found to be mostly driven by perceived social norms (IRR = 0.9990, p < .001) and, to a lesser extent, by perceived severity (IRR = 0.9996, p < .001) and worry (IRR = 0.9999, p = .022). This means that the majority of the effect of the epidemiological context on adherence to health protective behaviours remained largely unexplained by the conventional factors drawn from the leading social cognitive models of health behaviour.
Discussion
The COVID-19 pandemic has resulted in a need for rapid behavioural change in terms of protective measures to fight the spread and resultant health burden of this novel, infectious disease. Largescale adoption and maintenance of individual protective behavioural actions are therefore critical in achieving this goal34,60, as is understanding their underlying determinants. The results of the present investigation suggest that the social epidemiological context, in terms of incidence and time, influenced protective behavioural engagement during the COVID-19 epidemic in France, with time partly moderating the effect of incidence on the adoption of mitigation measures.
Whilst researchers in the past have alluded to ecological factors as having an impact upon social cognitions and resultant health behaviour, empirical research has focused primarily on the impact on behaviour of environmental, sociodemographic or social contextual factors61. Indeed, when applied to chronic disease, or infectious diseases which evolve slowly, and for which the epidemiological environment is relatively stable, it is of less relevance to consider the impact of the epidemiological circumstances. In contrast, in a highly dynamic, volatile epidemiological setting, such as the one that characterised the COVID-19 pandemic outbreak, it appears logical that the epidemiological context would result in people’s adapting both their risk appraisal and subsequent behaviour as a function of this constantly changing environment. Unexpectedly, however, our results suggest that social cognitions only partially mediated the effect of the epidemiological context on protective behaviour.
Through our research, we sought to discover which context-dependent factors served to mediate the epidemiological context–protective behaviour relationship. Contrary to our expectations, these results indicate that the majority of the constructs drawn from the social cognitive models of health behaviour were largely insensitive to the epidemiological context during the first year of the pandemic. This was particularly true for perceived vulnerability to COVID-19, assumed likely to represent the main mediator of the incidence–behaviour relationship42. In contrast, perceived social norms and, to a lesser extent, perceived severity and worry were found to be somewhat sensitive to the epidemiological context.
Perceived social norms have been frequently found to predict protective behavioural engagement51, particularly during the COVID-19 pandemic2,3,4,38,45,46,47,62,63,64 and in two instances, have played a strong mediational role between these protective behaviours and social media65 and cultural worldviews4. The reason as to why perceived social norms played a leading mediational role in our study may be that they are more other- rather than self-focused. Indeed, in contrast to individualistic worldviews, which have been associated with non-adherence to COVID-19 protective behaviours4,5,66,67, in the case of both injunctive and descriptive perceived social norms, a person’s attentional focus, rather than being individualistic, is instead centred around others, on what they approve of and do regarding protective measures. Perhaps the changing social and epidemiological context motivates people to consider the health and wellbeing of others, thereby accentuating the focus on prosocial behaviour, observed in the literature to predict risk perception66 and protective behaviour5,68,69,70. Behavioural motivation may therefore arise out of concern for others7,71, a sense of altruism72, empathy70,73 or perceived social obligation74, rather than perceived personal risk.
The somewhat small contribution of other social cognitions to mediating the epidemiological context–behavioural response relationship is echoed elsewhere in the COVID-19 health psychology literature, leading researchers to conclude that in this particular pandemic setting, perceived risk of infection was not a key motivational driver of preventive measures38,42,75. It may therefore be possible that there are more, and perhaps different, factors at play than those targeted in the current, and previous investigations38,42,75,76, such as moral norms77,78 and prosocial attitudes68,69,79, as well as those mentioned above.
Exploring individual variations in social cognitions and protective behaviour, one longitudinal study found injunctive social norms to be negatively associated with behavioural intention at the inter- but not the intra-individual level75. Whilst supporting our findings that risk perception was a poor predictor of protective behaviour, the authors found the epidemic context to have an inconsistent effect on protective behaviour. Including descriptive norms and measures of the epidemic context that were less prone to the underrepresentation associated with daily case numbers and deaths, such as new hospitalisations4,80, may have enhanced these results, possibly leading to findings more akin to our own, as well as to those of others7,40.
Related determinants of COVID-19 preventive behaviour that may be sensitive to the epidemiological context, and therefore potential mediating factors worthy of further investigation, are disease familiarity81 or experience66 and uncertainty82. Indeed, uncertainty regarding the perceived risk of COVID-19 may have varied as a function of familiarity83 in an inverse manner. Moderating the effect of incidence on behaviour, time may in our study have served as a proxy for (decreasing) uncertainty, or more aptly increasing certainty, as it could for increasing familiarity with the virus. These variables therefore merit further exploration in future studies of the underlying mechanisms involved in epidemic protective decision-making.
In addition to considering further mediational factors, thought should also be given to expanding upon existing ones. For example, whereas a single measure of trust (in Government) was not associated with protective behaviour41, the opposite was the case when multiple measures (trust in the World Health Organisation (WHO), scientific advisors, experts) were incorporated [84], highlighting the need to broaden the scope of measures of existing variables.
Acknowledging the socially motivated nature of behavioural engagement, existing theory, traditionally focused on the individual, should perhaps be expanded upon in future research to incorporate not only perceptions for oneself, but also for others, for instance regarding measures of perceived risk, worry85,86 and fear87,88. In a highly unpredictable epidemic environment, understanding the underlying psychological factors and mechanisms involved in behavioural engagement represents a vital step in combatting current and future epidemics.
The idea that different behavioural decision-making pathways may operate during an epidemic, in which the social epidemiological setting is in a constant state of flux, raises the question as to whether existing health behaviour models are adequate in explaining protective behavioural response under such conditions. It would appear from our findings that existing theory should, as Abraham et al.89 suggest, be expanded upon to include such a dynamic, epidemic environment.
Indeed, acknowledgement of the influence of context on behaviour is not new90,91, but has seldom been applied to epidemic behavioural response. As Fisher92 states, “the behaviour of the individual is viewed as guided by layers of influences including the family, proximal and social influences such as social networks or neighbourhoods, organisational influences such as worksite or community systems or healthcare systems and larger social influences such as government, policy or large economic structures.” (p 4.)92. It therefore follows that such a layered approach, through multilevel analysis of possible causal or at the very least, influential pathways, represents an exciting prospect for better understanding and predicting epidemic and pandemic behavioural response.
Moreover, concerns are increasingly being voiced that we are giving the health behaviour theories neither the attention nor the nourishment they deserve93. Under non-epidemic circumstances, these models typically explain 20–30% of the variance of engagement in health protective behaviours94,95. However, during the COVID-19 pandemic, these conventional models only explained 10–20% of the reported health protective behaviours83, which is congruent with our results. This encourages us to reflect upon the need to consider whether one should trade a widely held individual and universal perspective for a more dynamic and multi-factorial approach to health protective behaviour change in response to an emerging health threat. Such a stance would involve developing health behaviour models that incorporate intra-individual (i.e., perceived risk), structural (i.e., socioeconomic status) and contextual factors (i.e., incidence)96. Critical to the advancement of scientific theory is the measurement and testing of potential causal mechanisms, therefore the future should perhaps bear witness to more rigorous testing of theoretical pathways through which epidemiological parameters affect human protective behaviours. To date, only a few authors, such as Badham and Gilbert97 with their TELL ME model, have envisaged possible causal processes explaining this effect. Extending existing health behaviour theory to take into account the complex interplay between the epidemiological context, social and affective cognitions and protective behaviour, and the underlying mechanisms involved, represents a thought-provoking and challenging way forward in furthering our understanding of behaviour change.
Limitations
Despite its advantage of considering the ecological aspect of behavioural response to pandemic disease spread, the current investigation nonetheless has some limitations. Firstly, it relies upon subjective assessments of self-reported behaviour which may not entirely reflect actual behaviour and could be subject to certain biases, such as social desirability98, or inaccurate recall99. However, to date, these self-report surveys have been empirically validated100 and are considered to be reliable101, in addition to which, their online format is less subject to social desirability bias than are face-to-face surveys. It is nonetheless possible that the currently widely employed measures, particularly those of social cognitions, may not entirely capture the constructs they are designed to measure in this highly dynamic, constantly evolving epidemic setting.
Based on previous research40 and the results of the current investigation, we concluded that time played an important role in adherence to behavioural recommendations in response to an epidemic of an emerging infectious disease, in this instance, COVID-19. It is possible, however, that time may capture another factor, such as a declining fatality rate, increased herd immunity or progress in preventive or therapeutic treatments.
Although adopted frequently in the research literature, the use of single-item measures for most of the social cognitive constructs may pose a problem in terms of validity and reliability. Even though, to our knowledge, no validated questionnaire addressing such a variety of theoretical concepts exists that could have been applied rapidly to a large sample of the population, it is likely that the utilisation of scales would have provided measures with better accuracy than those based on a single item. Whilst the current investigation involved a wide range of protective behavioural measures, and despite their being highly correlated, it should be acknowledged that there are nonetheless differences between these behaviours and social cognitive mechanisms may not apply uniformly across all behaviours, particularly given possible variations in perceived barriers and social norms for each of the studied behaviours. However, in combining the behaviours into a composite behaviour score, we hoped to allow for such variations, thereby providing insight into the overall social cognitive–behavioural patterns.
A further limitation to our study may be that other factors are perhaps involved, ones not traditionally measured in research into more chronic illness or more slowly evolving epidemic disease, particularly those that are socially driven – moral norms, empathy, prosocial attitudes, concern for others and perceived social obligation. Finally, whilst our findings provide insight into the mediated effect of the epidemic context on protective behaviour over time, these results are nonetheless cross-sectional. It is possible that participants’ past behaviour influenced their risk appraisal, or that initial risk perception influenced behavioural engagement which, in turn, resulted in decreased levels of perceived risk43. Future extensive longitudinal studies involving a within-subjects design may allow us to gain a better appreciation of how individuals modify their behaviour in response to the epidemic context throughout the course of an epidemic, and subsequently improve further our understanding of the underlying individual psychological processes involved.
Conclusion
Understanding how epidemiological contexts, social cognitive factors and health protective behaviours are related and change over time, is crucial to better model, predict and mitigate the impact of emergent infectious disease epidemics on people’s health and lives. Unlike chronic illnesses, in which the epidemic setting remains relatively stable over time, that of an epidemic is characterised by its dynamic volatility. It is therefore not surprising that perceptions of risk and social cognitions, as traditionally understood and investigated, may manifest differently. It is also asking a great deal of existing theories and models to account for behavioural response under such different circumstances as those of a dynamic, novel epidemic outbreak of a highly contagious, rapidly mutating, unpredictable disease, during which actual and perceived threat are in a constant state of flux. The current study sought to bridge a gap in the literature between health psychology and behavioural modelling by exploring ecological factors contributing to behavioural engagement during the COVID-19 epidemic. Whilst our findings suggest that the epidemiological context influenced engagement in protective behaviour, as well as its social cognitive determinants, the epidemiological context–protective behaviour relationship was only partially mediated by social cognitive variables. Only perceived social norms and, to a lesser extent, perceived severity and worry, appear to be sensitive to the epidemic context, highlighting the salience of social factors and group dynamics during an epidemic. Other pathways and contributing moderating and mediating factors involved in this complex relationship remain unknown and should be the subject of future research. As engagement in protective measures during an epidemic is likely to be socially motivated, this represents not only a promising area for further investigation, but an aspect which merits attention when developing strategic, tailored public health campaigns and interventions. The current investigation raises broader theoretical research issues. Existing social cognitive theories of protective behaviour need to be nurtured by being tested, evaluated and even challenged in the context of outbreaks of infectious disease. When necessary, they should be extended and expanded upon so as to improve their predictive power in an unstable environment. Incorporating contextual factors into theories of health behaviour may prove to be a way forward in research and perhaps even key to comprehending and predicting behavioural response in an epidemic setting. Moreover, a deeper understanding of the layers and pathways involved in health behaviour models, one that includes an ecological component, may provide us with the tools necessary to improve the response to current and future epidemics and pandemics.
Methods
Participants and procedures
Data
Data were collected via a series of seventeen repeated, cross-sectional online CoviPrev surveys conducted by BVA (a market research company) on behalf of Santé Publique France (Public Health France) approximately every two weeks from March to November 2020 among French residents aged 18–99 years. Stratified sampling was used to obtain seventeen samples, drawn from a large research panel, which were representative of the metropolitan adult population according to age, sex, education, socio-economic status, occupation and region of residence, based on data from the 2016 national census102. Each survey wave represented a sample of approximately 2000 participants, with a total of 34,016 respondents participating in the study.
This research was conducted in accordance with the Declaration of Helsinki103 and the French national guidelines for ethical research in the social and human sciences. The study was approved by the EHESP School of Public Health Office for data Protection (Rennes, France) [Reference: MR 2510110520], and by the ethics committee of the University Hospital Institute, Méditerranée Infection (Marseille France) [Decision No. 2020-022]. Informed consent was obtained from participants prior to commencement.
Measures
Epidemic contextual variables
The COVID-19 epidemic conditions may comprise a variety of variables associated with the disease, such as its severity and contagiousness, the extent to which it is circulating in the population, as well as the mandated restrictive measures. Indeed, behavioural changes in response to the spread of the disease could be related not only to times of higher incidence but also to stricter government regulations. Three variables were used here as measures of the epidemic context: time (in weeks) since the implementation of the initial national lockdown in France (17 March 2020) (scale 2–36), government stringency (lockdown, no lockdown) and the weekly number of new hospitalisations due to COVID-19, representing incidence. The level of government stringency regarding mandated restrictions, as measured by lockdown or no lockdown, provided a stringency score of 0 or 1. The number of hospitalisations due to COVID-19, rather than prevalence or incidence rates, was used as a measure of the actual epidemiological setting, as it has been found to capture more accurately the number of (serious) cases4,80. The number of hospitalisations was calculated in terms of the number of people hospitalised due to COVID-19 per day, using a seven-day moving average of the number of COVID-19 hospitalisations (scale 92–3010).
Health protective behaviours
Engagement in eight health protective behaviours was measured by asking participants whether, over the past few days, they had engaged in either social distancing or hygiene behaviours. Items referring to physical distancing included staying home as much as possible, avoiding close contact with other people (from outside the household), staying at least one metre away from other people and avoiding physical contact (shaking hands, hugging etc.). Hygiene measures comprised observing hand hygiene, using a tissue only once, covering one’s mouth when coughing or sneezing and wearing a mask. Participants reported whether they engaged in these behaviours and the frequency with which they did so, answering according to a four-point Likert scale: “Yes, systematically”, “Yes, often”, “Yes, sometimes” or “No, never”. Due to a ceiling effect5, answers were re-coded into a dichotomous scale, with “Yes, systematically” coded as 1 (high compliance) and the other three responses as 0 (low compliance). Finally, the values for each item were added to generate a cumulative score (range 0–8) that enabled us to measure participants’ adherence to recommended protective behaviours.
Sociodemographic variables
Participants also provided sociodemographic data, including age, sex, education, occupation, socio-economic status, household composition, housing (number of rooms), rural or urban dwelling, as well as health-related information, such as pre-existing health conditions.
Social cognitive variables
Based on constructs derived from social cognitive models of health behaviour used widely in health psychology17,18,19,20,21,28,94,104, the current study incorporated measures of the following social cognitive variables (See Table 3): perceived risk (as measured by perceived vulnerability and perceived severity), worry, perceived barriers, perceived behavioural control, perceived efficacy of the measures (scale 0–10). Believed to best capture perceived social norms, a combination of measures of both injunctive (behaviours a person perceives his/her close social group members approve of) and descriptive (behaviours in which members of a person’s close family and/or social network are engaging) social norms was used62,63,77, using two questionnaire items for each (scale 0–4). Perceived behavioural control18,45,46,47, rather than self-efficacy5,17,35,74, was included as it is thought to encompass both external and internal factors18.
Data analysis
Non-parametric one-way ANOVA were used to test for differences in the distribution of social cognitive and behavioural variables across surveys, which allow to account for non-negative whole numbers, as well as for the fact that most variables had a skewed distribution. Poisson regression models were then conducted to estimate adjusted coefficients and associated 95% confidence intervals, examining the associations between the contextual variables and engagement in preventive behaviours during the first year of the COVID-19 pandemic and determining whether time moderated the incidence–behaviour relationship. Given the nested structure of data collected through repeated cross-sectional surveys, models were adjusted for survey clustering by using generalised linear mixed models (GLMMs). Here the database includes 34,016 individual observations nested in 17 surveys conducted all throughout the first year of the COVID pandemic to follow the temporal variations in protective behaviours and their contextual and personal determinants. Multilevel modelling allows us to analyse the cross-level interactions – from moderation to mediation – between individual variables (Level 1), such as perceived vulnerability to and severity of COVID-19 infection, and contextual variables (Level 2), such as weekly new hospitalisations at the time of the survey.
To facilitate the interpretation of the results, only the incidence rate ratios (IRR), i.e., the exponential of the GLMMs coefficients, will be reported. IRRs higher than 1 indicate a positive association between the variables, and IRRs lower than 1 a negative one. It is important to note here that the IRRs of the contextual and personal variables cannot be directly compared with each other, as their metrics are different. Next, the following variables were successively introduced in the multilevel analysis to reveal potential interactions between the contextual and personal determinants of preventive behaviour: sociodemographic characteristics (sex, age group, occupation, and location (urban versus rural neighbourhood)) and social cognitive variables (worry, perceived vulnerability, perceived severity, perceived effectiveness of the measures, perceived barriers, perceived behavioural control, and perceived social norms). Only the sociodemographic and social cognitive variables that were significantly associated with protective behaviour in bivariate analyses were introduced in multivariate analyses. Finally, a multilevel mediation analysis, using Poisson regression, was performed to identify the potential social cognitive mediators of the epidemiological context–behaviour relationship. The multilevel analyses were carried out by using IBM SPSS Version 21, and JAMOVI 2.3.26, while multilevel mediation modelling was performed by using STATA 15, which applies the gsem command, a procedure to appropriately test mediational effects in clustered data.
Data availability
The data that support the findings of this study are available from Santé Publique France but restrictions apply to the availability of these data, which were used under licence for the current study, and so are not publicly available. Data are however available from the authors (kathleen.mccoll@ehesp.fr or Jocelyn.Raude@ehesp.fr) upon reasonable request and with the permission of Santé Publique France.
References
Michie, S. & West, R. Behavioural, environmental, social, and systems interventions against covid-19. BMJ 370, m2982. https://doi.org/10.1136/bmj.m2982 (2020).
Lin, C. Y. et al. Using an integrated social cognition model to predict COVID-19 preventive behaviours. Br. J. Health Psychol. 25 (4), 981–1005. https://doi.org/10.1111/bjhp.12465 (2020).
Raude, J. et al. Determinants of preventive behaviors in response to the COVID-19 pandemic in france: comparing the sociocultural, psychosocial, and social cognitive explanations. Front. Psychol. 11, 584500. https://doi.org/10.3389/fpsyg.2020.584500 (2020).
Savadori, L. & Lauriola, M. Risk perception and protective behaviors during the rise of the COVID-19 outbreak in Italy. Front. Psychol. 3822 https://doi.org/10.3389/fpsyg.2020.577331 (2021).
Schneider, C. R. et al. COVID-19 risk perception: a longitudinal analysis of its predictors and associations with health protective behaviours in the united Kingdom. J. Risk Res. 24 (3–4), 294–313. https://doi.org/10.1080/13669877.2021.1890637 (2021).
Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C. & Mobbs, D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the united States. R Soc. Open. Sci. 7 (9), 200742. https://doi.org/10.1098/rsos.200742 (2020).
Al-Zubaidy, N. et al. Exploring the relationship between government stringency and preventative social behaviours during the COVID-19 pandemic in the united Kingdom. J. Health Inf. 29 (4), 14604582231215867. https://doi.org/10.1177/14604582231215867 (2023).
Farboodi, M., Jarosch, G. & Shimer, R. Internal and external effects of social distancing in a pandemic. J. Econ. Theory. 196, 105293. https://doi.org/10.1016/j.jet.2021.105293 (2021).
Makris, M. Covid and social distancing with a heterogenous population. J. Econ. Theory. 1–50. https://doi.org/10.1007/s00199-021-01377-2 (2021).
Cherif, A., Barley, K. & Hurtado, M. Homo-psychologicus: reactionary behavioural aspects of epidemics. Epidemics 14, 45–53. https://doi.org/10.1016/j.epidem.2015.09.003 (2016).
Ferguson, N. Capturing human behaviour. Nature 446 (7137), 733–733. https://doi.org/10.1038/446733a (2007).
Funk, S. et al. Nine challenges in incorporating the dynamics of behaviour in infectious diseases models. Epidemics 10, 21–25. https://doi.org/10.1016/j.epidem.2014.09.005 (2015).
MacKinnon, D. P. & Luecken, L. J. How and for whom? Mediation and moderation in health psychology. J. Health Psychol. 27 (2S), 99. https://doi.org/10.1037/0278-6133.27.2 (2008). S99.
Bish, A. & Michie, S. Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. Br. J. Health Psychol. 15 (4), 797–824. https://doi.org/10.1348/135910710X485826 (2010).
Sutton, S. Determinants of health-related behaviours: theoretical and methodological issues. The Sage Handbook of Health Psychology (eds Sutton, S., Baum, A. & Johnston, M.) 94–126 (Sage, London, (2004).
Weinstein, N. D. Exploring the links between risk perceptions and preventive health behavior. Social Psychological Foundations of Health and Illness (eds Suls, J. & Wallston, K. A.) 22–53 (Blackwell Publishing Ltd, (2003).
Rosenstock, I. M. Historical origins of the health belief model. Health Educ. Monogr. 2 (4), 328–335. https://doi.org/10.1177/109019817400200403 (1974).
Ajzen, I. From Intentions To Actions: A Theory of Planned Behavior 11–39 (Springer, 1985).
Rogers, R. W. A protection motivation theory of fear appeals and attitude change1. J. Psychol. 91 (1), 93–114. https://doi.org/10.1080/00223980.1975.9915803 (1975).
Bandura, A. Social Foundations of Thought and Action23–28 (Englewood Cliffs, NJ, 1986).
Weinstein, N. D. Testing four competing theories of health-protective behavior. J. Health Psychol. 12 (4), 324. (1993).
Brewer, N. T. & Gilkey, M. B. Comparing theories of health behavior using data from longitudinal studies: a comment on gerend and shepherd. Ann. Behav. Med. 44 (2), 147–148. https://doi.org/10.1007/s12160-012-9396-z (2012).
Endersby, J. Lumpers and splitters: darwin, hooker, and the search for order. Science 326 (5959), 1496–1499. https://doi.org/10.1126/science.1165915 (2009).
Weinstein, N. D., Rothman, A. J. & Commentary Revitalizing research on health behavior theories. Health Educ. Res. 20 (3), 294–297. https://doi.org/10.1093/her/cyg125 (2005).
Brug, J., Aro, A. R. & Richardus, J. H. Risk perceptions and behaviour: towards pandemic control of emerging infectious diseases: international research on risk perception in the control of emerging infectious diseases. Int. J. Behav. Med. 16, 3–6. https://doi.org/10.1007/s12529-008-9000-x (2009).
Raude, J., McColl, K., Flamand, C. & Apostolidis, T. Understanding health behaviour changes in response to outbreaks: findings from a longitudinal study of a large epidemic of mosquito-borne disease. Soc. Sci. Med. 230, 184–193. https://doi.org/10.1016/j.socscimed.2019.04.009 (2019).
Xu, J. & Peng, Z. People at risk of influenza pandemics: the evolution of perception and behavior. PloS One. 10 (12), e0144868. https://doi.org/10.1371/journal.pone.0144868 (2015).
Weston, D., Ip, A. & Amlôt, R. Examining the application of behaviour change theories in the context of infectious disease outbreaks and emergency response: a review of reviews. BMC Public. Health. 20 (1), 1–19. https://doi.org/10.1186/s12889-020-09519-2 (2020).
Brewer, N. T., Weinstein, N. D., Cuite, C. L. & Herrington, J. E. Risk perceptions and their relation to risk behavior. Ann. Behav. Med. 27, 125–130. https://doi.org/10.1207/s15324796abm2702_7 (2004).
Sheeran, P., Harris, P. R. & Epton, T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol. Bull. 140 (2), 511. https://doi.org/10.1037/a0033065 (2014).
Murugan, S., Rajavel, S., Aggarwal, A. K. & Singh, A. Volatility, uncertainty, complexity and ambiguity (VUCA) in context of the COVID-19 pandemic: challenges and way forward. Int. J. Health Syst. Implement. Res. 4 (2), 10–16 (2020). https://ijhsir.ahsas-pgichd.org/index.php/ijhsir/article/view/93
Viscusi, W. K. A bayesian perspective on biases in risk perception. Econ. Lett. 17 (1–2), 59–62. https://doi.org/10.1016/0165-1765(85)90127-2 (1985).
Ward, C., Deardon, R. & Schmidt, A. M. Bayesian modeling of dynamic behavioral change during an epidemic. Infect. Dis. Model. 8 (4), 947–963. https://doi.org/10.1016/j.idm.2023.08.002 (2023).
Bottemanne, H. & Friston, K. J. An active inference account of protective behaviours during the COVID-19 pandemic. Cogn. Affect. Behav. Neurosci. 1–13. https://doi.org/10.3758/s13415-021-00947-0 (2021).
Scholz, U. & Freund, A. M. Determinants of protective behaviours during a nationwide lockdown in the wake of the COVID-19 pandemic. Br. J. Health Psychol. 26 (3), 935–957. https://doi.org/10.1111/bjhp.12513 (2021).
Qin, H., Sanders, C., Prasetyo, Y., Syukron, M. & Prentice, E. Exploring the dynamic relationships between risk perception and behavior in response to the coronavirus disease 2019 (COVID-19) outbreak. Soc. Sci. Med. 285, 114267. https://doi.org/10.1016/j.socscimed.2021.114267 (2021).
Wambua, J. et al. The influence of risk perceptions on close contact frequency during the SARS-CoV-2 pandemic. Sci. Rep. 12 (1), 5192. https://doi.org/10.1038/s41598-022-09037-8 (2022).
Fullerton, M. K., Rabb, N., Mamidipaka, S., Ungar, L. & Sloman, S. A. Evidence against risk as a motivating driver of COVID-19 preventive behaviors in the united States. J. Health Psychol. 27 (9), 2129–2146. https://doi.org/10.1177/13591053211024726 (2022).
Zickfeld, J. H., Schubert, T. W., Herting, A. K., Grahe, J. & Faasse, K. Correlates of health-protective behavior during the initial days of the COVID-19 outbreak in Norway. Front. Psychol. 11, 564083. https://doi.org/10.3389/fpsyg.2020.564083 (2020).
Martin-Lapoirie, D., McColl, K., Gallopel-Morvan, K., Arwidson, P. & Raude, J. Health protective behaviours during the COVID-19 pandemic: risk adaptation or habituation? Soc. Sci. Med. 342, 116531. https://doi.org/10.1016/j.socscimed.2023.116531 (2024).
Petherick, A. et al. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Hum. Behav. 5 (9), 1145–1160. https://doi.org/10.1038/s41562-021-01181-x (2021).
Lee, Y. H. et al. The association between the risk perceptions of COVID-19, trust in the government, political ideologies, and socio-demographic factors: A year-long cross-sectional study in South Korea. Plos One. 18 (6), e0280779. https://doi.org/10.1371/journal.pone.0280779 (2023).
Weinstein, N. D., Rothman, A. J. & Nicolich, M. Use of correlational data to examine the effects of risk perceptions on precautionary behavior. Psychol. Health. 13 (3), 479–501. https://doi.org/10.1080/08870449808407305 (1998).
Cipolletta, S., Andreghetti, G. R. & Mioni, G. Risk perception towards COVID-19: A systematic review and qualitative synthesis. Int. J. Environ. Res. Public. Health. 19 (8), 4649. https://doi.org/10.3390/ijerph19084649 (2022).
Trifiletti, E., Shamloo, S. E., Faccini, M. & Zaka, A. Psychological predictors of protective behaviours during the Covid-19 pandemic: theory of planned behaviour and risk perception. J. Community Appl. Soc. Psychol. 32 (3), 382–397. https://doi.org/10.1002/casp.2509 (2022).
Bronfman, N. C., Repetto, P. B., Cisternas, P. C. & Castañeda, J. V. Factors influencing the adoption of COVID-19 preventive behaviors in Chile. Sustainability 13 (10), 5331. https://doi.org/10.3390/su13105331 (2021).
Jandawapee, S., Siripipatthanakul, S., Phayaphrom, B. & Limna, P. Factors influencing intention to follow the preventive COVID-19 protocols among Thai people. Int. J. Behav. Analytics. 2 (1), 1–15 (2022). https://ssrn.com/abstract=4021365
Rubin, G. J., Potts, H. W. & Michie, S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 National telephone surveys in the UK. Health Technol. Assess. 14 (34), 183–266. https://doi.org/10.3310/hta14340-03 (2010).
Aschwanden, D. et al. Preventive behaviors during the COVID-19 pandemic: associations with perceived behavioral control, attitudes, and subjective norm. Front. Public. Health. 9, 662835. https://doi.org/10.3389/fpubh.2021.662835 (2021).
Schumpe, B. M. et al. Predictors of adherence to public health behaviors for fighting COVID-19 derived from longitudinal data. Sci. Rep. 12 (1), 3824. https://doi.org/10.1038/s41598-021-04703-9 (2022).
Sheeran, P. et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. J. Health Psychol. 35 (11), 1178. https://doi.org/10.1037/hea0000387 (2016).
Wong, L. P. & Sam, I. C. Temporal changes in psychobehavioral responses during the 2009 H1N1 influenza pandemic. Prev. Med. 51 (1), 92–93. https://doi.org/10.1016/j.ypmed.2010.04.010 (2010).
Martin-Lapoirie, D., D’Onofrio, A., McColl, K. & Raude, J. Testing a simple and frugal model of health protective behaviour in epidemic times. Epidemics 42, 100658. https://doi.org/10.1016/j.epidem.2022.100658 (2023).
O’Connell, C. P. et al. When do people increase COVID-19 protective behaviors? A longitudinal analysis of the impact of infections among close contacts and in the community. Prev. Med. Rep. 34, 102251. https://doi.org/10.1016/j.pmedr.2023.102251 (2023).
Hale, T. et al. A global panel database of pandemic policies (Oxford COVID-19 government response Tracker). Nat. Hum. Behav. 5 (4), 529–538. https://doi.org/10.1038/s41562-021-01079-8 (2021).
American Psychological Association. APA Dictionary of Psychology: context. March (2018). https://dictionary.apa.org/context (9.
American Psychological Association. APA Dictionary of Psychology: epidemic. November (2023). https://dictionary.apa.org/epidemic (15.
Institut National de la Statistique et des Études Économiques. Statistics and Studies: France, Social Portrait. The Covid-19 pandemic: 4 waves, 116 deaths and severe consequences for the healthcare system. Institut National de la Statistique et des Études Économiques (INSEE) (2021). https://www.insee.fr/en/statistiques/6438589?sommaire=6438617 (20 March 2021).
Heck, R. H., Thomas, S. L. & Tabata, L. N. Multilevel and Longitudinal Modeling with IBM SPSS (Routledge, 2013).
Smith, L. E. et al. Engagement with protective behaviours in the UK during the COVID-19 pandemic: a series of cross-sectional surveys (the COVID-19 rapid survey of adherence to interventions and responses [CORSAIR] study). BMC Public. Health. 22 (1), 1–11. https://doi.org/10.1186/s12889-022-12777-x (2022).
Salgado, M. et al. Environmental determinants of population health in urban settings. A systematic review. BMC Public. Health. 20, 1–11. https://doi.org/10.1186/s12889-020-08905-0 (2020).
Heiman, S. L. et al. Descriptive norms caused increases in mask wearing during the COVID-19 pandemic. Sci. Rep. 13 (1), 11856. https://doi.org/10.1038/s41598-023-38593-w (2023).
Latkin, C. A. et al. Social norms and prevention behaviors in the united States early in the COVID-19 pandemic. Psychol. Health Med. 27 (1), 162–177. https://doi.org/10.1080/13548506.2021.2004315 (2022).
Gupta, D. & Rudisill, C. Timing of preventive behavior in the case of a new and evolving health risk: the case of COVID-19 vaccination. Health Econ. Rev. 14 (16). https://doi.org/10.1186/s13561-024-00484-9 (2024).
Choi, D. H. & Noh, G. Y. The impact of social media on preventive behavior during the COVID-19 outbreak in South korea: the roles of social norms and Self-Efficacy. Sage Open. 13 (3), 21582440231184969. https://doi.org/10.1177/21582440231184969 (2023).
Dryhurst, S. et al. Risk perceptions of COVID-19 around the world. J. Risk Res. 23 (7–8), 994–1006. https://doi.org/10.1080/13669877.2020.1758193 (2020).
Siegrist, M. & Bearth, A. Worldviews, trust, and risk perceptions shape public acceptance of COVID-19 public health measures. Proc. Nat. Acad. Sci. 118(24), e2100411118; (2021). https://doi.org/10.1073/pnas.2100411118
Betsch, C. et al. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc. Natl. Acad. Sci. 117 (36), 21851–21853. https://doi.org/10.1073/pnas.2011674117 (2020).
Coroiu, A., Moran, C., Campbell, T. & Geller, A. C. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PloS One. 15 (10), e0239795. https://doi.org/10.1371/journal.pone.0239795 (2020).
Dinić, B. M. & Bodroža, B. COVID-19 protective behaviors are forms of prosocial and unselfish behaviors. Front. Psychol. 1128 https://doi.org/10.3389/fpsyg.2021.647710 (2021).
Liekefett, L. & Becker, J. Compliance with governmental restrictions during the coronavirus pandemic: A matter of personal self-protection or solidarity with people in risk groups? Br. J. Soc. Psychol. 60 (3), 924–946. https://doi.org/10.1111/bjso.12439 (2021).
Neumann-Böhme, S., Sabat, I. & Attema, A. E. Altruism and the link to pro-social pandemic behavior. Front. Health Serv. 2, 871891. https://doi.org/10.3389/frhs.2022.871891 (2022).
Pfattheicher, S., Petersen, M. B. & Böhm, R. Information about herd immunity through vaccination and empathy promote COVID-19 vaccination intentions. J. Health Psychol. 41 (2), 85. https://doi.org/10.1037/hea0001096 (2022).
Ayre, J. et al. Contextualising COVID-19 prevention behaviour over time in australia: patterns and long-term predictors from April to July 2020 in an online social media sample. PLoS One. 16 (6), e0253930. https://doi.org/10.1371/journal.pone.0253930 (2021).
Scholz, U., Bermudez, T. & Freund, A. M. COVID-19 protective behaviors: A longitudinal study applying an extended protection motivation theory. J. Health Psychol. 42 (11), 822–834. https://doi.org/10.1037/hea0001322 (2023).
Moussaoui, L. S., Ofosu, N. D. & Desrichard, O. Social psychological correlates of protective behaviours in the COVID-19 outbreak: evidence and recommendations from a nationally representative sample. Appl. Psychol. : Health Well-Being. 12 (4), 1183–1204. https://doi.org/10.1111/aphw.12235 (2020).
Hagger, M. S. & Hamilton, K. Social cognition theories and behavior change in COVID-19: A conceptual review. Behav. Res. Ther. 104095; (2022). https://doi.org/10.1016/j.brat.2022.104095
Hagger, M. S., Smith, S. R., Keech, J. J., Moyers, S. A. & Hamilton, K. Predicting social distancing intention and behavior during the COVID-19 pandemic: an integrated social cognition model. Ann. Behav. Med. 54 (10), 713–727. https://doi.org/10.1093/abm/kaaa073 (2020).
Campos-Mercade, P., Meier, A. N., Schneider, F. H. & Wengström, E. Prosociality predicts health behaviors during the COVID-19 pandemic. J. Public. Econ. 195, 104367. https://doi.org/10.1016/j.jpubeco.2021.104367 (2021).
Lau, H. et al. Evaluating the massive underreporting and undertesting of COVID-19 cases in multiple global epicenters. Pulmonology 27 (2), 110–115. https://doi.org/10.1016/j.pulmoe.2020.05.015 (2021).
Slovic, P. Perception of risk. Science 236 (4799), 280–285. https://doi.org/10.1126/science.3563507 (1987).
Berrigan, D. et al. Uncertainty: a neglected determinant of health behavior? Front. Psychol. 14, 1145879. https://doi.org/10.3389/fpsyg.2023.1145879 (2023).
Orom, H. et al. Causes and consequences of uncertainty about illness risk perceptions. J. Health Psychol. 25 (8), 1030–1042. https://doi.org/10.1177/1359105317745966 (2020).
Kerr, J. R. et al. Correlates of intended COVID-19 vaccine acceptance across time and countries: results from a series of cross-sectional surveys. BMJ Open. 11 (8), e048025. https://doi.org/10.1136/bmjopen-2020-048025 (2021).
Sobkow, A., Zaleskiewicz, T., Petrova, D., Garcia-Retamero, R. & Traczyk, J. Worry, risk perception, and controllability predict intentions toward COVID-19 preventive behaviors. Front. Psychol. 11, 582720. https://doi.org/10.3389/fpsyg.2020.582720 (2020).
Vacondio, M., Priolo, G., Dickert, S. & Bonini, N. Worry, perceived threat and media communication as predictors of self-protective behaviors during the COVID-19 outbreak in Europe. Front. Psychol. 12, 577992. https://doi.org/10.3389/fpsyg.2021.577992 (2021).
Harper, C. A., Satchell, L. P., Fido, D. & Latzman, R. D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment Health Addict. 19, 1875–1888. https://doi.org/10.1007/s11469-020-00281-5 (2021).
Jørgensen, F., Bor, A. & Petersen, M. B. Compliance without fear: Individual-level protective behaviour during the first wave of the COVID‐19 pandemic. Br. J. Health Psychol. 26 (2), 679–696. https://doi.org/10.1111/bjhp.12519 (2021).
Abraham, C., Sheeran, P. & Henderson, M. Extending social cognition models of health behaviour. Health Educ. Res. 26 (4), 624–637. https://doi.org/10.1093/her/cyr018 (2011).
Golden, S. D. & Earp, J. A. L. Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Health Educ. Behav. 39 (3), 364–372. https://doi.org/10.1177/1090198111418634 (2012).
Lazarus, R. S. & Folkman, S. Stress, Appraisal, and Coping (Springer Publishing Company, 1984).
Fisher, E. B. The importance of context in Understanding behavior and promoting health. Ann. Behav. Med. 35 (1), 3–18. https://doi.org/10.1007/s12160-007-9001-z (2008).
Michie, S., Rothman, A. J. & Sheeran, P. Current issues and new direction in psychology and health: advancing the science of behavior change. Psychol. Health. 22 (3), 249–253. https://doi.org/10.1080/14768320701233582 (2007).
Conner, M. & Norman, P. Predicting and changing health behaviour: A social cognition approach. Predicting and changing health behaviour: Research and practice with social cognition models, 3, 1–29 (McGraw-Hill Education (UK), (2015).
Armitage, C. J. & Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 40 (4), 471–499. https://doi.org/10.1348/014466601164939 (2001).
Chevance, G., Perski, O. & Hekler, E. B. Innovative methods for observing and changing complex health behaviors: four propositions. Trans. Behav. Med. 11 (2), 676–685. https://doi.org/10.1093/tbm/ibaa026 (2021).
Badham, J. & Gilbert, N. TELL ME design: Protective behaviour during an epidemic [CRESS Working Paper 2]. The University of Surrey (2015). http://cress.soc.surrey.ac.uk/web/publications/working-papers/tell-me-design-protective-behaviour-during-epidemic
Sapsford, R. Survey Research 1-296 (Sage, 2006).
Bartlett, F. C. Remembering: A Study in Experimental and Social Psychology (Cambridge University Press, 1995).
Weinstein, N. D., Marcus, S. E. & Moser, R. P. Smokers’ unrealistic optimism about their risk. Tob. Control. 14 (1), 55–59. https://doi.org/10.1136/tc.2004.008375 (2005).
Jensen, U. T. Is self-reported social distancing susceptible to social desirability bias? Using the crosswise model to elicit sensitive behaviors. J. Behav. Pub Admin. 3 (2). https://doi.org/10.30636/jbpa.32.182 (2020).
Institut National de la Statistique et des Études Économiques. Statistiques et Études: Bilan démographique 2016. Institut National de la Statistique et des Études Économiques (INSEE) https://www.insee.fr/fr/statistiques/2554860#:~:text=Au%201er%20janvier%202017,hausse%20de%200%2C4%20%25 (17 January 2017).
World Medical Association. World medical association declaration of Helsinki ethical principles for medical research involving human subjects. JAMA: J. Am. Med. Assoc. 310 (20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Brewer, N. T. et al. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. J. Health Psychol. 26 (2), 136. https://doi.org/10.1037/0278-6133.26.2.136 (2007).
Acknowledgements
The authors are grateful to Dr Pierre Arwidson and the COVIPREV group from the Department of Health Promotion and Prevention (Santé Publique France), and to the members of the ACMÉ consortium.
Funding
This work was supported by Santé Publique France (Public Health France) under Grant [number 21DPPA046-0]; the ACMÉ Project (Améliorer l’acceptabilité et l’accessibilité des Contre-Mesures préventives dont les vaccins lors d’émergences Épidémiques) designed to improve the acceptability and accessibility of preventive measures, including but not limited to vaccination, in response to epidemics of emerging infectious diseases, under Grant ANRS-23-PEPR-MIE-0011.
Author information
Authors and Affiliations
Contributions
K.M. and J.R. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in compliance with the French national guidelines for ethical research in the social and human sciences. The research was declared to the EHESP School of Public Health Office for Personal Data Protection (Rennes, France) [Reference: MR 2510110520], and approved by the ethics committee of the University Hospital Institute, Méditerranée Infection (Marseille France) [Decision No. 2020-022]. Informed consent was obtained from participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
McColl, K., Mueller, J., Martin-Lapoirie, D. et al. Understanding the interplay between epidemiological and social cognitive drivers of behaviour change during the Covid-19 pandemic. Sci Rep 15, 30556 (2025). https://doi.org/10.1038/s41598-025-14644-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-14644-2