Abstract
Early diagnosis of refractory Mycoplasma pneumoniae pneumonia (RMPP) in children presents significant clinical challenges. Emerging evidence suggests that circ_0054633 may serve as a promising diagnostic biomarker for pulmonary infections. We developed a comprehensive nomogram integrating circ_0054633 expression with clinical features to evaluate its predictive efficacy for early RMPP diagnosis in children. This retrospective study analyzed 244 children with Mycoplasma pneumoniae pneumonia (MPP) admitted to Tianjin Children’s Hospital during 2023. Multivariate analysis identified six independent predictors: elevated circ_0054633 (OR = 6.28, 95% CI: 2.73–14.47), prolonged fever duration (OR = 1.50, 95% CI: 1.24–1.81), hypoxemia (OR = 10.64, 95% CI: 2.75–41.20), extrapulmonary complications (OR = 2.95, 95% CI: 1.17–7.40), elevated IL-6 (OR = 1.02, 95% CI: 1.00-1.03), and atelectasis (OR = 3.16, 95% CI: 1.25-8.00). The nomogram demonstrated excellent discrimination (AUC = 0.920) and calibration. RMPP patients required longer hospitalization (median 9 vs. 7 days, P < 0.001) and more interventions. The circ_0054633-based nomogram, incorporating clinical predictors, exhibits strong predictive value for RMPP in children. Serum circ_0054633 shows promise as a novel diagnostic biomarker for RMPP.
Similar content being viewed by others
Mycoplasma pneumoniae (M. pneumoniae) is one of the major pathogens responsible for community-acquired pneumonia (CAP) in children1,2. In some cases, MPP may progress to RMPP, characterized by the absence of clinical or radiological response to macrolide antibiotics, potentially advancing to severe and complicated pneumonia3.
Pediatric RMPP may lead to severe pulmonary and extrapulmonary complications. Certain sequelae, such as bronchiolitis obliterans, may substantially impair quality of life, cause persistent functional disabilities, or rarely result in mortality. The incidence of RMPP has markedly increased in recent years4 highlighting the critical importance of early identification to halt disease progression and improve prognosis. Current diagnosis of RMPP primarily relies on clinical manifestations and imaging findings. Proposed biomarkers for RMPP prediction—including C-reactive protein (CRP), lactate dehydrogenase (LDH), ferritin(FER), and D-dimer—demonstrate limited predictive value. Individual biomarkers yield area under the receiver operating characteristic curve (AUC) values ranging from 0.7 to 0.85,6. Consequently, single-parameter approaches lack sufficient discriminative accuracy for prognostic prediction, underscoring an urgent need to identify more effective biomarkers and develop advanced predictive models.
Circular RNAs (circRNAs) represent a novel class of long non-coding RNAs (lncRNAs) characterized by a covalently closed continuous loop structure, conferring the absence of 5’−3’ polarity and polyadenylated tails. Accumulating evidence indicates that circRNAs modulate gene expression at both transcriptional and post-transcriptional levels by functioning as microRNA (miRNA) sponges. CircRNAs exhibit distinct differential expression patterns during M. pneumoniae infections and modulate multiple biological processes, serving as indispensable mediators in the initiation and progression of Mycoplasma-related pathologies5. These findings suggest circRNAs may serve as potential biomarkers or therapeutic targets for RMPP. Studies on RMPP pathogenesis indicate its association with aberrant host immune responses triggered by M. pneumoniae infection6. Notably, silencing of circ_0054633 has been demonstrated to attenuate inflammatory responses through suppression of nuclear factor-κB (NF-κB) activation7. While circ_0054633 was previously identified as a biomarker in gestational diabetes mellitus and vascular endothelial dysfunction8,9 emerging evidence suggests serum circ_0054633 levels exhibit superior diagnostic value in children with severe pneumonia complicated by acute respiratory distress syndrome (ARDS)10. Given its established role in pulmonary inflammation and NF-κB pathway modulation, we prioritized circ_0054633 for investigation in pediatric RMPP. However, the functional significance and regulatory mechanisms of circ_0054633 in RMPP remain poorly characterized. This study aims to evaluate the early predictive value of serum circ_0054633 in pediatric RMPP, develop a clinically applicable nomogram integrating circ_0054633 with established biomarkers and clinical features, and ultimately enhance risk-stratification and therapeutic decision-making for RMPP management.
Materials and methods
Study design and participants
This retrospective case-control study analyzed clinical data from 244 children with MPP admitted to Tianjin Children’s Hospital during 2023. All patients had a disease duration of ≤ 7 days at admission. Based on progression to RMPP, participants were stratified into two groups: the RMPP group (47 cases) and the non-refractory MPP (non-RMPP) group (197 cases).
Diagnostic criteria for MPP and RMPP followed the Diagnosis and Treatment Guidelines for Mycoplasma pneumoniae Pneumonia in Children (2023 Edition)3:
MPP diagnosis: (1) Clinical symptoms, signs, or radiological evidence of pneumonia at admission; (2) Evidence of M. pneumoniae infection was as follows: serum M. pneumoniae-IgM ≥ 1:160, or seroconversion (increased antibody titers (≥ 4 folds), or M. pneumoniae-DNA positive on real-time polymerase chain reaction(PCR) using a sputum sample.
RMPP diagnosis: MPP patients with persistent fever, worsening clinical/radiological manifestations, or extrapulmonary complications despite ≥ 7 days of standard macrolide therapy.
Inclusion criteria: Age 2 months to 16 years; RMPP group meeting RMPP diagnostic criteria; non-RMPP group meeting MPP criteria without progression to RMPP; written informed consent from guardians. Exclusion criteria: Respiratory tract malformations; preexisting chronic or congenital diseases; mixed infections; chronic lung disease; history of recurrent respiratory infections; incomplete clinical records.The study protocol was approved by the Ethics Committee of Tianjin Children’s Hospital (Approval No.2022-LXKY-008). Guardians of all participants provided informed consent.
Data collection
Clinical data were extracted from electronic medical records and follow-up assessments, including: Demographics: Age and sex. Clinical features: Peak body temperature, fever duration, hypoxemia (SpO2 < 92%), diminished breath sounds on auscultation, extrapulmonary complications, and plastic bronchitis. Laboratory parameters (within 24 h of admission): circ_0054633 expression, white blood cell count (WBC), neutrophil count (NE), neutrophil-to-lymphocyte ratio (NLR), platelet count (PLT), C-reactive protein (CRP), procalcitonin (PCT), interleukin-6 (IL-6), lactate dehydrogenase (LDH), ferritin (FER), erythrocyte sedimentation rate (ESR), alanine aminotransferase (ALT), creatine kinase-MB (CK-MB), and D-dimer (D-D). Imaging findings: Atelectasis and pleural effusion. Treatment outcomes: Use of glucocorticoids, intravenous immunoglobulin (IVIG), and bronchoscopy; macrolide resistance rate; and length of hospital stay.
Measurement of serum circ_0054633 levels
Fasting peripheral venous blood (3 mL) was collected within 24 hours of admission, clotted at room temperature for 20 minutes, and centrifuged at 3000 rpm for 10 minutes (radius: 15 cm). The supernatant was stored at − 80℃ for subsequent analysis. Total RNA was extracted from serum using TRNzol Universal Reagent (Tiangen Biotech, Cat. DP424), with RNA quality confirmed spectrophotometrically (A260/A280 > 1.8). Reverse transcription was performed using the RevertAid First Strand cDNA Synthesis Kit (Thermo Fisher Scientific, Cat. K1622). qRT-PCR (Quantitative real-time PCR) primers included circ_0054633 (Forward: 5’-ATTTATTTGCTTTCTACACTTTCAGG-3’; Reverse: 5’-GAAGGGGAAGGTTTTGTTTTACT-3’) and the reference gene PGK1 (Forward: 5’-AAAGCCGAGCCAGCCAAAATAG-3’;Reverse: 5’-TCATCAAAAACCCACCAGCCTTC-3’). Reactions (20µL) contained 2µL cDNA, 0.5µL of each primer (10µM), 10µL 2 × SYBR Green Master Mix, 0.4µL ROX Reference Dye II (50×), and 6.6µL nuclease-free water. Amplification on a QuantStudio 5 system (Thermo Fisher Scientific) involved: 95℃ for 30 s (initial denaturation); 40 cycles of 95℃ (5 s) and 60℃ (35 s); and a final melt curve (95℃, 15 s). Relative circ_0054633 expression was normalized to PGK1 and analyzed via the 2−ΔΔCtmethod.
Statistical analysis
SPSS 22.0 statistical software was used for the descriptive analysis of the data. The classification data are presented as percentages (%), and continuous data with a normal distribution are presented as the means ± standard deviations; otherwise, they are presented as median (minimum, maximum). The chi-square test was used for categorical data, and the t test and Mann‒Whitney U test were used for continuous data. The factors with significant differences were included in multivariate logistic regression analysis. The nomogram was constructed using R Studio software (version 4.1.0). Model evaluation incorporated receiver operating characteristic curve (ROC) and calibration plot analyses. P < 0.05 was considered statistically significant.
Results
Demographic, clinical, and radiological characteristics
A total of 244 children with MPP were included, comprising 47 RMPP cases and 197 non-RMPP cases. No significant differences were observed between groups in age (P = 0.39), sex distribution (P = 0.755), or peak temperature (P = 0.28) (Table 1).
Compared with non-RMPP patients, RMPP patients exhibited significantly higher incidences of hypoxemia (23.40% vs. 3.55%, P < 0.001), diminished breath sounds (38.30% vs. 27.92%, P < 0.001), extrapulmonary complications (55.32% vs. 28.43%, P < 0.001), plastic bronchitis (38.30% vs. 10.60%, P < 0.001), pleural effusion (40.43% vs. 20.30%, P < 0.001), and atelectasis (51.06% vs. 26.40%, P < 0.001), along with prolonged fever duration (10.62 ± 2.41 days vs. 8.06 ± 2.67 days, P < 0.001).
circ_0054633 and laboratory biomarkers
Relative to non-RMPP patients, the RMPP group demonstrated significantly elevated levels of circ_0054633 (3.56 ± 0.47 vs. 2.87 ± 0.71, P < 0.001), NLR (2.92 vs. 2.54, P = 0.02), IL-6 (30.05 vs. 22.32 ng/L, P < 0.001), LDH (450.00 vs. 331.00 U/L, P < 0.001), ferritin (195.10 vs. 132.20 µg/L, P < 0.001), and D-dimer (0.37 vs. 0.20 mg/L, P = 0.002), though no significant intergroup differences were observed for WBC, NE, PLT, CRP, PCT, ESR, ALT, or CK-MB(Table 2).
Therapeutic interventions and clinical outcomes
Compared with non-RMPP patients, RMPP patients demonstrated significantly higher utilization rates of glucocorticoids (100% vs. 48.73%, P < 0.001), IVIG (12.77% vs. 0%, P = 0.001), and bronchoscopy (82.98% vs. 36.55%, P < 0.001), along with prolonged hospitalization duration (median 9 days vs. 7 days, P < 0.001). In contrast, macrolide resistance rates showed no significant difference between RMPP and non-RMPP groups (95.74% vs. 91.37%, P = 0.54). All patients in both cohorts achieved clinical improvement or recovery without requiring mechanical ventilation or mortality (Table 3).
Independent risk factors for RMPP
Multivariate logistic regression identified six independent risk factors for RMPP progression: circ_0054633 (OR = 6.28, 95% CI: 2.73–14.47, P < 0.001), fever duration (OR = 1.50, 95% CI: 1.24–1.81, P < 0.001), hypoxemia (OR = 10.64, 95% CI: 2.75–41.20, P = 0.001), extrapulmonary complications (OR = 2.95, 95% CI: 1.17–7.40, P = 0.021), IL-6 (OR = 1.02, 95% CI: 1.00–1.03, P = 0.010), and atelectasis (OR = 3.16, 95% CI: 1.25–8.00, P = 0.015) (Table 4).
Development and validation of the RMPP prediction nomogram
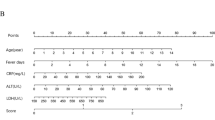
A comprehensive nomogram integrating circ_0054633, fever duration, hypoxemia, extrapulmonary complications, IL-6, and atelectasis was constructed (Fig. 1). The model demonstrated exceptional discriminative capacity, with an area under the ROC curve (AUC) of 0.920 (95% CI: 0.881–0.958, P < 0.001) (Fig. 2). The calibration analysis included 243 patients (one patient excluded due to incomplete data). Calibration analysis confirmed robust agreement between predicted and observed outcomes (Hosmer-Lemeshow test, P = 0.852) (Fig. 3).
Nomogram model for early prediction of refractory Mycoplasma pneumoniae pneumonia. Instructions for using the nomogram: (a) Draw a line perpendicular from each of the six variables to the top line labeled “Points” to obtain the corresponding number of points; (b) add the points obtained from each of the six variables to obtain the total number of points; and (c) draw a line descending from the axis labeled “Total points” until it intercepts the RMPP type. The risk value corresponding to the RMPP type represents the specific risk at which RMPP will occur.
Discussion
RMPP may precipitate severe complications and long-term sequelae. Early diagnosis and timely therapeutic intervention are therefore pivotal for improving clinical outcomes11. Currently, prevalent methodologies for estimating RMPP severity are predicated on clinical characteristics, pulmonary imaging severity, and therapeutic efficacy, which are insufficient for effective identification of early-stage RMPP12,13.Therefore, identification of novel biomarkers and predictive tools for early RMPP diagnosis represents an urgent clinical imperative.
In this investigation, we developed a nomogram integrating circ_0054633 and clinical features, which demonstrated exceptional discriminative accuracy (AUC = 0.920), significantly surpassing the performance of individual biomarkers(AUC: 0.7–0.8)14,15. This model provides a robust framework for early RMPP identification and intervention.
Advances in epigenetics have identified circular RNAs (circRNAs)—stable, covalently closed non-coding RNA molecules-as key regulators of disease pathogenesis16. CircRNAs are implicated in malignancies, cardiovascular disorders, and respiratory diseases17,18[,19 modulating processes such as inflammation, apoptosis, and drug resistance20. Their stability and tissue-specific expression profiles position them as promising diagnostic biomarkers21,22. Notably, differential circRNA expression between RMPP and non-RMPP cases suggests their potential utility in RMPP diagnosis23. Among these, circ_0054633 has emerged as a diagnostic marker across diverse pathological conditions9,22. Our study further identified elevated circ_0054633 as an independent predictor of RMPP progression (OR = 6.28, 95% CI: 2.73–14.47). Mechanistically, circ_0054633 may exacerbate systemic inflammation by activating the NF-κB pathway, thereby promoting the release of pro-inflammatory cytokines (e.g., IL-17 A, TNF-α)7. These molecular pathways are central to MPP pathogenesis and dysregulated immune responses24,2526. While our findings underscore circ_0054633’s predictive value, its role in Mycoplasma pneumoniae-driven inflammation warrants further mechanistic investigation.
IL-6, a pivotal mediator of immune activation, correlates with disease severity in MPP27. Our results align with Zhang et al.28 demonstrating elevated IL-6 levels in RMPP (OR = 1.02, 95% CI: 1.00-1.03) and reinforcing the role of hyperinflammation in RMPP pathogenesis. Although the odds ratio for IL-6 (1.02 per unit increase) appears modest, the clinical impact becomes significant when considering the wide range of observed IL-6 levels (e.g., from 20 to 70 ng/L). Prolonged fever, a hallmark of RMPP, was also independently associated with disease progression (OR = 1.50, 95% CI: 1.24–1.81), consistent with prior studies identifying fever duration > 10 days as a risk factor29,30. Extrapulmonary complications and atelectasis further reflect heightened immune dysregulation and airway obstruction in RMPP, corroborating Bi et al.’s findings31.
Although macrolide resistance and excessive host immune responses are proposed RMPP mechanisms6,32 our study revealed comparable macrolide resistance rates between RMPP and non-RMPP groups. By contrast, RMPP patients required more utilization rates of glucocorticoids (100% vs. 48.73%, P < 0.001) and IVIG (12.77% vs. 0%, P = 0.001), suggesting immune dysregulation-rather than antibiotic resistance-drives RMPP progression. Early immunomodulatory therapy (e.g., glucocorticoids, IVIG) may mitigate lung injury and accelerate recovery33,34 supporting this hypothesis35. However, the precise mechanisms underlying RMPP remain elusive, necessitating further mechanistic studies.
Despite robust performance in development and validation datasets, this study has limitations. First, the single-center design may restrict generalizability to diverse populations. Second, circ_0054633 was measured only in serum; bronchoalveolar lavage fluid (BALF) analysis could provide critical insights into local pulmonary inflammation. Third, while we identified IL-6 as a predictor, other NF-κB-regulated cytokines (e.g., TNF-α, IL-17 A) were not measured, limiting mechanistic interpretation. Fourth, the absence of comparator groups with other respiratory diseases precludes assessment of the model’s specificity for RMPP diagnosis. Future studies should: (1) validate the model in multi-center cohorts, (2) correlate serum and BALF circ_0054633 levels, (3) quantify NF-κB pathway cytokines, and (4) evaluation of biomarker specificity through controlled comparisons with other respiratory pathologies, particularly pneumonia of differing etiologies.
Conclusion
We have developed a nomogram incorporating circ_0054633 and five clinical parameters (fever duration, hypoxemia, extrapulmonary complications, IL-6, and atelectasis) to accurately predict the progression from MPP to RMPP, facilitating early diagnosis and timely therapeutic intervention. This model exhibits high discriminative accuracy (AUC = 0.920) and robust calibration, enabling early identification of high-risk MPP patients. Circ_0054633 may additionally serve as a potential biomarker or therapeutic target for RMPP management.
Data availability
All the data generated or analysed during this study are included in this published article. All analyzed data are available from the corresponding author upon reasonable request.
References
Søndergaard, M. J., Friis, M. B. & Hansen, D. S. & Jørgensen,I.M. Clinical manifestations in infants and children with Mycoplasma pneumoniae infection. PLoS One 13(4), e0195288 (2018).
Liu, W. K. et al. Epidemiology of acute respiratory infections in children in guangzhou:a three-year study. PLoS One. 9 (5), e96674 (2014).
National Health Commission of the People’s Republic of China. Diagnosis and treatment guidelines for Mycoplasma pneumoniae pneumonia in children (2023 Edition). Int. J. Epidemiol. Infect. Dis. 50 (2), 79–85 (2023).
Liu, J. H. et al. Analysis of predictive factors for bronchiolitis obliterans in children with refractory Mycoplasma pneumoniae pneumonia. Chin. J. Pediatr. 61 (4), 317–321 (2023).
Gan, T., Yu, J., He, J. & miRNA LncRNA and circrna: targeted molecules with therapeutic promises in Mycoplasma pneumoniae infection. Arch. Microbiol. 205 (8), 293 (2023).
Wang, K. et al. Transcriptome analysis of Bronchoalveolar lavage fluid from children with Mycoplasma pneumoniae pneumonia reveals natural killer and T cell-proliferation responses. Front. Immunol. 9, 1403 (2018).
Yang, C. L. et al. Quietness of circular RNA circ_0054633 alleviates the inflammation and proliferation in lipopolysaccharides-induced acute lung injury model through NF-κB signaling pathway. Gene 766, 145153 (2021).
Zhao, Z. et al. Hsa_circ_0054633 in peripheral blood can be used as a diagnostic biomarker of pre-diabetes and type 2 diabetes mellitus. Acta Diabetol. 54 (3), 237–245 (2017).
Pan, L. et al. Human circular RNA-0054633 regulates high glucose-induced vascular endothelial cell dysfunction through the microRNA-218/roundabout 1 and microRNA-218/heme oxygenase-1 axes. Int. J. Mol. Med. 42 (1), 597–606 (2018).
Mu, S. Y. et al. Early diagnostic and prognosis prediction of circ_0054633 for acute lung injury/acute respiratory distress syndrome in children with severe pneumonia. Chin. Crit. Care Med. 36 (9), 957–961 (2024).
Zhao, S. Y. et al. Key interpretations of the National health commission’s diagnosis and treatment guidelines for Mycoplasma pneumoniae pneumonia in children (2023 Edition). J. Clin. Pediatr. 41 (3), 224–228 (2023).
Waites, K. B. et al. Mycoplasma pneumoniae from the respiratory tract and beyond. Clin. Microbiol. Rev. 30 (3), 747–809 (2017).
Rogozinski, L. E., Alverson, B. K. & Biondi, E. A. Diagnosis and treatment of Mycoplasma pneumoniae in children. Minerva Pediatr. 69 (2), 156–160 (2017).
Wen, J., Su, Y., Sun, H., Zhang, H. P. & Li, H. The combination of initial markers to predict refractory Mycoplasma pneumoniae pneumonia in Chinese children: a case control study. Respir Res. 22 (1), 89 (2021).
Huang, X. et al. Clinical significance of D-dimer levels in refractory Mycoplasma pneumoniae pneumonia. BMC Infect. Dis. 21 (1), 14 (2021).
Kristensen, L. S. et al. The biogenesis, biology and characterization of circular RNAs. Nat. Rev. Genet. 20 (11), 675–691 (2019).
Zhang, H. D., Jiang, L. H., Sun, D. W., Hou, J. C. & Ji Z.L. CircRNA: a novel type of biomarker for cancer. Breast Cancer. 25 (1), 1–7 (2018).
Altesha, M. A. et al. Circular RNA in cardiovascular disease. J. Cell. Physiol. 234 (5), 5588–5600 (2019).
Jeck, W. R. et al. Circular RNAs are abundant, conserved, and associated with ALU repeats. RNA 19 (2), 141–157 (2013).
Li, X., Yang, L. & Chen, L. L. The biogenesis, functions, and challenges of circular RNAs. Mol. Cell. 71 (3), 428–442 (2018).
Lou, Z. et al. Minor and major circrnas in virus and host genomes. J. Microbiol. 59 (3), 324–331 (2021).
Zhou, H. et al. Microarray and bioinformatics analysis of circular RNA differential expression in newborns with acute respiratory distress syndrome. Front. Pediatr. 9, 728462 (2021).
Huang, F. et al. Ribosomal RNA-depleted RNA sequencing reveals the pathogenesis of refractory Mycoplasma pneumoniae pneumonia in children. Mol. Med. Rep. 24 (5), 761 (2021).
Xu, C. et al. Long Non-Coding RNA PACER regulates Mycoplasma pneumoniae-induced inflammatory response through interaction with NF-κB. Ann. Clin. Lab. Sci. 52 (1), 21–26 (2022).
Yang, M. et al. Interleukin 17A as a good predictor of the severity of Mycoplasma pneumoniae pneumonia in children. Sci. Rep. 7 (1), 12934 (2017).
Li, G. et al. High co–expression of TNF–α and CARDS toxin is a good predictor for refractory Mycoplasma pneumoniae pneumonia. Mol. Med. 25 (1), 38 (2019).
Saghafian-Hedengren, S. et al. Assessment of cytokine and chemokine signatures as potential biomarkers of childhood Community-acquired pneumonia severity: A nested cohort study in India. Pediatr. Infect. Dis. J. 36 (1), 102–108 (2017).
Zhang, Y. et al. The clinical characteristics and predictors of refractory Mycoplasma pneumoniae pneumonia in children. PLoS One. 11 (5), e0156465 (2016).
Gong, H. et al. The risk factors of children acquiring refractory Mycoplasma pneumoniae pneumonia: a meta-analysis. Medicine 100 (11), e24894 (2021).
Qu, B. N. et al. Clinical characteristics and high risk factors of Mycoplasma pneumoniae pneumonia in children. Chin. Pediatr. Integr. Traditi Western Med. 11, 58–62 (2019).
Bi, Y. et al. Development of a scale for early prediction of refractory Mycoplasma pneumoniae pneumonia in hospitalized children. Sci. Rep. 11 (1), 6595 (2021).
Wang, M. et al. Clinical and laboratory profiles of refractory Mycoplasma pneumoniae pneumonia in children. Int. J. Infect. Dis. 29, 18–23 (2014).
Zhang, Y. et al. Cytokines as the good predictors of refractory Mycoplasma pneumoniae pneumonia in school–aged children. Sci. Rep. 6, 37037 (2016).
Youn, Y. S. et al. Early additional immune-modulators for Mycoplasma pneumoniae pneumonia in children: an observation study. Infect. Chemother. 46 (4), 239–247 (2014).
He, Y. S., Yang, M. & Qian, S. Y. Predictive role of cytokines in refractory Mycoplasma pneumoniae pneumonia. Chin. J. Pediatr. 59 (5), 422–425 (2021).
Funding
This work was supported by grants from Tianjin Health Research Project (Grant No.TJWJ2022QN081), Tianjin Municipal Health Commission Key Discipline Special Fund (TJWJ2022XK038), and Tianjin Key Medical Discipline Construction Project (TJYXZDXK-040 A).
Author information
Authors and Affiliations
Contributions
S.M.,J.Z. and Y.Z. wrote the main manuscript text.S.M. and Y.Z. conducted the study design and review of the article.Y.G. and B.H. performed all clinical data analysis and interpretation. J.Z. and Y.Z. conducted supervision and project administration. All authors have read and agreed to the pub lished version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This investigation was conducted in accordance with the Declaration of Helsinki (2013 revision) and received approval from the Institutional Ethics Committee of Tianjin Children’s Hospital (Approval number:2022-LXKY-008).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mu, S., Zhai, J., Guo, Y. et al. Combining circ_0054633 and clinical features to predict refractory Mycoplasma pneumoniae pneumonia in children. Sci Rep 15, 31406 (2025). https://doi.org/10.1038/s41598-025-15333-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15333-w