Abstract
This study aimed to comparatively evaluate the hematological profile and sports performance in CrossFit® practitioners training using Elevation Training Mask (ETM) 2.0 after recovering from COVID-19 (1 month with no symptoms). Twenty trained male athletes were assigned to an experimental group (EG) (n = 10) using configured ETM and a control group (CG) (n = 10) using sham ETM device. Both groups completed 12 weeks of CrossFit® training after 1 month of finishing SARS-CoV-2 symptoms. Pre- and post-training testing included assessment of hematological biomarkers, and sports performance parameters in a single-blind randomized clinical trial (ID NCT06806124) following the Consolidated Standards of Reporting Trials. No significant differences (p > 0.05) were observed comparing EG and CG in the hematological profile and sports performance parameters evaluated. Significant differences (p < 0.05), group by time interaction effect, were observed throughout the 36 training sessions for CrossFit® Total and Fran WOD. Our findings could indicate improvements in both groups, CG and EG, in performance tests, without reaching pre-SARS-CoV-2 infection levels. Furthermore, ETM does not appear to function as an altitude simulator under the experimental conditions developed in the present intervention.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) can be asymptomatic or cause a wide variety of clinical symptoms. Approximately 80% of patients have mild or moderate symptoms, but the 20% remaining develop severe symptoms related to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1. These include alterations in hematological parameters and morphological abnormalities in blood cells2. SARS-CoV-2 infection modifies the structure and rigidity of the erythrocyte membrane as a result of the immune response itself3. These alterations appear during the acute phase and remain months later, causing significant hemolysis4. SARS-CoV-2 attacks hemoglobin (Hb), through CD147 or CD26 blood receptors, released after hemolysis, reducing significantly its levels5. Therefore, moderate to severe cases of anemia have been described2. Altogether, secondary anemia, hemolytic alterations in erythrocytes and Hb destruction result in a lower capacity to supply oxygen to the body tissue, aggravating the disease2,4. It is known that an optimal hematological profile in athletes is key to improving sports performance and optimizing health6. One way to achieve optimal hematological parameters is through training under hypoxic conditions (real or simulated)7. In addition, hypoxia improves the rate of oxygen utilization resulting in better sports performance, and decreases heart rate with particular workloads8. All this evidence may suggest that training under hypoxic conditions could be a strategic option to reverse hematological alterations associated to COVID-199. Therefore, exercise in hypoxia would have a therapeutic use because exercise would multiply the physiological stress of the organism induced by hypoxia and would substantially increase the benefits of exercise in normoxia10.
Over the past twenty years, athletes have used a variety of elevation training masks (ETM), purportedly designed to simulate altitude. These devices seem to enable improvements in aerobic fitness and athletic performance11. ETM recreates simulated altitude conditions, from 914 to 5,486 m (m)12, by inducing a decrease in oxygen saturation (SpO2) during exercise13,14. This is achieved through insufficient hyperventilation and re-breathing of carbon dioxide (CO2), generating a hypoxic microenvironment by modifying the concentration of breathing gases15.
In this context, mild and moderate symptoms related to COVID-19 have been described in athletes16, although prolonged symptoms are related to the onset of “Post-COVID-19 Syndrome”17. Post-COVID encompasses the effects derived from clinical states due to post-SARS-CoV-2 infection sequelae and/or the variety of symptoms that may remain after an acute SARS-CoV-2 infection (“Long COVID”)18. These conditions would affect the return to training or competition19,20, influencing performance negatively16. In this sense, the implementation of therapeutic exercise programs, which include strength routines, aerobic, and anaerobic exercise21, in patients with post-COVID-19 syndrome stimulates functional recovery, improves quality of life22 and provides immune protection19,23. CrossFit® is a multimodal, interval training system that involves standardized routines to optimize physical fitness through strength training of skeletal muscles, increasing their flexibility, power, endurance, speed of execution, coordination, agility and precision24 and could be useful as an exercise program to restore weakened functions in the post-COVID period.
Therefore, the recovery of the hematological profile and physical condition are important in athletes to prevent short- and long-term post-COVID symptoms and complications and accelerate the return to athletic practice. Subsequently, ETM could serve as a therapeutic tool to reverse post- SARS-CoV-2 infection hematological alterations in athletes. However, no studies have been conducted to evaluate the effectiveness of ETM in athletes who have overcome COVID-19 when they return to perform exercise. To our knowledge, there is only one study25 that used a moderate-intensity exercise protocol in a cyclic hypoxic environment for the rehabilitation of recovered COVID-19 individuals with persistently low cardiorespiratory fitness, 30 days since the recovery of clinical signs or medical discharge. Given the above, the hypothesis of the present study was to evaluate the use of ETM in athletes resuming CrossFit® training at least one month after the cessation of COVID-19 symptoms in improvements in hematological biomarkers and sports performance compared to a sham ETM participants.
Methods
Study design and participants
A single-blind randomized clinical trial was conducted with twenty volunteer male CrossFit® athletes from 2 sports centers in Salamanca and Soria (Spain), after COVID-19 without hospitalization. The “Consolidated Standards of Reporting Trials” (CONSORT) were followed for conducting randomized trials of parallel groups (Appendix I)26. The study evaluated the effect of the ETM 2.0 (Training Mask LLC, Cadillac, Michigan) during 12 weeks of training on hematological parameters: red blood cells (RBC), Hb, and hematocrit (Hct); hematopoietic biomarkers reticulocytes (RET) and erythropoietin (EPO). Sports performance was evaluated by Work of the Day (WOD), which included “Fran WOD” and “CrossFit® Total.”
The sample size considered necessary to carry out this study was 20 athletes, calculated using the statistical power analysis software G* Power 3.1.97 (University of Dusseldorf, Dusseldorf, Germany; available at https://es.freedownloadmanager.org/Windows-PC/Gpower-GRATIS.html ) (accessed on December 23, 2021)27. On the other hand, the sample size of recently published publications related to the topic of the study has been assessed11,28. Following the recommendations of Sedar et al.29, considering type one error (a) of 0.05 and type two error (b) of 0.20 (power = 80%) we used 1.3 as standard deviation (SD) and 1.1 as the difference in mean (d) of Hb as key variable. In addition, a percentage of refusal to participate in the study of 20% has been estimated. All study subjects were consecutively selected between January 2022 and December 2023, meeting the inclusion and exclusion criteria (Table 1). Participants were also asked to avoid any intense physical activity outside the training protocol, follow dietary guidelines and no consumption of illegal drugs according to the World Anti-Doping Agency (WADA)30. In addition, all participants were instructed not to take any drugs or nutritional supplements (doping-free) that might alter hematological response or sports performance, such as iron, vitamin B12, vitamin B9, vitamin C, among others31.
Participants (n = 20) were divided into two groups using a stratified block random sampling method using the “Random” application. Sequence Generator” https//www.random.org/sequences/ (accessed January 7, 2022): study group (EG, n = 10) and control group (CG, n = 10) (Fig. 1). This randomization was carried out by a person outside the research team once the patient signed the informed consent.
Each subject visited the laboratory 3 days before the start of this study and was carefully familiarized with the procedures to be performed (Fig. 1), to avoid learning delays.
The study was conducted over 12 weeks. The first day and the final day included the same test, performed at the same time (starting at 9:00 am) to reduce circadian influence. To standardize the procedure, all tests were performed using the same protocol and in the same order.
Data collection
Two study investigators collected specific data before the intervention, including sociodemographic information, anthropometric parameters, CrossFit® sports history32, perception of severity of SARS-CoV-2 infection33 and clinical history of COVID- 19.
Training
All study participants performed the same training program that began at least 1 month after the cessation of symptoms of SARS-CoV-2 infection, to avoid possible residual effects of COVID-19 accoding Hueghes et al.34 and recommendations of the Spanish Society Of Sports Medicine For athletes who have suffered from SARS-CoV-2 infection35. To guarantee adherence to the training protocol, the training sessions were supervised by 2 licensed CrossFit® trainers from the corresponding gyms. The training routine lasted 12 weeks, with 3 weekly sessions on alternate days (Monday, Wednesday and Friday). Each session lasted one hour and was divided into 3 parts: general warm-up; main part based on WODs32; return to calm (Table 2). Exercise intensity was assessed using the Borg CR-10 perceived exertion scale36.
Dietary indications
A qualified and registered nutritionist prescribed a diet adjusted to the training load for the participants. The amount of macronutrients on training days was adjusted to the amounts described for interval sports disciplines: 4–6 g (g) of carbohydrates/kilograms (kg) of body weight, 1–1.5 g of lipids/kg of body weight and 1.4–1.8 g of protein/kg of body weight37. In addition, the diet contained the recommended dietary amounts for minerals and vitamins38. Diet was monitored weekly through regular meetings with the nutritionist, to solve doubts and control possible deviations.
Using the elevation training mask 2.0
The ETM recreates an altitude of 914 to 5,486 m in situ12. ETM 2.0 was used in all 36 training sessions over the 12 weeks of the study with progressive increases in air restriction to simulate altitude training. This methodology of using ETM during exercise was chosen following the study by Porcari et al.28. The first week, the additional altitude simulation was 914 m and in the second, 1,829 m. These initial 2 weeks served to adjust the use of the ETM during training, as a process of acclimatization to the altitude simulation and airflow restriction. For the period between weeks 3 and 6 (both inclusive) the simulated altitude was 2,743 m, and for weeks 7–12 (both inclusive), the ETM was set to simulate 3658 m altitude (Table 3).
The manufacturer’s instructions were followed in configuring the ETM using the corresponding air restriction openings and filters (Appendix II) to apply air limitation and thus recreate the desired altitude.
For the CG, the ETM used for 12 weeks was visually identical with the largest openings and no air restriction filters that prevent the generation of a hypoxic environment. This resulted in a little respiratory obstruction, but the reduction in air flow was minimal, with the aim of having a simulated ETM treatment.
Oxygen saturation (SpO2) was determined using a finger pulse oximeter (OMRON Spain, Madrid, Spain) before, during and after each training session. If the saturation was less than 85% the athlete had to stop training.
Extraction and analysis of hematological biomarkers
During the collection and transport of blood samples, the World Anti-Doping Agency (WADA) regulations39. Blood samples were drawn from the antecubital venous blood of CrossFit® athletes at the beginning of the study (T1) without previous use of ETM and after 12 weeks of training with ETM or fake ETM (T2). All samples were collected, transported, and received following protocols of our previous studies7. Hematological biomarkers RBC, Hb, Hct, and hematopoietic biomarkers EPO and RET were analyzed using the methodology of Fernández-Lázaro et al.7.
Percentage changes in plasma volume (% ΔPV) were calculated using the Van Beaumont equation40. In addition, values of analytical markers were adjusted for changes in plasma volume using the following formula: Corrected value = Uncorrected value x ((100 + % ΔPV) / 100)41.
Sports performance evaluation
The sports performance of the participants was evaluated by means of two WODs: Fran WOD, and CrossFit® Total (squat (back squat), shoulder press (press) and deadlift (deadlift)), according to the international standards of CrossFit®32.
Statistical analysis
The analyses were performed using STATA® version 15.0 (StataCorp, College Station, TX, USA), SPSS version 24.0 (SPSS, Inc., Chicago, IL, USA), and Microsoft Excel (Microsoft Excel version 19). Data are presented as means and standard deviations. Values with p < 0.05 are considered statistically significant. The Shapiro-Wilk test was used to determine normality. Parametric tests were used because the data followed a normal distribution.
Barlett’s and Levene ‘s tests were used to measure equality of variance. Comparisons between groups were made using a one-way analysis of variance (ANOVA).
The two-variate repeated measures ANOVA test was used to examine the effects of interactions (time x group) between study groups (Control and Experimental) for hematological biomarkers (RBC, Hb, Hct), hematopoietic parameters (RET and EPO), and WODs (Fran WOD and CrossFit® Total).
Likewise, the differences between T1 (start) and T2 (end of the study) were analyzed in each group using Student ‘s t tests for paired samples (parametric data).
The effect size within participants was calculated using partial eta-squared (η2p)42. Because this measure is likely to overestimate effect sizes, values were interpreted as indicating no effect if η2p < 0.05; minimal effect if 0.05 < η2p < 0.26; moderate effect if 0.26 < η2p < 0.64; and strong effect if η2p ≥ 0.64.
Blinding
To calculate the level of blinding, a questionnaire was distributed at T1 and T2, which generated results with values between 0 (all participants knew which research group they belonged to) and 1 (no participant knew which research group they belonged to). To consider the level of blinding adequate, values > 0.5 should be obtained43.
Ethical considerations
The study protocol received approval from the local institutional review board, named the Ethics Committee for Drug Research in the Valladolid area (PI 19-1361). This research was performed in accordance with the Declaration of Helsinki and the 2013 Fortaleza review44. Also, all participants signed informed consent before their involvement. The protocol, ETMEXCOVID, of this intervention study was registered on ClinicalTrials.gov (03/02/25025, ID NCT06806124).
Results
Selection and characteristics of participants
Initially, 35 CrossFit® athletes who had suffered SARS-CoV-2 infection, were recruited. Eight were excluded from the study for not meeting the inclusion criteria, 4 athletes refused to participate in the study, and 3 subjects were excluded for other reasons. Finally, 20 athletes were included in the study, which were randomly divided into 2 groups EG (n = 10) and CG (n = 10), using a stratified block design. None of the participants dropped out of the study or had to discontinue the intervention, nor suffered side effects derived from the use of ETM, or injury derived from the CrossFit® sports activity (Fig. 2).
Flow chart of the enrolment and randomization process, according to the CONSORT26 regulations.
The characteristics of the participants are indicated in Table 4. All participants were male athletes with more than 30 months of experience in CrossFit® training. They performed Fran WOD in less than 240 s (s) prior to SARS-CoV-2 infection and lived in Soria or Salamanca, with a very similar altitude. On the other hand, the anthropometric parameters indicated that participants displayed an optimal fat mass and a normal weight.
Symptoms of SARS-CoV-2 infection are shown in Table 4. Participants presented cough (45%), dyspnea (35%), ageusia or anosmia (75%), fever (40%), myalgia (45%), and the perception of severity of COVID-19 was 1.8 ± 0.2 on a 0–3 Likert-type scale (30).
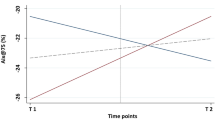
Hematological biomarkers
Hematological (RBC, Hb, Hct) and hematopoietic (RET and EPO) parameters did not show significant differences (p > 0.05) in their behavior between the when comparing EG vs. CG over 12 weeks of training with the ETM. No significant differences (p > 0.05) were observed between EG and CG or between T1 and T2 in any hematological biomarker (Table 5).
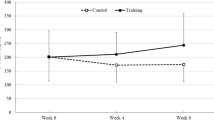
Sports performance
In Fran WOD and CrossFit® Total (29) significant differences (p < 0.05) were observed in performance between the EG and CG over 36 training sessions, showing a moderate effect of 0.346 and 0.379 η2p respectively. In addition, both groups, EG and CG, showed a statistically significant improvement (p < 0.05) between T1 and T2, although no significant differences (p > 0.05) were observed in Fran WOD and CrossFit® Total between the EG and CG (Table 6).
Blinding index
The blinding index at T2 was 0.91. Three of the participants claimed to know the group they belonged to, although only two of them were correct. This suggests that the blinding process was adequate43.
Discussion
To our knowledge, this is the first study carried out in a population with a previous illness, at least 1 month after the cessation of COVID-19 symptoms, to evaluate the potential of ETM during exercise on the hematological profile and physical condition. In this line, all prior studies have analyzed the use of ETM in healthy, physically active or athletic adults or adolescents. Therefore, the present study is a novel contribution and with a clear scientific interest in the fields of sports, exercise and health.
The use of ETM during CrossFit® training had no benefits on hematological parameters when comparing CG and EG and according to or in the same line that preliminary studies12,28,45. The published improvements seem to be conditioned by the intensity and duration of the hypoxic stimulus. In our intervention, possibly duration could be insufficient to trigger beneficial hematological or hematopoietic responses, that need to be explored in future interventions. The hypoxic microenvironment generated by ETM induces mild arterial hypoxemia during exercise by reducing respiratory rate due to airflow restriction through resistance plugs and flow valves46. Hypoxemia could be accentuated by re-inspiration of CO2, due to the small dead space of ETM (approximately ∼350 mL), and the subsequent shift of in the oxygen dissociation curve15. Although this mechanism of modifying the concentration of respirable gases by the configuration of the ETM would be similar to stages in altitude7, microhypoxic environment of the ETM only achieves modest decreases in SpO2 (13–15), around ∼96–92% in the EG athletes of this study, corresponding to simulated altitudes of 2743 and 3658 m. This modest change seems to be insufficient to generate a stimulus with the threshold intensity necessary to modify the hematological profile9. Indeed, Barbiere et al.46 and Boyle et al.47 found no differences in SpO2 (∼ 96%), according to our results. In the same line, Porcari et al.28 described decreases in SpO2 of ≤ 2%28 between the EG and CG during exercise. High altitude or very high altitude (real or simulated with hypoxicants) reaches SpO2 levels < 90%48, which are much higher than those observed when using ETM. In this context, high altitude induces body responses and physiological adaptations7. Hematological adaptations are part of these changes6, resulting in optimal performance compared to training in normoxia7. In this sense, the increase in the EPO level is greater when there is a greater decrease in SpO245, specifically the effective erythropoietin stimulation requires an SpO2 < 90%49. Therefore, our oxygen saturation measurements (SpO₂ ∼92–96%) would be too high to induce significant hematological changes.
Furthermore, the duration of the hypoxic exposure stimulus was ∼180 min per week. This suggests that this time would not be long enough, according to the results obtained, to cause changes in the hematological profile of the participants. The total time of interval training in hypoxia with ETM of 60 min per week28 or 70 min per week45, and 114 min per week with hypoxicants50, did not produce benefits on hematological parameters compared to sham treatment in normoxia. At natural altitude, it is accepted that “the longer the better” with regard to hematological adaptations, since additional benefits have been demonstrated as hypoxic exposure increases beyond 16 h/day. Under these conditions, the minimum daily exposure to stimulate erythropoiesis is 12 h/day8, for periods of at least 20 days51. In fact, it has been described that a natural altitude of 2500 m for 20–22 h/day for at least 20 days, would be sufficient to increase erythropoiesis and improve performance at sea level8. Moreover, intermittent hypoxia exposure of 60–90 min/day for 30–60 days has shown significant benefits on hematological and hematopoietic parameters6,7. EPO levels have also been shown to increase after several minutes (around 12) or several hours of acute hypoxia exposure51.
On the order hand, since hematological biomarkers showed a normal range at T1, this would limit the usefulness of ETM. Indeed, we did not observe significant differences in hematological parameters when comparing EG versus CG after 12 weeks. Ethics Committee considered unable to conduct the intervention while symptoms were fully present and following the recommendations of Hughes et al.34 and the Spanish Society of Sports Medicine35, resuming exercise after COVID-19 infection should be at least 1 month after symptom resolution. Moreover, CrossFit® or High Intensity Interval Training (HIIT) may be more limited in inducing hematological adaptations compared to continuous aerobic exercise52,53. Hematological adaptations (particularly EPO increases and erythropoiesis) are generally known to occur better with prolonged continuous hypoxic exposure6,7 and aerobic exercise52. The HITT nature of CrossFit® may not have provided sufficient stimulus to induce such adaptations, even induced hematological improvements, and even produces significant decreases (< 2%) in Hb, HCT and red blood cells53. Perhaps these findings could be applied in practice by coaches considering the use of this device using a low-to-moderate intensity exercise protocol in a hypoxic environment for the rehabilitation of individuals who have recovered from COVID-19, thereby improving their cardiorespiratory fitness and hematological biomarkers25.
The use of ETM has been accepted in the sports environment as a proposed device to improve sports performance complementary to hypoxic methods. We evaluated performance using CrossFit® Total and Fran WOD, which serve as a reference to assess physical capacity and progress54. These are the most demanding WODs in terms of strength and exercise intensity respectively55. In both study conditions (EG and CG), significant differences (p < 0.05) were observed between T1 and T2, increasing the international reference level from “intermediate” to “advanced” for CrossFit® Total, but without reaching pre-SARS-CoV-2 infection performance levels. However, no significant differences (p > 0.05) were observed when comparing the EG with the identical structured training program, without ETM configured for the two WODs. This would indicate that the performance results are an effect of CrossFit® training. Our results are similar to those reported in other studies that do not show significant improvements (p > 0.05) between EG and CG for VO2max28,45,51, anaerobic power28, and WODs (Grace and CrossFit® Total)11. Nevertheless, the studies using ETM in CrossFit® or HIIT are scarce45. Therefore, there is limited available evidence on ETM use during high-intensity exercise. In addition, the sports modalities of the main part of studies are different from CrossFit®. On the other hand, and as future working hypothesis, we could consider that our athletes probably had weakened respiratory muscles, because of COVID-19 and the consequent inactivity. In this post-infection condition of SARS-CoV-2, the exercise program during CrossFit® training has to add the extra respiratory load on the respiratory muscles of the ETM exerted simultaneously during CrossFit® training, which would significantly increase transdiaphragmatic pressure47 and possible early fatigue of the respiratory muscles56 or early stimulation of the metaboreflex57. In addition dyspnea would increase due to the full configuration of the ETM12. These factors would condition the performance of the WODs and could even have decreased it in the EG compared to the CG. In fact, some authors47,58,59 have published in healthy physically active subjects that the use of ETM reduces performance during a cycling test to exhaustion with constant59 or incremental load47, as well as the maximum speed of execution in back squad and bench press58, versus those participants who did not use ETM. Our training program was not interrupted by any athletes in the current study who used full- or sham-configured ETM (both were well tolerated), and nor did any athlete deviate from the proposed training program. Therefore, ETM would thwarts the ability to achieve desired workload or to increase training volume in the athletes.
The present study, as it is an exploratory or pilot trial, is limited by the following facts: low number of subjects (n = 20), who were only CrossFit® practitioners and were exclusively males. Therefore, they might not be representative of the general athlete population. In this line, the demanding inclusion criteria contributed to this small sample size, which limited participant recruitment, although justified via power analysis for Hb outcomes and software G* Power 3.1.97 Finally, the age range of participants may be considered a limitation, given that COVID-19 is known to affect different age groups differently. Therefore, the present findings should be considered preliminary and interpreted with caution, serving as starting points for future studies with a larger number of participants. Despite these limitations, this study also has several notable strengths. First, food intake was controlled using dietary guidelines from a sports nutrition expert. Therefore, participants did not receive ergogenic supplements, which would not distort hematological parameters. Furthermore, 20% of the total hematological analyses were evaluated duplicate as quality control and all results were consistent. Therefore, this could suggest that the analyses and results could be considered consistent. In this study, the ETM was set from 914 m to 3658 m. Nevertheless, an ETM configured to reach 4572 m and 5486 m, could give different results. These simulated altitudes (4572 m and 5486 m) were not used because of the potential of ETM to increase cerebral blood flow which may be related to an increase in intracranial pressure, which in turn is an important risk condition for cerebral dysregulation14. For the control condition, we used a simulated ETM (with earplugs but no filters) so that the athlete would have the same sensation during training as the EG. However, our simulated ETM is not a true simulated control, as it may provide very mild respiratory training effects but does not generate a hypoxic environment. Adequate control should include the absence of a mask or a completely non-restrictive device. The study has followed the CONSORT rules for conducting parallel group randomized trials26 and this intervention study was registered on ClinicalTrials.gov (03/02/25025, ID NCT06806124).
In conclusion, although ETM is supposed to simulate altitude training, there were no changes in hematological or hematopoietic variables before and after the 36 training sessions. ETM would not work as an altitude simulator. Therefore, real or simulated altitude training with hypoxic devices is considered to remain the optimal mode for altitude training so far. CrossFit® performance increased significantly in both, although they failed to reach pre-SARS-CoV-2 infection levels, suggesting that the modifications are likely due to the nature of the high-intensity exercise program implemented. Thus, CrossFit® training with ETM or without is effective for functional recovery in post-COVID athletes. Therefore, it is currently premature to recommend the use of ETM for post-COVID fitness recovery on a widespread basis. The use of ETM could be recommended considering the type of exercise, its intensity, and the individual physical or health status of the athlete. Future studies should consider longer intervention periods, the inclusion of additional control parameters or biomarkers, expanding the sample to include female athletes, addressing potential discomfort caused using the mask establish more precise protocols for the use of the ETM.
Data availability
The original contributions presented in the study are included in the article; Further inquiries can be directed to the corresponding author.
References
Fernández-Lázaro, D. et al. Convalescent plasma therapy, therapeutic formulations of repurposed drugs in 20th century epidemics against COVID-19: A systematic review. Pharmaceutics 14, 1020 (2022).
Aro, P. et al. Alteraciones En Los parámetros hematológicos y anormalidades morfológicas En células Sanguíneas En Pacientes hospitalizados Con COVID-19. Rev. Hematol. 27, 20–28 (2023).
Cacelín Garza, J. R. et al. Anemia hemolítica autoinmune desencadenada Por SARS-CoV-2 reporte de Un Caso. Rev. La. Fac. Med. 65, 26–36 (2022).
Kubánková, M. et al. Physical phenotype of blood cells is altered in COVID-19. Biophys. J. 120, 2838–2847 (2021).
Cavezzi, A. et al. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin. Pract. 10, 1271 (2020).
Fernández-Lázaro, D., Mielgo-Ayuso, J., Caballero-García, A., Pascual-Fernández, J. & Martínez, C. Artificial altitude training strategies: is there a correlation between the haematological and physical performance parameters? Arch. Med. Deport. 37, 35–42 (2020).
Fernández-Lázaro, D. et al. Adequacy of an altitude fitness program (Living and Training) plus intermittent exposure to hypoxia for improving hematological biomarkers and sports performance of elite athletes: A Single-Blind randomized clinical trial. Int. J. Environ. Res. Public. Health. 19, 9095 (2022).
Millet, G. P., Roels, B., Schmitt, L., Woorons, X. & Richalet, J. P. Combining hypoxic methods for peak performance. Sports Med. 40, 1–25 (2010). (2010).
Córdova Martínez, A., Pascual Fernández, J., Fernandez Lázaro, D. & Mon, A. Muscular and heart adaptations of execise in hypoxia. Is training in slow hypoxy healthy? Med. Clin. (Barc). 148, 469–474 (2017).
Millet, G. P., Debevec, T., Brocherie, F. & Malatesta, D. Girard, O. Therapeutic use of exercising in hypoxia: promises and limitations. Front. Physiol. 7, 224 (2016).
Fernández Lázaro, D. et al. Sport, muscle, and hormonal evaluation in CrossFit® athletes using the elevation training mask. Arch. Med. Deport. 38, 274–281 (2021).
Fernández Lázaro, D. et al. Analysis of the potential of elevation training mask on biomarkers, respiratory parameters, and sports performance indicators: what ergogenic mechanisms are involved? Systematic review. Arch. Med. Deport. 39, 10–18 (2022).
Jung, H. C., Lee, N. H., John, S. D. & Lee, S. The elevation training mask induces modest hypoxaemia but does not affect heart rate variability during cycling in healthy adults. Biol. Sport. 36, 105–112 (2019).
Romero-Arenas, S., López-Pérez, E., Colomer-Poveda, D. & Márquez, G. Oxygenation responses while wearing the elevation training mask during an incremental cycling test. J. Strength. Cond Res. 35, 1897–1904 (2021).
Granados, J., Gillum, T. L., Castillo, W., Christmas, K. M. & Kuennen, M. R. Functional respiratory muscle training during endurance exercise causes modest hypoxemia but overall is well tolerated. J. Strength. Cond Res. 30, 755–762 (2016).
Williams, Z. & Hull, J. H. Respiratory complications following COVID-19 in athletic populations: A narrative review. Scand. J. Med. Sci. Sports. 34, e14275 (2024).
Juhász, V. et al. Retrospective study of COVID-19 experiences in elite multinational aquatic athletes. Sci. Rep. 13, 13978 (2023).
Fernández-Lázaro, D. et al. Long COVID a new derivative in the chaos of SARS-CoV-2 infection: the emergent pandemic?? J. Clin. Med. 10, 5799 (2021).
Fernández-Lázaro, D., Santamaría, G., Sánchez-Serrano, N., Lantarón Caeiro, E. & Seco-Calvo, J. Efficacy of therapeutic exercise in reversing decreased strength, impaired respiratory function, decreased physical fitness, and decreased quality of life caused by the Post-COVID-19 syndrome. Viruses 14, 2797 (2022).
Hull, J. H., Ansley, L., Robson-Ansley, P. & Parsons, J. P. Managing respiratory problems in athletes. Clin. Med. 12, 351–356 (2012).
Fernández-de-las-Peñas, C. Special issue latest research in Post-COVID (Long COVID): pathological and treatment studies of sequelae and complications. Biomedicines 12, 1188 (2024).
del Corral, T. et al. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: randomized controlled trial. Ann. Phys. Rehabil Med. 66, 101709 (2023).
Fernández-Lázaro, D. et al. Physical exercise as a multimodal tool for COVID-19: could it be used as a preventive strategy?? Int. J. Environ. Res. Public. Health. 17, 1–13 (2020).
Claudino, J. G. et al. CrossFit overview: systematic review and Meta-analysis. Sport Med. – open. 4, 11 (2018).
de Dellavechia, C. et al. Effects of Moderate-Intensity training under Cyclic hypoxia on cardiorespiratory fitness and hematological parameters in people recovered from COVID-19: the AEROBICOVID study. Sports Health. 15, 558–570 (2022).
Moher, D. et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 10, 28–55 (2012).
Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 39, 175–191 (2007).
Porcari, J. P. et al. Effect of wearing the elevation training mask on aerobic capacity, lung function, and hematological variables. J. Sport Sci. Med. 15, 379–386 (2016).
Serdar, C. C., Cihan, M., Yücel, D. & Serdar, M. A. Sample size, power and effect size revisited: simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem. Med. 31, 010502 (2020).
World Anti-Doping Agency (WADA). International Standards World Anti Doping Agency. Available online: (2025). https://www.wada-ama.org/en/what-we-do/international-standards (accessed on 25 January 2025).
Fernández-Lázaro, D., Mielgo-Ayuso, J., Córdova Martínez, A. & Seco-Calvo, J. Iron and physical activity: bioavailability enhancers, properties of black pepper (Bioperine®) and potential applications. Nutrients 12, 1886 (2020).
Glassman, G. & Glassman, G. Benchmark workouts. CrossFit J. 13, 1–5 (2003).
Fossum, G. H. et al. Symptoms, symptom severity, and contact with primary health care among nonhospitalized COVID-19 patients: a Norwegian web-based survey. Scand. J. Prim. Health Care. 41, 427–434 (2023).
Hughes, D. C., Orchard, J. W., Partridge, E. M., La Gerche, A. & Broderick, C. Return to exercise post-COVID-19 infection: A pragmatic approach in mid-2022. J. Sci. Med. Sport. 25, 544 (2022).
Spanish Society of Sports Medicine. Recommendations of the Spanish Society of Sports Medicine for Athletes who have suffered from Sars-Cov-2 Infection. (2022). https://www.femede.es/documentos/Recomendaciones_reinicio_deporte-COVID-1.pdf [Accessed January 29, 2025].
Dawes, H. N. et al. Borg’s rating of perceived exertion scales: do the verbal anchors mean the same for different clinical groups? Arch. Phys. Med. Rehabil. 86, 912–916 (2005). chrome- (2005).
Malsagova, K. A. et al. Sports nutrition: diets, selection factors, recommendations. Nutrients 13, 3771 (2005).
Thomas, D. T., Erdman, K. A. & Burke, L. M. Position of the academy of nutrition and dietetics, dietitians of canada, and the American college of sports medicine: nutrition and athletic performance. J. Acad. Nutr. Diet. 116, 501–528 (2016).
World Anti-Doping Agency (WADA). ISTI Guidelines for Sample Collection. (2025). https://www.wada-ama.org/en/resources/world-anti-doping-program/isti-guidelines-sample-collection [Accessed January 29, 2025].
Van Beaumont, W. Evaluation of hemoconcentration from hematocrit measurements. J. Appl. Physiol. 32, 712–713 (1972).
de Oliveira, A. et al. The importance of adjustments for changes in plasma volume in the interpretation of hematological and inflammatory responses after resistance exercise. J. Exerc. Physiol. 17, 72–83 (2014).
Ferguson, C. J. An effect size primer: A guide for clinicians and researchers. Prof. Psychol. Res. Pract. 40, 532–538 (2009).
Hróbjartsson, A., Forfang, E., Haahr, M. T., Als-Nielsen, B. & Brorson, S. Blinded trials taken to the test: an analysis of randomized clinical trials that report tests for the success of blinding. Int. J. Epidemiol. 36, 654–663 (2009).
World Medical Association World Medical Association Declaration. Of helsinki: ethical principles for medical research involving human subjects. JAMA 310, 2191–2194 (2013).
Abouzeid, N., ELnaggar, M., FathAllah, H. & Amira, M. Eight weeks of High-Intensity interval training using elevation mask May improve cardiorespiratory fitness, pulmonary functions, and hematological variables in university athletes. Int. J. Environ. Res. Public. Health. 20, 3533 (2023).
Barbieri, J. F. et al. The effect of an airflow restriction mask (ARM) on metabolic, ventilatory, and electromyographic responses to continuous cycling exercise. PLoS One. 15, 0237010 (2020).
Boyle, K. G., Napoleone, G., Ramsook, A. H., Mitchell, R. A. & Guenette, J. A. Effects of the elevation training Mask® 2.0 on dyspnea and respiratory muscle mechanics, electromyography, and fatigue during exhaustive cycling in healthy humans. J. Sci. Med. Sport. 25, 167–172 (2022).
Mathew, T. M. & Sharma, S. High Altitude Oxygenation. StatPearls. (2023).
Roczniok, R. et al. Impact of SARS-CoV-2 on aerobic and anaerobic capacity in professional ice hockey players. J. Clin. Med. 14, 3478 (2025).
Roels, B. et al. Effects of hypoxic interval training on cycling performance. Med. Sci. Sports Exerc. 37, 138–146 (2005).
Biggs, N. C., England, B. S., Turcotte, N. J., Cook, M. R. & Williams, A. L. Effects of simulated altitude on maximal oxygen uptake and inspiratory fitness. Int. J. Exerc. Sci. 10, 127–136 (2017).
Oko, I. A. et al. L.I. Moderate aerobic exercise improves haematological indices without altering cardio-metabolic enzyme activities in sedentary healthy young adults. BMC Sports Sci. Med. Rehabil. 28, 32 (2025).
Petro, J. L., Idarraga, L., Buriticá, A., Ramírez, L. E. & Bonilla, D. A. Response of hematological parameters to a high-intensity interval training session of the CrossFit® type. Phys. Educ. Sport. 35, 43–62 (2017).
Fernández-Lázaro, D. et al. The effects of 6 weeks of tribulus terrestris L. Supplementation on body composition, hormonal response, perceived exertion, and CrossFit® performance: A randomized, Single-Blind, Placebo-Controlled study. Nutrients 13, 3969 (2021).
Fernández-Lázaro, D. et al. 6-Week supplementation with tribulus terrestris L. to trained male CrossFit® athletes on muscle, inflammation, and antioxidant biomarkers: A randomized, Single-Blind, Placebo-Controlled trial. Int. J. Environ. Res. Public. Health. 19, 6158 (2022).
Fernández-Lázaro, D. et al. Effects on respiratory pressures, spirometry biomarkers, and sports performance after inspiratory muscle training in a physically active population by Powerbreath®: A systematic review and Meta-Analysis. Biology (Basel). 12, 0056 (2022).
Fernández-Lázaro, D. et al. Inspiratory muscle training program using the PowerBreath®: does it have ergogenic potential for respiratory and/or athletic performance?? A systematic review with Meta-Analysis. Int. J. Environ. Res. Public. Health. 18, 6703 (2021).
Jagim, A. R. et al. Acute effects of the elevation training mask on strength performance in recreational weight lifters. J. Strength. Cond Res. 32, 482–489 (2018).
López-Pérez, M. E., Romero-Arenas, S., Colomer-Poveda, D., Keller, M. & Márquez, G. Undefined Psychophysiological responses during a cycling test to exhaustion while wearing the elevation training mask. J. Strength. Cond Res. 36, 1282–1289 (2022).
Acknowledgements
The authors would like to thank the Ministry of Science and Innovation of the Government of Spain for funding the study and the recognized research group “Neurobiology” of the University of Valladolid for their collaboration and CIBEROBN is an initiative of the Carlos III Health Institute, Spain.
Funding
This study was funded by Project PID2022-141358OBI00 of the Call for Projects Knowledge Generation-Oriented Research 2022 of the Spanish Research Agency, FEDER Funds, and the Ministry of Science and Innovation of the Government of Spain. Principal Investigator: Dr. Diego Fernández Lázaro.
Author information
Authors and Affiliations
Contributions
DJD: Data curation, Formal Analysis, Methodology, Investigation, Software, Supervision, Validation, Visualization.MG: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.JFGS: Conceptualization, Data curation, Formal Analysis, Investigation, Resources, Supervision, Validation. GS: Data curation, Formal Analysis, Investigation, Supervision, Validation, Visualization, Writing – review & editing.JSC: Data curation, Formal Analysis, Investigation, Methodology, Supervision, Project administration, Resources, Validation, Funding acquisition, Visualization. ER: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization and Writing – review & editing.ALL: Data curation, Formal Analysis, Investigation, Supervision, Validation, Visualization, Writing – review & editing.DFL: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Validation, Visualization, Supervision, Project administration, Writing – original draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Institutional review board statement
This study was conducted in accordance with the Declaration of Helsinki, and it was approved by the Institutional Review Board (Ethics Committee) of the Ethics Committee for Drug Research in the Valladolid area (PI 19-1361) and date of approval was April 25, 2019. ClinicalTrials.gov, identifier (ID NCT06806124). The trial was registered on February 3, 2025.
Informed consent statement
All participants signed informed consent before examination.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jerves-Donoso, D., Garrosa, M., Garcia-Sierra, J.F. et al. Analysis of blood biomarkers and sports performance in crossfit athletes using the elevation training mask 2.0 post SARS-CoV-2 infection. Sci Rep 15, 29547 (2025). https://doi.org/10.1038/s41598-025-14916-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-14916-x