Abstract
Although breast cancer incidence and mortality are rising globally and China has a screening programme, participation remains low due to poor awareness and financial barriers. This cross-sectional study aimed to assess the knowledge, attitude, and practice (KAP) of breast cancer screening among 964 non-breast cancer women, averaging 29.79 years old, through web-based questionnaires and face-to-face interviews. The knowledge, attitude and practice scores were 7.04 ± 4.19 (possible range: 0–20), 25.37 ± 6.09 (possible range: 10–50), and 15.07 ± 2.84 (possible range: 0–20), respectively. Key barriers included embarrassment (65.45%), fear of radiation (49.48%), and treatment costs (70.34%). Structural equation modeling indicated that income had a direct effect on both knowledge (β = 0.36, P = 0.010) and attitude (β = 1.34, P < 0.001). The logistic regression analysis found that identifying as “housewife” (OR = 2.87, 95%CI: 1.11–7.37, P = 0.029) and having no medical insurance (OR = 3.19, 95%CI: 1.13–9.04, P = 0.028) were significantly associated with unwillingness to undergo breast cancer screening. In conclusion, this study shows that there is a significant gap in KAP regarding breast cancer screening among women in China, particularly among low-income groups. To improve screening rates, it is crucial to address these barriers, enhance knowledge, and provide better risk assessment resources.
Similar content being viewed by others
Introduction
Breast cancer is one of the most predominant cancers, being the leading cause in cancer mortality and disability-adjusted life years among women worldwide1,2. In 2022 there were approximately 2.3 million new cases of breast cancer diagnosed among women worldwide, with about 670,000 deaths attributed to the disease, with the increasing trend suggesting a continued rise in both morbidity and mortality3,4. In response to rising incidence, China launched a free breast cancer screening programme in 2009 for rural women aged 35–64, later expanding to urban women aged 45–74. The programme provides clinical breast examinations, ultrasonography, and/or mammography based on age and local policy. Women are typically invited to participate every two to three years, depending on regional implementation and available resources5,6. Despite all efforts, participation remained low, the rate was approximately 25.7% in 2015, rising to 30.9% by 2018–2019. Meanwhile, the agestandardized incidence of breast cancer increased from 17.1 to 35.6 per 100,000 by 2019, with a notable peak among women aged 40–49 years6. A variety of factors can significantly influence women’s decisions to undergo screening, as high costs, lack of health insurance, or limited access to affordable healthcare services may deter them from seeking preventive care7. Women from low-income backgrounds, particularly those not covered by the programs, may prioritize other financial needs over screening, despite understanding its importance, resulting in delayed diagnosis and poorer health outcomes8,9.
Rapid development of early screening programs should be, therefore, accompanied by identifying vulnerable groups and promoting changes in their help-seeking behaviors, emphasizing that screening is related to health promotion and early diagnosis10. Knowledge, Attitude, and Practice (KAP) study is a structured survey method designed to assess awareness of disease risk factors and warning signs, including those for breast cancer; it evaluates individuals’ understanding and acceptance of cancer risks and can also serve as a tool to promote behavioral changes for better health outcomes11,12. Among numerous recently published KAP studies on breast cancer, reported results differed significantly between countries, ranging from appropriate to poor9,12,13. Several barriers to improving practice were identified, including a busy schedule, excessive optimism without adequate risk awareness, and a lack of knowledge regarding methodologies14,15.
In addition to the absence of awareness, other objective factors may delay detection of breast cancer16. Two recent systemic reviews that included over 90 KAP studies on breast cancer screening up to July 2021 15, 17 reported poor knowledge, negative attitudes, and low practice among respondents. Higher knowledge levels were mainly observed in the countries with improved breast cancer education plans implemented by the government and nongovernmental organizations17. Women in the healthcare profession also reportedly had higher knowledge of breast cancer and breast cancer screening; however, their practice was worse than expected18. Furthermore, although mammography screening appeared to be a cost-effective strategy in high-income countries, the data for low- and middle-income countries is very limited19while the fear of financial burden significantly influences help-seeking and screening behaviours20. Still, many recent articles have discussed educational programs as the only way to encourage regular screening10,15,21. The economic burden of breast cancer screening should be further discussed as one of the obvious barriers to better practice15and more data is needed for Chinese population.
Therefore, this study aimed to evaluate knowledge, attitude, and practice toward breast cancer screening among non-breast cancer women in China. It was hypothesized that in addition to the lack of knowledge, economic factors would influence attitude and practice in the study population.
Methods
Study design and participants
This web-based cross-sectional study was conducted in China between January 2023 and February 2023. The study enrolled women aged over 18 years without a history of breast cancer, who voluntarily agreed to participate. No further restrictions based on age were imposed, and all eligible adults were welcome. Incomplete questionnaires were excluded.
This study was approved by Ethics Committee of North Minzu University, and informed consent was obtained from all study participants before completing the questionnaire.
Procedures
A self-administered questionnaire was developed based on the National Breast Cancer Screening Guidelines for Chinese Women (2022 version)22 and Chinese Guidelines for Breast Cancer Screening and Early Diagnosis23. It was modified based on input from four experts (two in healthcare and two in experimental economics) across two rounds of comments. A small pre-test that involved 50 participants was conducted before the official launch, yielding a Cronbach’s α value of 0.869, which indicated a high internal consistency.
The final questionnaire (supplementary material) was in the Chinese language, and it comprised four following dimensions: (1) demographic information, such as age, residence, and education; (2) the knowledge dimension, consisting of ten questions scored with 2 points for “Well known” 1 point for “Heard of” and 0 points for “Uncertain”; (3) the attitude dimension, consisting of seven questions with ten items, all evaluated using a 5-point Likert scale that ranged from strongly agree (5 points) to strongly disagree (1 point); (4) the practice dimension, consisting of two questions with four items, with Question 2 (P2) being directed to participants who chose “willing” for Question 1 (P1), scored 5 points for willing and 0 points for unwilling.
In order to ensure the accuracy and completeness of the study, four research assistants were trained to explain the purpose of the research and the necessary precautions. Convenience sampling was used for recruitment, and different strategies were employed to reach women of different age groups. Women < 25 years old were recruited primarily through an online form. Participants who could not complete the online questionnaire participated in face-to-face interviews, and the research assistants addressed any questions or issues these participants encountered. The study utilized an online questionnaire constructed using the WeChat-based Wen Juan Xing (WJX) platform (https://www.wjx.cn). Participants accessed and completed the questionnaire by scanning the quick response (QR) code via WeChat. In order to ensure the quality and completeness of the questionnaire results, each IP address could only be submitted once, and all items were mandatory. The research team checked all questionnaires for completeness, internal consistency, and reasonableness.
Statistical analysis
The Stata Statistical Software 17.0 (StataCorp LLC, College Station, TX, USA; version 17.0; available at https://www.stata.com) was used for statistical analysis. Continuous variables were described using mean ± standard deviation (SD) and compared by t-test and one-way ANOVA. Categorical variables were described using frequency (%). Univariate and multivariate linear regression analyses were used for the assessment of factors that independently associated with KAP scores. Univariate and multivariate logistic analyses were carried out to explore independent factors associated with the unwillingness to undergo breast screening. Structural Equation Modeling (SEM) was used to test the following five hypotheses: (1) knowledge directly affects attitude; (2) attitude directly affects practice; (3) knowledge directly affects practice; (4) income directly affects knowledge, attitude, and practice; and (5) insurance directly affects knowledge, attitude, and practice. A two-sided P < 0.05 represented statistical significance.
Results
General characteristics
A total of 968 questionnaires were collected; among these, 964 were valid and were filled out by participants with a mean age of 29.79 ± 9.94 years. The majority of participants resided in urban areas (58.40%), were unmarried (59.85%), and employed (55.91%). Regarding monthly per capita income, 37.97% of respondents reported earning 2000–5000 yuan, while 35.27% reported earning 5000–10,000 yuan. The mean knowledge, attitude and practice scores were 7.04 ± 4.19 (possible range: 0–20), 25.37 ± 6.09 (possible range: 10–50), and 15.07 ± 2.84 (possible range: 0–20), respectively (Table 1).
Characteristics of knowledge, attitude, and practice
In the knowledge dimension, over 50% of participants were unaware about knowledge related to screening modalities (50.21% of respondents, question K4) and carcinoma in situ (55.19% of respondents, question K9). Moreover, low awareness was also noted for the following key topics: the lower accuracy of mammography in dense breasts common among Asian women (K5, 54.98% not aware), the independence of breast US from breast density (K6, 61.51% not aware), and the advantages of US as a non-invasive, low-cost screening method and potential alternative to mammography for dense breasts (K7, 50.31% not aware) (Table 2). In respondents who were older than 40 years knowledge scores were significantly lower compared to younger participants (P = 0.015). Older respondents also had significantly lower correctness rate answering questions K6, K7 and K9 than their younger counterparts (Supplementary Table 1).
In the attitude dimension, 37.34% agreed, and 28.11% strongly agreed that it is embarrassing to expose oneself to the doctor for breast examination. Half of the participants expressed worry that radiation exposure during the screening might be harmful.
In the practice dimension, only 3.84% of non-breast cancer women were unwilling to undergo the screening; 30.53% were more willing to undergo mammography than other options, while 44.66% were more willing to choose MRI screening (Table 3). Although Practice scores did not differ in older participants, significantly more respondents older than 40 years were willing to undergo breast US examination compared to those younger than 40 (Supplementary Table 2).
The answers to knowledge/attitude questions were compared between the participants who indicated being unwilling to undergo the screening (n = 37) and all others, as shown in Supplementary Tables 3 and 4. In addition to the significantly lower scores for general knowledge (questions K1-3), some specific barriers to screening were uncovered, such as beliefs that mammography is inherently radioactive and can cause pain and discomfort (K8). At the same time, no significant differences were found in the attitude dimension (all P > 0.05), except for the examination costs (P = 0.049).
Factors influencing KAP score and willingness to undergo cancer screening
The linear regression analysis (Table 4) revealed that residence other than rural (urban, coefficient: 1.26, 95%CI: 0.08–2.44, P = 0.035; suburban, coefficient: 2.81, 95%CI: 0.79–4.83, P = 0.006), higher monthly income (5000–10000 CNY, coefficient: 2.27, 95%CI: 0.20–4.34, P = 0.031; 10000–20000 CNY, coefficient: 3.57, 95%CI:1.20–5.95, P = 0.003; >20000 CNY, coefficient: 3.54, 95%CI:0.47,6.61, P = 0.024) and having both social and commercial medical insurance (coefficient: 2.22, 95%CI:0.94–3.51, P < 0.001) were independent predictors of higher KAP scores. At the same time, staying at home (e.g., identifying as “housewife”) was independently associated with lower KAP scores (coefficient: −2.3, 95%CI: −4.4–0.3, P = 0.023).
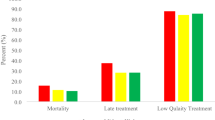
The SEM analysis was performed to further assess the relationship between KAP scores and demographic characteristics of participants, showing that income had a direct effect on both knowledge (β = 0.36, P = 0.010) and attitude (β = 1.34, P < 0.001). Furthermore, insurance had a direct effect on attitude (β = 0.69, P = 0.001), and knowledge had a direct effect on practice (β = 0.08, P < 0.001) (Fig. 1). In the subgroup of women over 40 years old, education (β = 0.69, P = 0.003) and worry about treatment costs (β = 4.10, P < 0.001) had the most significant effect on practice (Fig. 2).
Additionally, logistic regression analysis was utilized in participants willing and unwilling to screen (Supplementary Table 5). It was found that identifying as “housewife” (OR = 2.87, 95%CI: 1.11–7.37, P = 0.029) and having no medical insurance (OR = 3.19, 95%CI: 1.13–9.04, P = 0.028) were significantly associated with unwillingness to undergo breast cancer screening.
Discussion
The present study found a lack of awareness concerning breast cancer screening among non-breast cancer women in China and identified several barriers to screening, including embarrassment, fear of radiation, and concerns about treatment costs, as well as some factors associated with unwillingness to undergo screening, such as identifying as “housewife” and having no medical insurance. To the best of our knowledge, this is the first study on KAP towards breast cancer screening in China that proposed a detailed discussion of economic burden. Our results differ from those reported in other populations and might be used to discuss and plan regional-specific policy changes or interventions, while data obtained on breast cancer screening might be helpful to reform policies, enhance screening rates, and promote early detection. Reducing economic and psychological barriers to breast cancer screening by expanding insurance reimbursement policies, conducting targeted public education campaigns, and offering communication and empathy training for healthcare providers may help improve participation rates and ultimately reduce the burden of breast cancer in China.
The majority of previously published studies have discussed the low rates of women undergoing breast cancer screening; however, some reported sufficient knowledge about breast cancer among respondents10,16. Recent KAP study conducted among women at high risk of breast cancer in China reports insufficient knowledge24while most recent meta-analysis pointed out lower awareness levels among Chinese and Asian women compared to women from other countries25. In line with above, the population of non-breast cancer women in this study that consisted of female Chinese nationals with a mean age of 29.79 ± 9.94 years, demonstrated poor knowledge regarding breast cancer diagnostic/screening methods. Although participants were primarily young women, the mean age in this study was slightly higher than average for this kind of KAP evaluation, mostly involving university students12,13,26. Part of this study population also included undergraduate students, but more than half of the respondents (55.91%) were employed, potentially covering a wider population. Additionally, the incidence of breast cancer increases with age, and this study explored specific perceptions among women over 40 in comparison to younger women, highlighting differences in awareness, attitudes, and practices related to breast cancer screening, providing valuable insights into how age influences perceptions of risk and screening behaviors. These differences may reflect the increasing integration of newer concepts, such as breast density and overdiagnosis, into recent health communication efforts, which younger women may encounter more frequently through digital platforms or recent education27. In contrast, older women may have had fewer opportunities to access or update such knowledge28. Future research should explore how different age groups access and interpret breast cancer screening information, and whether tailored communication strategies can help bridge these knowledge gaps.
One-third of the respondents lived in rural areas, which was associated with lower KAP scores in previous studies11,15. Likewise, in the current study urban or suburban residence was independently linked to better KAP scores. However, it is important to note that knowledge about certain issues was equally poor among urban, suburban, and rural residents. Notably, more than 50.0% of respondents were unaware that Asian ancestry is related to a higher density of breast tissue, potentially impacting the sensitivity and accuracy of mammography29. In contrast, women aged over 40 showed even lower awareness about ultrasound and breast density but were more willing to consider US as a screening option, partly due to its lower cost. The US has been recently suggested as a feasible alternative to mammography for breast cancer screening, especially for women with dense breasts30a topic that requires further discussion since most women are unaware of it. Finally, more than half of participants expressed concern that the radiation would cause them harm during the screening; participants unwilling to undergo screening (n = 37) more often expressed the belief that mammography is inherently radioactive and painful. This may stem, in part, from general health education campaigns that emphasize the importance of protecting oneself from excessive or unnecessary radiation, which, while well-intentioned, may contribute to public apprehension even in the context of low-dose diagnostic procedures such as mammography31. According to the recent comprehensive benefit to risk analysis32the radiation dose and associated risk for a single examination is dependent upon breast density; however, with 65 induced cancers and 8 deaths per 100,000 women over a screening lifetime, this results in 62:1 ratio of lives saved to deaths from induced cancer. Since identifying the best breast cancer screening technique will undoubtedly improve cancer management, gaps detected in the knowledge dimension should be considered during future educational interventions.
Previous studies used logistic regression analysis, finding that lack of awareness regarding mammograms was significantly associated with age and profession, years of experience, geographic region, and personal history of breast cancer33,34,35. Education also influenced breast cancer screening practice21,33. Abeje et al.21 discussed economic factors in their study, where women with a high level of income were about 3 times more likely to be aware of breast cancer screening methods, while Alenezi et al. identified low income as one of the factors associated with the low uptake of mammogram screening programs in33. Begum et al.35 and de Oliveira et al.11 reported expenditure concerns as the leading cause for not seeking medical advice for the prevention of breast cancer. In the present study, higher income was associated with better KAP scores, while the influence of knowledge on attitude and practice was notably less strong. Moreover, identifying as “housewife” and having no medical insurance were significantly associated with unwillingness to undergo breast cancer screening, outlining the most vulnerable participants. It may at least partly explain the lack of obvious progress in awareness regarding breast cancer over time, reported by recent cumulative meta-analysis, despite ongoing educational efforts25. Present study demonstrated that residence and monthly income were predictors of higher KAP scores. Worry regarding treatment costs upon detection of breast cancer on screening was identified as one of the new economic barriers, which is comparable to the worry about the cost of screening itself; moreover, in the subgroup of women aged over 40 years old this concern affected practice scores even more significantly. These findings complement a previously published systematic review of English-language KAP studies, which identified one key reason for avoiding regular screening as an overly optimistic belief in personal health and low perceived risk of breast cancer15and suggest that in Chinese women educational interventions focusing on the risk of the disease might not be enough to promote timely breast cancer screening. Moreover, our findings suggest that women in different age groups may face unique challenges and concerns, which should be taken into account when designing future efforts to promote early detection and improve screening participation.
Although health education might not be enough to overcome the economic burden of breast cancer screening, some steps in this direction were proven to be effective. Specifically, educational model-based interventions (Health belief model, Health Promotion Model) have been shown to promote self-care and create a foundation for improving breast cancer screening behavior36. Empowering women in the healthcare profession also positively impact the attitudes and beliefs of female patients in the hospital and the general public18. Finally, in the present study, only 30.53% of respondents have chosen mammography compared to other options, while 53.29% were more willing to undergo US screening. Based on that, the introduction of US screening as the less expensive alternative might ease some worries regarding the screening cost, as well as the widespread fear of radiation exposure during mammography. Thus, future policies should focus on accessibility (such as introducing US), financial support, and awareness. For instance, culturally tailored media campaigns using social media and community health workers could address misconceptions and promote awareness37. Incorporating modules on empathetic communication and patient counseling into continuing education for healthcare professionals may foster more supportive screening environments and reduce anxiety among participants38. Additionally, employer and community-based initiatives, along with a national screening registry, can help track progress and refine policies for better long-term outcomes39.
Study limitations
The present study has several limitations. First, the study was conducted in China, which may limit the generalizability of the results to other countries and cultures. Moreover, the governmental breast cancer screening program in China is directed at women older than 45 6, so the discussed economic burden may not apply to countries where breast cancer screening is free of cost for all ages. Meanwhile, although formal screening in China begins at age 45, younger women were included because risk-stratified guidelines permit earlier screening, incidence is rising in this group, and they face economic barriers to accessing care. Characterizing their profiles thus informs future programme expansion and equitable screening strategies. Although the inclusion of respondents younger than 45 may have introduced a degree of generalisation bias, participants were not restricted by age, which allowed to capture a wider range of perspectives across age groups. Additionally, while age-related differences in knowledge were observed, the study did not assess participants’ prior exposure to breast cancer-related information, such as via traditional media or digital platforms, which may have contributed to these differences. Secondly, using a self-administered questionnaire may have introduced response bias, which could affect the accuracy of the results. Selection bias also could not be completely excluded, as participants who volunteer for KAP studies might differ systematically from the general population in terms of knowledge, lifestyle, or other factors. Future studies with broader and more diverse participant groups are necessary to confirm and expand upon our findings. Finally, it was not possible to check whether or not respondents who answered positively would undergo timely screening; better results might be explained by social bias40 when respondents gave the answer that was expected according to the nature of the study. As we did not assess the impact of interventions aimed at increasing breast cancer screening rates, whether the proposed targeted efforts would be effective should be further investigated in the future.
There is a strong need to improve knowledge, attitude, and practice towards breast cancer screening among women in China; barriers such as lack of knowledge regarding the methodology and inadequate risk assessment should be addressed, especially among women from rural areas and with low monthly income. Breast cancer screening in China should be improved by focusing on identified barriers through educational initiatives and awareness campaigns that could help to promote screening and address concerns while promoting private and comfortable examination facilities and respectful care. Policy changes or interventions, such as subsidies or insurance coverage, may help address treatment cost-related issues.
Data availability
The data set supporting the results of this article is included within the article.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263 (2024).
Sathishkumar, K., Chaturvedi, M., Das, P., Stephen, S. & Mathur, P. Cancer incidence estimates for 2022 & projection for 2025: result from National cancer registry programme, India. Indian J. Med. Res. 156, 598–607 (2022).
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 74, 12–49 (2024).
Cardoso, M. J., Poortmans, P., Senkus, E., Gentilini, O. D. & Houssami, N. Breast cancer highlights from 2023: knowledge to guide practice and future research. Breast 74, 103674 (2024).
Alpeza, F. et al. Scoping review of primary breast cancer risk reduction strategies in East and Southeast Asia. Cancers (Basel) 17(2), 168 (2025).
Pace, L. E. Risk-Based approaches to breast cancer screening in China. JAMA Netw. Open. 5, e2241448–e2241448 (2022).
Xia, C. et al. Cancer screening in china: a steep road from evidence to implementation. Lancet Public. Health. 8, e996–e1005 (2023).
Castaldi, M., Smiley, A., Kechejian, K., Butler, J. & Latifi, R. Disparate access to breast cancer screening and treatment. BMC Womens Health. 22, 249 (2022).
Srinath, A., van Merode, F., Rao, S. V. & Pavlova, M. Barriers to cervical cancer and breast cancer screening uptake in low- and middle-income countries: a systematic review. Health Policy Plan. 38, 509–527 (2023).
Rakhshani, T., Dada, M., Kashfi, S. M., Kamyab, A. & Jeihooni, A. K. The Effect of Educational Intervention on Knowledge, Attitude, and Practice of Women towards Breast Cancer Screening. Int J Breast Cancer. 5697739 (2022).
de Oliveira, R. D. P., Santos, M. C. L., Moreira, C. B. & Fernandes, A. F. C. Detection of breast cancer: knowledge, attitude, and practice of family health strategy women. J. Cancer Educ. 33, 1082–1087 (2018).
Terui-Kohbata, H., Egawa, M., Yura, K. & Yoshida, M. Knowledge and attitude of hereditary breast cancer among Japanese university female students. J. Hum. Genet. 65, 591–599 (2020).
Rahman, S. A. et al. Awareness about breast cancer and breast Self-Examination among female students at the university of sharjah: A Cross-Sectional study. Asian Pac. J. Cancer Prev. 20, 1901–1908 (2019).
Alsalamh, R. et al. Barriers to breast cancer screening in Saudi arabia: A systematic review and Meta-Analysis. Cureus 16, e65103 (2024).
Meshkani, Z. et al. Systematic review of women’s knowledge, attitude, and practice towards breast cancer. J. Educ. Health Promot. 11, 171 (2022).
Pal, A. et al. Knowledge, attitude, and practice towards breast cancer and its screening among women in india: A systematic review. J. Cancer Res. Ther. 17, 1314–1321 (2021).
Banegas, M. P. et al. Fau - Thompson, B.& Thompson, B. Breast cancer knowledge, attitudes, and early detection practices in United States-Mexico border Latinas.
Heena, H. et al. Knowledge, attitudes, and practices related to breast cancer screening among female health care professionals: a cross sectional study. BMC Womens Health. 19, 122 (2019).
Icanervilia, A. V. et al. Economic evaluations of mammography to screen for breast cancer in low- and middle-income countries: A systematic review. J. Glob Health. 12, 04048 (2022).
Ng, C. W. Q., Lim, J. N. W., Liu, J. & Hartman, M. Presentation of breast cancer, help seeking behaviour and experience of patients in their cancer journey in singapore: a qualitative study. BMC Cancer. 20, 1080 (2020).
Abeje, S., Seme, A. & Tibelt, A. Factors associated with breast cancer screening awareness and practices of women in addis ababa, Ethiopia. BMC Womens Health. 19, 4 (2019).
Health Commission Of The People’s Republic Of China, N. National guidelines for diagnosis and treatment of breast cancer 2022 in China (English version). Chin. J. Cancer Res. 34, 151–175 (2022).
Huang, Y. et al. Interpretation of breast cancer screening guideline for Chinese women. Cancer Biol. Med. 16, 825–835 (2019).
Lu, J. et al. Knowledge, attitude, and willingness toward breast magnetic resonance imaging screening among women at high risk of breast cancer in beijing, China. BMC Public. Health. 24, 2909 (2024).
Wang, Y. J. et al. Worldwide review with meta-analysis of women’s awareness about breast cancer. Patient Educ. Couns. 105, 1818–1827 (2022).
Abo Al-Shiekh, S. S., Ibrahim, M. A. & Alajerami, Y. S. Breast Cancer Knowledge and Practice of Breast Self-Examination among Female University Students, Gaza. ScientificWorldJournal. 6640324 (2021).
Kressin, N. R., Battaglia, T. A., Wormwood, J. B., Slanetz, P. J. & Gunn, C. M. Dense breast notification laws’ association with outcomes in the US population: A Cross-Sectional study. J. Am. Coll. Radiol. 18, 685–695 (2021).
Smith, J. et al. Randomized trial of information for older women about cessation of breast cancer screening invitations. J. Gen. Intern. Med. 39, 1332–1341 (2024).
Sung, H. et al. Breast cancer risk factors and mammographic density among high-risk women in urban China. NPJ Breast Cancer. 4, 3 (2018).
Aristokli, N., Polycarpou, I., Themistocleous, S. C., Sophocleous, D. & Mamais, I. Comparison of the diagnostic performance of magnetic resonance imaging (MRI), ultrasound and mammography for detection of breast cancer based on tumor type, breast density and patient’s history: A review. Radiography (Lond). 28, 848–856 (2022).
Ivanova, A. & Kvalem, I. L. Psychological predictors of intention and avoidance of attending organized mammography screening in norway: applying the extended parallel process model. BMC Womens Health. 21, 67 (2021).
Hooshmand, S., Reed, W. M., Suleiman, M. E. & Brennan, P. C. A review of screening mammography: the benefits and radiation risks put into perspective. J. Med. Imaging Radiat. Sci. 53, 147–158 (2022).
Alenezi, A. M. et al. Female healthcare workers’ knowledge, attitude towards breast cancer, and perceived barriers towards mammogram screening: A multicenter study in North Saudi Arabia. Curr. Oncol. 29, 4300–4314 (2022).
Ayoub, N. M. et al.,. Knowledge and Practice of Breast Cancer Screening Methods among Female Community Pharmacists in Jordan: A Cross-Sectional Study. Int J Breast Cancer. 9292768 (2021). (2021).
Begum, S. A. et al. Knowledge, attitude and practice of Bangladeshi women towards breast cancer: A cross sectional study. Mymensingh Med. J. 28, 96–104 (2019).
Saei Ghare Naz, M., Simbar, M., Rashidi Fakari, F. & Ghasemi, V. Effects of Model-Based interventions on breast cancer screening behavior of women: a systematic review. Asian Pac. J. Cancer Prev. 19, 2031–2041 (2018).
Nayyar, S. et al. From awareness to action: A review of efforts to reduce disparities in breast cancer screening. Cureus 15, e40674 (2023).
Broadbridge, E. et al. Facilitating psychological adjustment for breast cancer patients through empathic communication and uncertainty reduction. Patient Educ. Couns. 114, 107791 (2023).
Riganti, P. et al. Shared decision-making for supporting women’s decisions about breast cancer screening. Cochrane Database Syst. Rev. 5, Cd013822 (2024).
Patel, P. K. A. P. & Survey Does it really measure knowledge, attitudes and practices?? Natl. J. Community Med. 13, 271–273 (2022).
Acknowledgements
Not applicable.
Funding
This work was supported by Fundamental Research Funds for the Central Universities, North Minzu University(Grant Number: 2025ZLGTTYS40); Fundamental Research Funds for the Central Universities, North Minzu University (Grant Number: 2025XYSJJ02); Ningxia Philosophy and Social Science Planning Project (Grant Number: 24NXBYJ04). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Yan Zhou carried out the studies, collected data, and drafted the manuscript, performed the statistical analysis and participated in its design, read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by Ethics Committee of North Minzu University, and informed consent was obtained from all study participants before completing the questionnaire. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, Y. Knowledge, attitude, and practice among non-breast cancer women towards breast cancer screening with a focus on economic factors. Sci Rep 15, 29854 (2025). https://doi.org/10.1038/s41598-025-15478-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15478-8