Abstract
Focused ultrasound (FUS) has emerged as a promising neuromodulation technique for reducing regional brain excitability, offering a potential therapeutic approach for drug-resistant epilepsy (DRE). However, its underlying mechanisms remain unclear, particularly regarding functional connectivity alterations in seizure-related brain networks. This study investigates the relationship between FUS-induced seizure suppression and brain functional connectivity using EEG and resting-state fMRI (rs-fMRI). Using a pentylenetetrazol (PTZ)-induced epilepsy rat model (n = 28), we applied burst-mode FUS with 0.25 MI, ISPTA = 0.3 W/cm2 with low (30s-on-90s-off)/high (90s-on-30s-off) doses with 10-minute sonication durations to the anterior nucleus of the thalamus (ANT), resulting in approximately 36% reduction in hippocampal spike activity. Rs-fMRI analysis (36 × 36 connectivity matrix) revealed that the PTZ-induced seizure reduction strongly correlates with significant whole-brain connectivity changes, including a 45.1% decrease in connectivity between the anterior thalamic and hippocampal networks. Histological analysis confirmed that FUS preferentially modulates key brain regions involved in epileptic circuits, particularly the thalamus and hippocampus. These findings provide compelling evidence that FUS selectively alters seizure-related functional networks, highlighting its potential as a noninvasive therapeutic approach for epilepsy.
Similar content being viewed by others
Introduction
Epilepsy is a common neurological disorder characterized by neuronal excitation and hypersynchrony, resulting in abnormal electroencephalographic discharges1. Currently, over 50 million people worldwide are affected by epilepsy2,3 which can be classified into focal epilepsy with onset in a specific region of the brain and generalized epilepsy with bi-hemispheric onset4. Generalized seizures are associated with abnormal discharges in brain circuits and connecting axonal fiber bundles in multiple bilateral brain regions5. Despite the development of over 20 anti-seizure medications for treating epilepsy, more than one-third of epilepsy patients show a therapeutically inadequate response, a condition known as Drug-Resistant Epilepsy (DRE)6. For some patients with DRE, resection surgery or laser ablation is an option. However, surgery has risks and is not suitable for patients with poorly localized or widespread seizure onset zones or seizure onsets involving eloquent cortex7.
Neuromodulation, often loosely called neurostimulation, is another approach to DRE. The United States Food and Drug Administration approved therapies based on deep brain stimulation (DBS), vagus nerve stimulation (VNS), and responsive neurostimulation (RNS)8. The Circuit of Papez, connecting the hippocampus to posterior hypothalamus, anterior nucleus of thalamus (ANT) and cingulate is involved in many seizures originating in mesial temporal and frontal lobes, rendering ANT as an attractive target for some focal onset seizures9,10. However, VNS, RNS and DBS are invasive and not always effective. Noninvasive transcranial magnetic stimulation and transcranial direct current stimulation have reduced seizures in several laboratory and clinical trials, but they also have limitations. Electromagnetic energy is difficult to focus and deliver to deep brain structures11,12.
Focused ultrasound (FUS) offers accurate and non-invasive targeting of specific brain regions, including deep sites. FUS can modulate neural activity in animal models, temporarily affecting sodium or calcium ion channels13. In one drug-induced animal epilepsy model, two three-minute sessions of FUS significantly reduced abnormal brain electrical discharges14. Chen et al. observed the effective suppression of epileptic spikes with FUS by deactivating excitatory cells and stimulating GABAergic inhibitory neurons15. Recent research indicates that transcranial ultrasound stimulation has a neuroprotective action in chronic epilepsy models, inhibiting epileptic bursts at the onset of seizures16 and effectively improving the abnormal behavior and focal brain atrophy produced by the convulsant, kainic acid17,18. In patients with DRE, Lee et al. used a neuro-navigated FUS system to treat the seizure onset zone in DRE patients and observed intracranial EEG power changes without lesions or signs of brain edema19. A pilot study in the Taipei Veterans General Hospital on six patients with focal onset epilepsy showed seizure reduction in two and general safety, except for one provoked seizure19. A United States pilot trial targeting hippocampus in six sessions over three weeks resulted in a significant mean reduction in seizure frequency in six patients with temporal lobe epilepsy20. Despite these suggestions of efficacy of FUS for focal DRE, the mechanisms of action remain largely unknown.
Seizures develop and propagate through brain networks. Connectivity of different regions of the network is altered in epilepsy, with a seizure focus often having increased connectivity with multiple brain regions, even in the resting state21. Other studies with resting-state functional MRI (rs-fMRI) identified reduced functional connectivity between bilateral thalami in patients with right temporal lobe epilepsy (TLE)22. One potential mechanism of FUS might be to partially normalize seizure-induced connectivity changes. Connectivity can be measured by rs-fMRI or EEG23. rs-fMRI measures the coincidence and correlation of the synchronized changes in blood oxygen levels across various brain regions, enabling the assessment of functional connectivity24,25. EEG frequencies in the 4–8 Hz theta band can correlate with seizure onsets at a specific brain target1,26.
This study aims to elucidate the neuromodulatory effects of FUS on epileptic suppression by EEG analysis with rs-fMRI in a rodent model of epilepsy. Specifically, we chose the ANT because it serves as a central hub in seizure propagation, effectively modulating epileptic activities through extensive connections with critical regions such as the hippocampus and cingulate cortex. Additionally, the Circuit of Papez was targeted due to its recognized role in facilitating seizure spread across interconnected brain regions. Lastly, ANT is currently the only United States FDA-approved target for treating focal-onset epilepsy with deep brain stimulation. By targeting these specific neural pathways, this study investigates whether FUS can effectively modulate seizure-related brain networks and restore functional connectivity. Our study provides a comprehensive multi-modal assessment of FUS-induced neuromodulation, bridging the gap between functional connectivity alterations and seizure suppression. Unlike previous studies focusing solely on electrophysiological changes, we leverage rs-fMRI to characterize the network-level effects of FUS in epilepsy. The results demonstrated a significant reduction in EEG epileptic activity following FUS stimulation, accompanied by altered functional connectivity in the targeted brain region. By demonstrating a significant correlation between EEG spike suppression and functional connectivity normalization. Our findings support the potential of FUS as a precise, noninvasive alternative to conventional neuromodulation techniques.
Results
FUS modulates pentylenetetrazol (PTZ)-induced epileptiform activity: EEG and fMRI observations
A FUS transducer targeted the anterior nucleus of the thalamus (ANT) to modulate epileptiform signal propagation in the pentylenetetrazol (PTZ)-FUS group throughout the experimental time course, assessing FUS effects on epileptic activity. EEG and rs-fMRI monitoring were conducted to evaluate neuronal activity in experimental animals, with an MR-compatible electrode implanted in the hippocampus.
Following intraperitoneal injection of PTZ, animals in the PTZ-alone and PTZ-FUS groups exhibited an increase in EEG spikes, compared to normal controls (Fig. 1). During the 60-minute EEG measurements, PTZ injection doses ranging from 40 to 70 mg/kg induced a dose-dependent increase in spikes within 10 min after injection (see Supplementary S1). At the dose of 70 mg/kg, the EEG spike signals showed no declining trend even after 60 min, so 70 mg/kg PTZ was selected as the optimized dose for subsequent EEG/rs-fMRI analysis. Following a 10-minute FUS exposure, spikes declined over the subsequent 40 min, compared to the PTZ-alone group (Fig. 1). During the ultrasound exposure, the strong radiofrequency emissions produced severe EEG and fMRI artifact and therefore data could not be analyzed during the actual FUS treatment times.
The Normal control group showed minimal Blood-oxygenation-level–dependent (BOLD) signals for 60 min, resulting in overall low region-to-region correlations (Fig. 1). In contrast, the PTZ-alone group showed BOLD signals with significantly increased spiking in the cortex, right hippocampus, and partial thalamus areas 10 min after PTZ injection. This coincided with the onset of EEG epileptiform discharges, sustaining for the entire 60-minute observation period (Fig. 1). Concurrently, the functional connectivity also demonstrated a significant increase (Fig. 1). In the PTZ-FUS group, BOLD signals demonstrated that FUS-induced connectivity decreases coincided with reduction in epileptiform spiking.
Longitudinal EEG and functional connectivity assessment reveals sustained FUS suppression of PTZ-Induced epileptiform spikes
Figure 2 illustrates the longitudinal and quantitative observation of FUS exposure on PTZ-induced EEG spikes and functional connectivity analysis. Animals receiving PTZ injections showed epileptiform EEG discharges for PTZ-alone and PTZ-FUS groups within 10 min. Following a 10-minute FUS exposure in the PTZ-FUS group, epileptiform discharges in the 4–8 Hz theta band showed significant reduction compared to the PTZ-alone group (see Supplementary S2A and S2B). Variable pulsing paradigms were tested (0.25 mechanical index (MI), 30% duty cycle, spatial-peak temporal average (ISPTA) = 0.3 W/cm2 with 30 s inter-stimulus interval (ISI), referred to as “high-dose”, and with 90 s ISI, referred to as “low-dose”) to examine different impacts on spike reduction.
EEG spike counts among groups in (A) Theta band (4–8 Hz), and (B) Mean correlation coefficient (C.C.) value from the functional connectivity analysis correspond to (A). * indicates significance between the PTZ-alone and Normal group (*P < 0.05, **P < 0.01, ***P < 0.001), and # indicates significance between the PTZ + FUS group and the PTZ-alone group (#P < 0.05, ##P < 0.01, ###P < 0.001).
Following PTZ administration, spike counts remained high throughout the 55-minute observation period in the PTZ-alone animals. In both “low-dose” and “high-dose” sonication groups, spike counts significantly decreased by 29–42% (p < 0.05 compared to the PTZ-alone group, Fig. 2A) with this effect lasting for 10–20 min. Therefore, data from the two groups were pooled for analysis of functional connectivity.
The additional spike count analysis of the delta (0.5–4 Hz), alpha (8–13 Hz), and gamma (40–100 Hz) bands is presented in Supplementary S3. PTZ administration resulted in an increase in epileptiform spike numbers across all three bands. Subsequent FUS stimulation led to a reduction in epileptic spike counts, demonstrating a suppressive effect in each band. Notably, the spike suppression effect was more pronounced in the delta and theta bands compared to the alpha and gamma bands. These changes are consistent with findings of Tecchio et al. in patients with epilepsy treated with transcranial cathodal direct current stimulation27.
Ten minutes after PTZ injection, both the PTZ-alone and PTZ-FUS groups (including low- and high-dose FUS exposure) exhibited increased BOLD signals—1.25 ± 0.2 a.u. in the thalamus and 1.2 ± 0.28 a.u. in the hippocampus—compared to BOLD signal of 1 ± 0.1 a.u. in the Normal group (Supplementary S4), coinciding with a marked increase in EEG spike activity. In the PTZ-FUS group, BOLD signal values decreased to 1.03 ± 0.11 a.u. in the thalamus and 1.06 ± 0.01 a.u. in the hippocampus by 60 min after FUS stimulation, paralleling the reduction in EEG spikes. In contrast, elevated BOLD signals persisted in the PTZ-alone group, suggesting that FUS inhibited abnormal neuronal activity along the epileptic propagation pathway.
At a time 10 min after PTZ injection both PTZ-alone and PTZ-FUS groups showed increased mean correlation coefficients (C.C.) analyzed in 36 paired sites (refer to Supplementary S5) in a connectivity matrix (Fig. 2B). C.C were increased from 0.23 to 0.57 within 10 min after PTZ injection, at the same time that EEG spikes greatly increased. However, unlike the sustained high spike frequency observed in the PTZ-alone group, the mean C.C. in this group gradually decreased from 10 to 60 min post-injection. Mean C.C. values in the PTZ-FUS group rapidly dropped from 0.57 to 0.25 (56% decrease, p < 0.001) at the first measured observation and then gradually elevated. Although EEG spike frequency and rs-fMRI connectivity showed distinct long-term trends following FUS, both parameters exhibited immediate post-sonication decreases. This concurrent reduction in spike change (Fig. 2A) and mean C.C. (Fig. 2B) may reflect co-existing phenomena28 associated with FUS modulation in specific brain networks .
fMRI analysis evaluates FUS-induced functional connectivity changes in PTZ epilepsy model
In order to further understand whether FUS exposure specifically influences brain-to-brain functional connectivity in animals with PTZ-induced seizures, we attempted to analyze the specific connectivity reflected by the C.C values for specific brain-to-brain regions. In order to simplify the correlation map, C.C values of the original 36 brain regions of interest were grouped into eight major epilepsy-related brain regions, including thalamus, hippocampus, primary visual cortex, cingulate cortex, retrosplenial cortex granular, somatosensory cortex, motor cortex and caudate-putamen (Fig. 3A). With the brain region grouping to eight instead of the original 36, the C.C. value increases occurred both in the PTZ-alone and PTZ-FUS groups immediately after PTZ administration; whereas, the control group remained at the original C.C baseline values. Similar to the original 36*36 C.C maps, in the treatment of FUS, the C.C values rapidly returned to the baseline level with combined eight groups. This supports the equivalence of the correlation maps between the original 36*36 and the simplified 8*8 maps.
(A) Simplified functional connectivity matrix within the PTZ-alone group and PTZ-FUS group over 60 min for specific region-to-region connectivity analysis. (B) C.C. longitudinal change of thalamus-hippocampus functional connectivity (circuit of Papez). (C) C.C. longitudinal change of thalamus-primary visual cortex functional connectivity (visual process pathway). (D) C.C. longitudinal change of cingulate cortex- retrosplenial cortex functional connectivity (default mode network). (E) C.C. longitudinal change of hippocampus-cingulate cortex functional connectivity (limbic system circuit). (F) C.C. longitudinal change of hippocampus-somatosensory cortex functional connectivity (thalamocortical circuit). (G) C.C. longitudinal change of thalamus-motor cortex functional connectivity (thalamocortical circuit). (H) C.C. longitudinal change of thalamus-caudate putamen functional connectivity (basal ganglia circuit). * denotes significant differences between the Normal group and PTZ-alone group, *p < 0.05, **p < 0.01; # denotes significant differences between the PTZ-alone group and PTZ-FUS group, #p < 0.05, ##p < 0.01.
Figure 3B and H illustrates efficacy of FUS neuromodulation across various brain circuits and the circuit of Papez (thalamus (Thal) - hippocampus (Hipp); (Fig. 3B), visual process pathway (Thal - Primary visual cortex (V1); Fig. 3C), default mode network (cingulate cortex (Cing) - retrosplenial cortex (RSC); Fig. 3D), limbic system circuit (Hipp – Cing; Fig. 3E), thalamocortical circuit (Thal - primary somatosensory cortex (S1FL); Fig. 3F), Thal - primary motor cortex (M1); Fig. 3G), and Basal ganglia circuit (Thal - caudate putamen (Cpu); Fig. 3H). Despite measurement in a model of generalized seizures, FUS exposure altered connectivity most significantly with the Thal-Hipp network.
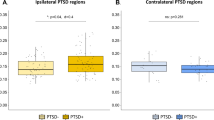
Thal-Hipp functional connectivity (Fig. 3B) remained at a baseline 0.24 ± 0.09 over the baseline period. After PTZ, C.C rapidly increased to 0.58 ± 0.17 (p < 0.05) and remained at 0.46 ± 0.16 (p < 0.05) by 30 min, and 0.38 ± 0.01 by the end of observation at one hour.
The elevated Thal-Hipp functional connectivity after PTZ injection was interrupted by FUS treatments, such that C.C. for Thal-Hipp functional connectivity significantly dropped to 0.25 ± 0.05 (45.1% decrease; p < 0.05), and the effect persisted until the end of observation period (C.C. = 0.28 ± 0.01, 26.4% decrease, p < 0.05). This demonstrates the high correlation between PTZ-induced spike suppression and the interruption of Thal-Hipp functional connection introduced by FUS exposure.
In contrast (Fig. 3C), FUS had little consistent effect on Thal-to-V1 functional connectivity. The C.C of Thal-V1 at PTZ-alone group (0.27 ± 0.14) and in the PTZ-FUS group (0.39 ± 0.14) was similar at 55 min. post of the PTZ administration, demonstrating an anatomical specificity of FUS on spike suppression.
C.C. changes from other brain regions were similar to those of Thal-V1. Both default mode network (Cing - RSC); Fig. 3D) and a limbic system network (Hipp - Cing); Fig. 3E) presented similar C.C values for PTZ-alone and PTZ-FUS groups. Similarly, thalamocortical circuits (Thal to S1FL or M1) and basal ganglia circuit (Thal to Cpu) (Fig. 3F-H), only showed transient C.C. changes. Supplementary S6 and supplementary video S1 provide topological information of these longitudinal connectivity changes among the seven brain circuits.
Histological analysis reveals FUS preferentially reduces PTZ-Induced neuronal activation in the Thalamus-Hippocampus circuit
Histological hematoxylin and eosin (H&E) staining was performed to assess neuronal damage after FUS treatment. Coronal sections of brains from the Normal and PTZ-FUS groups were examined for tissue damage (Supplementary S7). No obvious tissue disruption was observed, regardless of FUS stimulation. High magnification H&E images revealed no immune cell infiltration or microglial activation and expansion around the cortex, thalamus, or hippocampus in brain tissue of PTZ-FUS group. These findings indicate that FUS does not cause detectable histological damage in the rat brain.
In order to evaluate the effects of FUS treatments in each brain circuit from the histological perspective, c-Fos staining was conducted for the three animal groups. In the PTZ-alone group, increased c-Fos signals (compared to control group) were observed in the thalamus, hippocampus, and cortical areas, including the somatosensory, motor, and visual cortices (Fig. 4A). In the PTZ-FUS group, c-Fos staining revealed significantly lower levels of positive signals in the thalamus and hippocampus regions, compared to the PTZ-alone group. However, the c-Fos expression change in the primary visual cortex in the PTZ-FUS group was not as evident as it was in the hippocampus region after FUS-thalamus exposure, compared to the PTZ-alone group. (Fig. 4A).
C-Fos expression in the thalamus across different conditions. (A) Representative coronal sections of the thalamus from normal rats (top), PTZ-injected rats (middle), and PTZ-FUS-treated rats (bottom). The presence of c-Fos-positive cells is indicated by red arrows in the magnified images on the right panel. (B) Quantitative analysis of c-Fos-positive cell distribution across different neural circuits. The bar graphs depict the changes in c-Fos expression within the circuit of Papez (Thal-Hipp) and visual processing pathway (Thal-V1) under the following conditions: Normal, PTZ-alone, and PTZ-FUS treatment. Data are presented as mean ± SEM.
The staining signals of various brain regions with those of the thalamus were quantitatively analyzed and compared via proceeding signal counting normalization. High c-Fos expression were detected in each region in PTZ-alone group (5.59 ± 2.76 in the Thal-Hipp regions, and 6.44 ± 1.68 in the Thal-V1 regions, compared to 0.14 ± 0.01 and 2.1 ± 0.39 respectively to the Normal group; Fig. 4B). After FUS treatment, c-Fos signals in both brain circuits in PTZ-FUS animals significantly decreased, thereby approximating the signals in normal animals (down to 0.16 ± 0.04, p < 0.05) in the circuit of Papez. In the contrast, the signals remained high at 2.84 ± 0.45 in the visual process pathway, implying that anterior thalamic FUS did not directly interfere with the visual pathway, as well as confirming the connectivity change observation in Fig. 3 from a histological perspective. Anterior thalamic FUS after PTZ appears to have a preferential effect on the Thal-Hipp circuit of Papez.
Discussion
This study demonstrates that FUS targeting the anterior nucleus of thalamus (ANT) significantly suppresses PTZ-induced epileptiform activity, with concurrent alterations in functional connectivity. FUS reduced hippocampal spike counts by approximately 36%, while rs-fMRI revealed a strong correlation between seizure suppression and connectivity reduction (normalization), particularly in the thalamus-hippocampus circuit, a key network in seizure propagation. Histological analysis further confirmed FUS-induced neuronal modulation. Our findings support FUS as a promising noninvasive approach for epilepsy treatment, expanding beyond previous studies that focused primarily on electrophysiological changes14,15,16. Unlike research that examined seizure suppression in isolation, we show that FUS influences both local neuronal activity and broader brain connectivity. This aligns with emerging evidence that epilepsy involves dynamic brain-wide interactions.
Resting state connectivity of seizure foci with other brain regions is complex, depending upon the type of seizures, local versus global connections, chronicity and frequency band of synchronization27. With focal seizures, resting state connectivity variably tends to be stronger in the region of the seizures focus and weaker distally. Patients with idiopathic generalized epilepsy demonstrate increased EEG functional connectivity in the theta and delta frequency bands and decreased connectivity in the alpha band29. Treatment with the anti-seizure medicine valproic acid partially normalizes connectivity. This observation in patients is consistent with our finding of increased functional connectivity between thalamus and hippocampus (among other regions) after PTZ and partial normalization by FUS. By combining EEG and rs-fMRI, our study provides new insights into the network-level effects of FUS, reinforcing its potential for treating DRE.
Ultrasound therapy design demonstrates variable suppressive effects on generalized seizures. Chen et al. increased the MI to 0.75 and the duty cycle to 30% with a resulting spike inhibition of 88.5%15. However, these parameters significantly elevated superficial cortical temperatures16. Targeting the cerebral cortex with a reduced MI and duty cycle limited spike reduction to 34%26. However, increasing the inter-stimulus interval (ISI) and reducing the duty-cycle can provide cooling time during treatment, with retained spike inhibition30. In this study, the use of low-dose FUS treatment (90-sec ISI) and high-dose (30-sec ISI) exhibited similar spike-suppressing effects. Another strategy would be to employ multiple sessions of FUS to achieve additive benefits20.
This study again supports the ability of FUS to reduce epileptiform activity in a rat model of epilepsy. Our prior studies showed this effect in a model of hippocampal epilepsy produced by kainic acid16,30. Results are here extended to a generalized PTZ model, including recordings from electrodes implanted in hippocampus and ANT, which is the only currently approved target for deep brain stimulation for epilepsy. We used fMRI to serve as a biomarker to indicate the scale and level of epileptiform activity (Supplementary S8). A high correlation exists between EEG spike frequency and functional connectivity, with a dramatic correlation coefficient histogram shift from normal to time of induced spiking. We did not specifically analyze functional connectivity of thalamic nuclei other than the anterior nucleus, but other nuclei are likely relevant to generalized seizures and might also demonstrate changes in connectivity with various brain regions. The centromedian nucleus of thalamus, in particular, has been a neuromodulation target for generalized and highly multifocal seizures31.
In this study, the network connectivity of 36 regions of interest was grouped into eight functional categories for easier quantitative analysis. Systemic PTZ injection led to connectivity changes, with the most significant effects seen in the ANT-hippocampal network within the Circuit of Papez. c-Fos induction, a marker of neuronal activity, also increased after PTZ injection and was partially normalized by thalamic sonication, supporting these findings from a histological perspective. A proposed mechanism underlying the inhibitory effects of FUS is that it selectively suppresses hypersynchronous epileptic activity by mechanically modulating ion channels or synaptic transmission within critical nodes involved in seizure propagation32. This is supported by our fMRI data, which demonstrated restored functional connectivity between the ANT and hippocampus, paralleling clinical observations where thalamic modulation disrupts abnormal cortico-thalamo-cortical networks33. Furthermore, the observed normalization of c-Fos expression within the ANT-hippocampal pathway suggests that FUS preferentially reduces activity in hyperexcitable excitatory neurons, thereby rebalancing overall network excitability13. Additionally, previous studies indicate that FUS can modulate extracellular neurotransmitter concentrations, particularly enhancing inhibitory tone through increased expression of glutamic acid decarboxylase (GAD65), a key enzyme involved in GABA synthesis15,34. Overall, FUS targeting the ANT significantly reduced abnormally heightened connectivity provoked by PTZ, and the reduced connectivity was accompanied by a decrease in epileptiform activity.
Our study has several limitations. The measure of epileptogenicity was EEG spiking, which correlates only approximately with clinical seizures35. Measures had to be taken under general anesthesia, making it unclear whether recordings were interictal, ictal or postictal. In children with focal epilepsy, several studies showed decreased, not increased, functional connectivity, but this depends on brain region36. To preserve the broader effects of functional connectivity related to generalized epileptic activity and FUS intervention, this study did not apply nuisance correction methods37because such methods could obscure biologically meaningful widespread changes and introduce artifactual negative correlations38particularly in PTZ seizure models. However, the absence of confound correction may affect the interpretation of localized neural activity, since abnormal signals from non-neuronal tissue or motion artifacts could distort the true relationship between seizure-related brain regions, complicating the identification of specific circuits involved in epileptic activity. Connectivity among distant brain regions usually is lower in the interictal state and higher during seizures and postictally39. Our data show increased connectivity after PTZ, suggesting being on the ictal spectrum, but this could not be directly documented with anesthetized animals. Servoflurane has potential to influence the functional connectivity in certain brain regions40 and inhibit cortical high-frequency EEG activity and promotes synchronous low-frequency EEG firing, potentially affect the interfering outcome of FUS stimulation. Reduction of spikes and connectivity correlated, but no inference can be made about causality. Despite these limitations, this study supports further pursuit of modulatory FUS as a treatment for epilepsy and suggests that attention to specific network relationships may play a role in possible benefits.
Methods
Animals
The methods were carried out in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals. All animal experiments were approved by the Institutional Animal Care and Use Committee of National Taiwan University, Taiwan (IACUC No. NTU-110-EL-00148). Thirty-two male Sprague-Dawley rats (290–340 g) were purchased from BioLASCO Co., Ltd, in Taiwan and were supported by the Animal Resource Center at National Taiwan University at Taipei. Animals were housed with a 12-h light/dark cycle and ad libitum access to food and water. The housing facility was maintained at 21–24 °C and kept at 40–60% humidity. Among them, 28 received PTZ injections, four received non-PTZ sham injection. All animals were evaluated experimentally with EEG and rs-fMRI monitoring (Fig. 5A). All methods are reported in accordance with ARRIVE guidelines.
(A) Experimental Design of the Study. (B) MR-compatible 16-channel platinum electrodes dimensions. (C) Electrode implanted into the hippocampal CA1 region41and confirmed through MRI T2 structural imaging.
Electrode implantation and pentylenetetrazol (PTZ) injection
All animals were anesthetized with 2% isoflurane mixed with oxygen at 6 L/ min. An MR-compatible electrode42 (with a long shaft (14.9 mm in length) and 16 electrodes (5 μm-thick and 16 μm in radius), Fig. 5B) was inserted into the CA1 region (AP: -9.0 mm, ML: 4.5 mm, DV: 9.0 mm)41 of hippocampus (Fig. 5C). A small polylactic acid window was placed for locating FUS exposure above the anterior nuclei group of thalamus (ANT) (AP: -2.5 mm, ML: 0 mm from bregma). Dental acrylic was paved to fix the electrode and FUS exposure window.
The experimental animals underwent intraperitoneal injection of pentylenetetrazol (PTZ) to induce acute generalized seizures, with injection doses ranging from 40 to 70 mg/kg for optimization (see supplementary S1). To record EEG and rs-fMRI, the animals were anesthetized with air at 8 L/min and 2% sevoflurane, utilized consistently throughout the experiments involving FUS-neuromodulation43 PTZ-induced epilepsy44 or fMRI45. Sevoflurane is believed to enhance epilepsy-specific biomarkers, specifically increasing abnormal activity in epileptic networks46 including the thalamus-hippocampus pathway, which plays a key role in epilepsy propagation. Previous reports indicate that under sevoflurane anesthesia, abnormal epileptiform signals can be detected by EEG across a broad frequency spectrum47,48,49 and can also be translated into meaningful rs-fMRI signals50.
FUS setup and parameters design
A custom focused ultrasound transducer (fundamental frequency = 1 MHz, radius curvature = 16 mm) was attached to a custom-made gel coupler. Burst-tone signals with carrier frequency of 1 MHz were generated from a function generator (AFG-3022, GWInstek, Taiwan), with the RF signals amplified by a radiofrequency power amplifier (210 L, E&I, USA). The acoustic pressure was calibrated by a needle-type hydrophone (HNA-0400, ONDA Corp., Sunnyvale, California, USA) in a free-field filled with deionized/ degassed water. The diameter and length of the − 6 dB dimension of pressure field were 1.5 mm and 4 mm, respectively (Fig. 6A). An ex vivo rat skull was placed between the transducer and hydrophone to acquire the attenuated acoustic pressure.
(A) Ultrasound transducer and custom holder; Measured FUS distributions along the axial planes. (B) External view of the electrode animals and experimental setup. (C) Ultrasound sonication position, targeting ANT, to disrupt propagation of epileptiform activity41. (D) Time course and experimental design of this study among the three experimental groups.
FUS exposure level was set to 0.25 mechanical index (MI). The duty cycle was set to 30% based on previous FUS-epilepsy studies15,16 which was equivalent to FUS exposure intensities (defined as spatial-peak temporal average, ISPTA) of 0.7 W/cm2. This ISPTA was well below the FDA-specified maximum allowable limit for power output into the brain of 0.72 W/cm251, resulting non-thermal effects15,17. Recent studies have shown that incorporating an inter-stimulus interval (ISI) into FUS parameters can further reduce the thermal effect and seizure frequency20,30. In this study, the exposure duration was 600 s with high-dose protocol of 90-sec “on” periods, with 30 s ISI for 5 cycles and low-dose protocol of 30-sec “on” periods, with 90-sec ISI for 5 cycles (ISI = 90). During sonication, ultrasonic gel was carefully filled in the coupled holder to maintain coupling. The sonicating target was set at AP: -2.5 mm, ML: 0 mm, DV: 6.0 mm, covering ANT, in order to interfere with EEG epileptiform signal propagation10,52a 3D-printed ultrasound window (FUS window)16 was placed at the ANT location (AP: -2.5 mm, ML: 0 mm) along with the electrode, and fixed in place with dental cement to ensure that the transducer can correctly emit ultrasound above the ANT and form the focal point at this location, as illustrated in (Fig. 6B,C).
FUS sonication protocol
Figure 6D illustrates the FUS sonication protocol and time course. All animals in the study were anesthetized with 2% sevoflurane for EEG collection. Animals in the Normal group had EEG recorded for 80 min under anesthesia. PTZ-only animals underwent 20 min of EEG recording before receiving PTZ injection, followed by 60 min of EEG recording. Animals in the PTZ-FUS group received 10 min of EEG recording after PTZ injection. FUS exposure with parameters 0.25 MI, 30% duty cycle, ISPTA = 0.3 W/cm2 with low (30s-on-90s-off)/high (90s-on-30s-off) dose cycles was delivered for 10 min, and then EEG was recorded for another 40 min.
MRI T2 image scanning started with shimming of the magnetic field. A baseline was established with two sets of fMRI scans for lasting 20 min. Animals in the Normal group underwent 6 fMRI scans, totaling 60 min. Animals in the PTZ-alone group received PTZ 70 mg/kg by intraperitoneal injection and underwent six sets of fMRI scans. PTZ-FUS animals received one set of fMRI scans following the PTZ injection. After 10 min of FUS stimulation with low/high dose, animals underwent 4 sets of fMRI scans after sonication (40 min in total).
EEG monitoring and analysis
During EEG measurements, animals were anesthetized (sevoflurane, 2%) and then placed inside a Faraday cage to isolate external electrical noise. Intracranial electrical signals from right hippocampus were recorded using MR-compatible electrodes with an RS232 connector. The 4-channel electrophysiological recording system, MP36 (BIOPAC System, California, USA), was employed for data acquisition. Once the EEG signals were received by MP36, the system applied 60 Hz filtering and amplification with a factor of 1000.
For the analysis of spikes, AcqKnowledge 4.2 (BIOPAC System, California, USA) was used to perform spectral filtering on the raw EEG data, selecting delta (0.5–4 Hz) theta (4–8 Hz), alpha (8–13 Hz) and gamma (40–100 Hz) waves for subsequent analysis15,26. Epileptiform interictal spikes were defined as signals with amplitudes exceeding three times the standard deviation of the background activity for a duration of 40 to 60 milliseconds. The positions of spikes were then determined. The number of these defined spikes (spike counts) was then quantified and compared across different treatment groups and frequency bands.
Functional magnetic resonance imaging
Rats were placed in an acrylic holder and positioned in the center of the magnet during FUS sonication and MRI acquisition. MR images were performed using a 7-Tesla magnetic resonance scanner (Clinscan, Bruker, Germany; 7 Tesla) with a custom single-channel coil (Fig. 6B). Rats were secured at the teeth with a bite bar and a pair of ear bars in the head holder. A free breath air pressure sensor (SA Instruments, Inc., New York, NY, USA) was positioned under the abdomen of the animal to monitor respiration and the respiratory rate maintained at 70–80 breaths/min throughout the scanning period. The water temperature of the circulating pad was adjusted to maintain body temperature at 36.5 ℃.
T2-weighting anatomical images were obtained by turbo-spin-echo (TSE) with scanning parameters of TE/TR = 14ms/4000 ms, FOV = 30 × 30 mm2matrix size = 256 × 256, slice thickness = 1 mm, number of average = 2. For functional scans, 300 consecutive volumes with 15 coronal slices were acquired using gradient echo echo-planar-imaging (EPI) with TE/TR = 20 ms/1000 ms, FOV = 30 × 30 mm2matrix size = 64 × 64, and slice thickness = 1 mm. For each rat, a total of 600 consecutive volumes were acquired with a temporal resolution of one second. The fMRI scan was performed at eight different time points, consisting of two 10-min scans before FUS sonication and six 10-min scans after PTZ injection.
A set of anatomical brain regions were created based on one of our rat brain’s T2 image. The selection of region of interest (ROI) was based on the rat brain atlas of Paxinos and Watson53 and the study of Todd et al.54. Supplementary S5 illustrates the 36 seed regions chosen as ROIs. There were 18 bilateral seed regions consisting of left and right primary visual cortex (V1), secondary visual cortex lateral area (V2L), secondary visual cortex medial area (V2M), primary auditory cortex (Au1), hippocampus (Hipp), the thalamus (Thal), the ventral posteromedial thalamic nuclei (VPM/VPL), primary somatosensory cortex trunk region (S1Tr), primary somatosensory cortex barrel field (S1BF), primary somatosensory cortex hind limb region (S1HL), primary somatosensory cortex front limb region (S1FL), secondary somatosensory cortex (S2), primary somatosensory cortex jaw region (S1J), primary motor cortex (M1), insular cortex (Ins), caudate putamen (CPu), retrosplenial cortex granular (RSC), and the cingulate cortex (Cing). Within each anatomically defined area, a smaller ROI was defined and used for fMRI analysis to avoid erroneous results due to boundary mismatches.
fMRI data processing and analysis
The analysis of resting state fMRI can be divided into two parts including data preprocessing and data analysis. Data pre-processing was performed by SPM12 software (https://www.fil.ion.ucl.ac.uk/spm/software/spm12/) including following steps. Image realignment was used to realign a time-series of images to the first image using a six-parameter (rigid body) spatial transformation to remove most movement artifacts in the fMRI time-series55; Co-registration was used to overlay the anatomical and the functional image to a standard image; Slice timing correction was used to correct the signal from different time points to the same time, and fMRI data was obtained with interleaved slice acquisition and adjacent parts of the brain were acquired at different time points within a certain TR; Image smoothing was used with a 0.8 mm kernel to enhance signal SNR. Finally, the data were temporally detrended and bandpass frequency filtered (0.01 ~ 0.08 Hz) by the code from RESTplus V1.21. (http://restfmri.net/forum/RESTplusV1.2).
The time course of the BOLD response was calculated for the ROIs in the hippocampus and thalamus using the amplitude of low-frequency fluctuation (ALFF) analysis, individually processed in RESTplus software. This method has been used to assess neuronal states in epilepsy-related networks, potentially identifying the epileptogenic regions56.
Time course of signals from the 36 defined brain regions (Supplementary S9) were extracted and Pearson’s correlation coefficient used to calculate the correlation between one brain region and every other brain region54. These functional connectivity values can be portrayed in a 36 × 36 correlation coefficients (C.C.) matrix (Supplementary S9) for each rat. Then each C.C. matrix was transformed to z scores by using Fisher’s R to Z transform and averaged across all C.C. matrices in each group. To facilitate the analysis of brain functional connectivity within major epilepsy-related circuits, the selection of brain regions was filtered to seven specific pathways: the Circuit of Papez, Visual Processing Pathway, Default Mode Network, Limbic System Circuit, Thalamocortical Circuit, and Basal Ganglia Circuit. The corresponding brain regions are listed in (Table 1).
Histology
To identify changes in neuronal activity following FUS exposure, c-Fos immunohistochemistry (IHC) was used to analyze expression level changes in brain regions associated during the time of epileptiform activity onset and evaluate the effect focused ultrasound had on neuron excitability among the major brain regions. Rat brains were post-fixed in 10% buffered neutral formalin for 48 h, then cut into a series of coronal blocks and embedded in paraffin. The blocks were serially sectioned at 5 μm and stained with hematoxylin and eosin (H&E) and c-Fos primary antibody (1:500, Abcam, UK). To evaluate the effect of sonication on tissue integrity, histological examinations were conducted on rats in the Normal group (n = 4), PTZ-alone group (n = 4), and PTZ-FUS group (n = 8). The relative changes in c-Fos positive signals triggered by epileptiform activity and the suppressive effects of sonication were analyzed using the QuPath software (v0.5.1)63.
Statistical analysis
Statistical analysis was performed using R Statistical Software (v. 3.6.3) and RStudio (v. 1.2.5042). EEG data and fMRI data were analyzed using one-way ANOVA with REGWQ test post hoc analysis at an alpha criterion of 0.05, with comparison of the PTZ-FUS group to the Normal group and PTZ alone group.
Data availability
No datasets were generated or analysed during the current study.
References
Fisher, R. S. et al. Epileptic seizures and epilepsy: definitions proposed by the international league against epilepsy (ILAE) and the international bureau for epilepsy (IBE). Epilepsia 46, 470–472. https://doi.org/10.1111/j.0013-9580.2005.66104.x (2005).
Behr, C., Goltzene, M. A., Kosmalski, G., Hirsch, E. & Ryvlin, P. Epidemiology of epilepsy. Rev. Neurol. (Paris). 172, 27–36. https://doi.org/10.1016/j.neurol.2015.11.003 (2016).
Fiest, K. M. et al. Prevalence and incidence of epilepsy: A systematic review and meta-analysis of international studies. Neurology 88, 296–303. https://doi.org/10.1212/WNL.0000000000003509 (2017).
Fisher, R. S. et al. Operational classification of seizure types by the international league against epilepsy: position paper of the ILAE commission for classification and terminology. Epilepsia 58, 522–530. https://doi.org/10.1111/epi.13670 (2017).
Ferreira, T. A. Jr., Middlebrooks, E. H., Tzu, W. H., Neto, M. R. & Holanda, V. M. Postmortem dissections of the Papez circuit and nonmotor targets for functional neurosurgery. World Neurosurg. 144, e866–e875. https://doi.org/10.1016/j.wneu.2020.09.088 (2020).
Wong, M. A critical review of mTOR inhibitors and epilepsy: from basic science to clinical trials. Expert Rev. Neurother. 13, 657–669. https://doi.org/10.1586/ern.13.48 (2013).
Jobst, B. C. & Cascino, G. D. Resective epilepsy surgery for drug-resistant focal epilepsy: a review. JAMA 313, 285–293. https://doi.org/10.1001/jama.2014.17426 (2015).
Markert, M. S. & Fisher, R. S. Neuromodulation - Science and practice in epilepsy: vagus nerve stimulation, thalamic deep brain stimulation, and responsive neurostimulation. Expert Rev. Neurother. 19, 17–29. https://doi.org/10.1080/14737175.2019.1554433 (2019).
Dell, K. L., Cook, M. J. & Maturana, M. I. Deep brain stimulation for epilepsy: biomarkers for optimization. Curr. Treat. Options Neurol. 21, 47. https://doi.org/10.1007/s11940-019-0590-1 (2019).
Fisher, R. et al. Electrical stimulation of the anterior nucleus of thalamus for treatment of refractory epilepsy. Epilepsia 51, 899–908. https://doi.org/10.1111/j.1528-1167.2010.02536.x (2010).
Williams, N. R. et al. High-dose spaced theta-burst TMS as a rapid-acting antidepressant in highly refractory depression. Brain 141, e18. https://doi.org/10.1093/brain/awx379 (2018).
Schulz, R., Gerloff, C. & Hummel, F. C. Non-invasive brain stimulation in neurological diseases. Neuropharmacology 64, 579–587. https://doi.org/10.1016/j.neuropharm.2012.05.016 (2013).
Murphy, K. R. et al. A tool for monitoring cell type-specific focused ultrasound neuromodulation and control of chronic epilepsy. Proc. Natl. Acad. Sci. U S A. 119, e2206828119. https://doi.org/10.1073/pnas.2206828119 (2022).
Min, B. K. et al. Focused ultrasound-mediated suppression of chemically-induced acute epileptic EEG activity. BMC Neurosci. 12, 23. https://doi.org/10.1186/1471-2202-12-23 (2011).
Chen, S. G. et al. Transcranial focused ultrasound pulsation suppresses Pentylenetetrazol induced epilepsy in vivo. Brain Stimul. 13, 35–46. https://doi.org/10.1016/j.brs.2019.09.011 (2020).
Chu, P. C., Yu, H. Y., Lee, C. C., Fisher, R. & Liu, H. L. Pulsed-Focused ultrasound provides Long-Term suppression of epileptiform bursts in the Kainic Acid-Induced epilepsy rat model. Neurotherapeutics https://doi.org/10.1007/s13311-022-01250-7 (2022).
Chu, P. C. et al. Pulsed focused ultrasound reduces hippocampal volume loss and improves behavioral performance in the Kainic acid rat model of epilepsy. Neurotherapeutics 20, 502–517. https://doi.org/10.1007/s13311-023-01363-7 (2023).
Hakimova, H. et al. Ultrasound stimulation inhibits recurrent seizures and improves behavioral outcome in an experimental model of mesial Temporal lobe epilepsy. Epilepsy Behav. 49, 26–32. https://doi.org/10.1016/j.yebeh.2015.04.008 (2015).
Lee, C. C. et al. Pilot study of focused ultrasound for drug-resistant epilepsy. Epilepsia https://doi.org/10.1111/epi.17105 (2021).
Bubrick, E. J. et al. Transcranial ultrasound neuromodulation for epilepsy: A pilot safety trial. Brain Stimulation: Basic. Translational Clin. Res. Neuromodulation. 17, 7–9 (2024).
Centeno, M. & Carmichael, D. W. Network connectivity in epilepsy: resting state fMRI and EEG-fMRI contributions. Front. Neurol. 5, 93. https://doi.org/10.3389/fneur.2014.00093 (2014).
Chiang, S., Stern, J. M., Engel, J. Jr., Levin, H. S. & Haneef, Z. Differences in graph theory functional connectivity in left and right Temporal lobe epilepsy. Epilepsy Res. 108, 1770–1781. https://doi.org/10.1016/j.eplepsyres.2014.09.023 (2014).
Chen, L. S., Mitchell, W. G., Horton, E. J. & Snead, O. C. Clinical utility of video-EEG monitoring. Pediatr. Neurol. 12, 220–224. https://doi.org/10.1016/0887-8994(95)00021-7 (1995).
Ives-Deliperi, V. & Butler, J. T. Mechanisms of cognitive impairment in Temporal lobe epilepsy: A systematic review of resting-state functional connectivity studies. Epilepsy Behav. 115, 107686. https://doi.org/10.1016/j.yebeh.2020.107686 (2021).
Courtiol, J., Guye, M., Bartolomei, F., Petkoski, S. & Jirsa, V. K. Dynamical mechanisms of interictal Resting-State functional connectivity in epilepsy. J. Neurosci. 40, 5572–5588. https://doi.org/10.1523/JNEUROSCI.0905-19.2020 (2020).
Kim, T. et al. Modulation of EEG frequency characteristics by low-intensity focused ultrasound stimulation in a pentylenetetrazol-induced epilepsy model. IEEE Access. 9, 59900–59909 (2021).
Tecchio, F. et al. Brain functional connectivity changes after transcranial direct current stimulation in epileptic patients. Front. Neural Circuits. 12, 44 (2018).
Wirsich, J. et al. The relationship between EEG and fMRI connectomes is reproducible across simultaneous EEG-fMRI studies from 1.5 T to 7T. NeuroImage 231, 117864 (2021).
Clemens, B. et al. Valproate treatment normalizes EEG functional connectivity in successfully treated idiopathic generalized epilepsy patients. Epilepsy Res. 108, 1896–1903. https://doi.org/10.1016/j.eplepsyres.2014.09.032 (2014).
Chu, P. C., Yu, H. Y., Fisher, R. S. & Liu, H. L. Neuromodulatory focused ultrasound for epilepsy: are animal models useful?? ACS Chem. Neurosci. 15, 1728–1731. https://doi.org/10.1021/acschemneuro.4c00198 (2024).
Dalic, L. J. et al. DBS of thalamic centromedian nucleus for Lennox-Gastaut syndrome (ESTEL Trial). Ann. Neurol. 91, 253–267. https://doi.org/10.1002/ana.26280 (2022).
Zhang, M. et al. Different modes of Low-Frequency focused Ultrasound-Mediated Attenuation of epilepsy based on the topological theory. Micromachines (Basel). 12. https://doi.org/10.3390/mi12081001 (2021).
Kuhn, T. et al. Transcranial focused ultrasound selectively increases perfusion and modulates functional connectivity of deep brain regions in humans. Front. Neural Circuits. 17, 1120410. https://doi.org/10.3389/fncir.2023.1120410 (2023).
Choi, T. et al. Bidirectional neuronal control of epileptiform activity by repetitive transcranial focused ultrasound stimulations. Adv. Sci. (Weinh). 11, e2302404. https://doi.org/10.1002/advs.202302404 (2024).
Karoly, P. J. et al. Interictal spikes and epileptic seizures: their relationship and underlying rhythmicity. Brain 139, 1066–1078. https://doi.org/10.1093/brain/aww019 (2016).
Feng, X., Piper, R. J., Prentice, F., Clayden, J. D. & Baldeweg, T. Functional brain connectivity in children with focal epilepsy: A systematic review of functional MRI studies. Seizure 117, 164–173. https://doi.org/10.1016/j.seizure.2024.02.021 (2024).
Frassle, S. et al. TAPAS: an Open-Source software package for translational neuromodeling and computational psychiatry. Front. Psychiatry. 12, 680811. https://doi.org/10.3389/fpsyt.2021.680811 (2021).
Murphy, K., Birn, R. M., Handwerker, D. A., Jones, T. B. & Bandettini, P. A. The impact of global signal regression on resting state correlations: are anti-correlated networks introduced? NeuroImage 44, 893–905. https://doi.org/10.1016/j.neuroimage.2008.09.036 (2009).
Rijal, S. et al. Functional connectivity discriminates epileptogenic States and predicts surgical outcome in children with drug resistant epilepsy. Sci. Rep. 13, 9622. https://doi.org/10.1038/s41598-023-36551-0 (2023).
Palanca, B. J. et al. Resting-state functional magnetic resonance imaging correlates of Sevoflurane-induced unconsciousness. Anesthesiology 123, 346–356. https://doi.org/10.1097/ALN.0000000000000731 (2015).
Paxinos, G. & Watson, C. The Rat Brain in Stereotaxic Coordinates: Hard Cover Edition (Elsevier, 2006).
Chen, Y. Y. et al. Design and fabrication of a polyimide-based microelectrode array: application in neural recording and repeatable electrolytic lesion in rat brain. J. Neurosci. Methods. 182, 6–16. https://doi.org/10.1016/j.jneumeth.2009.05.010 (2009).
Lu, G. et al. Transcranial focused ultrasound for noninvasive neuromodulation of the visual cortex. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 68, 21–28. https://doi.org/10.1109/TUFFC.2020.3005670 (2021).
Piwowarczyk, P. et al. Propofol and Sevoflurane anesthesia in early childhood do not influence seizure threshold in adult rats. Int. J. Environ. Res. Public Health. 18, 12367 (2021).
Elbel, G., Kalisch, R., Czisch, M., Hipp, R. & Auer, D. Proc ISMRM 8th Scientific Meeting.
Wada, K. et al. Sevoflurane-based enhancement of phase-amplitude coupling and localization of the epileptogenic zone. Clin. Neurophysiol. 134, 1–8. https://doi.org/10.1016/j.clinph.2021.11.004 (2022).
Dahal, R. et al. Effect of Sevoflurane anesthesia on intraoperative spikes, High-Frequency oscillations, and Phase-Amplitude coupling in MRI-Normal hippocampus. J. Clin. Neurophysiol. 41, 589–596. https://doi.org/10.1097/WNP.0000000000001031 (2024).
Firestone, E. et al. Sevoflurane-induced high-frequency oscillations, effective connectivity and intraoperative classification of epileptic brain areas. Clin. Neurophysiol. 150, 17–30. https://doi.org/10.1016/j.clinph.2023.03.004 (2023).
Watts, A. D., Herrick, I. A., McLachlan, R. S., Craen, R. A. & Gelb, A. W. The effect of Sevoflurane and isoflurane anesthesia on interictal Spike activity among patients with refractory epilepsy. Anesth. Analg. 89, 1275–1281 (1999).
Vedaei, F., Alizadeh, M., Romo, V., Mohamed, F. B. & Wu, C. The effect of general anesthesia on the test-retest reliability of resting-state fMRI metrics and optimization of scan length. Front. Neurosci. 16, 937172. https://doi.org/10.3389/fnins.2022.937172 (2022).
Duck, F. A. Medical and non-medical protection standards for ultrasound and infrasound. Prog Biophys. Mol. Biol. 93, 176–191. https://doi.org/10.1016/j.pbiomolbio.2006.07.008 (2007).
Fisher, R. S. Deep brain stimulation of thalamus for epilepsy. Neurobiol. Dis. 179, 106045. https://doi.org/10.1016/j.nbd.2023.106045 (2023).
Paxinos, G. & Watson, C. The Rat Brain in Stereotaxic Coordinates 5th edn (Elsevier Academic, 2005).
Todd, N. et al. Focused ultrasound induced opening of the blood-brain barrier disrupts inter-hemispheric resting state functional connectivity in the rat brain. NeuroImage 178, 414–422. https://doi.org/10.1016/j.neuroimage.2018.05.063 (2018).
Hoffmann, M., Carpenter, T. A., Williams, G. B. & Sawiak, S. J. A survey of patient motion in disorders of consciousness and optimization of its retrospective correction. Magn. Reson. Imaging. 33, 346–350. https://doi.org/10.1016/j.mri.2014.11.004 (2015).
Morgan, V. L. & Abou-Khalil, B. Investigations of Brain Network Alterations in Epilepsy Using Functional Magnetic Resonance Imaging. Manag. Epilepsy–Res. Results Treat. 85 (2011).
Oikawa, H., Sasaki, M., Tamakawa, Y. & Kamei, A. The circuit of Papez in mesial Temporal sclerosis: MRI. Neuroradiology 43, 205–210. https://doi.org/10.1007/s002340000463 (2001).
Jacobs, J., Dubeau, F., Olivier, A. & Andermann, F. Pathways of seizure propagation from the Temporal to the occipital lobe. Epileptic Disord. 10, 266–270. https://doi.org/10.1684/epd.2008.0217 (2008).
Danielson, N. B., Guo, J. N. & Blumenfeld, H. The default mode network and altered consciousness in epilepsy. Behav. Neurol. 24, 55–65. https://doi.org/10.3233/BEN-2011-0310 (2011).
Cassidy, R. M. & Gale, K. Mediodorsal thalamus plays a critical role in the development of limbic motor seizures. J. Neurosci. 18, 9002–9009. https://doi.org/10.1523/JNEUROSCI.18-21-09002.1998 (1998).
Timofeev, I. et al. in Jasper’s Basic Mechanisms of the Epilepsies (eds J. L. Noebels) (2012).
Vuong, J. & Devergnas, A. The role of the basal ganglia in the control of seizure. J. Neural Transm (Vienna). 125, 531–545. https://doi.org/10.1007/s00702-017-1768-x (2018).
Bankhead, P. et al. QuPath: open source software for digital pathology image analysis. Sci. Rep. 7, 16878. https://doi.org/10.1038/s41598-017-17204-5 (2017).
Acknowledgements
This work was supported by the National Science and Technology Council (grant number 111-2221-E-002 -032 -MY3, 112-2321-B-002-021, and 113-2321-B-002-030), and by the Center for Advanced Computing and Imaging in Biomedicine (CACIB; grant number NTU-112L900703 and NTU-114L900703)”. Dr. Fisher is supported by the James Anderson and Steve Chen Funds for epilepsy research. We thank Prof. You-Yin Chen, PhD, Department of Biomedical Engineering, National Yang Ming Chiao Tung University for the assistance of MR-compatible electrodes. We thank the Animal Resource Center, National Taiwan University, for laboratory provision. We thank 7T animal MRI Core Lab of the Neurobiology and Cognitive Science Center for technical and facility support, and You-Cheng Wang for producing videos.
Author information
Authors and Affiliations
Contributions
P.-C. C., H.-Y. Y., R. S. F., and H.-L. L. conceptualized the study; P.-C. C. and J.-H. C. developed the methodology; C.-S. H. and W.-H. R. validated the results; P.-C. C., C.-S. H., W.-H. R., and Y.-J. J. conducted formal analysis; P.-C. C. and Y.-J. J. carried out the investigation; H.-L. L. provided resources. P.-C. C. handled data curation; P.-C. C. and C.-S. H. wrote the original draft; R. S. F. and H.-L. L. reviewing and editing the manuscript. P.-C. C., C.-S. H., W.-H. R., and Y.-J. J. performed visualization; H.-Y. Y., R. S. F., and H.-L. L. supervised the project; P.-C. C. managed the project administration; H.-L. L. acquired funding.
Corresponding author
Ethics declarations
Competing interests
Hao-Li Liu served as a technical consultant of NaviFUS Corp., Taiwan and currently holds a number of therapeutic ultrasound related patents; Po-Chun Chu concurrently served as a part-time RD scientist of NaviFUS Corp., Taiwan; The other authors have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Material 10
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chu, PC., Ruan, WH., Huang, CS. et al. Focused ultrasound suppresses pentylenetetrazol-induced epileptiform activity in rats and alters connectivity measured by functional MRI. Sci Rep 15, 29551 (2025). https://doi.org/10.1038/s41598-025-15305-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15305-0