Abstract
Traditional interventions are largely offline, lack continuous support, and primarily focus on improving knowledge. This study aimed to explore the feasibility, acceptability, and preliminary effects of a phased online support program for patients with diabetes. A mixed-methods design with convenience sampling was adopted in this study. A total of 27 patients with diabetes were recruited from a tertiary hospital in Hainan Province. The patients underwent a phased online support program. Feasibility was assessed based on recruitment, participation, and retention rates. After the patients received the intervention at the 9-month follow-up, acceptability was assessed using one-on-one semi-structured interviews. The preliminary effects of the program were assessed by observing changes in clinical and psychosocial indicators. A designated researcher collected all the data from January 2022 to March 2023. The recruitment, participation, and retention rates were all over 80%. Participants perceived positive changes after participating in the program; they considered the program to be highly acceptable and expressed eagerness for ongoing support. Significant improvements were observed in HbA1c, fasting blood glucose, blood pressure, blood lipid profile, weight, body mass index, self-efficacy, diabetes distress, diabetes knowledge, self-management behavior, and chronic disease resource utilization at the 12-month follow-up. The phased online support program for patients with diabetes is feasible and acceptable, with promising preliminary results.
The study was registered in the Chinese Clinical Trial Registry (ChiCTR2400082136, http//www.chictr.org.cn/, 21/3/2024).
Similar content being viewed by others
Background
By 2021, approximately 537 million adults worldwide were living with diabetes mellitus (DM)1. In China, where the prevalence of diabetes is 12.8%, with approximately 140 million patients, ranking first globally, over 90% of diabetic patients have type 2 diabetes mellitus (T2DM)2. Diabetes and its related complications pose a severe challenge to public health. There is evidence showing that patients with high self-efficacy, low diabetes distress, and greater diabetes knowledge often exhibit better self-management behaviors (SMB)3,4,5,6. This indicates that a program addressing the above four variables can be delivered to patients with DM.
Diabetes self-management education (DSME) is a recognized approach for managing diabetes domestically and internationally7,8. However, owing to the lack of continuous support and the fact that most DSME programs for patients with diabetes focus primarily on knowledge/cognition improvement, the prevention and control effects are challenging to maintain for long periods and tend to diminish within 6–12 months9,10. A study on a self-management behavioral change model indicated the critical role of enhancing self-efficacy in achieving long-term improvements in SMB and reductions in diabetes distress up to a 12-month follow-up11. Thus, in addition to increasing diabetes knowledge during the initial stage, a phased support program focusing on systematically boosting self-efficacy and reducing diabetes distress might effectively help patients with T2DM maintain diabetes self-management (DSM).
In addition, previous DSME programs have mostly been conducted in an offline, face-to-face format12,13,14. These programs are susceptible to interruption by epidemic diseases such as COVID-19. It is recommended that technology be utilized to deliver education programs15. Online support formats can overcome time and location limitations16, effectively increasing program accessibility and providing opportunities for sustainable support from healthcare providers. A systematic review found that the biomedical benefits obtained from the online education services were at least comparable with the face-to-face interventions16. This indicates the feasibility of providing online support for patients with DM.
Currently, research on the systematic integration of phased and online support interventions, with a focus on improving patients’ self-efficacy and reducing diabetes distress, is limited. To address these gaps, this study built upon structured education programs previously developed by the research team13,17 and was guided primarily by the Tyler Model18, Social Cognitive Theory19, Self-efficacy Theory20, and the Self-Management Behavioral Change Model11. The Tyler Model structured the program in terms of objectives, content, methods, and evaluation, thus ensuring practicality18. Social Cognitive Theory described the interactive relationship between individual behaviors and internal (e.g., self-efficacy) and external factors (e.g., chronic disease resource utilization), offering insights into behavioral change mechanisms19. Self-efficacy Theory emphasized individuals’ self-efficacy and highlighted its direct impact on self-management behaviors13,17. Moreover, the Self-Management Behavioral Change Model provided implications for intervention priorities at different time points11. Consequently, a Phased Online Support Program (POSP) was developed, comprising a structured education program centered on self-efficacy and a phased diabetes self-management support component aimed at systematically enhancing self-efficacy and reducing diabetes distress20. However, the feasibility, acceptability, and preliminary effects of the POSP in patients with T2DM remain unclear. Therefore, this study aimed to evaluate the feasibility, acceptability, and preliminary effects of the POSP in patients with T2DM.
Methods
Study design
A mixed-methods convergent study design combining quantitative and qualitative approaches was adopted to evaluate the feasibility, acceptability, and preliminary effects of the POSP. Quantitative assessments included analysis of clinical outcomes and psychological changes at baseline and at 3, 6, 9, and 12 months using a pre-post self-control trial. Qualitative insights were gathered utilizing a descriptive phenomenological approach through one-to-one semi-structured interviews to assess the acceptability of the intervention at 9 months.
Sample and setting
Using a convenience sampling method, 27 patients with T2DM from the Endocrinology Department of a tertiary hospital in Hainan, China, were recruited between December 2021 and January 2022. Inclusion criteria were: (1) diagnosis of T2DM based on China’s Type 2 Diabetes Prevention and Treatment Guidelines (2020 edition)8; (2) aged 18–75 years; (3) HbA1c of ≥ 7.5% in the previous three months; (4) not currently treated with insulin or insulin analogues; (5) no previous participation in systematic diabetes health education courses; and (6) agreement to participate in the study and provision of informed consent. Exclusion criteria included: (1) pregnant or planning for pregnancy; (2) mobility difficulties, mental disorders, cognitive disabilities, and inability to cooperate; (3) severe diabetic complications; (4) presence of tumors and receipt of radiotherapy or chemotherapy within the previous six months; and (5) participation in other similar research projects. The sample size was calculated using an HbA1c mean difference and standard deviation of 1.59% and 1.18%, respectively, according to a previous study13. In addition, α was set at 0.05 (two-sided test), β was set at 0.10, and the attrition rate was set at 20%. The total number of participants in the quantitative part was determined to be at least 10. For the qualitative interviews, a purposive sampling method was used to ensure a representative selection of interviewees. Participants were selected from patients who had received all interventions in the quantitative component. Data saturation was used to determine the appropriate number of participants for interviews.
Intervention: POSP
The POSP consisted of two sessions (seven modules): a self-efficacy-focused structured education session (four modules) and a phased self-management support session (three modules). Sessions, modules, and their associated theoretical frameworks are presented in Table 1. The POSP was developed based on the Self-Management Behavioral Change Model11, Self-efficacy Theory, the basic curriculum and instructional principles proposed by Tyler, and the Taxonomy of Educational Objectives14,18. The content of the POSP was developed by the research team during the preliminary stages, and the first session was previously validated and widely disseminated13,14,18,20. All seven modules were administered to small-groups (6–8 participants per group) via the Lizhi Micro-Courses platform within a structured, internet-based delivery framework (screenshots of online modules are provided in Supplementary A). Each module in Session One lasted 60–90 min, was scheduled at weekly intervals, and was implemented consecutively over four weeks. Modules in Session Two lasted 30–40 min each and were delivered at 3-, 6-, and 9-month follow-up intervals. The researcher facilitated the intervention and promptly answered participants’ questions. Endocrinologists and nurses provided additional support, communication, and guidance to participants as needed.
Feasibility evaluation
Recruitment, participation, and retention rates were used to assess feasibility. The recruitment rate was defined as the percentage of individuals who met the initial recruitment criteria and consented to participate in the intervention. The participation rate was defined as the percentage of patients who participated in all interventions. The retention rate was defined as the retention of patients at the 12-month follow-up and was calculated as follows: [(total number of intervention participants - total number of dropout participants at the end of the intervention)/total number of intervention participants] × 100%.
Preliminary effect evaluation
The preliminary effect evaluation included assessments of the primary outcome (HbA1c) and the secondary outcomes (blood lipid profile, diabetes knowledge, self-management behavior, self-efficacy, diabetes distress, and chronic disease resource utilization) at baseline (T0), 3 months (T1), 6 months (T2), 9 months (T3), and 12 months (T4). The additional secondary outcomes (fasting blood glucose (FBG), blood pressure (BP), and weight) were evaluated at baseline (T0), 2 weeks, 3 weeks, 4 weeks, 3 months (T1), 6 months (T2), and 9 months (T3).
Primary outcome
The primary outcome (HbA1c) was examined at the central laboratory by collecting intravenous blood at each assessment time point.
Secondary outcomes
The secondary clinical outcomes (blood lipid profile, including total cholesterol (TC), triglycerides (TG), high-density lipoprotein (HDL), and low-density lipoprotein (LDL)) were examined at the central laboratory by collecting intravenous blood at each assessment time point. Additional secondary outcomes (FBG, body weight, and BP) were measured using fixed instruments and standardized methods before initiating the intervention.
Other secondary outcomes
Diabetes knowledge
This was assessed using a diabetes-related knowledge questionnaire in the Chinese language. The questionnaire, translated and adapted by Liu21, contained 10 items, with each item worth one point. Scores ranged from 0 to 10, with higher scores indicating greater mastery of diabetes knowledge. The Cronbach’s α of the questionnaire was 0.70321.
Self-management behavior
This was evaluated using the Chinese version of the Summary of Diabetes Self-Care Activities. The Chinese version of the scale, translated and adapted by Wan et al.22, contained 11 items across six dimensions: general diet, specific diet, exercise, blood glucose monitoring, foot care, and medication adherence. Each item was scored from 0 to 7, and total scores ranged from 0 to 77. Higher scores indicated better diabetes self-management behaviors. The Cronbach’s α of the scale was 0.62, and the load factor of the scale was > 0.822.
Diabetes self-efficacy
This was assessed using the Chinese version of the Self-Efficacy for Diabetes scale, developed by Wei et al.23. The 9-item scale covered four dimensions: diet, exercise, blood glucose, and disease control. A 5-point Likert scale was used for scoring, with total scores ranging from 9 to 45. Higher scores indicated greater diabetes self-efficacy. The Cronbach’s α of the scale was 0.94123.
Diabetes distress
This was assessed using the Chinese version of the Diabetes Distress Scale. The Chinese version of the scale translated and adapted by Yang et al.24, contained 17 items and comprised four dimensions: emotion-related, doctor-related, lifestyle-related, and interpersonal relationship-related distress. A 6-point Likert scale was used for scoring, with total scores ranging from 17 to 102. Higher mean scores indicated greater diabetes-related distress. The Cronbach’s α of the scale and its dimensions ranged from 0.842 to 0.95124,25.
Chronic disease resource utilization
This was assessed using the Chinese version of the Chronic Disease Resource Scale, translated and adapted by Hua et al.26. The scale originally contained 27 items across seven dimensions. This study adopted 17 items related to the six dimensions (medical staff, family and friends, self-regulation, neighbourhood and community, media policy, and social groups) due to limitations in the participants’ work environments. A 5-point Likert scale was used for scoring, with total scores ranging from 17 to 85. Higher scores indicated greater availability of resources to participants. The Cronbach’s α coefficient and test-retest reliability were 0.840 and 0.704, respectively27.
Demographic information
Demographic data were collected using a self-designed questionnaire. The information included general demographic characteristics (sex, age, education level, occupation, co-residents, marital status, economic income, smoking and alcohol consumption habits, and use of electronic devices for health management), and health-related factors (height, weight, body mass index [BMI], number of diseases and complications, family history of diabetes, and duration of illness).
Evaluation of acceptability
Upon completion of the ninth-month intervention, the principal investigator conducted one-on-one semi-structured interviews to evaluate the acceptability of the POSP. Each interview primarily covered the participants’ experiences and perceptions, factors influencing the maintenance of self-management behaviors, suggested improvements for the intervention, participants’ commitment to continuing self-management support, and their willingness to recommend the program to others (Supplementary B). With participant consent, the entire interview process was recorded using a voice recorder.
Data collection
The researchers collected all data from January 2022 to March 2023. Quantitative baseline data were collected in person. However, follow-up data were collected via telephone and WeChat because of the coronavirus disease 2019 pandemic. After completion of the survey, the researchers checked the questionnaires promptly. In the event of omissions or obvious errors, the researchers asked the patients to promptly make necessary additions or modifications, respectively.
Regarding qualitative data, a researcher who had received training in qualitative theory and methods and specialized in diabetes self-management was responsible for the interviews. A quiet, comfortable environment was chosen, and open-ended questions were asked through face-to-face interviews. The interviews were recorded, and the interviewees’ nonverbal behaviors were carefully noted. Each interview lasted approximately 20–30 min. The participants’s information was kept anonymous and confidential. Two researchers were responsible for recording the written text and conducting a cross-check for accuracy within 24 h. Non-verbal information was appropriately labeled, and the transcribed texts were returned to the interviewees for verification to ensure accuracy. Finally, the transcribed texts were encoded, with attention paid to privacy protection.
Data analysis
Quantitative data analysis was performed using SPSS version 25.0. Missing data at follow-up points were addressed using multiple imputation methods. General demographic characteristics of participants and questionnaire and scale scores were presented as means (standard deviations) or frequencies (percentages). Intervention effects on various within-group indicators over time were analyzed using repeated-measures analysis of variance (RM-ANOVA). Differences between pre- and post-intervention time points were assessed using paired t-tests or Wilcoxon signed-rank tests. Statistical significance was defined as P < 0.05 (two-tailed).
Qualitative data were analyzed using Colaizzi’s seven-step analysis method28. The seven analysis steps were as follows: (1) reading textual materials repeatedly and become familiar with the text after collecting and transcribing; (2) extract and identify meaningful and representative statements; (3) encode recurring ideas; (4) scrutinize, reflect, and imagine all meaningful viewpoints, and cluster them into a preliminary thematic framework; (5) connect these themes with the research objective to form a cohesive narrative; (6) refine and determine the themes; and (7) validate the basic structure and form a collaborative report.
Ethical considerations
This study adhered to the Declaration of Helsinki. Moreover, this study was reviewed and approved by the Ethical Committee of Hainan Medical University (HYLL-2022-012). The study was also registered in the Chinese Clinical Trial Registry (ChiCTR2400082136, http://www.chictr.org.cn/, 21/3/2024). All participants involved in this study provided informed consent prior to their participation. Participants received a small amount of monetary compensation (400 RMB/person) after completing the research.
Results
Characteristics of participants
The mean age of the 27 participants was 47.11 ± 10.96 years, and the mean BMI at baseline was 24.99 ± 10.96 kg/m2. Among the 27 participants, 66.7% were men, 37.0% were college level or above, 44.4% had diabetes-related complications, 51.9% had diabetes for 1–5 years, and all had medical insurance. Detailed data are shown in Table 2.
Feasibility
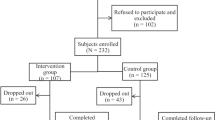
A total of 32 patients were initially recruited by physicians based on predefined inclusion and exclusion criteria and voluntary participation. Two patients were excluded due to the lack of intelligent devices, and three were disqualified due to work-related scheduling conflicts. Ultimately, 27 participants provided informed consent. Among these, two withdrew voluntarily during the seventh module due to occupational constraints, resulting in module non-completion. Finally, 25 participants completed all seven learning modules at the 9-month follow-up, and completed all assessments at the 12-month follow-up. The recruitment rate was calculated at 84.38% (27/32), and both participation and retention rates were 92.59% (25/27). (Fig. 1).
Preliminary results
Repeated-measures analysis of variance indicated significant time effects on patients’ HbA1c, TC, HDL, DK, DSMB, DSE, DD, and CDRU following the implementation of POSP (P < 0.05, Table 3). Pairwise comparisons revealed that the primary outcome, HbA1c, significantly improved at T1, T2, T3, and T4 compared with T0 (P < 0.05, Table 3). Regarding lipid profiles, total cholesterol (TC) improved significantly at T1, T2, T3, and T4 (P < 0.05; Table 3). Additionally, triglyceride (TG) levels significantly improved at T2, T3, and T4, and low-density lipoprotein cholesterol (LDL) significantly improved at T1, T2, and T4 (P < 0.05; Table 3). Notably, high-density lipoprotein cholesterol (HDL) showed significant improvement only at T4 (P < 0.05; Table 3). Concerning psychosocial indicators, diabetes self-management behaviors (DSMB), self-efficacy (DSE), diabetes distress (DD), and chronic disease resource utilization (CDRU) improved significantly at T1, T2, T3, and T4 compared to baseline (P < 0.05; Table 3). Other metabolic indicators, including fasting blood glucose (FBG), systolic blood pressure, diastolic blood pressure, body weight, and body mass index (BMI), consistently improved throughout the intervention (P < 0.05; Table 4).
Acceptability
Upon completion of the seven modules, semi-structured interviews were conducted with 9 participants. The mean age of the interviewees was 42.22 years (SD = 12.12), with 6 males. Regarding education, 4 participants had completed secondary vocational school, high school, or below, while 5 had education levels of college or above. Occupations included 2 farmers, 4 professionals, 1 worker, 1 salesperson, and 1 teacher. Among these participants, 6 were married, and 3 reported diabetes-related complications. The duration of diabetes diagnosis ranged from 1 month to 5 years (Table 5). In-depth thematic analysis revealed three themes and 9 sub-themes (Supplementary C).
Theme one: positive effects of the program on patients
Knowledge enhancement
Many interviewees indicated that the intervention significantly enriched their diabetes-related knowledge. “As someone with limited cultural knowledge, I previously knew little about the numerous complications of diabetes. At first, I was completely unaware of them.” (Patient 5).
Behavioral changes
Participants indicated that the increased knowledge acquired from the course translated into improved self-management behaviors. “After learning these things, I’ve become more mindful. For example, when eating, I follow the dietary guidance taught in the course. As a Hainanese who loves chicken, I used to enjoy chicken skin, but now I avoid it. I pay attention to details I didn’t know before. Previously, I thought avoiding fatty meat was enough for a healthy diet.” (Patient 2).
Confidence boost and worry alleviation
Most interviewees noted that understanding the benefits of self-management benefits enhanced their self-efficacy and confidence in disease management and reduced their anxiety. “Another positive aspect is feeling more at ease. I can ask questions about my condition without burdening my family, so I’m less anxious.” (Patient 1).
Theme two: factors influencing patient self-management support
Promoting factors
Interviewees identified multiple sources of support that facilitated self-management, including medical staff, fellow diabetes patients, family, and friends, as well as a positive attitude towards the disease. “You work so hard to teach us, and every now and then you ask me how my blood sugar control is going. Do I feel uncomfortable? You care so much about us; I definitely have the motivation to (stick to self-management)!” (Patient 4) “I think it’s great that we can share our experiences with each other (patients). We can exchange tips on managing and learn from each other!” (Patient 5).
Obstacle factors
The chronic, challenging, and complex nature of diabetes management presented several barriers for patients. These include insufficient awareness of the benefits of self-management, reliance on personal experience and inertia, work environment limitations, and initial discomfort with lifestyle changes. “Sometimes, I’m just too lazy to check my blood sugar or exercise, even though I know it’s beneficial.” (Patient 3) “I used to eat late-night snacks and drink wine with friends. Maybe I got used to it, but I still had some alcohol in the beginning, and it was difficult to change all of a sudden.” (Patient 9).
Theme three: feedback on this program
Acceptability
All interviewees expressed high acceptability of the program, highlighting its substantial benefits. “I think online teaching is quite good.” (Patient 5) “The course is excellent. The initial four classes on diabetes basics were easy to understand, and the periodic reinforcement helps with supervision.” (Patient 3) “I find this course quite meaningful. Especially during the pandemic, online teaching offers great convenience.” (Patient 6).
Recommendations
While recognizing the program’s strengths, several interviewees provided suggestions for improvement, such as recording sessions for convenient review, conducting diabetes education sessions in outpatient clinics, and slowing the teaching pace. “It would be convenient if the courses were recorded as videos for us to watch at any time.” (Patient 3) “Offline education in outpatient clinics could allow patients to learn while waiting for treatment.” (Patient 7) “The teaching pace is a bit fast; it would be better if it could be slower.” (Patient 9).
Desire for sustained support
Diabetes self-management is a lengthy process involving multiple aspects. Participants expressed a desire for continuous support from healthcare professionals, family, friends, and national policies. “The program is excellent. I wish to have access to such courses consistently” (Patient 2) “I hope that these courses can be widely promoted, and I also hope my employer can understand and support them.” (Patient 6).
Discussion
The POSP was feasible and acceptable for patients with T2DM. Preliminary results on HbA1c, some other metabolic indicators, and psychosomatic indicators showed significant improvements at the 12-month follow‐up.
In this study, the recruitment, participation, and retention rates were satisfactory, indicating that the POSP was acceptable according to the Quality Assessment Tool for Quantitative Studies29. The POSP’s 12-month participation and retention rates exceeded those reported Ruan et al.’s diabetes education program (60.83% retention)30. This can be attributed to three key factors. First, the POSP was well-designed based on behavioral change theories, evidence from guidelines and practice, and characteristics of the Chinese population. Second, the program gradually supported patients in two stages in small groups of 6–8 participants, fully considering the characteristics of patient behaviour change and facilitating patient interaction through group-format learning. Third, the small monetary compensation provided in the program likely enhanced participation and retention.
Compared with previous studies on DSME and structured education12,13,14,17 and routine practice, the core strengths of POSP lie in its continuity and accessibility. By providing online support, POSP established a closed-loop system of “demand triggering-immediate response-continuous tracking,” which proved particularly valuable during the pandemic. Online interventions overcame temporal and geographical constraints, satisfied the demand for “non-contact services,” and addressed issues related to uneven distribution of medical resources, as well as patient limitations in time and mobility. While online support might face challenges such as incomplete information delivery and operational barriers, especially for some elderly patients, POSP offers a practical alternative for both patients and clinical staff amid limited health resources and pandemic-related restrictions. Nonetheless, its overall effectiveness warrants further investigation.
Psychological indicators of self-efficacy, diabetes distress, diabetes knowledge, chronic disease resource utilization, and self-management behaviors improved significantly in this study. Improvements in self-efficacy and diabetes distress were also found in another online-based structured education program for T2DM conducted in England31. The qualitative interview results in this study confirmed that the POSP contributed to positive outcomes for patients, and the promoting factors further confirmed these findings. This might be due to the fact that the POSP was developed based on self-efficacy theory32 and the self-management behavioral change model11. Moreover, strategies adopted in the program, such as gradually setting goals, regular review and repetition, encouragement, providing positive feedback, explaining knowledge, small monetary incentives, discussing concerns, and introducing available and reliable external resources, were also useful. The qualitative interview results also indicated that resources from health professionals, family and friends, fellow patients, the work environment, and national policies were important for patients with T2DM. This indicated that obtaining additional external support could be beneficial for patients in sustaining behavior changes. However, the lack of detailed information on daily practices hindered understanding of resource integration and potential barriers to sustained self-management. Notably, the qualitative interviews revealed certain individual obstacles to self-management behaviors, such as insufficient perception of the benefits of self-management, reliance on previous habits (empiricism), inertia, and initial discomfort with lifestyle changes. However, these findings could not be quantitatively confirmed. Thus, these factors should be considered when delivering the POSP.
Based on the quantitative results, positive effects of the POSP on HbA1c, FBG, blood lipid profile, BP, weight, and BMI were observed in this study, similar to studies conducted by De la Fuente et al.33 Metabolic improvements likely stemmed from enhanced diabetes self-management behaviors, which were closely associated with HbA1c, FBG, and weight34. However, due to the lack of a control group, the impact of the POSP on metabolic indicators may have been influenced by other confounding factors, such as medication alteration. The effectiveness of the POSP can be evaluated in a broader setting and population in future randomized controlled trials.
The qualitative evaluation indicated that the program was highly acceptable for patients with T2DM. The acceptability of the POSP was mainly attributed to its design based on patient-needs assessments and compliance with the characteristics of behavioral change20,21. Online learning was convenient for patients during the COVID-19 pandemic, indicating that online learning has potential in diabetes education. However, one study noted that the completion rate of online programs is low31. Therefore, patients in this study expressed that they hoped to gain continuous support from healthcare professionals, family and friends, and national policies. Delivering the POSP online and providing continuous support for patients might have potential, but implementation relies on the commitment of participation of multiple parties, such as the government, hospitals, healthcare professionals, and supervision and support from family members and friends. Patients also provided additional suggestions for the program, such as recording the courses on video, conducting diabetes education in outpatient clinics, and slowing the speakers’ pace. Health professionals can consider these recommendations based on real-world conditions.
Strengths and limitations
This study employed a mixed-methods design to evaluate the feasibility, acceptability, and preliminary effects of the POSP. This design enabled a comprehensive understanding of the POSP from multiple dimensions. The real-world mixed-methods approach involved 9 months of continuous support by the POSP and a 12- month follow-up, yielding promising results in real clinical settings. However, several limitations should be acknowledged. First, the study lacked a control group and included a small sample size, which hindered the ability to draw definitive conclusions about the POSP’s effects and limited its generalizability. Future research should prioritize multi-centre randomized controlled trials (RCTs) with larger samples to rigorously evaluate program effectiveness. Additionally, in qualitative interviews, participants’ reflections on their achievements and perceptions might have been influenced by their prior engagement with quantitative questionnaires, though this effect was mitigated in the study design by scheduling qualitative interviews in the ninth month, when no questionnaire assessments were performed.
Conclusions
The Phased Online Support Program demonstrated feasibility and acceptability among patients with T2DM, showing promising preliminary effects. Health professionals are encouraged to implement this program to enhance patient self-efficacy, diabetes knowledge, self-management behaviors, chronic disease resource utilization, clinical outcomes, and to reduce diabetes-related distress. Future research should focus on developing a sustainable, online-based model offering continuous phased support, and include a control group for rigorous evaluation of program effectiveness.
Data availability
The datasets generated during and/or analyzed during this study are available from the corresponding author on reasonable request.
Abbreviations
- DM:
-
Diabetes Mellitus
- T2DM:
-
Type 2 Diabetes Mellitus
- SMB:
-
Self-Management Behaviors
- DSME:
-
Diabetes Self-Management Education
- POSP:
-
Phased Online Support Program
References
Sun, H. et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. : 109119. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=34879977&query_hl=1 (2022). 2022;183 https://doi.org/10.1016/j.diabres.2021.109119
Li, Y. et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross-sectional study. BMJ. 2020 2020;369:m997. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=32345662&query_hl=1https://doi.org/10.1136/bmj.m997
He, Q. et al. Diabetes self-management and its related factors among Chinese young adults with type 2 diabetes mellitus. Nurs Open. 2023 May 23. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=37221986&query_hl=1 (2023). https://doi.org/10.1002/nop2.1834
Jiang, X. et al. The Mediating Role of Self-Efficacy in Shaping Self‐Management Behaviors Among Adults with Type 2 Diabetes. Worldviews Evid Based Nurs. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/wvn.12354https://onlinelibrary.wiley.com/doi/pdf/ (2019). 2019;16(2):151 – 60 https://doi.org/10.1111/wvn.12354 doi: 10.1111/wvn.12354.
Lamptey, R. et al. Diabetes self-management education interventions and self-management in low-resource settings; A mixed methods study. PLoS One. : e0286974. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=37450431&query_hl=1 (2023). 2023;18(7) https://doi.org/10.1371/journal.pone.0286974
Patra, S., Patro, B. K., Padhy, S. K. & Mantri, J. Prevalence of diabetes distress and its relationship with self-management in patients with type 2 diabetes mellitus. Ind Psychiatry J. 2021 Jul-Dec;30(2):234 – 39. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=35017806&query_hl=1 (2021). https://doi.org/10.4103/ipj.ipj_60_19
American Diabetes Association. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes-2022. Diabetes Care. ;45(Supplement_1): S8-16. Available from: https://diabetesjournals.org/care/article/45/Supplement_1/S8/138915/1-Improving-Care-and-Promoting-Health-inhttps://diabetesjournals.org/care/article-pdf/45/Supplement_1/S8/637531/dc22s001.pdf (2022). https://doi.org/10.2337/dc22-S001
Chinese Diabetes Association. Guideline for the prevention and treatment of type 2 diabetes mellitus in China. Chin J Diabetes Mellitus. 2021;13(4):315–409. Available from: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjIxMjIyEg56aHRuYjIwMjEwNDAwNRoIZGltZjU3aWM%3D (2020). edition https://doi.org/10.3760/cma.j.cn115791-20210221-00095
Captieux, M. et al. Supported self-management for people with type 2 diabetes: a meta-review of quantitative systematic reviews. BMJ Open. : e024262. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=30552277&query_hl=1 (2018). 2018;8(12) https://doi.org/10.1136/bmjopen-2018-024262
Van Puffelen, A. L., Rijken, M., Heijmans, M., Nijpels, G. & Schellevis, F. G. Effectiveness of a self-management support program for type 2 diabetes patients in the first years of illness: Results from a randomized controlled trial. PLoS One. 2019 2019-1-1;14(6):e0218242. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=31247039&query_hl=1https://doi.org/10.1371/journal.pone.0218242
Jiang, X., Jiang, H. & Li, M. The Role of Self-Efficacy Enhancement in Improving Self-Management Behavior for Type 2 Diabetes Mellitus Patients. Diabetes Metab Syndr Obes. : 3131-38. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=39193548&query_hl=1 (2024). 2024;17 https://doi.org/10.2147/DMSO.S460864
Adam, L., O’Connor, C. & Garcia, A. C. Evaluating the Impact of Diabetes Self-Management Education Methods on Knowledge, Attitudes and Behaviors of Adult Patients with Type 2 Diabetes Mellitus. Can J Diabetes. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=29449096&query_hl=1 (2018). 2018;42(5):470 – 77 https://doi.org/10.1016/j.jcjd.2017.11.003
Jiang, X. et al. The Effectiveness of a Self-Efficacy-Focused Structured Education Program (SSEP) in Improving Metabolic Control and Psychological Outcomes of Type 2 Diabetes Patients: a 12-Month Follow-Up of a Multicenter Randomized Controlled Trial. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2021 2021; 14:305 – 13. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=33519219&query_hl=1https://doi.org/10.2147/DMSO.S290029
Liu, Y. et al. A culturally sensitive nurse-led structured education programme in patients with type 2 diabetes. Int J Nurs Pract. : e12757. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=31261444&query_hl=1 (2019). 2019;25(5) https://doi.org/10.1111/ijn.12757
American Diabetes Association Professional Practice Committee. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45(Suppl 1): S60-82. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=34964866&query_hl=1 (2022). https://doi.org/10.2337/dc22-S005
Alonso-Carril, N. et al. Could Online Education Replace Face-to-Face Education in Diabetes? A Systematic Review. Diabetes Ther. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=38743305&query_hl=1 (2024). 2024;15(7):1513-24 https://doi.org/10.1007/s13300-024-01595-6
Jiang, X. et al. The effectiveness of a self-efficacy-focused structured education programme on adults with type 2 diabetes: a multicentre randomised controlled trial. J Clin Nurs. 2019. ;28(17–18):3299 – 309. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=31066115&query_hl=1 (2019). https://doi.org/10.1111/jocn.14908
Tyler, R. W. Basic Principles of Curriculum and Instruction [M] (People’s Education, 1994).
Bandura, A. Toward a psychology of human agency: pathways and Reflections[J]. Perspect. Psychol. Sci. 13 (2), 130–136 (2018).
Xing, S. et al. Construction of a self-management support intensive phase intervention programs for Type 2 Diabetes Mellitus patients. Chinese Nursing Management. ;23(10):1493-99. (2023). Available from: https://kns.cnki.net/kcms2/article/abstract?v=Y2wviAwYlnKJJ3z1312oO7G4rLYWfgoF1GK-CvLlTcaHz99ZIEWpjCJ8u_ZDjqHNqKT1u6_JqYz-g5L8XLSH1kWev9Ct6kNQgYL62sfmgb0H_UBr402cI5bVz3pxWucgMGETVKcyWlDDoXltrewspg==&uniplatform=NZKPT&language=CHS
Liu, Y. et al. A pilot study of structured treatment and education program for type 2 diabetic patients without insulin therapy. Chin J Diabetes. ;24(7):638 – 44. Available from: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjIxMjIyEhB6Z3RuYnp6MjAxNjA3MDE2GghkaW1mNTdpYw%3D%3D (2016). https://doi.org/10.3969/j.issn.1006-6187.2016.07.016
Wan, Q., Shang, S., Lai, X. & Pan, J. Study on the reliability and validity of summary of diabetes self-care activities for type 2 diabetes patients. Chinese Journal of Practical Nursing. ;24(7):26–27. Available from: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMwMTEyEg9zeWhsenoyMDA4MDcwMDkaCGNkczFpNWt2 (2008). https://doi.org/10.3760/cma.j.issn.1672-7088.2008.07.009
Wei, J. Research on Relationship between Diabetes Knowledge, Self-Efficacy and Self-management among Rural Elderly Patients[D], Hangzhou Normal University, Hangzhou; (2013). Available from: https://d.wanfangdata.com.cn/thesis/ChJUaGVzaXNOZXdTMjAyMzAxMTISCFkyMjgzNjMyGghjZHMxaTVrdg%3D%3D
Yang, Q. Reliability and validity and clinical practice of the Chinese version of Diabetes Distress Scale[D], Southern Medical University, Guangzhou; (2010). Available from: https://d.wanfangdata.com.cn/thesis/ChJUaGVzaXNOZXdTMjAyMzAxMTISCFkxNzY5OTMwGghjZHMxaTVrdg%3D%3D
Fisher, L., Hessler, D. M., Polonsky, W. H. & Mullan, J. When is diabetes distress clinically meaningful: establishing cut points for the Diabetes Distress Scale. Diabetes Care. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=22228744&query_hl=1 (2012). 2012;35(2):259 – 64 https://doi.org/10.2337/dc11-1572
Li, H. et al. The social ecological model of self-management activities in type 2 diabetes: a structural equation modeling analysis. Chinese Journal of Health Statistics. ;31(3):437 – 39. (2014). Available from: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMwMTEyEg96Z3dzdGoyMDE0MDMwMTkaCGQ4cTl5Z2d0
Jing, Y. & Li, Y. Reliability and validity test of Chinese version of chronic disease resources scale used for community patients with type 2 diabetes. Chinese Nursing Research. ;28(6):767 – 69. Available from: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMwMTEyEg9zeGhsenoyMDE0MDYwNjYaCDZtdXd2c3Qx (2014). https://doi.org/10.3969/j.issn.1009-6493.2014.06.065
Wirihana, L. et al. Using Colaizzi’s method of data analysis to explore the experiences of nurse academics teaching on satellite campuses. Nurse Res. 2018. ;25(4):30–34. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=29546965&query_hl=1 (2018). https://doi.org/10.7748/nr.2018.e1516
National Collaborating Centre for Methods and Tools. Quality assessment tool for quantitative studies method resource details National Collaborating Centre for methods and tools: 2018 update. (2018). Retrieved from http://www.nccmt.ca/knowledge-repositories/search/15
Jiang, X. et al. The Mediating Role of Self-Efficacy in Shaping Self-Management Behaviors Among Adults with Type 2 Diabetes. Worldviews Evid Based Nurs. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=30895743&query_hl=1 (2019). 2019;16(2):151 – 60 https://doi.org/10.1111/wvn.12354
Poduval, S., Marston, L., Hamilton, F., Stevenson, F. & Murray, E. Feasibility, Acceptability, and Impact of a Web-Based Structured Education Program for Type 2 Diabetes: Real-World Study. JMIR Diabetes. ;5(1): e15744. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31904580 (2020). https://doi.org/10.2196/15744
Bandura, A. Social Foundations of Thought and Action: a Social Cognitive Theory (Prentice Hall, 1986).
De la Fuente, C. M., Cruz-Cobo, C. & Santi-Cano, M. J. Effectiveness of a primary care nurse delivered educational intervention for patients with type 2 diabetes mellitus in promoting metabolic control and compliance with long-term therapeutic targets: Randomized controlled trial. Int J Nurs Stud. 2020. ; 101:103417. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=31683226&query_hl=1 (2020). https://doi.org/10.1016/j.ijnurstu.2019.103417
Ruissen, M. M. et al. Clinical impact of an integrated e-health system for diabetes self-management support and shared decision making (POWER2DM): a randomized controlled trial. Diabetologia. 2023. ;66(12):2213-25. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=37775611&query_hl=1 (2023). https://doi.org/10.1007/s00125-023-06006-2
Acknowledgements
The authors also thanks for all participants.
Funding
The work was supported by the Project of National Natural Science Foundation of China (82304262, 2023), and the Hainan Provincial Natural Science Foundation of China (820RC631, 2021; 825RC766, 2025).
Author information
Authors and Affiliations
Contributions
S.X., W. T., B. L., and X. J. contributed to the design of the study. S.X. completed the data collection and analysis, and the first draft of the manuscript. B. L. and X. J conceptualized and supervised the study. W. T., Y. L., B. L., and X. J. reviewed the data analysis and revised the manuscript. All authors reviewed and approved the final version for submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical Consideration and consent to participate
The study was approved by the Ethical committee of Hainan Medical University (HYLL-2022-012). Moreover, the research was registered in Chinese Clinical Trial Registry (ChiCTR2400082136, http://www.chictr.org.cn/). All participants involved in this study provided informed consent prior to their participation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
XING, S., TU, W., LIN, Y. et al. A phased online support program improves self-efficacy and reduces distress in type 2 diabetes patients using mixed methods design. Sci Rep 15, 29731 (2025). https://doi.org/10.1038/s41598-025-15786-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15786-z