Abstract
Data on liver issues including liver cirrhosis, hepatocellular carcinoma, and hepatic failure in renal transplant patients with HCV infection are scarce. In the present study, we conducted a large-scale population-based analysis to investigate the long-term outcomes of renal recipients with HCV infection. Propensity score matching with a ratio of 1:1 was applied. A total of 6,473renal recipients with HCV infection in case group were enrolled after PSM. Our findings showed that subjects with HCV infection in kidney transplant had significantly higher risk of hepatoma, cirrhosis, hepatic failure, and overall hepatic disease than those without HCV infection. (hepatoma: HR: 8.957; 95% CI: 5.324–15.069; cirrhosis: HR: 5.378; 95% CI: 4.363–6.631; hepatic failure: HR: 3.258; 95% CI: 2.527-4.200; overall hepatic disease: HR: 4.128; 95% CI: 3.428–4.971). In the present study, our findings show that renal recipients with HCV infection is significantly associated with a remarkably high risk of hepatic complications post-kidney transplantation.
Similar content being viewed by others
Introduction
Hepatitis C virus infection is a global health problem worldwide. It is a well-known entity of liver disease, but HCV infection has also been reported in patients with chronic renal failure. For example, it has been estimated that hepatitis C virus (HCV) has infected approximately 1% of the general population in the US, with rates of up to 3–14% in patients with chronic kidney disease (CKD)1.
In dialysis patients, HCV infection rates of 10–65% have been reported and 6–46% of kidney transplant recipients were reported to be infected with HCV, which suggests that overall HCV prevalence may reach as high as 5 times greater in chronic kidney disease compared with the general population2,3.
For patients with end-stage renal disease (ESRD), kidney transplantation offers a better quality of life compared to that of patients on dialysis. Kidney transplantation is still considered to be a better treatment for ESRD with HCV infection compared with those remaining on dialysis4,5,6. Hence, HCV infection status in ESRD patients does not affect their suitability to receive kidney transplantation7,8,9,10,11.
However, some concerns still exist in renal transplant recipients, including cardiovascular disease, malignancy, and infection risk. HCV infection has been demonstrated to possibly adversely affect long-term outcomes of kidney transplantation because of post-transplant renal allograft nephropathy, post-transplantation diabetes mellitus, and various liver diseases. In HCV renal transplantation, higher risk of post-transplant glomerulonephritis was reported in renal recipients12. Additionally, a pyramid of evidence suggests that post-transplant diabetes is significantly associated with cardiovascular events in renal recipients and that HCV has also been associated with a higher risk for insulin resistance and diabetes mellitus post-transplantation5. Moreover, hepatic complications are still a critical concern in HCV recipients after transplantation including liver cirrhosis, hepatocellular carcinoma (HCC), and hepatic failure. In cases who develop tumor or cirrhosis caused by the detrimental effect of HCV, a much longer period of time is warranted after transplantation13. Data on liver issues in renal transplant patients with HCV infection are scarce and most previous studies have been limited by very small sample sizes without a long observational period, limited comorbidity data, and in particular a lack of information on HCV sero-status in registry datasets, as well as a lack of comparable control cases4. In the present study, we conducted a large-scale population-based analysis to investigate the long-term outcomes of renal recipients with HCV infection.
Methods and materials
Our study population was drawn from 89 Healthcare Organizations (HCOs), comprising 195,071 transplant individuals. Patients who received kidney transplantation [ICD-10: Z94.0] and had been diagnosed with HCV before kidney transplantation served as the case group in this study, while those who were not diagnosed with HCV before kidney transplantation served as the control group. Propensity score matching with a ratio of 1:1 was applied, which was based on sex, age at index, and comorbidities.
Data source
TriNetX is a multicenter federated health research network that includes various healthcare institutions, such as academic medical centers, specialty physician practices, and community hospitals. They provide electronic health records (EHR) data, which are anonymized to protect identifiable patient health information, and ensure that the data remains de-identified in all circumstances. As a federated network, research studies using TriNetX do not require ethical approval or patient informed consent since no identifiable information is received. The specific database we utilized within TriNetX is the Research Network. The available data in this database include demographics and diagnoses, which are coded using ICD-10 (International Classification of Diseases, 10th edition).
Study population
Our study population was drawn from 89 Healthcare Organizations (HCOs), comprising 195,071 transplant individuals. Patients who received kidney transplantation [ICD-10: Z94.0] and had been diagnosed with HCV before kidney transplantation served as the case group in this study, while those who were not diagnosed with HCV before kidney transplantation served as the control group. Propensity score matching with a ratio of 1:1 was applied, which was based on sex, age at index, and comorbidities. Participants who were aged < 18 years were eliminated from the study.
Main outcome and covariates
There were seven outcomes in this study, which were all defined at least one year follow-up time after the index event. The outcomes of interest were:
-
(1)
Death.
-
(2)
Overall hepatic disease: Liver cell carcinoma (ICD-10: C22.0), Liver (ICDO3: C22.0), Fibrosis and cirrhosis of liver (ICD-10: K74), Hepatic failure, not elsewhere classified (ICD-10: K72).
-
(3)
Hepatoma: Liver cell carcinoma (ICD-10: C22.0), Liver (ICDO3: C22.0).
-
(4)
Cirrhosis: Unspecified cirrhosis of liver (ICD-10: K74.60), Hepatic fibrosis (ICD-10: K74.0).
-
(5)
Hepatic failure (ICD-10: K72).
-
(6)
Graft failure: Dependence on renal dialysis (ICD-10: Z99.2), Creatinine [Mass/volume] in Serum, Plasma or Blood (at least 6.00 mg/dL) (TNX:9024), Glomerular filtration rate/1.73 sq M.predicted [Volume Rate/Area] in Serum, Plasma or Blood by Creatinine-based formula (MDRD) (at most 5.00 mL/min/{1.73_m2}(TNX:8001), Glomerular filtration rate/1.73 sq M.predicted [Volume Rate/Area] in Serum, Plasma or Blood by Creatinine-based formula (CKD-EPI) (at most 5.00 mL/min/{1.73_m2} (LNC:62238-1).
-
(7)
Rejection (ICD-10: T86.11): Furthermore, we incorporated some covariates in our study, such as age, sex, race, ethnicity, some related comorbidities, and medications. The related comorbidities included hypertension (ICD-10: I10-I15), heart failure (ICD-10: I50), type 2 diabetes mellitus (ICD-10: E11), overweight and obesity (ICD-10: E66), glomerular diseases (ICD-10: N00-N08), and Unspecified viral hepatitis B (ICD-10: B19.1). For medications, we included glucocorticoids tacrolimus, mycophenolate mofetil, mycophenolic acid, and basiliximab. The relevant comorbidities and medications were defined within 10 years before the index date.
Statistical analyses
Baseline categorical variables were assessed by chi-square test, and the difference of mean age and follow-up time was estimated by the Student’s t test. HRs with 95% CIs were calculated using a proportional hazard model wherein the cohort to which the patient belonged was used as the independent variable. The proportional hazard assumption was tested using the generalized Schoenfeld approach built in the TriNetX platform. Survival probability was demonstrated using Kaplan–Meier’s survival curve and the log-rank test was also used to calculate the difference. All analyses were performed on the TriNetX platform. The statistical significance level was set at a two-sided p-value of < 0.05. Additionally, differences in all variables between the two cohorts were also compared by the standardized mean difference (SMD). If the SMD value was less than 0.1, the difference between the two cohorts was considered negligible.
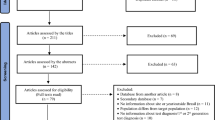
Comparison of overall hepatic disease (A), hepatoma (B) and cirrhosis (C) between renal recipients with and without chronic hepatitis c virus infection in panel A, B and C, respectively. A high risk of overall hepatic disease, hepatoma and cirrhosis was noted in renal recipients with HCV which reached statistical significance (p < 0.001).
Results
Table 1 shows the demographic characteristics and comorbidities of the case and control groups before and after propensity score matching. In the study population, over 60% of the patients were male and aged 40–65 years. Additionally, we found that the majority of the study population was not Hispanic or Latino. After matching, the differences in demographic characteristics and comorbidities between the two groups were small and well matched.
We observed that before matching, the number of individuals in each age group varied between the HCV and non-HCV groups (age 18–40: 344 vs. 33150 / age 40–65: 4399 vs. 99991 / age > 65: 1741 vs. 41721). After matching, the number of individuals in each age group tended to be similar between the two groups (age 18–40: 344 vs. 358 / age 40–65: 4390 vs. 4391 / age > 65: 1736 vs. 1721). Furthermore, the number of individuals in each gender also varied between the HCV and non-HCV groups (male: 4434 vs. 100450 / female: 1803 vs. 72618). However, after matching, the number of males and females in the HCV and non-HCV groups also tended to be similar (male: 4425 vs. 4423 / female: 1801 vs. 1797).
As Table 2 shows, subjects with HCV after receiving a kidney transplant had significantly higher risk of death, hepatoma, cirrhosis, hepatic failure, and overall hepatic disease than those without HCV after receiving a kidney transplant in this study cohort (death: HR: 1.19; 95% CI: 1.098–1.290; P =<0.001 / hepatoma: HR: 8.957; 95% CI: 5.324–15.069; P =<0.001 / cirrhosis: HR: 5.378; 95% CI: 4.363–6.631; P =<0.001 / hepatic failure: HR: 3.258; 95% CI: 2.527-4.200; P =<0.001 / overall hepatic disease: HR: 4.128; 95% CI: 3.428–4.971; P =<0.001). However, subjects with HCV after receiving a kidney transplant had significantly lower risk of graft failure and rejection than those without HCV after receiving a kidney transplant in this study cohort (graft failure: HR: 0.696; 95% CI: 0.597–0.812; P =<0.001 / rejection: HR: 0.696; 95% CI: 0.598–0.807; P =<0.001). As shown in Table 3, before PSM, among female or male patients, the risk of death in patients who had been diagnosed with HCV after receiving a kidney transplant was significantly higher than that of the non-HCV patients after receiving a kidney transplant (female: aHR: 1.448; 95%CI: 1.300-1.612 / male: aHR: 1.406; 95%CI: 1.319–1.499). Similarly, patients aged 18 to 40 years old and 40 to 65 years old showed the same trend (age 18–40: aHR: 4.084; 95%CI = 2.651–6.293 / age 40–65: aHR: 1.663; 95%CI = 1.502–1.842). Furthermore, regardless of whether the subjects were male or female, the risk of Overall hepatic Disease in patients who had been diagnosed with HCV after receiving a kidney transplant was significantly higher than in the non-HCV group (female: aHR: 4.832; 95%CI: 3.865–6.041 / male: aHR: 5.692; 95%CI: 4.985–6.499). In patients of different age groups receiving a kidney transplant, the results also showed that the risk of Overall hepatic Disease was significantly higher in patients who had been diagnosed with HCV receiving kidney transplant compared to those not diagnosed with HCV after the transplant (age 18–40: aHR: 6.184; 95%CI = 2.755–13.879 / age 40–65: aHR: 5.104; 95%CI = 4.206–6.193/ age > 65: 5.017; 95%CI = 4.384–5.742).
After PSM, it can be seen that in male patients, the risk of death was significantly higher in those diagnosed with HCV after receiving a kidney transplant compared to those not diagnosed with HCV after the kidney transplant (male: aHR: 1.198; 95%CI: 1.091–1.317). Patients aged 18 to 40 years old and 40 to 65 years old also showed the same results as male patients (age 18–40: aHR: 2.408; 95%CI = 1.160–4.998 / age 40–65: aHR: 1.394; 95%CI = 1.193–1.629). When we examined Overall hepatic Disease, prevalence rates in patients who had been diagnosed with HCV after receiving a kidney transplant were significantly higher than those of the non-HCV cohort (female: aHR: 3.150; 95%CI: 2.211–4.486 / male: aHR: 4.649; 95%CI: 3.710–5.825). Additionally, regardless of age group the risk of Overall hepatic Disease was significantly higher in patients who had been diagnosed with HCV after receiving a kidney transplant compared to those who had not been diagnosed with HCV after the transplant (age 18–40: aHR: 5.351; 95%CI = 1.077–26.587 / age 40–65: aHR: 4.211; 95%CI = 1.502–1.842/ age > 65: 3.712; 95%CI = 3.013–4.573).
Furthermore, most of the comorbidity results indicated that regardless of whether patients had comorbidities, those diagnosed with HCV after receiving a kidney transplant had a significantly higher risk of death and Overall hepatic Disease compared to those not diagnosed with HCV after the transplant.
The Kaplan-Meier curve of survival probability of death, renal allograft are shown in Fig. 1A, B and overall hepatic disease including hepatoma, cirrhosis and hepatic failure in Fig. 2 A, B, C, respectively after PSM selection.
Discussion
In the present 10-year observational study, associated confounding factors including age, transplant year, sex, and comorbidities, such as hypertension, diabetes mellitus, obesity, primary glomerulonephritis and immunosuppressant agents, were included in a large-scale analysis of a HCV renal recipient cohort that was propensity score-matched with a non-HCV renal cohort. Our findings showed that there was only a slightly higher mortality risk among renal recipients with HCV infection, with a 1.19-fold increased mortality risk. In a previous study, a high mortality and graft failure risk was reported in HCV-infected renal recipients. HCV renal recipients were thus presumed to have a greater likelihood of having an unfavorable outcome after kidney transplantation14. Moreover, a higher risk for death was found during the first 6 months after transplant. However, transplantation still had a superior outcome compared with remaining on dialysis in terms of long-term outcomes in an investigation of patients receiving either transplantation or continuing to receive hemodialysis15. In the present study, we directly compared renal recipients with and without HCV infection, and the findings showed only a slightly increased risk of mortality in HCV infection, suggesting a significant improvement in post-transplantation care for HCV-infected renal recipients. Moreover, our findings showed a favorable survival of renal allograft in HCV infection with a significantly lower risk of graft failure (0.696-fold decrease). This result is consistent before and after propensity score matching, which reached statistical significance. In previous studies, the risk associated with renal allograft loss was remarkably attenuated in multivariable models that included associated confounders, such as longer duration of waiting list, higher PRA, and re-transplantation16. Our findings support results reported in previous studies.
In kidney transplantation with HCV infection, whether HCV infection could increase the risk of acute rejection remains considerably controversial5,14. ,17,18,19,20 In the previous literature, the results were conflicting because certain data, including PRA level, waiting time, and immunosuppressive agents, such as induction therapy, were not assessed, and many studies had small case numbers with a short study period6. In the present study, our results showed a lower risk of renal allograft rejection in HCV-infected recipients. There was a 0.561-fold decreased risk before PSM and 0.694-fold decreased risk after PSM, which both reached statistical significance. These findings are notable as they have never been reported previously. In the case of HCV-infected renal recipients, a previous study suggested that a decreased number of naive T helper lymphocytes, as well as low responses of T helper lymphocytes to stimulation by mitogens would result in an immunodeficient state and that may account for the decreased acute rejection risk in HCV-infected renal recipients6,21. Our results appear to provide solid evidence supporting these findings. Taken together, in comparison to the renal recipients without HCV infection, a distinct improvement of renal allograft survival with a lower graft failure risk and a low rejection risk was noted in this study. The application of modern immunosuppression and superior post-transplant care may account for the better renal allograft results in this study.
Hepatic complications remain a major concern in renal recipients with chronic HCV infection and data on the cause-specific risks of liver cirrhosis, hepatoma, and liver failure post-transplantation remain lacking. Previous studies suggested that HCV-infected recipients had higher death rates caused by liver disease than HCV-negative patients in a univariate analysis22,23,24,25. In the present study, multiple relevant variables were included to eliminate bias to the greatest extent possible through propensity score matching. A comparison of renal recipients groups with and without HCV infection demonstrated that HCV-infected recipients were significantly associated with a remarkably high risk of hepatic complications post-kidney transplantation. A 5.425-fold increased risk was noted before PSM, which was consistent with a 4.128-fold risk after PSM. Moreover, a 12.12-fold increased risk of new onset hepatoma post-kidney transplantation was observed before PSM and there was an 8.957-fold greater risk after PSM. With respect to other hepatic complications, including liver cirrhosis as well as hepatic failure, the trend was consistent and was significantly different. To the best of our knowledge, this is the first study to report the cause-specific risk ratio of post-transplantation hepatic disease, including hepatoma, cirrhosis, and liver failure in renal recipients with HCV infection. To date, the hepatoma risk in HCV-infected recipients has been neglected and data on the hepatoma risk post-transplantation in HCV-infected recipients remain lacking. In one study with a small case number, very few isolated cases of hepatocellular carcinoma (HCC) were reported. It has been proposed that the risk of developing chronic liver disease post-transplantation is closely associated with duration of disease, possibly over 20 years26. A high risk of HCC post-transplantation was observed in the study, which reached a 8.957-fold increased risk in HCV-infected transplantation and this finding has never been reported previously. Our findings indicate that hepatic complications after kidney transplantation remain a major concern in renal recipients with HCV infection, which has to date been neglected.
Our study was focused on hepatic outcomes and did not explore non-hepatic post-transplant complications (e.g., cardiovascular events, new-onset diabetes), which are also clinically important and warrant further investigation in future studies.
Recently, direct-acting antivirals (DAAs) have been demonstrated to dramatically transform the care of patients with chronic hepatitis C virus (HCV) infection3,27,28,29,30. In kidney transplantation, DAAs have been demonstrated to remarkably reduce the risk of death after renal transplantation and that early commencement of DAAs post-transplantation would improve patient and allograft survival among HCV-positive recipients3. Because a high risk of hepatic complication has been demonstrated, early eradication of HCV infection is recommended for patients requiring renal transplantation17.
Limitations
While, the results presented herein are robust, there were some limitations in this study. First, some clinical data associated with renal transplant recipients could not be obtained. For example, although the important etiology of acute rejection could be identified in the database, other findings regarding renal allograft biopsy and relevant immunological data could not be accessed to further clarify the etiology of renal allograft failure, such as post-transplant glomerulonephritis related to HCV, Bk virus nephropathy, chronic pyelonephritis and CNI nephropathy. Second, because of the observational nature of this study, some inherent bias may have existed despite the inclusion of associated confounders in the analysis of propensity score matching (PSM).
Conclusion
Improvements of patient and renal allograft survival were noted in renal recipients with HCV infection. However, post-transplantation liver complications remain a major concern in renal recipients with HCV infection. Further research on renal recipients with HCV is warranted, particularly with respect to the role of DAA, which is a highly effective treatment in HCV infection.
Data availability
Data from the TriNetX database is not publicly available. However, the data of this study are openly accessible upon reasonable request to the TriNetX administrators through their website ( https://trinetx.com) as well as that the corresponding author may also be contacted.
Abbreviations
- HCV:
-
Hepatitis C virus
- CKD:
-
Chronic kidney disease
- ESRD:
-
End stage renal disease
- HCC:
-
Hepatocellular carcinoma
- ICD-10-CM:
-
International classification of diseases, 10th edition, clinical modification
- EHR:
-
Electronic health records
- CIs:
-
Confidence intervals
- SMD:
-
Standardized mean difference
- HR:
-
Hazard ratio
- PSM:
-
Propensity score matching
- PRA:
-
Panel reactive antibodies
References
Saab, S., Martin, P., Brezina, M., Gitnick, G. & Yee, H. F. Jr. Serum Alanine aminotransferase in hepatitis c screening of patients on Hemodialysis. Am. J. Kidney Dis. 37 (2), 308–315 (2001).
Yu, T. M. et al. Increased risk of hepatic complications in kidney transplantation with chronic virus hepatitis infection: A nationwide population-based cohort study. Sci. Rep. 6, 21312 (2016).
Axelrod, D. A. et al. The impact of direct-acting antiviral agents on liver and kidney transplant costs and outcomes. Am. J. Transpl. 18 (10), 2473–2482 (2018).
Sawinski, D. et al. Mortality and kidney transplantation outcomes among hepatitis C Virus-Seropositive maintenance Dialysis patients: A retrospective cohort study. Am. J. Kidney Dis. 73 (6), 815–826 (2019).
Ladino, M., Pedraza, F. & Roth, D. Hepatitis C virus infection in chronic kidney disease. J. Am. Soc. Nephrol. 27 (8), 2238–2246 (2016).
Morales, J. M. & Fabrizi, F. Hepatitis C and its impact on renal transplantation. Nat. Rev. Nephrol. 11 (3), 172–182 (2015).
Roth, D. et al. Effect of kidney transplantation on outcomes among patients with hepatitis C. J. Am. Soc. Nephrol. 22, 1152–1160 (2011).
Sezer, S. et al. Renal transplantation offers a better survival in HCV infected ESRD patients. Clin. Transpl. 18, 619–623 (2004).
Knoll, G. A., Tankersley, M. R., Lee, J. Y., Julian, B. A. & Curtis, J. J. The impact of renal transplantation on survival in hepatitis C-positive end-stage renal disease patients. Am. J. Kidney Dis. 29, 608–614 (1997).
Pereira, B. J. et al. Effects of hepatitis C infection and renal transplantation on survival in end-stage renal disease. Kidney Int. 53, 1374–1381 (1998).
Bloom, R. D. et al. Outcome of hepatitis C virus-infected kidney transplant candidates who remain on the waiting list. Am. J. Transpl. 5, 139–144 (2005).
Baid-Agrawal, S. et al. Overlapping pathways to transplant glomerulopathy: chronic humoral rejection, hepatitis C infection, and thrombotic microangiopathy. Kidney Int. 80, 879–885 (2011).
Legendre, C. et al. Harmful long-term impact of hepatitis C virus infection in kidney transplant recipients. Transplantation 65, 667–670 (1998).
Fabrizi, F., Martin, P., Dixit, V., Bunnapradist, S. & Dulai, G. Hepatitis C virus antibody status and survival after renal transplantation: meta-analysis of observational studies. Am. J. Transpl. 5 (6), 1452–1461 (2005).
Roth, D. et al. Effect of kidney transplantation on outcomes among patients with hepatitis C. J. Am. Soc. Nephrol. 22 (6), 1152–1160 (2011).
Forman, J. P., Tolkoff-Rubin, N., Pascual, M., Lin, J. & Hepatitis, C. Acute humoral rejection, and renal allograft survival. J. Am. Soc. Nephrol. 15 (12), 3249–3255 (2004).
Terrault, N. A. & Adey, D. B. The kidney transplant recipient with hepatitis C infection: pre- and posttransplantation treatment. Clin. J. Am. Soc. Nephrol. 2 (3), 563–575 (2007).
Meier-Kriesche, H. U., Ojo, A. O., Hanson, J. A. & Kaplan, B. Hepatitis C antibody status and outcomes in renal transplant recipients. Transplantation 72, 241–244 (2001).
Rao, K. V. & Ma, J. Chronic viral hepatitis enhances the risk of infection but not acute rejection in renal transplant recipients. Transplantation 62, 1765–1769 (1996).
Ponz, E. et al. Hepatitis C virus infection among kidney transplant recipients. Kidney Int. 40, 748–751 (1991).
Corell, A. et al. Immunosuppression induced by hepatitis C virus infection reduces acute renal-transplant rejection. Lancet 346 (8988), 1497–1498 (1995).
Pereira, B. J. G., Wright, T. L., Schmid, C. H. & Levey, A. S. The impact of pretransplantation hepatitis C infection on the outcome of renal transplantation. Transplantation 60, 799–805 (1995).
Bouthot, B. A., Murthy, B. V. R., Schmid, C. H., Levey, A. S. & Pereira, B. J. G. Long-term follow-up of hepatitis C virus infection among organ transplant recipients. Transplantation 63, 849–853 (1997).
Gentil, M. A. et al. Impaired kidney transplant survival in patients with antibodies to hepatitis C virus. Nephrol. Dial Transpl. 14, 2455–2460 (1999).
Breitenfeldt, M. K. et al. Impact of hepatitis B and C on graft loss and mortality after kidney transplantation. Clin. Transpl. 16, 130–136 (2002).
Morales, J. M. & Campistol, J. M. Transplantation in the patient with hepatitis C. J. Am. Soc. Nephrol. 11 (7), 1343–1353 (2000).
Charlton, M. et al. Ledipasvir and Sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology 149 (3), 649–659 (2015).
Alqahtani, S. A. et al. Safety and tolerability of ledipasvir/sofosbuvir with and without ribavirin in patients with chronic hepatitis C virus genotype 1 infection: analysis of phase III ION trials. Hepatology 62 (1), 25–30 (2015).
Reddy, K. R. et al. Ledipasvir and Sofosbuvir in patients with genotype 1 hepatitis C virus infection and compensated cirrhosis: an integrated safety and efficacy analysis. Hepatology 62 (1), 79–86 (2015).
Curry, M. P. et al. Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N Engl. J. Med. 373 (27), 2618–2628 (2015).
Acknowledgements
We are grateful to Taichung veterans general hospital for providing administrative, technical and funding support. The funders had no role in the study design, data collection and analysis, the decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly, and that all authors are in agreement with the content of the manuscript: Conceptualization: Shih-Ting Huang, Shih-Sheng Chang, Ya-Wen Chuang, Chih-Wei Chiu, I-Kuan Wang, Brain K Lee, Shiang-Cheng Kung, Chi-Yuan Li, Kuo-Ting Sun, Tung-Min YuMethodology: Shih-Ting Huang, Ya-Wen Chuang, Chih-Wei Chiu, Chi-Yuan Li, Tung-Min YuSoftware: Shih-Ting Huang, Tung-Min YuValidation: Shih-Ting Huang, Ya-Wen Chuang, Chih-Wei Chiu, Chi-Yuan Li, Tung-Min YuFormal Analysis: Shih-Ting Huang, Tung-Min YuInvestigation: Shih-Ting Huang, Tung-Min YuResources: Shih-Ting Huang, Tung-Min YuData Curation: Shih-Ting Huang, Tung-Min YuWriting – Original Draft Preparation: Shih-Ting Huang, Tung-Min YuWriting – Review and Editing: Shih-Ting Huang, Shih-Sheng Chang, Ya-Wen Chuang, Chih-Wei Chiu, I-Kuan Wang, Brain K Lee, Shiang-Cheng Kung, Chi-Yuan Li, Kuo-Ting Sun, Tung-Min Yu.Visualization: Tung-Min YuSupervision: Tung-Min Yu.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
The study has received approval from the institutional review board (IRB) committee of Taichung Veterans General Hospital (approval number: SE22220A, TCVGH). The informed consent of the TriNetX database was waived by the Institutional Review Board of Taichung Veterans General Hospital (TCVGH) due to the anonymous nature of the database and its strict adherence to the guidelines stipulated by the Health Insurance Portability and Accountability Act and the General Data Protection Regulation (approval number: SE22220A, TCVGH).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, ST., Chuang, YW., Chiu, CW. et al. High risk of hepatic complications in kidney transplantation with chronic hepatitis C virus infection. Sci Rep 15, 29275 (2025). https://doi.org/10.1038/s41598-025-15169-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15169-4