Abstract
The global prevalence of depression continues to rise, making it a leading cause of suicide. Although evidence-based treatments for mental disorders exist, over 75% of affected individuals in low- and middle-income countries lack access to care. Consequently, cost-effective exercise interventions are increasingly recognized as viable therapeutic options. However, conclusive evidence comparing the relative efficacy and acceptability of different exercise modalities for alleviating depressive symptoms remains lacking. Therefore, this study employed a network meta-analysis to directly compare the relative efficacy and acceptability of various exercise interventions for individuals with depression. Adhering to PRISMA-NMA guidelines, a comprehensive literature search was conducted across seven electronic databases (PubMed, Cochrane Library, PsycINFO, Embase, CNKI, MEDLINE, and Web of Science) to identify randomized controlled trials (RCTs) examining exercise interventions for depression.Studies meeting the predefined inclusion criteria were selected for analysis.Methodological quality and risk of bias of the included studies were evaluated using the Cochrane Handbook for Systematic Reviews of Interventions (Version 5.1).The quality of evidence derived from the network meta-analysis was assessed using the Confidence in Network Meta-Analysis (CINeMA) framework. Network meta-analysis was performed using Stata software (version 17.0). The final analysis included 58 articles (encompassing 62 RCTs) with a total of 3,751 participants, evaluating three exercise categories: aerobic exercise, mind-body exercise, and resistance training. All three exercise modalities showed significantly greater antidepressant efficacy than control conditions (routine control, control condition, waiting list), with statistical significance (P < 0.05). Notably, mind-body exercise (SMD: -0.43, 95% CI [-0.82, -0.04], P < 0.05) demonstrated superior efficacy in alleviating adult depression compared to aerobic exercise. The efficacy ranking for depression relief was: mind-body exercise (94.1%) > resistance training (81.0%) > aerobic exercise (63.9%). Regarding acceptability, the ranking was aerobic exercise (67.1%) > mind-body exercise (61.5%) > resistance training (39.3%). Subgroup analysis indicated that mind-body exercise consistently ranked highest in efficacy for depression intervention, regardless of intervention duration. Specifically, mind-body exercise ranked first across all durations: >4 to ≤ 8 weeks (86.9%), > 9 to ≤ 12 weeks (83.2%), and > 12 weeks (98.5%). Mind-body exercises demonstrated superior efficacy relative to other interventions for individuals with depression, yet its acceptability was marginally lower than that of aerobic exercise. Further rigorous studies are necessary to confirm this finding.
Similar content being viewed by others
Introduction
Depression is a prevalent and debilitating condition that significantly impacts patients’ quality of life and overall health1,2. In 2017, the World Health Organization (WHO) reported that the global annual incidence of depression is approximately 4.4%, with over 300 million individuals affected by varying degrees of the condition3. The incidence of depression increased by approximately 27.6%4,5,6,7 during the COVID-19 pandemic and is projected to become the leading global disease burden by 20308. The primary treatments in clinical practice include antidepressant medications and psychotherapy; however, their limitations have become increasingly apparent9. Antidepressant medications are often associated with side effects and relapses, manifesting as withdrawal symptoms including nausea, vomiting, insomnia, seizures, and other adverse reactions. As depression severity increases, the risk of suicide attempts, significant impairment in social functioning, and a chronic disease course may escalate10. Although psychotherapy does not carry the adverse effects of medications, it is time-consuming, expensive, and yields a remission rate of only 50%11. Consequently, medical professionals and researchers must urgently explore alternative treatments that are simple, effective, cost-efficient, and safe, while also reducing the disease course.
The “Healthy China 2030” Plan outlines strategies to improve the physical fitness of the entire population through national fitness campaigns, integration of physical and medical health services, non-medical interventions, and promotion of physical activity among key demographic groups12. Exercise is recommended as an adjunctive therapy for depression in the WHO Guidelines on Physical Activity and Sedentary Behaviour13. Exercise therapy, a non-pharmacological treatment for depression, has gained widespread recognition among psychiatrists and researchers due to its low cost, ease of implementation, high adherence rates, and minimal adverse effects14. Research indicates that exercise therapy may influence neurogenesis and brain remodeling through the modulation of neurobiochemical levels and inhibition of inflammatory and apoptotic pathways, thereby producing antidepressant effects similar to those of pharmacological treatments14. Several meta-analyses have demonstrated the positive effects of various exercise modalities on alleviating depressive symptoms15-18.
The primary exercise modalities include aerobic exercise, mind-body exercise, and resistance training. Aerobic exercise, characterized by physical activity performed with adequate oxygen intake19engages large muscle groups and allows for the modulation of intensity based on the individual’s preferred pace. Common activities include walking, jogging, and running. Mind-body exercise, in contrast, is a distinct form of physical activity that emphasizes the dynamic interaction between the brain, mind, body, and behavior, highlighting the influence of psychological factors on physiological health. Notable examples of mind-body exercises include yoga, Pilates, Tai Chi, and qigong20which are characterized by relatively low intensity and MET values ranging from 1.5 to 421. Resistance training, in contrast, involves exercises performed against resistance, typically using equipment such as push-ups, dumbbells, and barbells22. Unlike aerobic and mind-body exercises, resistance training focuses on repeatedly overloading muscles through static, isometric, or dynamic contractions, establishing a stronger connection between muscle tissue and the nervous system. Most current studies on adult patients with depression have either conducted meta-analyses on the effects of aerobic exercise23mind-body exercise24and resistance training25,26or failed to differentiate between exercise types when analyzing their effects27. Few studies have directly compared the efficacy of aerobic exercise and resistance training in patients with depression18,28 making it challenging to distinguish the antidepressant effects of these exercise modalities. Additionally, a significant proportion of existing studies have conflated patients with depressive tendencies with those clinically diagnosed with depression, as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD). This methodological limitation may introduce bias, leading to inaccurate conclusions about the comparative efficacy and acceptability of these exercise modalities. Therefore, this study aims to perform a network meta-analysis to compare the antidepressant efficacy and acceptability of three common exercise modalities (aerobic exercise, mind-body exercise, and resistance training) in patients with clinically diagnosed depression.
Methods
Network meta-analysis is performed according to the preferred reporting items in the System Review and Metaanalysis (PRISMA) guide29. (PROSPERO: CRD42023424536).
Literature search strategy
A literature search team was first established. Subsequently, two researchers independently conducted searches in the China National Knowledge Infrastructure (CNKI), PubMed, Cochrane, Embase, Web of Science, PsycINFO, and Medline databases. The search focused on published Clinical Randomized Controlled Trials (RCTs) regarding exercise interventions for depression. The search period extended from the inception of each database until January 8, 2025. Search terms included variations of “Exercise,” “Walk,” “Jogging,” “Hiking,” “Swim,” “Aquatic,” “Cycling,” “Bicycling,” “Concurrent Training,” “Cross Training,” “Functional Training,” “Resistance Training,” “Aerobic,” “Qigong,” “Mind-Body Exercise,” “Tai Chi,” “Baduanjin,” “Wuqinxi,” “Yijinjing,” “Yoga,” “Pilates,” “Depression,” “Depressive Disorder,” and “Randomized Controlled Trial.” The search terms were adapted for each database using appropriate subject terms such as MeSH (PubMed) and Emtree (EMBASE), in addition to free-text terms. An example of the PubMed search strategy is provided in Table 1.
Inclusion and exclusion criteria
Inclusion criteria: (1)The study design must be a randomized controlled trial (RCT) with publicly available literature for complete data collection; (2)Participants must meet diagnostic criteria such as the Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD-3), Diagnostic and Statistical Manual of Mental Disorders (DSM-IV or DSM-5), International Classification of Diseases (ICD-10), or DSM-V, or be adults aged 18 or older who have been identified as having depressive symptoms above a certain threshold through validated screening tools (e.g., Beck Depression Inventory (BDI) or Hamilton Depression Scale (HAM-D); no restrictions based on nationality, race, gender, illness duration, or comorbid symptoms; (3)The intervention should involve exercise therapy, including aerobic exercise, resistance training, and mind-body exercises, with the control group receiving standard care, control conditions, or placed on a waitlist. Refer to Table 2 for precise definitions.
Exclusion criteria: (1)The study design was not a randomized controlled trial (RCT), case report, famous doctor experience, book report, animal test, or studies in which the intervention period was less than four weeks; (2)Subjects were minors (≤ 18 years old); (3)Patients lacked baseline clinical depression or were only possibly diagnosed with depression; (4)The intervention was a combined intervention or could not be fully classified as aerobic exercise, resistance training, or mind-body exercise; (5) The results of the study were unclear or the data were incomplete.
Literature screening and data extraction
The articles retrieved from various databases were imported into EndNote 20 software for duplicate title searches, and any duplicates were removed. Three researchers independently screened potential articles based on the title, abstract, and full text to identify those that met the inclusion criteria, forming a final list by consensus. If the full text of any article was unavailable, the corresponding author was contacted to provide it. Five researchers evaluated the articles for compliance, resolving any disagreements through discussion. Data extraction was performed using Excel, including: (1) Basic information (first author, year of publication, country); (2) Patient information (diagnostic criteria, age, gender, sample size); (3) Trial details (diagnostic tools, interventions, intervention duration); (4) Outcome measures (symptom relief score, acceptability); and (5) Information regarding the quality assessment of the included studies.
Quality assessment
The methodological quality of the literature was assessed according to the Cochrane Handbook for Systematic Reviews of Interventions version 5.130.The assessment included: (1)Random sequence generation; (2)Allocation concealment; (3) Blinding of participants and personnel; (4)Blinding of outcome assessors; (5)Selective reporting of outcomes; (6)Incomplete outcome data; (7)Other sources of bias. The risk of each bias item was assessed as low, unclear, or high risk based on the trial report. Two investigators independently assessed the risk of bias in each study and reached consensus through discussion when disagreements arose. If a dispute persisted, it was resolved through consultation with a third researcher.
Outcome indicators
(1)Symptom relief score (presented by the endpoint depression scale scores for depressive symptoms in response to the exercise intervention); (2)acceptability (using the number of participants who withdrew from the study before the end of the intervention period as a measure of acceptability).
Statistical analyses
In this study, the quality of the included studies was assessed using RevMan 5.4, and frequency-based reticulated meta-analysis was performed using Stata 17. Due to significant variations in evaluation tools (e.g., scale items, scoring criteria) across the individual studies, primary outcome results were pooled using the standardized mean difference (SMD), while secondary outcome results were pooled using the odds ratio (OR). In the reticulated meta-analysis, consistency was tested using the point score method. A P-value greater than 0.05 indicates that the difference between direct and indirect comparisons was not statistically significant. When a closed-loop structure exists between interventions, both global and local inconsistency tests were conducted. A lower limit of the 95% confidence interval (CI) for the inconsistency factor (IF) at or near 0 suggests strong agreement between direct and indirect comparison results31. The results of indirect comparisons in the reticulated meta-analysis were interpreted using effect sizes and 95% confidence intervals (95% CIs). This study ranks the likelihood of each intervention by integrating both the effect size and the Surface Under the Cumulative Ranking Curve (SUCRA) plot. The SUCRA value is a statistical measure used to compare the relative effectiveness of multiple interventions. The intervention effect is assessed by ranking the effects of different intervention groups and calculating the average percentage of the area under the cumulative ranking curve for each intervention group32. Publication bias was evaluated using funnel plots, with the Egger test conducted for additional validation. Evidence certainty in the network meta-analysis was appraised via the Confidence in Network Meta-Analysis (CINeMA) framework.
Results
Literature selection
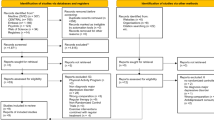
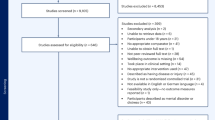
By searching CNKI (n = 251), PsyclNFO (n = 728), PubMed (n = 1138), Embase (n = 3268), Cochrane (n = 2904), Web of Science (n = 2129), Medline (n = 1905), a total of 12,323 documents were obtained. After removing duplicates, 6692 pieces of eligible literature remained. Initial screening of titles and abstracts narrowed it down to 813 articles. After full-text assessment, 755 articles were excluded for not meeting the inclusion criteria, resulting in a final inclusion of 58 articles33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89. A visual representation of the search results can be found in the PRISMA fow chart in Fig. 1.
Characteristics of the included studies
Four of the 58 studies were three-arm studies, while the remaining studies were two-arm studies, encompassing a total of 3751 participants, with 1790 in the experimental group and 1961 in the control group. Participants were assigned to experimental and control groups based on the principle of randomization. The experimental group included 62 distinct treatment protocols representing different exercise modalities (aerobic, mind-body, and resistance training), with 27 protocols for aerobic, 28 for mind-body, and 8 for resistance training. The control group consisted of 29 conventional control protocols, 1 control condition, and 10 waiting list protocols. The basic characteristics of the included studies are presented in Table 3.
Result of assessment
A total of 58 studies were included in the analysis, all of which referenced the term “random”. Among these, one study employed the lottery method68while seven studies used the random number table method35,49,67,70,83,88. Study 16 employed a computerised randomisation process33,37,39,42,44,47,53,54,55,57,58,64,while four studies used a randomized block method36,40,51,63.The remaining studies did not specify the randomization method employed. The distribution of studies is as follows: 10 studies mention centre33,35,39,44,45,46,51,63,68,70while 4 studies mention opaque envelopes54,55,66,75.The remaining studies do not mention allocation concealment. Additionally, blinding was mentioned in only two studies, specifically regarding the outcome measure blinding37while the remaining studies did not address blinding of subjects, experimenters, or outcome measures. Regarding data completeness, two patients were lost to follow-up at a rate exceeding 20%73,75, while the remaining studies were within the acceptable range. The extent of selective reporting of study results, along with other potential sources of bias, remains unclear.
Credibility assessment
The quality of evidence in the network meta-analysis was evaluated using the Confidence in Network Meta-Analysis (CINeMA) framework. This assessment covered six domains: within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. Evidence quality was categorized into four levels: high, moderate, low, or very low. For efficacy outcomes, evidence across intervention comparisons was judged moderate. Regarding acceptability, evidence quality ranged from high to low, depending on specific comparisons. Key factors influencing these ratings included: (1) inadequate reporting of randomization procedures, blinding, or allocation concealment in some studies, elevating bias risk; (2) variability in diagnostic criteria, treatment duration, and sample sizes across studies, potentially impacting result consistency and precision; and (3) moderate heterogeneity contributing to lower overall evidence quality assessments.
Results of reticulation Meta-analysis
Evidence networks and inconsistency analysis
The two closed rings in Fig. 2 represent efficacy (symptom relief score) and acceptability for the respective interventions. In the relationship between interventions, the dots represent the exercise intervention modality, the area of the dots indicates sample size, and the connecting lines between dots signify a direct comparison between interventions. A thicker connecting line indicates a larger number of studies. The absence of a connecting line between two interventions indicates no direct comparison; these interventions can be compared indirectly using network meta-analysis. Refer to Fig. 3 for a diagram illustrating the evidence network.
The overall inconsistency test indicated that both efficacy (symptom relief score) and acceptability for each outcome index had P-values > 0.05, with low heterogeneity, indicating good overall consistency. The consistency of each closed loop was further assessed. The IF values for each intervention ranged from 0.17 to 0.59, with the lower limit of the 95% CI including 0. The acceptability of each intervention showed IF values ranging from 0.05 to 1.33, with the lower limit of the 95% CI including 0, indicating good consistency for each closed loop, thereby justifying the use of the consistency model for analysis.
Comparison of efficacy between interventions
Sixty-two studies assessed the efficacy of each intervention. A comparison was conducted between the antidepressant efficacy of three exercise modalities (aerobic exercise, mind-body exercise, and resistance training) and the control group (conventional control, control condition, and waiting list) (Table 4). The antidepressant efficacy of the three exercise modalities was statistically significant (P < 0.05), suggesting a statistically significant difference (P < 0.05) in depression relief among patients. Aerobic exercise, mind-body exercise, and resistance training were significantly more effective than the control group. The difference between mind-body exercise (SMD: −0.43, 95% CI [−0.82, −0.04], P < 0.05) and aerobic exercise was statistically significant, suggesting that mind-body exercise was more effective in alleviating depression. No other pairwise comparisons were statistically significant. The cumulative probabilities from the network meta-analysis were as follows: mind-body exercise (94.1%), resistance training (81.0%), aerobic exercise (63.9%), control condition (30.5%), waiting list (23.9%), and conventional control (6.7%). A line chart illustrating the cumulative probabilities is shown in Fig. 4.
Comparison of acceptability between interventions
All 62 studies reported the acceptability of each intervention. The network meta-analysis revealed that the confidence interval for all pairwise comparisons of exercise methods included 1, indicating no statistically significant differences. The cumulative probabilities from the network meta-analysis were ranked as follows: aerobic exercise (67.1%), mind-body exercise (61.5%), resistance training (39.3%), control condition (20.5%), waiting list (65.5%), and conventional control (46.1%). A line chart illustrating the cumulative probabilities is presented in Fig. 5.
Subgroup analysis of the network meta-analysis
Subgroup analysis of the network meta-analysis was conducted based on the primary outcome, efficacy (symptom relief score). The 62 studies reported the intervention duration: 23 studies lasted between four and eight weeks, 29 studies between eight and 12 weeks, and 10 studies for more than 12 weeks. The subgroup analysis revealed that mind-body exercise was the most effective form of exercise intervention for depression, with efficacy percentages of 86.9% for 4–8 weeks, 83.2% for 9–12 weeks, and 98.5% for more than 12 weeks (Table 5).
Literature publication bias tests
LPublication bias in literature is typically assessed using comparison-corrected funnel plots when more than ten studies are included. The efficacy funnel plot revealed asymmetry, with several data points outside the inverted funnel, suggesting potential publication bias. In contrast, the acceptability funnel plot, after correction, showed a symmetrical distribution of studies around the midline, indicating a lower risk of publication bias. The dispersion of individual studies could be attributed to factors such as sample size and study quality (Fig. 6). As only the funnel plot method was employed, the analysis was relatively unidimensional, and the statistical effect was minimal. Therefore, the Egger test was conducted. The Egger test revealed significant publication bias (P = 0.000, p < 0.05). However, the Egger test for acceptability showed no significant publication bias (P = 0.243, p > 0.05).
Discussion
In recent years, exercise interventions have become increasingly prevalent in clinical settings for the prevention and treatment of depression. Aerobic exercise, mind-body exercise, and resistance training are three modalities recognized as effective adjuncts to non-pharmacological treatments. These approaches are valued for their low cost, convenience, high adherence rates, and minimal side effects14,90. Psychiatrists and researchers worldwide have increasingly acknowledged the benefits of these interventions. Mechanistic studies in both animals and humans have demonstrated that exercise can enhance the expression of PGC-1α in skeletal muscle, modulate peripheral kynurenine metabolism, regulate inflammatory responses, influence endocrine secretion, and affect neurotrophic factors, glucocorticoid hormone levels, CNS morphology, cytokine release, and hippocampal neurogenesis. These effects collectively stimulate the central nervous system (CNS) and alleviate depressive symptoms91,92. Such CNS stimulation parallels the biological actions of antidepressant medications14. Exercise may also provide neurogenic benefits that some pharmaceutical treatments do not, warranting further investigation. This study aimed to objectively assess the clinical efficacy and acceptability of various exercise modalities through a comprehensive meta-analysis of 65 clinical trials. The results show that exercise significantly reduces depression symptoms, with mind-body and physical exercises demonstrating the highest efficacy, while aerobic exercise has the greatest acceptability.
Antidepressant efficacy of different exercise modalities
Although exercise is a well-established treatment for depression, the comparative effectiveness of various exercise modalities remains contentious. This study aimed to evaluate the efficacy of different exercise modalities in managing depression, emphasizing the comparative advantages of mind-body exercises. The results demonstrated that mind-body exercises significantly improved adult depression symptoms, outperforming resistance training and aerobic exercise, which ranked subsequently. These effects are primarily explained by the unique physiological and psychological characteristics inherent to mind-body movements. A key attribute of mind-body exercise is its ability to induce relaxation, characterized by softness, slowness, and tranquility. This relaxation response has been shown to decrease sympathetic nervous system activity, facilitate cortical neuron rest, and protect against external stressors. Consequently, it alleviates internal anxiety and conflict, thereby reducing depressive symptoms93,94. The distinctive respiratory patterns inherent in mind-body exercises also warrant attention. Compared to other exercise forms, mind-body practices emphasize deep, slow, steady, and prolonged breathing. This breathing pattern has been demonstrated to improve circulation, enhance organ function, and modulate the autonomic nervous system95effectively alleviating emotional distress. Mind-body exercises also possess distinctive psychological attributes. Unlike other exercises, mind-body practices emphasize the integration of mental and physical processes through meditation, fostering holistic development96. This state is associated with increased alpha brain wave activity, which correlates with elevated endorphin and catecholamine levels, thereby mitigating depressive symptoms97,98. Notably, distinct mind-body exercises exhibit unique neurophysiological characteristics. For example, Tai Chi has been demonstrated to suppress left hemispheric activity while enhancing right hemispheric excitation, resulting in increased positive emotions and reduced depressive symptoms15.It is worth noting that this ranking both aligns with and diverges from findings reported in other studies. A 2019 network meta-analysis of elderly populations ranked exercise efficacy for depression improvement as mind-body exercise > aerobic exercise > resistance training99corroborating our findings that mind-body practices are superior in alleviating adult depression. Nevertheless, discrepancies exist between studies evaluating aerobic exercise and resistance training, likely stemming from subject heterogeneity across studies. For instance, Miller exclusively studied elderly participants, highlighting that most research accounts for the health status of older adults and special populations with muscle dysfunction. Conversely, among young and healthy individuals, low-intensity, short-duration resistance training shows poor compliance and challenges in sustaining regular adherence100,101. Consequently, resistance training appears less effective than aerobic exercise in alleviating depression. A network meta-analysis examining resistance, aerobic, and combined exercises in depressed patients found resistance training superior to aerobic exercise for young adults102consistent with our results. Subgroup analysis further identified mind-body exercise as the most effective intervention for depression, showing efficacy across durations > 4 to ≤ 8 weeks (86.9%), > 9 to ≤ 12 weeks (83.2%), and > 12 weeks (98.5%). These findings further substantiate the therapeutic advantages of mind-body exercises in treating adult depression.
Antidepressant acceptability of different exercise modalities
Aerobic exercise was found to be more acceptable than other exercise modalities, reflecting its superior preference among participants. This higher level of acceptability may be attributed to the simplicity of activities such as walking, running, and cycling, which comprised 72.4% of the studies examined in this review. Existing research suggests that initiating exercise with less complex activities can encourage initially reluctant individuals with depression to engage, thereby improving the effectiveness of interventions91. Nevertheless, this study focuses solely on acceptability and does not explore the specific factors that might explain the preference for one exercise modality over another. Furthermore, acceptability is likely influenced by factors such as exercise intensity, duration, and workload, highlighting the need for further research to confirm the study’s findings.
Limitations of this study
The application of network meta-analysis to evaluate the efficacy and acceptability of various exercise interventions for patients with depression is subject to several limitations: (1) In terms of study characteristics, more than 50% of participants in this review had comorbid somatic disorders, which introduced complexity due to variations in factors such as disease severity, gender, age, and clinical history (e.g., first vs. recurrent episodes), potentially leading to study heterogeneity; (2) With regard to study design, discrepancies exist in the assessment tools for depression, intervention settings, duration, intensity, frequency, and other parameters, which could affect the accuracy of the results; (3) During literature screening, this study exclusively searched electronic databases and did not include grey literature or sources other than Chinese and English publications. This limitation may have introduced database and language biases. Additionally, the study excluded combined interventions and non-randomized controlled trials, which may have further restricted the findings. Moreover, the inability to access the full text of some studies may have compromised the reliability of the results.
Summary
Limited evidence indicates that mind-body exercises may have superior antidepressant efficacy compared to other modalities, while aerobic exercises generally demonstrate higher acceptability. Given patient preferences and medical recommendations, interventions with proven efficacy should be prioritized in clinical practice. However, due to the limitations of current studies, future research should rigorously stratify subjects based on disease status and conduct robust clinical trials for validation.
Data availability
Due to the nature of this study, participants in this study did not agree to share their data publicly, so no supporting data are available. Data can be obtained from the corresponding author upon reasonable request.
References
Bromet, E. et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 9, 90 (2011).
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and National incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 392 (10159), 1789–1858 (2018).
Depression and other common mental disorders: global health estimates. 2017-02.
Allen, S. F., Stevenson, J., Lazuras, L. & Akram, U. The role of the COVID-19 pandemic in altered psychological well-being, mental health and sleep: an online cross-sectional study. Psychol. Health Med. 27 (2), 343–351 (2022).
González-Sanguino, C., Ausín, B., Castellanos, M. A., Saiz, J. & Muñoz, M. Mental health consequences of the Covid-19 outbreak in spain. A longitudinal study of the alarm situation and return to the new normality. Prog Neuropsychopharmacol. Biol. Psychiatry. 107, 110219 (2021).
Veldhuis, C. B. et al. Addressing the critical need for long-term mental health data during the COVID-19 pandemic: changes in mental health from April to September 2020. Prev. Med. 146, 106465 (2021).
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398 (10312), 1700–1712 (2021).
Friedrich, M. J. Depression is the leading cause of disability around the world. JAMA 317 (15), 1517 (2017).
Malhi, G. S. et al. The 2020 Royal Australian and new Zealand college of psychiatrists clinical practice guidelines for mood disorders. Aust N Z. J. Psychiatry. 55 (1), 7–117 (2021).
Niu YJ. Interpretation of drug therapy of Chinese guidelines for prevention and treatment of depression. Clin. Medication J. 16(05), 6–8. https://doi.org/10.3969/j.issn.1672-3384.2018.05.002 (2018).
Cuijpers P, Oud M, Karyotaki E, Noma H, Quero S, Cipriani A, Arroll B, Furukawa TA. Psychologic Treatment of Depression Compared With Pharmacotherapy and Combined Treatment in Primary Care: A Network Meta-Analysis. Ann Fam Med. 19(3), 262-270. https://doi.org/10.1370/afm.2676 (2021).
Central Committee of the Communist Party of China. State Council of the People’s Republic of China. Outline of the Healthy China 2030 Plan. 2016-10-25.
WHO guidelines. on physical activity and sedentary behaviour.2020-11-25.
Zhang, S. Y. & Li, C. B. Research progress of exercise therapy for depression disorder. J. Shanghai Jiaotong Univ. (Med. Sci.). 43(07), 916–922. https://doi.org/10.3969/j.issn.1674-8115.2023.07.014 (2023).
Morres, I. D. et al. Aerobic exercise for adult patients with major depressive disorder in mental health services: A systematic review and meta-analysis. Depress. Anxiety. 36 (1), 39–53 (2019).
Yang, J., Liang, Y., Qiu, Z. Y., Wu M. & Li, A. Q. Effects of Mind-body exercise on depression: A Meta-analysis. Chin. J. Rehabilitation Theory Pract. 25(11), 1260–1271. https://doi.org/10.3969/j.issn.1006?9771.2019.11.004 (2019).
Gordon, B. R. et al. Association of efficacy of resistance exercise training with depressive symptoms: Meta-analysis and Meta-regression analysis of randomized clinical trials. JAMA Psychiatry. 75 (6), 566–576 (2018).
Pérez Bedoya, É. A., Puerta-López, L. F., López Galvis, D. A., Rojas Jaimes, D. A. & Moreira, O. C. Physical exercise and major depressive disorder in adults: systematic review and meta-analysis. Sci. Rep. 13(1), 13223. https://doi.org/10.1038/s41598-023-39783-2 (2023).
Mersy, D. J. Health benefits of aerobic exercise. Postgrad. Med. 90 (1), 103 (1991).
Herrmann, S. D. et al. 2024 adult compendium of physical activities: A third update of the energy costs of human activities. J. Sport Health Sci. 13 (1), 6–12 (2024).
Zhang, N. N. The regulation of resistance training on glucose metabolism in impaired glucose tolerant elderly has nothing to do with the intensity of glucose metabolism. Genomics Appl. Biol. 37(05), 2243–2249. https://doi.org/10.13417/j.gab.037.002243 (2018).
La Forge, R. Mind-body fitness: encouraging prospects for primary and secondary prevention. J. Cardiovasc. Nurs. 11 (3), 53–65 (1997).
Xia, J. & Han, J. S. Meta Analysis about Effects of Aerobic Exercise on Mood State of the Elderly. Sichuan Sport. Sci. 41(02), 73–76. https://doi.org/10.13932/j.cnki.sctykx.2022.02.16 (2022).
Dong, Y. et al. The effects of mind-body exercise on anxiety and depression in older adults: a systematic review and network meta-analysis. Front. Psychiatry. 15, 1305295 (2024).
Khodadad Kashi, S., Mirzazadeh, Z. S., Saatchian, V. A. & Systematic Review Meta-Analysis of resistance training on quality of life, depression, muscle strength, and functional exercise capacity in older adults aged 60 years or more. Biol. Res. Nurs. 25 (1), 88–106 (2023).
Cunha, P. M. et al. Can resistance training improve mental health outcomes in older adults? A systematic review and meta-analysis of randomized controlled trials. Psychiatry Res. 333, 115746 (2024).
Yu, P., Huang, X. X. & Cao, B. H.,Meta analysis of the promoting effect of physical activity on college students’ mental health underthe background of public health emergency. China J. Health Psychol. 32(03), 460–467. https://doi.org/10.13342/j.cnki.cjhp.2024.03.025 (2024).
Heissel, A. et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br. J. Sports Med. 57 (16), 1049–1057 (2023).
Fang C, Deng W, Fan JC, Zeng XT. Platforms for systematic review and meta-analysis registration:a briefly introduction. J. Tongji University (Medical Science) 40(3), 380. https://doi.org/10.16118/j.1008-0392.2019.03.022 (2019).
Wang, Y. Introduction to the Cochrane bias risk assessment tool. Chin. Gen. Practice 22(11), 1322. https://kns.cnki.net/nzkhtml/xmlRead/trialRead.html?dbCode=CJFD&tableName=CJFDTOTAL&fileName=QKYX201911019&fileSourceType=1&appId=KNS_BASIC_PSMC&invoice=D76neEsfuHLB4UT/fzoiCqlXalTc4+QwpKaEIajmCqIXrf1XVcLcUTQNOIJraqVB1A07P0zY8A+417lE9LRaydPeSwnsljXmmrONXHCnysG3N9Cg/rmVhsygHrswqdmjCi6z46KwkIsVs+LVUei0EJWy5z8iNDT4tEdvkw3TUAU= (2019).
Zhang C, Yan JZ,Sun F,Liu Q, Guo Y,Zeng XT. Differentiation and handling of homogeneity in network Meta-analysis. Chin. J. Evidence-Based Medicine 14(7), 884–888. https://doi.org/10.7507/1672-2531.20140146 (2014).
Salanti, G., Ades, A. E. & Ioannidis, J. P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J. Clin. Epidemiol. 64 (2), 163–171 (2011).
Belvederi Murri, M. et al. Safety and efficacy of exercise for depression in seniors (SEEDS) study group. Physical exercise for late-life major depression. Br. J. Psychiatry. 207 (3), 235–242 (2015).
Bieber, M. et al. Effects of body-oriented yoga: a RCT study for patients with major depressive disorder. Eur. Arch. Psychiatry Clin. Neurosci. 271 (7), 1217–1229 (2021).
Bressington, D. et al. Feasibility of a group-based laughter yoga intervention as an adjunctive treatment for residual symptoms of depression, anxiety and stress in people with depression. J. Affect. Disord. 248, 42–51 (2019).
Buttner, M. M., Brock, R. L., O’Hara, M. W. & Stuart, S. Efficacy of yoga for depressed postpartum women: A randomized controlled trial. Complement. Ther. Clin. Pract. 21 (2), 94–100 (2015).
Chu, I. H. et al. Effects of yoga on heart rate variability and depressive symptoms in women: A randomized controlled trial. J. Altern. Complement. Med. 23 (4), 310–316 (2017).
Chu, I. H., Buckworth, J., Kirby, T. E. & Emery, C. F. Effect of exercise intensity on depressive symptoms in women. Ment. Health Phys. Act. 2(1), 37–43. https://doi.org/10.1016/j.mhpa.2009.01.001 (2009).
Daley, A. J. et al. A pragmatic randomized controlled trial to evaluate the effectiveness of a facilitated exercise intervention as a treatment for postnatal depression: the PAM-PeRS trial. Psychol. Med. 45 (11), 2413–2425 (2015).
Doose, M. et al. Self-selected intensity exercise in the treatment of major depression: A pragmatic RCT. Int. J. Psychiatry Clin. Pract. 19 (4), 266–275 (2015).
Field, T., Diego, M., Delgado, J. & Medina, L. Tai chi/yoga reduces prenatal depression, anxiety and sleep disturbances. Complement. Ther. Clin. Pract. 19 (1), 6–10 (2013).
Forsyth, J., Boath, E., Henshaw, C. & Brown, H. Exercise as an adjunct treatment for postpartum depression for women living in an inner city-A pilot study. Health Care Women Int. 38 (6), 635–639 (2017).
Helgadóttir, B., Hallgren, M., Ekblom, Ö. & Forsell, Y. Training fast or slow? Exercise for depression: A randomized controlled trial. Prev. Med. 91, 123–131 (2016).
Hoffman, B. M. et al. Effects of aerobic exercise on sexual functioning in depressed adults. Ment. Health. Phys. Act. 2 (1), 23–28 (2009).
Imboden, C. et al. Aerobic exercise or stretching as add-on to inpatient treatment of depression: similar antidepressant effects on depressive symptoms and larger effects on working memory for aerobic exercise alone. J. Affect. Disord. 276, 866–876 (2020).
Khoshnab, L. P. & Nikseresht, A. Comparison of the effect of aerobic exercise and antidepressant medications on depression and sexual desire of depressed middle-aged women. peptides 8 : 9. (2017).
Krogh, J., Videbech, P., Thomsen, C., Gluud, C. & Nordentoft, M. DEMO-II trial. Aerobic exercise versus stretching exercise in patients with major depression-a randomised clinical trial. PLoS One. 7 (10), e48316 (2012).
La Rocque, C. L., Mazurka, R., Stuckless, T. J. R., Pyke, K. & Harkness, K. L. Randomized controlled trial of Bikram yoga and aerobic exercise for depression in women: efficacy and stress-based mechanisms. J. Affect. Disord. 280 (Pt A), 457–466 (2021).
Liu, J. et al. The effects of Tai Chi on heart rate variability in older Chinese individuals with depression. Int. J. Environ. Res. Public. Health. 15 (12), 2771 (2018).
McNeil, J. K., LeBlanc, E. M. & Joyner, M. The effect of exercise on depressive symptoms in the moderately depressed elderly. Psychol. Aging. 6 (3), 487–488 (1991).
Prathikanti, S. et al. Treating major depression with yoga: A prospective, randomized, controlled pilot trial. PLoS One. 12 (3), e0173869 (2017).
Shahidi, M. et al. Laughter yoga versus group exercise program in elderly depressed women: a randomized controlled trial. Int. J. Geriatr. Psychiatry. 26 (3), 322–327 (2011).
Singh, N. A., Clements, K. M. & Fiatarone, M. A. A randomized controlled trial of progressive resistance training in depressed elders. J. Gerontol. Biol. Sci. Med. Sci. 52 (1), M27–35 (1997).
Singh, N. A. et al. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 60(6), 768–776. https://doi.org/10.1093/gerona/60.6.768 (2005).
Sun, P. et al. Yijinjing qigong intervention shows strong evidence on clinical effectiveness and electroencephalography signal features for early poststroke depression: A randomized, controlled trial. Front. Aging Neurosci. 14, 956316 (2022).
Yeung, A. et al. Tai Chi treatment for depression in Chinese americans: a pilot study. Am. J. Phys. Med. Rehabil. 91 (10), 863–870 (2012).
Zhang, J. et al. The effect of Bafa Wubu of Tai Chi on college students’ anxiety and depression: A randomized, controlled pilot study. Front. Physiol. 14, 1036010 (2023).
Zhao, Y. et al. Personalized individual-based exercise prescriptions are effective in treating depressive symptoms of college students during the COVID-19: A randomized controlled trial in China. Front. Psychiatry. 13, 1015725 (2023).
Majumder, P., Sharma, I., Vostanis, P. & Bone, C. The effect of aerobic exercise in the maintenance treatment of depression. BJPsych Int. 12 (RESEARCH), S3–S6 (2015).
Mota-Pereira, J. et al. Moderate exercise improves depression parameters in treatment-resistant patients with major depressive disorder. J. Psychiatr Res. 45 (8), 1005–1011 (2011).
Sharma, V. K., Das, S., Mondal, S., Goswampi, U. & Gandhi, A. Effect of Sahaj Yoga on depressive disorders. Indian J. Physiol Pharmacol. 49(4), 462–468 (2005).
Uebelacker, L. A., Battle, C. L., Sutton, K. A., Magee, S. R. & Miller, I. W. A pilot randomized controlled trial comparing prenatal yoga to perinatal health education for antenatal depression. Arch. Womens Ment Health. 19 (3), 543–547 (2016).
Ciccolo, J. T. et al. Resistance training for black men with depressive symptoms: a pilot randomized controlled trial to assess acceptability, feasibility, and preliminary efficacy. BMC Psychiatry. 22 (1), 283 (2022).
Daley, A. et al. Feasibility of an exercise intervention for women with postnatal depression: a pilot randomised controlled trial. Br. J. Gen. Pract. 58 (548), 178–183 (2008).
Dritsa, M., Dupuis, G., Lowensteyn, I. & Da Costa, D. Effects of home-based exercise on fatigue in postpartum depressed women: who is more likely to benefit and why? J. Psychosom. Res. 67 (2), 159–163 (2009).
Dunn, A. L., Trivedi, M. H., Kampert, J. B., Clark, C. G. & Chambliss, H. O. Exercise treatment for depression: efficacy and dose response. Am. J. Prev. Med. 28 (1), 1–8 (2005).
Field, T., Diego, M., Delgado, J. & Medina, L. Yoga and social support reduce prenatal depression, anxiety and cortisol. J. Bodyw. Mov. Ther. 17 (4), 397–403 (2013).
Gerber, M. et al. Effects of aerobic exercise on cortisol stress reactivity in response to the Trier social stress test in inpatients with major depressive disorders: A randomized controlled trial. J. Clin. Med. 9 (5), 1419 (2020).
Sims, J. et al. Regenerate: assessing the feasibility of a strength-training program to enhance the physical and mental health of chronic post stroke patients with depression. Int. J. Geriatr. Psychiatry. 24 (1), 76–83 (2009).
Sims, J., Hill, K., Davidson, S., Gunn, J. & Huang, N. Exploring the feasibility of a community-based strength training program for older people with depressive symptoms and its impact on depressive symptoms. BMC Geriatr. 6, 18 (2006).
Pilu, A. et al. Efficacy of physical activity in the adjunctive treatment of major depressive disorders: preliminary results. Clin. Pract. Epidemiol. Ment Health. 3, 8 (2007).
Doyne, E. J. et al. Running versus weight lifting in the treatment of depression. J. Consult Clin. Psychol. 55 (5), 748–754 (1987).
Veale, D. et al. Aerobic exercise in the adjunctive treatment of depression: a randomized controlled trial. J. R Soc. Med. 85 (9), 541–544 (1992).
Blumenthal, J. A. et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 69(7), 587–596. https://doi.org/10.1097/PSY.0b013e318148c19a (2007).
Danielsson, L., Papoulias, I., Petersson, E. L., Carlsson, J. & Waern, M. Exercise or basic body awareness therapy as add-on treatment for major depression: a controlled study. J. Affect. Disord. 168, 98–106 (2014).
Nabkasorn, C. et al. Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. Eur. J. Public. Health. 16 (2), 179–184 (2006).
Chen, J. X., Li, Y. H., Wu, Y. Q. & Su, X. Y. Effects of Pilates exercise on body composition and serum inflammatory factors of obese female college students with depression. Chin. J. Sch. Health. 41(05), 783–786. https://doi.org/10.16835/j.cnki.1000-9817.2020.05.040 (2020).
Zheng, T. S., Zhang, Y. B., Dong, Z. H., Qian, L. & Ye, M. J. Effect of exercise therapy on depressive symptoms and cognitive function of depressive patients in a hospital of Wenzhou City. Med. Society 32(03), 107–111. https://doi.org/10.13723/j.yxysh.2019.03.027 (2019).
Chen, J. X., Li, Y. H. Wu, Y. Q. & Su, X. Y. Effects of Taijiquan exercise on depression and serum inflammatory factors in female college students. Chin. J. School Health 40(07), 1065–1068. https://doi.org/10.16835/j.cnki.1000-9817.2019.07.029 (2019).
Zhao, B. et al. Effects of Taijiquan on motor function and depression in patients with Post-stroke depression [J]. Chin. J. Rehabilitation Theory Practice 23(03), 334–337. https://doi.org/10.3969/j.issn.1006-9771.2017.03.019 (2017).
Cheng, X. et al. Health qigong Wuqinxi improves hydrogen proton magnetic resonance spectra in prefrontal cortex and hippocampus in college students with mild depression. J. South. Med. University 36(11), 1468–1476. https://doi.org/10.3969/j.issn.1673-4254.2016.11.04 (2016).
Ma, M. Y. To explore the influence of yoga on the psychological state of postpartum depression patients. Maternal Child. Health Care China 29(17), 2714–2716. https://doi.org/10.7620/zgfybj.j.issn.1001-4411.2014.17.24 (2014).
Liu, Y., Huo R., Lai Y., Yao Q. L., Chen C. Y. & Chen Y. Community-based study on effects of Chinese Qigong-Baduanjin on depression symptoms and life quality of patients with type 2 diabetes mellitus. Chin. J. Sports Medicine 31(03), 212–217. https://doi.org/10.3969/j.issn.1000-6710.2012.03.005 (2012).
Ma, S. H., Dou, N., Chen, C. X. & Zhao, Y. N. Rehabilitation effects of walking and Baduanjin to the perimenopausal syndrome with depression. Chin. J. Rehabilitation Medicine 26(08), 738–741. https://doi.org/10.3969/j.issn.1001-1242.2011.08.010 (2011).
Ma, S. H., Dou, N., Chen, C. X., Zhao, Y. N. & Li, S. X. Effect of traditional Baduanjin exercise in women with perimenopausal syndrome and depression. Chin. Gen. Practice 13(25), 2864–2865. https://doi.org/10.3969/j.issn.1007-9572.2010.25.030 (2010).
Lin, Y. H., Wang, J. Q. & Zhang, H. N. Sdudy for effect on on negative emotion and self-efficacy for patients with depression by YOGA relaxation training. J. Nurses Training 25(23), 2125–2127. https://doi.org/10.3969/j.issn.1002-6975.2010.23.005 (2010).
Wang, Q. L. et al. Influencing of exercise and nursing intervention on self-esteem and self-efficacy of depressedpatients. Chin. Nurs. Res. 34(01), 165–167. https://doi.org/10.12102/j.issn.1009-6493.2020.01.033 (2020).
Tabei, M., Ravari, A., Kataria, M., Mirzaei, T. & Kamiab, Z. The effect of laughter yoga and music intervention on depression, anxiety, and stress in the Rafsanjan-Iran aged: a randomized clinical trial study. Aging Ment Health. 29 (2), 274–281 (2025).
Amina, B. et al. Comparison of aerobic and pilates exercises on depression and sleep quality in primigravida females. Pak. J. Med. Health Sci. 17(11), 27–30. https://doi.org/10.53350/pjmhs02023171127(2023).
Hallgren, M. et al. Treatment guidelines for depression: greater emphasis on physical activity is needed. Eur. Psychiatry. 40, 1–3 (2017).
Chen, M., Zhang, X. B., Luo, Y. Z., Hu, Z. Q. & Sun, J. Q. Research progress of the Neurobiological mechanisms for exercise improving depression. China Sport Sci. Technol. 57(4), 89–97. https://doi.org/10.16470/j.csst.2020137 (2021).
Xia, J., Liu, W. N.,Qi, Z. T. & Ji, L. PGC-1α-mediated muscle /brain crosstalk and antidepressant effects of Exercise-Reflaction and prospect from integrative biolog. J. Shanghai Univ. Sport 41(4):8. https://doi.org/10.16099/j.sus.2017.04.010 (2017).
Gu, J. Y. & Cheng, J. P. Adjuvant treatment effect of health preserving of TCM on depression. J. Basic. Chin. Medicine 19(09), 1057–1059. https://doi.org/10.19945/j.cnki.issn.1006-32 (2013).
Yang, Z. M. The role and position of qigong in traditional health maintenance of Chinese medicine. J. Mod. Med. Health 20(14), 2. https://doi.org/10.3969/j.issn.1009-5519.2004.14.083 (2004).
Zhang, S. Q. Wang, J. L. & Wang, T. Network Meta-analysis of the effects of different Chinese traditional fitness exercises on blood lipid. J. Capital Univ. Phys. Educ. Sports 34(05), 545–554. https://doi.org/10.14036/j.cnki.cn11-4513.2022.05.010 (2022).
Zou, L. et al. Effects of mind⁻body movements on balance function in stroke survivors: A Meta-Analysis of randomized controlled trials. Int. J. Environ. Res. Public. Health. 15 (6), 1292 (2018).
Lou, H. & Liu, P. A. Meta-Meta-Analysis of the effect of physical exercise as a treatment on depression. J. Tianjin Univ. Spor 33(06), 500–507. https://doi.org/10.13297/j.cnki.issn1005-0000.2018.06.007 (2018)
Zha, Q. Q., Xu, L. Y., Chen, J., Huang, W. & Zhang, X. Q. Summary of best evidence for prevention of recurrence of Late-life depression. Chin. Gen. Pract. 26(19), 2332–2338. https://doi.org/10.12114/j.issn.1007-9572.2022.0727(2023).
Miller, K. J. et al. Comparative effectiveness of three exercise types to treat clinical depression in older adults: A systematic review and network meta-analysis of randomised controlled trials. Ageing Res. Rev. 58, 100999 (2020).
Tan, Z. G. Tan qw.study on the psychosomatic effects of health qigong Baduanjin on college students with depression[J]. Contemp. Sports Technol. 10 (04), 182–183 (2020).
Vankova, H. et al. The effect of dance on depressive symptoms in nursing home residents. J. Am. Med. Dir. Assoc. 15 (8), 582–587 (2014).
Liu, S., Liu, M. Y. & Jing, Y. Intervention effects of multiple exercise methods on depression and anxiety in children and adolescents: a network meta-analysis. Chin. J. Evidence-Based Med. 24(08), 910–920. https://doi.org/10.7507/1672-2531.202307091 (2024)
Acknowledgements
This work was support by Funding was provided by the“2020 provincial first-class undergraduate construction site”(2020ylzy03) and by Dr. Gang Liu at Anhui Xinhua University.
Funding
Funding was provided by the“2020 provincial first-class undergraduate construction site”(2020ylzy03).
Author information
Authors and Affiliations
Contributions
Siqi Zhang is responsible for the overall conception, framework design, data analysis and writing of the article; Siqi Zhang and Gang Liu were responsible for literature retrieval, screening, data extraction and quality evaluation; Jielin Yang is responsible for chart production and English revision; Jiawei Chen is responsible for the overall quality control and review of the paper; Junli Wang is responsible for research planning and guidance.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, S., Yang, J., Chen, J. et al. Effect and acceptability of different exercise modes on adult patients with clinically diagnosed depression: a network meta-analysis. Sci Rep 15, 33478 (2025). https://doi.org/10.1038/s41598-025-14648-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-14648-y