Abstract
Renal parenchyma thickness and hydronephrosis degree may predict stone-free rate (SFR) after lithotripsy. This study combined these factors and introduced a new index, the ratio of renal parenchymal volume to renal volume (RPRV) to investigate its prediction role of SFR after retrograde intrarenal surgery (RIRS). We collected data from 119 adult patients with upper ureteral or kidney stones who underwent RIRS from March to September 2023. They were divided into stone-free group (n = 85, 71.43%) and residual stone group. Multivariate logistic regression analyzed the relationship between RPRV and SFR. ROC curve analyzed the predictive efficacy of RPRV. Among the 119 patients, there was a difference in RPRV between the two group (P = 0.002). In overall sample, AUC of RPRV for predicting SFR after RIRS is 0.678 (cut-off value: 0.6890, sensitivity: 95.3%; specificity: 41.2%; P = 0.002). In the 2–2.9 cm group multivariate logistic regression analysis is statistically significant (OR 0.847, 95% CI 0.761–0.942, P = 0.002), with an AUC of 0.769 (cut-off value: 0.6887; sensitivity: 97.8%; specificity: 58.8%; P = 0.001). In the 3–4 cm stone group, no significant difference. RPRV is effective in predicting SFR after RIRS and has clinical guiding significance.
Similar content being viewed by others
Introduction
Urolithiasis is a prominent concern in urology, ranking third in terms of illness prevalence. The global incidence rate is 1%-20%, but in Asia it varies from 5 to 19.1%1,2,3,4. In recent years, the incidence rate has shown a continuous upward trend1,5.
With the progress of medical technology, lithotripsy is becoming less intrusive6. For renal calculus larger than 2.0 cm, the EAU guidelines recommend percutaneous nephrolithotomy (PCNL) as the primary option3. In recent years, the application of retrograde intrarenal surgery (RIRS) has increased significantly5, RIRS is not only the first choice for treating intrarenal stones < 2.0 cm, but it can also be employed when PCNL is not available3,7. However, with the popularization of minimally invasive surgeries and the expansion of the indications of RIRS, the problem of postoperative residual stone also follows closely, which can cause recurrence of calculus, urinary infection, urinary tract obstruction, and renal function impairment8,9.
The stone-free rate (SFR) after surgery is an indicator to evaluate the effect of stone clearance after surgery, which is usually determined by CT and KUB7. Stone size, location and number, stone hardness, stone type, patient’s gender, BMI, and the anatomy of the urinary tract, skin-to-stone distance, renal function, etc. are all influencing factors of the stone clearance rate10,11,12,13,14,15,16.
Patients with kidney stones usually accompany with hydronephrosis. After the renal parenchyma of the patient is compressed, the thickness of the cortex will become thinner. Some studies have found that the thickness of the renal parenchyma is related to the SFR and also possesses a certain predictive value17,18,19, but due to individual differences, especially for patients with hydronephrosis, it cannot reflect the relative thickness of renal parenchyma. Hence, this research introduces a new index, the ratio of renal parenchymal volume to renal volume (RPRV) of the affected kidney, with the goal of investigating its link with SFR after RIRS and its prediction role for SFR after RIRS in stones with a diameter of 2–4 cm.
Methods
Patients and study design
This study retrospectively investigated 119 urinary calculus patients who underwent holmium laser lithotripsy through RIRS in the Urology Department of the Fifth Affiliated Hospital of Guangzhou Medical University from March to September 2023. According to the postoperative stone clearance situation, all the patients were divided into a stone-free group and residual stone group, and the age, gender, BMI, stone information, preoperative data of the two groups were recorded. All patients gave informed consent to this study. This study was approved by the institutional committee review (GYWY-L2024-101), and it complies with the ethical principles of “ < Declaration of Helsinki > ”.
Inclusion criteria
-
Patients’ age ranges from 18 to 60 years old;
-
Diagnosed as urinary calculi, with single or cumulative diameter of stones being 20–40 mm, distributed in the upper ureteral segment or within the kidney;
-
Preoperative serum creatinine value is < 144 μmol/L.
Exclusion criteria
-
Patients with missing data, such as the lack of imaging data;
-
Patients with lower ureteral stones;
-
Patients with abnormal kidney anatomy, combined with renal insufficiency, chronic kidney disease;
-
Patients with preoperative uncontrolled urinary tract infection.
Surgical method
Patients with positive preoperative urine culture received anti-infective treatment. During the operation, patients were given general anesthesia and placed in lithotomy position; A 8.0/9.8Fr ureteral rigid endoscope (Richard–Wolf) was used to expand the ureter of the affected side to the renal pelvis and leave a zebra guide wire, after the rigid endoscope was withdrawn, a 12/14F sheath (Flexor Ureteral Access Sheath) was inserted along the guide wire, and a flexible endoscope (URF-V, Olympus) was put into the renal pelvis along the sheath. When stones were found it was shattered by holmium laser (Lumenis PowerSuite60w), and parameters were set as follow: 1–2 J, 10–30 Hz, 200–365 μm. Stone fragments were removed as much as possible, and the stone fragments was discharged by itself. A 6F ureteral stent was placed postoperatively and removed after 4 weeks. All surgeries were performed by the same urologist, who has over ten years of surgical experience and performs approximately 300 RIRS procedures annually. 4–12 weeks after the lithotripsy, KUB or CT was used to evaluate the stone clearance rate. No residual stones means stones were absented or a single asymptomatic stone less than 2 mm was found.
Study variable
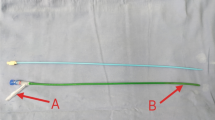
The data such as patient’s gender, age, BMI, stone size, location, and density were collected. The renal volume and renal parenchymal volume of the affected kidneys were retrospectively measured using the Canon 640 image processing and analysis software after 3D modeling with CT plain scan. (Toshiba’s third-generation super high-end 640-slice praseodymium gold CT—Aquilion ONE VISION/GE 64-row 128-layer high-end spiral CT). After loading the 5.0 mm thin slice image of the kidney scan, use the volume calc to outline the contour of the kidney at the appropriate CT value. When the boundary is discontinuous, close the contour of the kidney through the extension line. Similarly, after excluding the renal pelvis, fat, blood vessels, and other non-renal parenchymal tissues, outline the inner contour of the kidney to finally obtain the values of the renal parenchymal volume and the renal volume (see appendix Fig. 1.1). The ratio of the two is the RPRV, and the equation is as follows.
Statistical analyses
Patients were grouped into the stone-free group and the residual stone group based on the postoperative stone clearance. Data were analyzed by SPSS 25.0. The Shapiro–Wilk test assessed variable normality. Normal variables are reported as mean ± standard deviation (M ± SD) and compared with t-tests, while skewed ones are described by medians and analyzed using Mann–Whitney U tests. Categorical data, summarized as percentages, were tested with chi-square or Fisher’s exact tests, considering P < 0.05 (two-tailed) as significant. According to the stone size, it was divided into 2–2.9 cm and 3–4 cm groups, and univariate and multivariate analyses were done with logistic regression to determine the risk factors of residual stones. The ROC curve was applied to assess the predictive efficiency. The AUC between 0.7 and 0.9 indicated good value, and > 0.9 indicated high accuracy.
Results
Baseline characteristics
This research included a total of 119 participants, among whom 86 were men (72.27%). The median age was 45 (38, 52) years old, the BMI was 24.8 ± 3.29 kg/m2, the median renal parenchymal volume was 146.5 (125.73, 172) cm3, the median renal volume was 194.55 (166.15, 225.01) cm3, and the median RPRV was 0.76 (0.71, 0.81); the stone median size was 2.9 (2.3, 2.5) cm; the average density was 730.85 ± 227.27 HU, and stones of multiple locations accounted for 77.31%. According to the postoperative stone clearance, it was divided into the stone-free group (n = 85, 71.43%) and the residual stone group, refer to Table 1 for details. Gender, age, BMI, kidney volumes, renal parenchymal volume and stone characteristics were similar between the two group. (P > 0.05). However, the RPRV values between the two groups showed a statistically significant difference (P = 0.002).
The relationship between different factors and SFR in different stone size subgroups
It was divided into two groups according to the stone size: 2–2.9 cm and 3–4 cm (Table 2).
There were 62 patients in the 2–2.9 cm group (52.10%), among which the stone-free subgroup accounted for 72.58% (n = 45), and the rest is the residual stone group. There was no statistical difference in gender, age, BMI, renal parenchymal volume, renal volume, stone size, stone density, and stone location between the two groups (P > 0.05); while the RPRV and the SFR were statistically significant (P = 0.008).
There were 57 patients in the 3–4 cm group. The stone-free subgroup accounted for 70.18% (n = 57). There was no statistical difference in gender, age, BMI, renal parenchymal volume, renal volume, RPRV, stone density, and stone location between the two groups (P > 0.05); but the stone size had statistical significance in the difference of the SFR (P = 0.049).
Multivariate regression analysis between influencing factors and residual stone risk
Patients’ gender, stone location, stone size, stone density, and RPRV were considered, and logistic regression analysis was performed on different stone sized groups to establish a multivariate regression model (Table 3). In the 2–2.9 cm group, RPRV was statistically significant for risk of residual stones (OR 0.847, 95% CI 0.761–0.942, P = 0.002), indicating that the risk of stone residue decreased with increasing RPRV. However, in the 3–4 cm stone group, the stone size has no statistical significance with the risk of postoperative residual stones (P > 0.05).
ROC analysis for RPRV
To explore whether the RPRV affects the SFR after RIRS, an ROC curve was plotted (Table 4, Figs. 1, 2 and 3), and the optimal cutoff value was defined. Among the overall sample and the 2–2.9 cm stone group, the RPRV could predict the SFR after RIRS (P < 0.05). The AUC of the overall sample was 0.678, the optimal cut-off value was 0.689, the sensitivity was 95.3%, and the specificity was 41.2%. The optimal cut-off value of 2–2.9 cm group was 0.6887 (AUC 0.769, sensitivity 97.8%, specificity 58.8%). However RPRV was not a reliable predictor of postoperative SFR in the 3–4 cm group (P > 0.05).
The ROC curves are shown in the figures below.
Discussion
In this study, among 119 patients, 85 are in the stone-free group (71.43%), showing the impressive effect of RIRS in clearing stones. The proportion of men is relatively large, with a median age of 45 years, conforming to the characteristics of nephrolithiasis4,20. There is no statistical difference in gender, age, BMI, and other aspects between the two groups, meaning the samples are comparable. The renal parenchymal thickness and RPRV in the stone-free group are higher, and the latter has a statistical difference, suggesting a correlation between RPRV and SFR after RIRS. RIRS in this study are not limited to 2 cm, and the SFR has not been affected due to the stone size, which can also be seen from multivariate regression analysis between stone size and SFR (Table 3, P > 0.05). Both in univariate analysis (P = 0.008) and multivariate logistic regression analysis (OR 0.847, 95% CI 0.761–0.942, P = 0.002), RPRV has statistical significance with SFR. The larger the RPRV, the lower the risk of residual stones and the higher the SFR. While in the 3–4 cm group, there is no statistical significance between RPRV and SFR, and the stone burden is a factor affecting SFR (P = 0.049), although this difference disappears after adjusting for confounding factors. We suspect that the stone size may interfere with the influence of RPRV, resulting in neither of the two risk factors has obvious statistical significance. The predictive impact is more significant in the 2–2.9 cm group (AUC: 0.769; cut-off value 0.6887; sensitivity: 97.8%; specificity: 58.8%; P = 0.001), according to this study’s evaluation of the predictive performance of RPRV. That might be because stones between 2–3 cm have a higher propensity to move and obstruct the ureter, which would induce hydronephrosis and affect the kidney function, which impacts the excretion of minerals in urine and the development of stones21,22. Consequently, stone clearance following surgery is impacted. The point was also confirmed by Courtney Lee et al. In a retrospective analysis, the SFR of several renal functions was compared among 27,299 individuals who underwent ESWL. It was discovered that individuals with a creatinine level between 2.0–2.9 mg/dL had a lower SFR than those with a level less than 2.0mg/dL23.
The renal volume and the renal parenchymal volume are correlated with age, gender, height, weight, BMI, body surface area and total body water24,25,26,27,28. The renal volume and glomerular filtration rate decrease with age26, and some studies have reported that in healthy adults under the age of 65, the renal parenchymal volume is affected by body size and gender, but not by age or race27. There are few studies on the relationship between the renal parenchymal volume and the SFR. Sedat Taştemur et al. performed a retrospective analysis of 238 patients who underwent RIRS and performed multivariate logistic regression analysis. They found that the renal parenchymal volume in the stone-free success group was thicker, and the difference was statistically significant (P < 0.001). In the ROC analysis, a renal parenchymal volume < 141.3 cm3 was an independent risk factor for the success of the operation (OR 5.923; 95% Cl 2.886–19.263; P = 0.008). The authors suggest that a larger renal parenchyma, indicating more nephrons, may improve diuresis and facilitate the passage of urinary stones29. However, our study found that renal volume and renal parenchymal volume were not related to the SFR, while RPRV < 0.6887 was a risk factor for residual stones after RIRS, for every 0.01 unit decrease in the RPRV, the risk of stone residue after RIRS surgery increases by 15.3%. This may be because the index introduced in this paper can not only offset the errors caused by individual differences, but also make the difference in cortical thinning more significant when there is hydronephrosis, which can better reflect the condition of hydronephrosis (this is also the reason why RPRV has high sensitivity). This index is novel and has not been discussed in any other studies. It not only has high sensitivity, but also is convenient, fast, inexpensive, painless, and non-invasive, and thus has strong potential for clinical application, especially for patients with hydronephrosis. It has unlimited potential in guiding clinical decisions. For example, for patients with a lower RPRV, more aggressive measures may need to be taken to promote the excretion of stone fragments, such as performing external physical vibration lithecbole (EPVL) after RIRS or even change treatments option to PCNL.
There are some limitations of this study. This study has a relatively small sample size and is restricted to one center. Due to limitations in data availability, variables such as stone composition and immediate stone-free rate were not assessed in this study. Future research should aim to include these variables to provide a more comprehensive evaluation. However, we are confident that this study will offer insightful information to the clinic. If possible, multi-center large-sample prospective studies are needed, a clinical prediction model can also be created to further improve the predictive function of RPRV.
Conclusion
The RPRV has a relatively good predictive effect on the SFR after RIRS, especially in stone size ranging 2–2.9 cm. This study introduces a novel, accurate, and non-invasive prognostic indicator for clinical practice, which has certain guiding value for clinical decision-making, along with starting targeted medical treatments for high-risk groups.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- RPRV:
-
Ratio of renal parenchymal volume to renal volume
- SFR:
-
Stone-free rate
- RIRS:
-
Retrograde intrarenal surgery
- PCNL:
-
Percutaneous nephrolithotomy
References
Thongprayoon, C., Krambeck, A. E. & Rule, A. D. Determining the true burden of kidney stone disease. Nat. Rev. Nephrol. 16, 736–746. https://doi.org/10.1038/s41581-020-0320-7 (2020).
Scales, C. D. Jr., Smith, A. C., Hanley, J. M. & Saigal, C. S. Prevalence of kidney stones in the United States. Eur. Urol. 62, 160–165. https://doi.org/10.1016/j.eururo.2012.03.052 (2012).
Türk, C. et al. EAU guidelines on interventional treatment for urolithiasis. Eur. Urol. 69, 475–482. https://doi.org/10.1016/j.eururo.2015.07.041 (2016).
Liu, Y. et al. Epidemiology of urolithiasis in Asia. Asian J. Urol. 5, 205–214. https://doi.org/10.1016/j.ajur.2018.08.007 (2018).
Ghani, K. R. & Wolf, J. S. Jr. What is the stone-free rate following flexible ureteroscopy for kidney stones?. Nat. Rev. Urol. 12, 281–288. https://doi.org/10.1038/nrurol.2015.74 (2015).
De Sio, M. et al. Recent advances in percutaneous lithotripsy techniques. Curr. Opin. Urol. 31, 24–28. https://doi.org/10.1097/mou.0000000000000829 (2021).
Zeng, G. et al. International alliance of urolithiasis guideline on retrograde intrarenal surgery. BJU Int. 131, 153–164. https://doi.org/10.1111/bju.15836 (2023).
Osman, M. M. et al. 5-year-follow-up of patients with clinically insignificant residual fragments after extracorporeal shockwave lithotripsy. Eur. Urol. 47, 860–864. https://doi.org/10.1016/j.eururo.2005.01.005 (2005).
Khaitan, A. et al. Post-ESWL, clinically insignificant residual stones: Reality or myth?. Urology 59, 20–24. https://doi.org/10.1016/s0090-4295(01)01494-7 (2002).
Hung, S. F., Chung, S. D., Wang, S. M., Yu, H. J. & Huang, H. S. Chronic kidney disease affects the stone-free rate after extracorporeal shock wave lithotripsy for proximal ureteric stones. BJU Int. 105, 1162–1167. https://doi.org/10.1111/j.1464-410X.2009.08974.x (2010).
Abdelghany, M., Zaher, T., El Halaby, R. & Osman, T. Extracorporeal shock wave lithotripsy of lower ureteric stones: Outcome and criteria for success. Arab. J. Urol. 9, 35–39. https://doi.org/10.1016/j.aju.2011.03.010 (2011).
Erbin, A. et al. External comparison of recent predictive nomograms for stone-free rate using retrograde flexible ureteroscopy with laser lithotripsy. J. Endourol. 30, 1180–1184. https://doi.org/10.1089/end.2016.0473 (2016).
Zou, X. C. et al. Develop a radiomics-based machine learning model to predict the stone-free rate post-percutaneous nephrolithotomy. Urolithiasis 52, 64. https://doi.org/10.1007/s00240-024-01562-7 (2024).
Niwa, N. et al. Simple and practical nomograms for predicting the stone-free rate after shock wave lithotripsy in patients with a solitary upper ureteral stone. World J. Urol. 35, 1455–1461. https://doi.org/10.1007/s00345-017-2014-8 (2017).
Perks, A. E. et al. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology 72, 765–769. https://doi.org/10.1016/j.urology.2008.05.046 (2008).
Nakasato, T., Morita, J. & Ogawa, Y. Evaluation of Hounsfield Units as a predictive factor for the outcome of extracorporeal shock wave lithotripsy and stone composition. Urolithiasis 43, 69–75. https://doi.org/10.1007/s00240-014-0712-x (2015).
Koc, E. et al. Does the renal parenchymal thickness affect the efficacy of the retrograde intrarenal surgery? A prospective cohort study. Urolithiasis 49, 57–64. https://doi.org/10.1007/s00240-020-01185-8 (2021).
Ng, C. F. et al. The effect of renal cortical thickness on the treatment outcomes of kidney stones treated with shockwave lithotripsy. Korean J. Urol. 56, 379–385. https://doi.org/10.4111/kju.2015.56.5.379 (2015).
Yildirim, Ü., Ezer, M., Uslu, M., Güzel, R. & Sarica, K. Can additional variables be used to predict stone-free rates following retrograde intrarenal surgery? Anticoagulants and parenchyma thickness: A detailed examination. Urolithiasis 51, 30. https://doi.org/10.1007/s00240-022-01404-4 (2023).
Khan, S. R. et al. Kidney stones. Nat. Rev. Dis. Prim. 2, 16008. https://doi.org/10.1038/nrdp.2016.8 (2016).
Kadlec, A. O., Greco, K. A., Fridirici, Z. C., Gerber, D. & Turk, T. M. Effect of renal function on urinary mineral excretion and stone composition. Urology 78, 744–747. https://doi.org/10.1016/j.urology.2011.04.007 (2011).
Patel, P. M. et al. Association of impaired renal function with changes in urinary mineral excretion and stone composition. Urology 141, 45–49. https://doi.org/10.1016/j.urology.2020.03.023 (2020).
Lee, C., Ugarte, R., Best, S. & Monga, M. Impact of renal function on efficacy of extracorporeal shockwave lithotripsy. J. Endourol. 21, 490–493. https://doi.org/10.1089/end.2006.0319 (2007).
Nakazato, T., Ikehira, H. & Imasawa, T. Determinants of renal shape in chronic kidney disease patients. Clin. Exp. Nephrol. 20, 748–756. https://doi.org/10.1007/s10157-015-1220-1 (2016).
Shin, H. S. et al. Measurement of kidney volume with multi-detector computed tomography scanning in young Korean. Yonsei Med. J. 50, 262–265. https://doi.org/10.3349/ymj.2009.50.2.262 (2009).
Gong, I. H. et al. Relationship among total kidney volume, renal function and age. J. Urol. 187, 344–349. https://doi.org/10.1016/j.juro.2011.09.005 (2012).
Johnson, S. et al. Determinants and functional significance of renal parenchymal volume in adults. Clin. J. Am. Soc. Nephrol. CJASN 6, 70–76. https://doi.org/10.2215/cjn.00030110 (2011).
Nakazato, T., Ikehira, H. & Imasawa, T. An equation to estimate the renal cortex volume in chronic kidney disease patients. Clin. Exp. Nephrol. 22, 603–612. https://doi.org/10.1007/s10157-017-1492-8 (2018).
Taştemur, S., Şenel, S., Ölçücüoğlu, E., Kasap, Y. & Uzun, E. Effects of renal parenchymal volume and total renal volume on success in retrograde intrarenal surgery. Endouroloji Bul. 14, 7–16. https://doi.org/10.54233/endouroloji.1011076 (2022).
Acknowledgements
The authors thank all the staff and patients involved in this study, without whom this article would not have been possible.
Funding
This work was supported by the Guangzhou Science and Technology Plan Project [grant number 202201010834]; the Natural Science Foundation of Guangdong Province [grant number 2021A15010065]; the Guangzhou Health Science and Technology Project [grant number 20211A011103]; the Ministry of Education’s Industry-University Cooperative Education Project in 2022 [grant number 220904082210823]; 2022 Guangzhou Medical University Student Innovation Ability Enhancement Plan Project (106) and the Doctoral Program of Guangdong Nature Foundation [grant number 2017A030310148]; Clinical research-Cultivation project of Guangzhou Medical University [grant number GMUCR2024-02007].
Author information
Authors and Affiliations
Contributions
XZ: Data collection, statistical analysis, visualization; MH: Writing-Original Draft, writing-review & editing, visualization; YX: Methodology, validation; YY, YZ, LL, YD: Data collecction. JC, YG: Data curation; MC: Supervision, project administration; JB: Supervision, project administration, funding acquisition; DL: Conceptualization, supervision, project administration, funding acquisition.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
All patients gave informed consent to this study. This study was approved by the institutional committee review (GYWY-L2024-101), and it complies with the ethical principles of “ < Declaration of Helsinki > ”.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhen, X., Huang, M., Xu, Y. et al. The impact of the ratio of renal parenchyma to renal volume on stone-free rates after RIRS: a retrospective study. Sci Rep 15, 32073 (2025). https://doi.org/10.1038/s41598-025-15494-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15494-8