Abstract
Upon initial presentation, initial brain metastasis velocity (iBMV) is a prognostic factor for patients with brain metastases (BMs). Based on this metric, this study validated the predictive value of iBMV and introduced a Graded Prognostic Assessment (GPA)-derived scale known as melanoma-GPA. We conducted a retrospective cohort study and enrolled patients diagnosed with malignant melanoma brain metastases (MBMs) between December 2010 and February 2023. We performed univariate and multivariate Cox regression analyses to identify prognostic factors affecting overall survival (OS). A novel prognostic scoring model was derived using these factors, then melanoma-GPA and GPA predictive capabilities were assessed and compared. We enrolled 111 patients with a median OS and iBMV of 11.80 months and 2.27, respectively. The Kaplan–Meier curves showed that patients with iBMV ≤ 2.27 have better prognostic performance (P < 0.001). Multivariate analysis showed that iBMV (P = 0.035), Karnofsky Performance Status (P < 0.001), serum lactate dehydrogenase (P = 0.028), serum albumin (P = 0.041), and the systemic immune-inflammation index (P = 0.042) were independent predictors of OS. Subsequently, we established the melanoma-GPA. After risk stratification, the low-risk group had significantly longer survival than the high-risk group (17.7 vs. 7.9 months). In addition, over 3 years, the melanoma-GPA area under the curve (AUC) values were superior to GPA AUC values, indicating that melanoma-GPA has greater predictive accuracy. This study has shown that iBMV is a prognostic indicator in MBMs. Based on this factor, we established the Melanoma-GPA to comprehensively and objectively assess the prognosis of MBMs.
Similar content being viewed by others
Introduction
Malignant melanoma (MM) originates from melanocytes or melanin precursor cells and is commonly found in the skin and mucosal tissues. Notably, up to 60% of individuals with stage IV melanoma develop brain metastases (BMs). The incidence of BMs has increased in recent years due to improved imaging technologies and advancements in systemic therapies that typically do not have brain efficacy1,2. Nevertheless, the outlook for individuals with malignant melanoma brain metastases (MBMs) is grim, as their overall survival (OS) typically falls within the range of 4–9 months post-diagnosis3. Consequently, a thorough analysis of the clinical features of patients with MBMs enables healthcare professionals to assess the prognosis more comprehensively and objectively, thereby offering valuable scientific support for clinical interventions and treatment strategies.
Farris et al. (2017) established the notion of brain metastasis velocity (BMV) as a predictive biomarker specifically applicable to the salvage therapy of newly emerging BM after stereotactic radiosurgery (SRS) alone4,5. However, the application of BMV is restricted to individuals who have experienced their first intracranial failure. Because patients with MBMs have a poor OS, a part of them die as a result of lesion progression before intracranial failure. This group of patients failed to determine their BMV. In response to this limitation, Soike et al. (2018) introduced a novel metric, initial brain metastases velocity (iBMV), derived from the ratio of BMs at initial SRS to the duration since the initial MM diagnosis6. The study revealed that iBMV is correlated with OS, and shows promise for guiding treatment decisions. However, the index validation is limited to specific cancer types, such as non-small cell lung cancer, breast cancer, and renal cell carcinoma7,8,9,10, with a lack of validation in patients with MBMs. In addition, while iBMV has been validated in patients undergoing SRS for BMs, its generalizability to all patients with BMs remains uncertain.
Consequently, this study aimed to assess iBMV utility in individuals with MBMs and construct a prognostic model for patients with MBMs by incorporating this novel metric to guide clinical decision-making.
Materials and methods
Patients
This study was conducted in a cohort of 1072 patients diagnosed with MM at Fujian Cancer Hospital between December 2010 and February 2023. Patients included in the study were those who developed BMs after their MM diagnosis, including those who developed BMs following adjuvant or first-line treatment. Patients without BMs or with BMs at the time of initial cancer diagnosis were excluded. The Ethics Committee of the Fujian Cancer Hospital, Fuzhou, China (No. K2023-030-01) approved this study.
Variables
The data collection procedure consisted of two steps. Basic patient information included age, sex, Karnofsky Performance Status (KPS), time to diagnosis of melanoma, and BMs development. Tumor information included the primary tumor site, number and maximum diameter of BMs, extracranial metastases, BM with midline shift, meningeal metastasis, cerebral hemorrhage, clinical symptoms, serum lactate dehydrogenase (LDH) level, serum albumin level, lymphocyte-to-monocyte ratio (LMR), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), prognostic nutritional index (PNI) and systemic immune-inflammation index (SII).
Initial brain metastasis velocity
iBMV was computed by dividing the number of BMs by the time interval (measured in years) between the original MM diagnosis and the dates when magnetic resonance images were collected to identify BM6,7. For instance, if a patient develops four brain metastases at the time of the initial brain event, which is 6 months (0.5 years) post-diagnosis of cancer, the iBMV is 8 BM/year.
Statistical analysis
The study’s primary endpoint was the OS, calculated from the time of the initial BM to the endpoint. Figure 1 shows the study’s flow diagram. Kaplan–Meier (KM) estimators with log-rank tests were employed to assess the differences in OS. Cox regression analysis was used to identify potential OS predictors. Second, based on the multivariate analysis results, a nomogram was constructed using the 1-, 2-, and 3-year OS rates. The C-index, area under the curve (AUC) values, and the calibration curve were calculated to validate and evaluate the model regarding discrimination and consistency.
Based on the results of the multivariate analysis, specific values for the different prognostic factors were obtained by multiplying the β coefficients by the same multiplier. The study’s score was the β coefficients × 311. A novel prognostic scoring system combined with Graded Prognostic Assessment (GPA) was developed. Finally, by selecting optimal cutoff values, all MBM patients were classified into low-risk and high-risk groups. The model’s discriminatory accuracy was assessed by calculating the time-dependent receiver operating characteristics (ROC) curve.
All statistical analyses were performed with the statistical software package R (v4.2.0; http://www.R-project.org). All cut-off points were generated using X-tile software (version 3.6.1 (https://x-tile.software.informer.com/3.6/). Statistical significance was considered at P < 0.05.
Results
Baseline characteristics
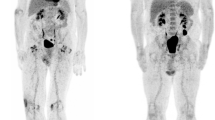
The baseline patient characteristics are presented in Table 1. A total of 111 eligible patients (55 men and 56 women) were screened. The mean and median survival times were 18.54 months and 11.80 months. MM occurred more frequently in the limbs (48.6%, 54/111). The median iBMV score for the entire study cohort was 2.27. KM survival analysis showed that patients with an iBMV above the median had a significantly shorter OS than patients with an iBMV below the median (p < 0.001, log-rank test) (Fig. 2a). The optimal cutoff values for LMR, NLR, PLR, PNI, and SII were obtained, and the KM curves are plotted in Fig. 2b,c,d,e,f.
Clinical outcomes according to different risk factors. Kaplan–Meier curve and log-rank test for OS. (a) OS stratified by patients with an iBMV above and below the median. (b) OS stratification of patients according to the optimal cut-off value for LMR. (c) OS stratification of patients according to the optimal cut-off value for NLR. (d) OS stratification of patients according to the optimal cut-off value for PLR. (e) OS stratification of patients according to the optimal cut-off value for PNI. (f) OS stratification of patients according to the optimal cut-off value for SII. OS, overall survival; iBMV, initial brain metastasis velocity; LMR, lymphocyte-to-monocyte ratio; NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio; PNI, prognostic nutritional index; SII, systemic immune-inflammation index; HR, hazard ratio; CI, confidence interval.
Nomogram construction and validation
Univariate and multivariate Cox regression analyses were conducted to examine factors influencing OS that were identifiable at initial BMs diagnosis. The univariate analysis revealed that the time to melanoma diagnosis and BMs development (p < 0.001), number of BMs (p = 0.022), iBMV (p < 0.001), KPS (p < 0.001), LDH level (p = 0.017), serum albumin level (P = 0.002), LMR (P = 0.041), NLR (P = 0.010), PLR (p < 0.001), PNI (P = 0.014), and SII (P = 0.001) were significantly associated with OS (Table 2). Subsequently, the significant factors identified in the univariate analysis were further examined using multivariate analysis. iBMV (Hazard Ratio [HR] 1.65, 95% Confidence interval [CI] 1.04–2.62, P = 0.035), KPS (HR 5.68, 95% CI 3.01–10.73, P < 0.001), LDH level (HR 1.61, 95% CI 1.05–2.46, P = 0.028), serum albumin level (HR 0.56, 95% CI 0.32–0.98, P = 0.041), and SII (HR 1.72, 95% CI 1.02–2.92, P = 0.042) were independent prognostic factors, as shown in Table 2.
Based on the multivariate models, we integrated the risk factors into a nomogram to predict patient survival at 1, 2, and 3 years (Fig. 3a). The C-index, a measure of the predictive accuracy of the nomogram, was 0.723. The calibration (Fig. 3b–d) and ROC (Fig. 3e) curves suggested that the nomogram was calibrated and discriminated appropriately. In Fig. 3e, the areas under the ROC curves at 1, 2, and 3 years were 0.802 (95%CI 0.720–0.885), 0.839 (95% CI 0.757–0.921), and 0.812 (95% CI 0.703–0.920), respectively. The precision-recall ROC curves based on 1, 2, and 3 years were shown in the Supplementary Fig. 1.
A nomogram and its validations for MBMs. (a) Nomogram predicting the OS rates at 1, 2 and 3 years for patients with MBMs. The nomogram summed the points identified on the scale for each variable. The total points projected on the bottom scales indicate the probabilities of OS rates at 1, 2 and 3 years. (b) Calibration of the nomogram for predicting 1-year OS rate. (c) Calibration of the nomogram for predicting 2-year OS rate. (d) Calibration of the nomogram for predicting 3-year OS rate. (e) The nomogram’s ROC curves and AUC values for predicting 1-, 2-, and 3-year OS rates. MBMs, malignant melanoma brain metastases; OS, overall survival; iBMV, initial brain metastasis velocity; KPS Karnofsky performance status, Serum LDH, serum lactate dehydrogenase; Serum Alb, serum albumin; SII, systemic immune-inflammation index; ROC, Receiver operating characteristic; AUC, Area under the curve; CI, confidence interval.
A novel melanoma-GPA based on initial brain metastasis velocity
Based on the multivariate regression analysis results and the GPA score, we established a novel prognostic scoring model, the Melanoma-GPA, which predicted the outcome better than the GPA score. The risk factors and distribution of points were as follows: serum albumin within the normal range: 3 points, LDH within the normal range: 1.5 points; iBMV ≤ 2.27, SII ≤ 610, age < 50, KPS between 90 and 100, number of BMs:1 and no extracranial metastases: 1 point each, age between 50 and 59, KPS between 70 and 80, number of BM 2–3:0.5 points each. The total Score ranges from 0 to 10, with a lower score indicating worse prognosis. A cut-off value of five was determined to be optimal, resulting in the categorization of patients into low-risk (56, 50.45%) and high-risk (55, 49.55%) groups. The median OS of the low- and high-risk groups were 17.7 and 7.9 months. The AUC was calculated at each time point and aggregated to generate a Time-dependent ROC plot (Fig. 4). As illustrated in Fig. 4, compared to GPA, Melanoma-GPA was significantly superior for each time point, including the AUC of 1-year (Melanoma-GPA, 0.779 (0.694–0.863) vs. GPA, 0.709 (0.617–0.802)), the AUC of 2-year (0.794 (0.690–0.899) vs. 0.664 (0.548–0.779)), and the AUC of 3-year (0.729 (0.585–0.874) vs. 0.591 (0.436–0.746)).
Discussion
As the incidence of MM continues to rise, diverse combination therapies, such as targeted therapy, immunotherapy, and SRS, are being actively explored and have resulted in improved OS for many patients12,13,14. Assessing a patient’s status at the initial presentation of BMs can facilitate the development of more holistic treatment decisions for MBMs, ultimately leading to further survival benefits.
Since iBMV was first proposed in 2018, several correlative studies have been conducted. Xu et al. retrospectively analyzed 132 patients with BM from lung adenocarcinoma and found a strong association between iBMV and OS. This suggests that iBMV may be a valuable prognostic indicator in patients with lung adenocarcinoma and BMs who underwent SRS9. Yamamoto et al. enrolled patients with BM originating from various primary tumors, including breast, lung, and kidney tumors. Their findings aligned with previous research, indicating that iBMV is a significant independent prognostic factor for patients following SRS10. A recent study examined the prognostic implications of three different types of BMV: “classic” BMV (cBMV), iBMV, and volume-based BMV (vBMV). These findings indicate that cBMV and iBMV are prognostic indicators of OS in patients with BMs treated with Stereotactic Radiosurgery, whereas vBMC has not been validated. Similarly, the study’s Cox regression analysis revealed that iBMV was associated with OS in patients with MBMs (HR 1.65, P = 0.035)15. Furthermore, we found that patients with higher iBMV exhibited a poorer prognosis than those with lower iBMV, regardless of whether they underwent SRS.
Systemic inflammatory markers, which indicate the body’s inflammatory and immune responses, are associated with increased cancer incidence and mortality16,17. In previous studies, the SII, derived from lymphocyte, neutrophil, and platelet counts, has emerged as a powerful prognostic indicator of unfavorable outcomes in patients with hepatocellular carcinoma, offering a potential tool for guiding treatment decisions18,19. Moreover, a meta-analysis of 8083 patients demonstrated a correlation between high SII and low OS in all ethnic groups, tumor types, and critical masses and increased SII was associated with lower progression-free survival (HR = 1.80, 95% CI 1.27–2.56, P = 0.001)20. Consistent with these findings, our study revealed that SII is an independent prognostic indicator of OS in patients with MBMs (HR 1.72, P = 0.042). Hence, using SII as a prognostic indicator can enhance the precision of evaluating disease progression and survival prognosis in patients, thereby facilitating the formulation of treatment strategies.
Numerous studies have been conducted on the prognostic factors of BMs, but limited research focuses specifically on MBMs due to their aggressive nature21,22,23. The GPA score, a commonly utilized clinical prognostic tool, incorporates age, KPS, the presence of extracranial metastases, and the number of BMs24. However, our findings indicate that LDH, serum albumin, iBMV, and SII significantly influence OS. Thus, a novel GPA scoring system was developed, and patients were categorized into low- and high-risk groups. The median OS of the high-risk group was notably inferior to that of the low-risk group (7.9 vs. 17.7 months). Furthermore, the predictive efficacy of the two scoring methods was evaluated using time-dependent ROC, which revealed that the AUC value of melanoma-GPA surpassed that of GPA across all time points within 1–3 years. Thus, melanoma-GPA has a better predictive value and can more comprehensively and objectively assess the prognosis of patients with MBMs. In clinical practice, physicians can utilize this scoring system at the time of a patient’s initial brain metastasis diagnosis. Without requiring complex calculations, the system provides an objective assessment of prognosis, enabling rapid risk stratification and providing valuable support for developing personalized treatment plans tailored to the patient’s condition.
This study has some limitations. First, it is a retrospective study conducted at a single center, which complicates the ability to control for potential confounding variables. Second, due to the low MM prevalence, the sample size of this study was limited. Third, future research should validate our findings in prospective studies to ensure model generalizability. And treatment-related factors should be incorporated to enhance the assessment of the effectiveness of various treatment approaches for MBMs. This will assist clinicians in selecting the optimal treatment modalities based on individual patient characteristics, ultimately leading to improved clinical outcomes in patients with MBMs.
Conclusion
In conclusion, iBMV is a prognostic prediction tool for patients with MBMs who develop such metastases after their initial cancer diagnosis. Consequently, we established Melanoma-GPA based on iBMV, which can more accurately assess patients’ prognosis compared to the GPA score. This new melanoma-GPA is expected to be a simple, convenient, and objective tool for predicting the survival of patients with MBMs in future clinical applications.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lamba, N., Wen, P. Y. & Aizer, A. A. Epidemiology of brain metastases and leptomeningeal disease. Neuro Oncol. 23 (9), 1447–1456. https://doi.org/10.1093/neuonc/noab101 (2021).
Chukwueke, U. N. & Brastianos, P. K. Precision medical approaches to the diagnoses and management of brain metastases. Curr. Treat. Opt. Oncol. 20 (6), 49. https://doi.org/10.1007/s11864-019-0649-y (2019).
Eroglu, Z. et al. How I treat brain metastases of melanoma. ESMO Open. 7 (6), 100598. https://doi.org/10.1016/j.esmoop.2022.100598 (2022).
Farris, M. et al. Brain metastasis velocity: A novel prognostic metric predictive of overall survival and freedom from Whole-Brain radiation therapy after distant brain failure following upfront radiosurgery alone. Int. J. Radiat. Oncol. Biol. Phys. 98 (1), 131–141. https://doi.org/10.1016/j.ijrobp.2017.01.201 (2017).
McTyre, E. R. et al. Multi-institutional validation of brain metastasis velocity, a recently defined predictor of outcomes following stereotactic radiosurgery. Radiother. Oncol.. 142, 168–174. https://doi.org/10.1016/j.radonc.2019.08.011 (2020).
Soike, M. H. et al. Initial brain metastasis velocity: does the rate at which cancers first seed the brain affect outcomes? J. Neurooncol. 139 (2), 461–467. https://doi.org/10.1007/s11060-018-2888-3 (2018).
Kimura, K. et al. Validation of the initial brain metastasis velocity in non-small cell lung cancer at a single cancer center. J. Neurooncol.. 162 (2), 435–441. https://doi.org/10.1007/s11060-023-04300-y (2023).
Yamamoto, M. et al. Three-institution study on applicability of initial brain metastasis velocity for breast cancer brain metastasis patients undergoing stereotactic radiosurgery. J. Neurooncol. 147 (1), 177–184. https://doi.org/10.1007/s11060-020-03412-z (2020).
Xu, G., Yang, X., Zhang, L. & Xu, M. Prognostic and predictive markers of limited (1–4) brain metastases in patients with lung adenocarcinoma after stereotactic radiosurgery: A retrospective analysis. World Neurosurg.. 164, e671–e680. https://doi.org/10.1016/j.wneu.2022.05.036 (2022).
Yamamoto, M. et al. Applicability and limitations of a recently-proposed prognostic grading metric, initial brain metastasis velocity, for brain metastasis patients undergoing stereotactic radiosurgery. J. Neurooncol. 143 (3), 613–621. https://doi.org/10.1007/s11060-019-03199-8 (2019).
Boursier, J. et al. A Stepwise algorithm using an at-a-glance first-line test for the non-invasive diagnosis of advanced liver fibrosis and cirrhosis. J. Hepatol. 66 (6), 1158–1165. https://doi.org/10.1016/j.jhep.2017.01.003 (2017).
Knispel, S. et al. Impact of a preceding radiotherapy on the outcome of immune checkpoint Inhibition in metastatic melanoma: a multicenter retrospective cohort study of the DeCOG. J. Immunother. Cancer. 8 (1), e000395. https://doi.org/10.1136/jitc-2019-000395 (2020).
Gabani, P. et al. Use of extracranial radiation therapy in metastatic melanoma patients receiving immunotherapy. Radiother. Oncol. 127 (2), 310–317. https://doi.org/10.1016/j.radonc.2018.02.022 (2018).
Bander, E. D. et al. Melanoma brain metastasis presentation, treatment, and outcomes in the age of targeted and immunotherapies. Cancer. 127 (12), 2062–2073. https://doi.org/10.1002/cncr.33459 (2021).
Christ, S. M. et al. External validation of three prognostic scores for brain metastasis velocity in patients treated with intracranial stereotactic radiotherapy. Radiother. Oncol. 189, 109917. https://doi.org/10.1016/j.radonc.2023.109917 (2023).
Ghuman, S. et al. Serum inflammatory markers and colorectal cancer risk and survival. Br. J. Cancer. 116 (10), 1358–1365. https://doi.org/10.1038/bjc.2017.96 (2017).
Yamamoto, T., Kawada, K. & Obama, K. Inflammation-related biomarkers for the prediction of prognosis in colorectal cancer patients. Int. J. Mol. Sci. 22 (15), 8002. https://doi.org/10.3390/ijms22158002 (2021).
Hu, B. et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin. Cancer Res. 20 (23), 6212–6222. https://doi.org/10.1158/1078-0432.Ccr-14-0442 (2014).
Wang, B. L. et al. Dynamic change of the systemic immune inflammation index predicts the prognosis of patients with hepatocellular carcinoma after curative resection. Clin. Chem. Lab. Med. 54 (12), 1963–1969. https://doi.org/10.1515/cclm-2015-1191 (2016).
Meng, L. et al. Prognostic value of the pretreatment systemic immune-inflammation index in patients with prostate cancer: a systematic review and meta-analysis. J. Transl. Med. 21 (1), 79. https://doi.org/10.1186/s12967-023-03924-y (2023).
Wu, Q. et al. A modified melanoma-molGPA scoring model: assessment of survival after and efficacy of different radiotherapy modalities in patients with melanoma brain metastases. Discov. Oncol. 14 (1), 116. https://doi.org/10.1007/s12672-023-00722-2 (2023).
Kuras, M. Exploring the complex and multifaceted interplay between melanoma cells and the tumor microenvironment. Int. J. Mol. Sci. 24 (18). https://doi.org/10.3390/ijms241814403 (2023).
Zhang, X. et al. Metabolism heterogeneity in melanoma fuels deactivation of immunotherapy: predict before protect. Front. Oncol. 12, 1046102. https://doi.org/10.3389/fonc.2022.1046102 (2022).
Sperduto, P. W. et al. A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int. J. Radiat. Oncol. Biol. Phys. 70 (2), 510–514. https://doi.org/10.1016/j.ijrobp.2007.06.074 (2008).
Acknowledgements
We would like to thank Editage (http://www.editage.cn) for English language editing.
Funding
This study was funded by Fujian Research and Training Grants for Youth and Middle-aged Leaders in Healthcare (2022); Fujian Province Natural Science Foundation, 2021J01433, 2024J08272; Joint Funds for the innovation of science and Technology, Fujian province, 2021Y9202, 2021Y9225; National Clinical Key Specialty Construction Program, 2021; Fujian Clinical Research Center for Radiation and Therapy of Digestive Respiratory and Genitourinary Malignancies.
Author information
Authors and Affiliations
Contributions
Y.Z.: Formal analysis; writing-original draft. F.L.: Methodology. H.L.: Software. Q.W.: Data curation. T.Z.: Investigation. J.C.: Resources. Y.W.: Visualization. J.L.: Supervision. L.T.: Writing-review and editing. Y.C.: Funding acquisition. P.L.: Writing-revise and editing. J.L.: Project administration.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This is a retrospective study and which was conducted in accordance with the 1964 Declaration of Helsinki and International Conference on Harmonization of Good Clinical Practice Tripartite guidelines. This clinical study was approved by the Ethics Committee of Fujian Cancer Hospital Fuzhou, China (No. K2023-030-01). Due to the retrospective nature of the study, Institutional Review Board waived the need of obtaining informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zeng, Y., Lin, F., Li, H. et al. Melanoma GPA as a novel prognostic scoring model based on initial brain metastasis velocity. Sci Rep 15, 29446 (2025). https://doi.org/10.1038/s41598-025-15635-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15635-z






