Abstract
While there are numerous studies on the association between climate change and poor sleep quality, there are few studies on large population with a validated outcome measure that can portray a various aspects of poor sleep quality. A total of 211,159 participants from Korean Community Health survey 2018 were included to assess the impact of temperature rise on sleep quality. The primary independent variables are temperature average and temperature difference. Temperature average is yearly average temperature of each district, while temperature difference is the difference between yearly average temperature and climate normal derived from 1961 to 1990. The main outcome is overall sleep quality and sleep components measured by the Pittsburgh sleep quality index. Of the participants, 120,166 (81.48%) were dwelling in urban districts. Urban participants were more likely to report poor sleep quality per 1 °C increase in temperature difference (aOR 1.16 95% CI 1.05–1.29), while 1 °C increase in average temperature was not associated with poorer overall sleep quality. The temperature difference was also associated with shorter sleep duration, sleep fragmentation, bad dreams, too cold, cough or snore, and pain during sleep time. The increase in temperature compared to climate normal was associated with higher prevalence of poor sleep quality. More research on the climate change’s long-term impact on sleep quality is needed.
Similar content being viewed by others
Introduction
Sleep is a biological necessity that accounts for approximately one-third of our life. Adequate sleep is important for both mental and metabolic health and helps minimize accidents and injuries caused by fatigue and sleeplessness1. Poor sleep—which is measured by validated methods like polysomnography, simple sleep duration, or sleep time events like snoring—is associated with increased risk of chronic disease, mental health, or even mortality1,2,3,4.
Heat is one of the multidimensional pathways of climate change that leads to increased heat-related illnesses, poor mental health, and poor work capacity5. For instance, higher temperature disrupt insulin activity and may cause an increase in diabetes incidence6 and may negatively affect both blood pressure and cardiovascular health, potentially leading to greater risk of hypertension7. In terms of sleep, a hot sleeping environment can lead to increased core body temperature, which can in turn leads to the disruption of the natural sleep-wake cycle8. This influence of climate change is more pronounced in highly populated urban areas, exacerbating pre-existing urban heat island effect due to urbanization9 and population-weighted impact of global temperature increase is likely to be far higher than the global average5.
Numerous studies on climate change and sleep have pointed out that the increase in ambient temperature leads to sleep disruption. However, many studies were based on small population ranging from a few dozen to a few hundred participants; these may not effectively estimate the impact of the temperature rise due to climate on the general population10,11,12. Few of the large-scale studies, which may represent nationwide or worldwide population, used limited in outcome measurements. Some used subjective sleep reports of participants, which did not use a validated measurement tool13. Others employed mean that can measure limited aspects of sleep quality, such as sleep duration or apnea-hypopnea index (AHI), which may not portray the full extent of climate change’s impact14,15,16.
The Pittsburg Sleep Quality Index (PSQI) is a self-report based assessment tool that evaluates sleep quality over one-month period17. It is comprised of seven components including sleep duration and sleep disturbance that can portray broader, multidimensional impact of climate change on sleep quality. This study explored the impact of the temperature rise due to climate change by using PSQI on nationwide population of Korea.
Methods
We investigated to determine the independent effect of the temperature difference between the yearly average temperature and climate normal on the prevalence of poor sleep quality in nationally representative population of Korea using the cross-sectional data of Korea Community Health Survey-2018 (KCHS-18). KCHS is collects data annually from national representative population of adult Koreans living in 256 administrative districts of Korea18. KCHS changes part of the survey questions periodically, and included Pittsburgh Sleep Quality Index (PSQI) questionnaire for 2018 survey, making KCHS-18 the only nationwide data with validated instrument to measure sleep quality of Korean population.
Of 228,343 KCHS-18 participants, 221,539 Koreans livening in continental Korea mainland were eligible for this study. First, 10,405 participants with missing value for PSQI or potential confounders were removed. A total of 2,581 participants did not respond to PSQI components. Most of the nonresponse or missing values were regarding household income (n = 7,734). In total, 211,134 participants were used for analysis. The response rate was 95.3% (Fig. 1).
Temperature and associated data used for analysis—yearly average temperature, average temperature difference, effective daily sunshine, and normalized difference vegetation index (NDVI)—were measured and analyzed at district level. ERA5 Daily Aggregates from Google Earth Engine were used to estimate annual average temperature for each district. Daily temperatures at the district level were used to calculate the yearly average temperature in 2018. Meteorological data from Korea Meteorological Administration’s 95 Automated Synoptic Observing System (ASOS) was used to extract climate normal temperature, and effective daily sunshine. Yearly average temperature from 1961 to 1990 was used for climate normal temperature. For metropolitan cities, the meteorological data was collected from each ASOS in center. For rural districts, the data was drawn from the closest ASOS. Average temperature difference was calculated by subtracting the climate normal from the yearly average temperature. Visualized 2018 temperature at district level is provided in the supplementary material (Supplementary figure S1, S2) Greenness, measured through NVDI, is known to moderate the impact of temperature on factors such as physical activity, depression, and mortality19,20,21. NDVI measures the vegetation or greenness by calculating the difference between the reflection of infrared and visible light by vegetation20. NDVI ranges between − 1 and 1, with high positive value indicating healthy plant growth in the area, near zero value indicating barren soil, and negative value indicating standing water like lake, ocean, or snow19,20. One of the key reasons of urban heat island effect is the increase in the impervious surface area, which does not allow water to soak into ground, relative to pervious surface area, which allows soaking22. According to a systematic review on urban heat island, NDVI is the most cited indicator in studies on urban heat island effect and land surface temperature23and could be used as a reliable indicator that shows significant negative correlation with urban heat island’s impact24. For this study we used the mean NDVI level at district level between June 2018 and August 2018. NDVI was calculated based on MODIS NDVI data that measures temporal and spatial variations in vegetation activity at 16-day interval with 500 m spatial resolution25. The NDVI zonal mean for each district was calculated using ArcGIS.
Age, sex, socioeconomic status (education level and household income), and health related factors (physical activity, hypertension, diabetes, and depression) were included as potential confounder. Education level was divided into three categories: ≥college, high school, and middle school≥. Household income was divided into three groups at 2 million Korean Won interval. The cutoff for physical activity was at least 30 min of walking for at least five day per week. Hypertension and diabetes status was determined based on the participants’ self-report of doctor’s diagnosis. Patient Health Questionnaire-9 (PHQ-9), a screening test for major depressive disorder, was used to measure depression status26. PHQ-9 score of 10 or more, which represents moderate to severe depressive symptom that require clinical assistance like antidepressant or hospitalization, was used as cutoff27. For regional factors, average yearly temperature, average temperature difference and effective daily sunshine rate were included.
The main outcome of this study is overall sleep quality measured by PSQI collected from each individual who participated in KCHS 2018. PSQI is a self-reported questionnaire that evaluates the sleep quality during the previous month28. The validated Korean version of PSQI was used for this study. The Cronbach’s α was 0.84, showing high internal consistency, and all seven component scores of PSQI showed significant differences between insomniac patients and the healthy control29. The PSQI score of 5 or higher, which indicates poor sleep relative to clinical and laboratory measures was used as cutoff28,30. Sleep disturbance components of PSQI (trouble falling asleep, sleep fragmentation, nocturia, trouble breathing, cough or snore, too cold during sleep, too hot during sleep, bad dreams, and pain) and sleep duration were also analyzed as secondary outcomes. PSQI measures the frequency of sleep disturbance events in four intervals: not during past month, < 1/week, 1–2/week, and ≥ 3/week. To estimate the association between the temperature increase due to climate change and regular occurrence of sleep disturbance event, the frequency of once or twice a week or higher was defined as sleep disturbance event for analysis purposes. Human adults require 7–8 h of sleep2,4. Sleep duration of less than 7 h was defined as insufficient sleep duration for this study.
We used chi-square test and student’s t-test to explore the differences in individual and regional level variables according to district type. Weighted values provided in the KCHS-18 were used to calculate the percentages of each category for categorical variables. To estimate the effects of regional-level and individual-level variables on the prevalence rate of reporting sleep-related problems, we used multilevel analysis with random intercept. Random slopes for temperature variables were tested and found to vary by region, but the final model used random intercept for consistency. Only regional level variables (meteorological variables, and district type) were adjusted for crude models. Adjusted model was adjusted for regional variables and individual variables. The participants were also stratified by district type for analysis. The partition of variance by individual and regional level variables was also calculated with intraclass coefficient based on covariance parameter estimates (Supplementary table S1).
For sensitivity analysis, temperature related variables of 2018 summer (temperature average and temperature difference of July and August 2018) and 2017 (temperature average and temperature difference of 2017) were used to measure potential effect of lagged temperature. Less rigorous frequency cutoff—less than once a week—was used to further test the association between temperature rise due to climate change and the likelihood of sleep disturbance events. Different cutoffs for sleep duration were also use to test the consistency of association. To account for potential interaction between household income and temperature difference, we performed an additional analysis with household income*temperature difference as interaction term.
SAS 9.4 was used (SAS Institute., Cary, NC, USA). The statistical significance level was P-value < 0.05.
Results
Among 211,159 participants, 120,166 (81.5%) lived in urban districts. On average, urban dwellers were younger, attained higher degree of education, have higher household income, and were more likely to participate in physical activity than rural dwellers. The prevalence rate of overall sleep disturbance measured by PSQI were similar between the two district types (Table 1). As for sleep disturbance related events, urban dwellers were more likely to report sleep fragmentation, but were less likely to report in all other sleep disturbance events (Supplementary table S2).
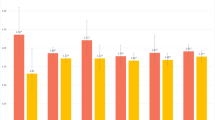
When stratified by district type, urban participants were more likely to report overall poor sleep quality per 1 °C increase in temperature difference. (aOR 1.16 95% CI 1.05–1.29). Increase in temperature average was not associated with overall poor sleep quality for all participants regardless of district type. (Fig. 2, Supplementary table S3). The above associations were consistent when 2018 summer temperature data or 2017 temperature data was used (Supplementary table S4, S5).
The odd ratios of reporting overall poor sleep quality according to district type. *Overall poor sleep quality is defined as pittsburgh sleep quality index score of 5 or higher. Temp avg: per 1 °C increase in 2018 yearly average temperature. Temp diff: per 1 °C increase in 2018 yearly average temperature compared to the climate normal temperature of 1961–1990. Adjusted by age, sex, education, household income, physical activity, hypertension diabetes, sunlight exposure rate, NDVI (normalized difference vegetation index), and district type.
Regarding sleep disturbance event, urban participants were more likely to report sleep fragmentation (aOR 1.17 95% CI 1.03–1.32), cough or snore (aOR 1.21 95% CI 1.01–1.44), too cold during sleep (aOR 1.21 95%CI 1.01–1.44), bad dreams (aOR 1.22 95%CI 1.06–1.39), and pain (aOR 1.25 95% CI 1.08–1.45) as temperature difference increased. The increase in temperature average was only associated with being too hot during sleep (aOR 1.15 95% CI 1.03–1.29). (Fig. 3, Supplementary table S6) In contrast, no significant associations were found between the temperature increase and the most of the sleep disturbance events—for instance in sleep fragmentation (aOR 0.98 95% CI 0.92–1.03) or pain (aOR 1.03 95% CI 0.96–1.10)—except for too hot during sleep (aOR 1.15 95% CI 1.03–1.29). The above association between sleep disturbance events and increase in temperature difference among urban dwellers was mostly consistent when more generous cutoff (sleep disturbance event frequency of less than once a week or higher) was used (Supplementary table S7).
The odds of reporting sleep disturbance related events among urban participants due to climate change’s impact on temperature rise. *The cut-off frequency for sleep disturbance is at least once a week. (A) the odds of reporting sleep disturbance related events among urban participants per 1 °C increase in temp diff. (B) the odds of reporting sleep disturbance related events among urban participants per 1 °C increase in yearly average temperature. Adjusted by age, sex, education, household income, physical activity, hypertension, diabetes, sunlight exposure, and NDVI (normalized difference vegetation index).
When the interaction term between the household income and temperature difference was included in the analysis, a gradient association between the impact of temperature difference on poor sleep quality and household income was found. By point estimate, the urban participants with high household income were 7% more likely to report poor sleep quality per 1 °C temperature difference, and those with middle or low household income were 17% and 23% more likely to report poor sleep quality (high household income: aOR 1.07 95% CI 0.96–1.20; middle household income: aOR 1.17 95% CI 1.05–1.30; low household income: aOR 1.23 95% CI 1.10–1.37). There was no association between the temperature difference’s impact and poor sleep quality among rural participants, regardless of household income level (Supplementary figure S3).
Discussion
This study showed that temperature rise due to climate change is associated with both poor sleep quality as shown by overall PSQI score, and poor sleep quantity as shown through lower sleep duration. A 1 °C rise from climate normal was associated with a 16% increase the likelihood of reporting an overall sleep-related problem among urban dwellers, and a 1 °C rise from climate normal was associated with 10% increase in the odds of reporting a sleep duration of less than 7 h. The population attributable risk of 1 °C rise from climate normal was 5.9% among urban dwelling Koreans; or in other words, 2.49 million urban dwelling Koreans suffered sleep-related problem per 1 °C rise from climate normal. Considering that the global mean temperature have already reached 1.45 °C above the preindustrial baseline 202331, the number of affected urban dwellers will become higher as the climate change worsens over time. The outcome of this study is consistent with general outcomes of previous studies8.
A multinational study on sleep duration revealed that the residents dwelling in hotter region tend to experience more sleep loss than those living in colder region, suggesting people’s limited adaptation to high ambient temperature32. Our study showed that higher average temperature was associated with sleep disturbance due to too high temperature during sleep, but most other sleep disturbance events were associated with increase in temperature from climate normal rather than higher average temperature. Sleep disturbance due to too high temperature during sleep may insinuate the impact of high baseline temperature on sleep while sleep disturbance due to other causes demonstrates the broader impact of temperature rise from climate normal on sleep. Human sleep cycle is deeply connected with thermoregulation, which is controlled by circadian rhythm and sleep regulation. Heat load suppress the decrease in core body temperature, disrupting thermoregulatory system and leading to delayed sleep onset33. Stress due to delayed sleep onset can also increase cortisol level through the activation of hypothalamic-pituitary-adrenal (HPA) axis which further sleep disruption34.
Urban dwellers have been reported to be more vulnerable to the impacts of climate change than rural dwellers5. Temperature in urban areas are reported to be rising more rapidly than the global average5and this rise in mean temperature over climate normal may contributed to higher mortality in urban populations35. Over 80% of the Korean population represented by KCHS lives in urban environments, far higher than the global average of 55%, and this proportion is expected to increase due to urban expansion and rural-urban migration5. Focusing on city level intervention could be an effective way to control climate change-related impact on sleep quality.
It is important to note that the significant association between temperature rises due to climate change and poor sleep quality persisted after controlling for depression. Poor sleep quality and depression have a bi-directional association36,37. It was particularly interesting find that the independent effect of temperature difference from climate normal significantly increased the likelihood of reporting sleep-related problems and shorter sleep duration, while higher average temperature did not have a significant independent effect on the increased odds of reporting poorer sleep quality.
Climate normal of a region likely represents temperature acclimatized by the region’s denizens. A previous study on temperature and sleep demonstrated that the increase in temperature during night caused delayed sleep onset and advanced offset which led to shorter sleep duration38. Ambient temperature higher than acclimatized climate normal, may hamper thermoregulatory mechanisms associated with sleep. Faster body heat dissipation leads to better subjective sleep latency onset39and it is possible that subjective sleep quality is associated with thermoregulatory functions and body temperature rhythms, which are in turn important for both sleep onset and quality40.
Integrating green-blue infrastructures into urban planning may help mitigating the climate change’s impact on the sleep health of the urban dwellers. Green infrastructures like street trees and green roofs can reduce urban air temperature by cooling and improving microclimate41. Permeable pavements, which allows the underlying soil to absorb precipitation and provide evaporative cooling, can also mitigate the heat burden begot by climate change42. All these integrating solutions should also take account for vulnerable population with fewer resources, like air conditioning for social integration of the measures against climate change42.
Limitation
This study has few limitations, coming from its study design and data source. KCHS-18 collects data from the community dwelling population who are available for computer-assisted personal interviews. Koreans with cognitive impairment or who are hospitalized due to illness are not represented in this study. We could not assess the availability of air conditioning or noise pollution status, which may moderate the association between the temperature rise due to climate change and sleep quality. Information on pre-existing sleep-related disorders, like insomnia or obstructive sleep apnea was not available. As the exact time of the survey was not available, we had to use yearly average temperature, rather than daily temperature, to estimate potential impacts of climate change on sleep within previous month of the KCHS. This study used NDVI to substitute urban heat island effect in its analysis. Future studies may consider using long term urban heat island effect to estimate the impact of the temperature rise due to climate change. ASOSs are concentrated in historically populated areas, and the paucity of ASOSs in rural areas, may have limited the accuracy of this study. Still, ASOSs are the best available meteorological data source that provided data as early as 1960s, and KCHS is the only nationwide survey that extracts survey data from every district of Korea collected by trained interviewers. The authors have used the most accurate and valid data available to represent the independent effect of climate change on the entire Korean population.
Strengths
This study utilized a wide range of potential confounders and nationwide population from KCHS database, and this study’s outcome represents the entire population living in contiguous Korea. To the authors’ knowledge, this is one of the first study that explored the potential long-term influence of temperature difference due to climate change on nationwide population, with a validated tool to measure sleep quality. This study also demonstrated that even after adjusting for depressive symptoms, the independent effect of the temperature rise on poor sleep quality remain significant.
Conclusion
This study showed that temperature rise due to climate change deteriorates sleep quality of urban dwellers through sleep disturbance events and a reduction in sleep time, using the best available regional and individual data that represent every district of Korea. Further studies regarding the daily, short-term effect and the yearly, long-term effect of climate change on the various dimensions of sleep is needed to mitigate the climate change’s impact on sleep health.
Data availability
The KCHS data (https://chs.kdca.go.kr/chs/index.do) and meteorological data (https://data.kma.go.kr/data/grnd/selectAsosRltmList.do) that support findings of this study are openly available in websites of respective government agencies.
References
Ramar, K. et al. Sleep is essential to health: an American academy of sleep medicine position statement. J. Clin. Sleep. Med. 17, 2115–2119. https://doi.org/10.5664/jcsm.9476 (2021).
Lu, C., Liao, B., Nie, J., Wang, W. & Wang, Y. The association between sleep duration and chronic diseases: a population-based cross-sectional study. Sleep. Med. 73, 217–222. https://doi.org/10.1016/j.sleep.2020.05.005 (2020).
Scott, A. J., Webb, T. L., Martyn-St James, M., Rowse, G. & Weich, S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep. Med. Rev. 60, 101556. https://doi.org/10.1016/j.smrv.2021.101556 (2021).
Del Brutto, O. H., Mera, R. M., Rumbea, D. A., Sedler, M. J. & Castillo, P. R. Poor sleep quality increases mortality risk: A population-based longitudinal prospective study in community-dwelling middle-aged and older adults. Sleep. Health. 10, 144–148. https://doi.org/10.1016/j.sleh.2023.10.009 (2024).
Romanello, M. et al. The 2023 report of the lancet countdown on health and climate change: the imperative for a health-centred response in a world facing irreversible harms. Lancet 402, 2346–2394. https://doi.org/10.1016/S0140-6736(23)01859-7 (2023).
Natour, S., Damri, O. & Agam, G. The effect of global warming on complex disorders (Mental disorders, primary hypertension, and type 2 Diabetes). Int. J. Environ. Res. Public. Health 19 https://doi.org/10.3390/ijerph19159398 (2022).
Park, S. et al. The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J. Clin. Hypertens. (Greenwich). 22, 438–444. https://doi.org/10.1111/jch.13762 (2020).
Chevance, G. et al. A systematic review of ambient heat and sleep in a warming climate. Sleep. Med. Rev. 75, 101915. https://doi.org/10.1016/j.smrv.2024.101915 (2024).
Yao, X. et al. How can urban parks be planned to mitigate urban heat Island effect in furnace cities ? An accumulation perspective. J. Clean. Prod. 330 https://doi.org/10.1016/j.jclepro.2021.129852 (2022).
Lappharat, S., Taneepanichskul, N., Reutrakul, S. & Chirakalwasan, N. Effects of bedroom environmental conditions on the severity of obstructive sleep apnea. J. Clin. Sleep. Med. 14, 565–573. https://doi.org/10.5664/jcsm.7046 (2018).
Li, W., Bertisch, S. M., Mostofsky, E., Vgontzas, A. & Mittleman, M. A. Associations of daily weather and ambient air pollution with objectively assessed sleep duration and fragmentation: a prospective cohort study. Sleep. Med. 75, 181–187. https://doi.org/10.1016/j.sleep.2020.06.029 (2020).
Mattingly, S. M. et al. The effects of seasons and weather on sleep patterns measured through longitudinal multimodal sensing. NPJ Digit. Med. 4, 76. https://doi.org/10.1038/s41746-021-00435-2 (2021).
An, R. & Yu, H. Impact of ambient fine particulate matter air pollution on health behaviors: a longitudinal study of university students in beijing, China. Public. Health. 159, 107–115. https://doi.org/10.1016/j.puhe.2018.02.007 (2018).
Bai, K. J. et al. Ambient relative humidity-dependent obstructive sleep apnea severity in cold season: A case-control study. Sci. Total Environ. 861, 160586. https://doi.org/10.1016/j.scitotenv.2022.160586 (2023).
Hou, J., Wang, C., Wang, H. & Zhang, P. Effects of temperature on mental health: evidence and mechanisms from China. China Econ. Rev. 79, 101953. https://doi.org/10.1016/j.chieco.2023.101953 (2023).
Mullins, J. T. & White, C. Temperature and mental health: evidence from the spectrum of mental health outcomes. J. Health Econ. 68, 102240. https://doi.org/10.1016/j.jhealeco.2019.102240 (2019).
Zitser, J. et al. Pittsburgh sleep quality index (PSQI) responses are modulated by total sleep time and wake after sleep onset in healthy older adults. PLoS One. 17, e0270095. https://doi.org/10.1371/journal.pone.0270095 (2022).
KCDA. Korea community health survey 2018 at a glance. Korea Disease Control Prev. Agency (2019).
Ho, J. Y. et al. Does surrounding greenness moderate the relationship between apparent temperature and physical activity? Findings from the PHENOTYPE project. Environ. Res. 197, 110992. https://doi.org/10.1016/j.envres.2021.110992 (2021).
Qiu, C., Ji, J. S. & Bell, M. L. Effect modification of greenness on temperature-mortality relationship among older adults: A case-crossover study in China. Environ. Res. 197, 111112. https://doi.org/10.1016/j.envres.2021.111112 (2021).
Song, H. et al. Association between urban greenness and depressive symptoms: evaluation of greenness using various indicators. Int. J. Environ. Res. Public. Health 16 https://doi.org/10.3390/ijerph16020173 (2019).
Rahimi, E., Dong, P. & Jung, C. Global NDVI-LST correlation: Temporal and Spatial patterns from 2000 to 2024. Environments 12 https://doi.org/10.3390/environments12020067 (2025).
Almeida, C. R., d., Teodoro, A. C. & Gonçalves, A. Study of the urban heat Island (UHI) using remote sensing data/techniques: A systematic review. Environments 8 https://doi.org/10.3390/environments8100105 (2021).
Ahmad, B., Najar, M. B. & Ahmad, S. Analysis of LST, NDVI, and UHI patterns for urban climate using Landsat-9 satellite data in Delhi. J. Atmos. Solar Terr. Phys. 265 https://doi.org/10.1016/j.jastp.2024.106359 (2024).
Kamel Didan, A. B. M. & Solano, R. Afredo Huete. MODIS Vegetation Index User’s Guide. Vegetation Index and Phenology Lab (2015).
Kroenke, K., Spitzer, R. L. & Williams, J. B. J. J. o. g. i. m. The PHQ-9: validity of a brief depression severity measure. 16, 606–613 (2001).
Kok, R. M. & Reynolds, C. F. Management of depression in older adults: A review. JAMA 317, 2114–2122. https://doi.org/10.1001/jama.2017.5706 (2017).
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., Kupfer, D. J. & rd, & The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Sohn, S. I., Kim, D. H., Lee, M. Y. & Cho, Y. W. The reliability and validity of the Korean version of the Pittsburgh sleep quality index. Sleep. Breath. 16, 803–812. https://doi.org/10.1007/s11325-011-0579-9 (2012).
Buysse, D. J. et al. Relationships between the Pittsburgh sleep quality index (PSQI), Epworth sleepiness scale (ESS), and clinical/polysomnographic measures in a community sample. J. Clin. Sleep. Med. 4, 563–571 (2008).
Romanello, M. et al. The 2024 report of the lancet countdown on health and climate change: facing record-breaking threats from delayed action. Lancet 404, 1847–1896. https://doi.org/10.1016/S0140-6736(24)01822-1 (2024).
Minor, K., Bjerre-Nielsen, A., Jonasdottir, S. S., Lehmann, S. & Obradovich, N. Rising temperatures erode human sleep globally. One Earth. 5, 534–549. https://doi.org/10.1016/j.oneear.2022.04.008 (2022).
Okamoto-Mizuno, K. & Mizuno, K. Effects of thermal environment on sleep and circadian rhythm. J. Physiol. Anthropol. 31, 14. https://doi.org/10.1186/1880-6805-31-14 (2012).
Aderinto, N. et al. Molecular basis of complex relationships between climate change, sleep disorders, and alzheimer’s disease. Egypt. J. Neurol. Psychiatry Neurosurg. 61 https://doi.org/10.1186/s41983-025-00957-6 (2025).
Bae, S., Lim, Y. H., Oh, J. & Kwon, H. J. Mediation of daily ambient Ozone concentration on association between daily mean temperature and mortality in 7 metropolitan cities of Korea. Environ. Int. 178, 108078. https://doi.org/10.1016/j.envint.2023.108078 (2023).
Fang, H., Tu, S., Sheng, J. & Shao, A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J. Cell. Mol. Med. 23, 2324–2332. https://doi.org/10.1111/jcmm.14170 (2019).
Pandi-Perumal, S. R. et al. Clarifying the role of sleep in depression: A narrative review. Psychiatry Res. 291, 113239. https://doi.org/10.1016/j.psychres.2020.113239 (2020).
Buguet, A., Radomski, M. W., Reis, J. & Spencer, P. S. Heatwaves and human sleep: stress response versus adaptation. J. Neurol. Sci. 454, 120862. https://doi.org/10.1016/j.jns.2023.120862 (2023).
Iijima, R. et al. Subjective sleep onset latency is influenced by sleep structure and body heat loss in human subjects. J. Sleep. Res. e14122 https://doi.org/10.1111/jsr.14122 (2024).
Harding, E. C., Franks, N. P. & Wisden, W. The temperature dependence of sleep. Front. Neurosci. 13, 336. https://doi.org/10.3389/fnins.2019.00336 (2019).
Iungman, T. et al. Cooling cities through urban green infrastructure: a health impact assessment of European cities. Lancet 401, 577–589. https://doi.org/10.1016/S0140-6736(22)02585-5 (2023).
Lin, B. B. et al. Integrating solutions to adapt cities for climate change. Lancet Planet. Health. 5, e479–e486. https://doi.org/10.1016/S2542-5196(21)00135-2 (2021).
Acknowledgements
The environmental health training program, provided by the Environmental Health Centre of the Catholic University of Korea and funded by the Ministry of Environment, Republic of Korea, supported Horim A. Hwang as a trainee (2024). This work was supported by Institute of Information & communications Technology Planning & Evaluation (IITP) under the Artificial Intelligence Convergence Innovation Human Resources Development (IITP-2024-RS-2023-00254177) grant funded by the Korea government (MSIT).
Author information
Authors and Affiliations
Contributions
Horim A Hwang, and Sanghyuk Bae conceptualized the research. Methodology regarding used in the research was discussed and determined primarily by Horim A. Hwang, Whanhee Lee, and Sanghyuk Bae. Regional level data were organized and collected by Jiwoo Park and Hyeon-Joo bae. Horim A. Hwang and Ayoung Kim curated raw data. The first draft of the manuscript were done by Horim A. Hwang. Overall process was supervised by Sanghyuk Bae. All authors reviewed and confirmed the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The Institutional Review Board of the Catholic University of Korea approved this study (approval No. MC24EISI0073) and was conducted in accordance with the declaration of Helsinki. Informed consent was obtained from all participants before their participation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hwang, H.A., Kim, A., Park, J. et al. Association between temperature rise from climate normal and sleep quality. Sci Rep 15, 29655 (2025). https://doi.org/10.1038/s41598-025-15315-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-15315-y