Abstract
This study explores potential associations among ambient particulate matter (PM) exposure, PM load in alveolar macrophage (AM), and biomarkers collected from 53 healthy, adult, nonsmoking residents of the Iztapalapa and Iztacalco municipalities in Mexico City. Ambient PM2.5 concentrations were estimated using an improved Land Use Regression (LUR) model to approximate PM exposure levels. The PM/carbon loading was quantified by the fraction of AM containing PM (%, %AMPM) and the PM area within the AM (µm2) from BAC cytospin microphotography using CellProfiler cell image analysis software. Concentrations of biomarkers were analyzed in bronchoalveolar lavage fluid (BALF), plasma, and urine. Most AM samples contained PM (median = 62.4%, interquartile range [IQR] = 50.0–73.0%). The median PM area in AM was 1.082 µm2 (IQR = 0.607–1.855 µm2). Participant with low %AMPM (< 33 percentile) showed 8% increase in %AMPM per 10 µg/m3 increments of six-month averaged, LUR-estimated PM2.5 concentrations. The %AMPM had a statistically significant, positive association with plasma von Willebrand Factor (vWF) (p = 0.016) and serum lactase dehydrogenase (LDH) (p = 0.026). These findings suggest that ambient urban PM exposure in Mexico City contributes to PM accumulation in AMs and may trigger systemic inflammation and oxidative stress in healthy young residents.
Similar content being viewed by others
Introduction
Inhalation exposure to air pollution particulate matter (PM) represents a substantial global public health concern because of its numerous adverse health effects, including respiratory, cardiovascular, nervous system, and cancer morbidity and mortality1. Rapid global urbanization has increased exposure to PM from household solid fuel combustion and ambient sources2.
The Mexico City Metropolitan Area (MCMA) is one of the biggest megacities and experiences high levels of air pollution, including from PM3,4. As one of the most populated urban environments, the MCMA also deals with tuberculosis (TB) as a considerable public health concern5.
PM exposure from household (solid fuel) and ambient combustion sources is the top level-3 risk factor ordered by risk-attributable global disability-adjusted life years (DALYs)6. There is strong epidemiological evidence for positive associations between exposures to air pollution PM from household or ambient sources and TB incidence rates as well as TB-associated mortality7,8. Experimental studies have provided biological plausibility of this epidemiological evidence.
PM impairs immune system functions and decreases pathogen response gene expression. Experimental studies from our group5,9,10,11,12,13 and others14,15,16,17,18 have reported PM exposure effects on immune cell responses to Mycobacterium tuberculosis (Mtb) infection. Experimental exposure to urban PM impairs various key immune responses to Mtb infection8 in A549 respiratory epithelial cells, human bronchoalveolar cells (BAC) and peripheral blood mononuclear cells (PBMC)5,9,10,11,12. Our findings also suggest that inhalation-acquired PM load in human alveolar macrophages (AM) influences these cells’ responsiveness to Mtb5.
AM reside in the bronchoalveolar spaces and smaller airways and take up inhaled fine particulate matter (PM2.5; PM with aerodynamic diameter < 2.5 microns). Solid PM cannot be broken down by AM easily19. The AM PM load has been used as a chronic exposure marker20, showing associations with various disease conditions (asthma, diabetes)21 and biomarkers such as low-density lipoprotein (LDL)22. However, associations between PM load in AM and other health responses are not well understood.
The aim of this study was to further explore PM load in AM as a biomarker of PM exposures and associations between this load, estimated ambient exposures, and other biomarkers of oxidative stress and cardiovascular risk. PM load in AM and other biomarker levels were measured from study participants recruited in the MCMA5,13. Associations between the biomarker levels and estimated ambient PM2.5 concentration using land use regression (LUR) were assessed. Evaluation of the PM load in AM together with systemic biomarkers allows linking the physical presence of PM within immune cells with broader immune function alterations and systemic health effects.
Methods
Research and ethics approvals
This observational research study was approved by the scientific and bioethics committees of the Instituto Nacional de Enfermedades Respiratorias “Ismael Cosío Villegas” in Mexico City, Mexico (INER, protocol B22-12), and the Institutional Review Board of Rutgers, The State University of New Jersey (protocol 2012001381) in New Brunswick, NJ. All experimental protocols were approved by the respective committees and conducted in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants for the study protocol.
Study population, location, and sample collection
Candidates were recruited for participation in the U.S. National Institute for Environmental Health Sciences (NIEHS)-funded research project entitled “Air Pollution Particle Effects on Human Antimycobacterial Immunity” at the Universidad Autónoma Metropolitana (UAM) and the Instituto Nacional de Enfermedades Respiratorias (INER), in Mexico City between 2013 and 2018. Study participants (n = 53) were healthy, HIV-seronegative adults (age = 21–60 years), male (n = 25) and female (n = 28) nonsmoking (urine cotinine-negative) students of the UAM and residents (> 6 months) of the Iztapalapa and Iztacalco municipalities in the MCMA (Fig. 1).
For the study of air pollution particle effects on human antimycobacterial immunity5, study participants completed three study visits for consent, a physical exam, and a bronchoalveolar lavage (BAL). At consent, subjects completed questionnaires to obtain demographic information, time-activity information (e.g., commuting in the city, outdoor activities, mode of transportation), household exposures (e.g., housing type, ventilation, cooking fuel, etc.), alcohol use, smoking status, and environmental tobacco smoke exposure. At the physical exam visit, subjects underwent medical history taking, a lung function test, and a chest x-ray. At the third visit, BAL was conducted to collect BAL fluids and bronchoalveolar cells (BAC) and venipuncture to collect peripheral blood mononuclear cells (PBMC). The venipuncture blood sample was used for serum biomarker analysis at the clinic. Spot urine samples were collected at each visit (3 times). BALF, plasma, and urine samples were analyzed for biomarkers, as explained below (2.4. Biomarker Analysis).
Particulate matter load in alveolar macrophages
Cytospin preparations from BAC of the study participants (n = 53) were prepared by centrifugation (800 x g) of 0.2 × 106 BAC onto a glass slide using a cytocentrifuge (Wescor Cytopro 7620 Cytocentrifuge, Wescor INC Logan, UT, USA). Following modified Wright’s staining with Accustain (Sigma Aldrich, St Louis, MO), the nuclear morphology of BAC and proportions of AM, neutrophils and alveolar lymphocytes were characterized on thin-layer cytospin preparations. Cytospin color photographs (Olympus DP71 digital microscope camera, Tokyo, Japan) were obtained by digital bright field microscopy (1000×, Olympus BX51 digital microscope, Tokyo, Japan).
PM load in AM was assessed using the CellProfiler, an open-source cell image analysis tool (CellProfiler 4.0, Broad Institute, Cambridge, MA), which uses modular processing pipelines, allowing users to automate image analysis23. Imported images were separated into three components using hue, saturation, and value channels. The AM object was identified based on size (10 μm diameter) and shape. Form factor (> 0.5, the ratio between the area and the perimeter; a perfectly circular object has a form factor of 1) and eccentricity (< 0.8, the ratio of the distance between the foci of the ellipse and its major axis length, equals 1 for a line segment and 0 for a circle) values were used to select for round-shaped objects. Then, PM objects larger than 0.4 μm were identified within the detected AM objects. The PM object size limit (0.4 μm) was selected based on the maximum resolution of the digital microscope. Finally, estimated variables are the fraction of AM containing PM (%AMPM), absolute PM area within AM (PM area in AM [µm2]), and AM size (µm2). The developed CellProfiler pipeline and example pictures are shown in Supplementary Fig. S1.
Biomarker analysis
BALF (n = 53), plasma (n = 27), and urine (n = 53) samples were shipped to Duke University and stored at −20 °C or −80 °C until laboratory analysis. Based on earlier research by our group24,25, we assessed concentrations of P-selectin, a marker of platelet activation; C reactive protein (CRP), a marker of inflammation; von Willebrand’s Factor (vWF), an index of endothelial dysfunction or damage; and fibrinogen, a blood clotting agent using commercial ELISA kits following manufacturers’ instructions (Sigma-Aldrich, MO, USA). Malondialdehyde (MDA), a marker of lipid damage and oxidative stress, in BAL and urine samples was analyzed using an HPLC-fluorescence detection method following thiobarbituric acid derivatization, as described previously24. Urinary 8-OHdG concentrations, a marker of oxidative stress, were measured with LC-MS/MS (TSQ Quantum Access Max, Thermo Fisher Scientific, MA, USA) after solid phase extraction by Bond Elut-certify cartridge (500 mg, 6 ml, Agilent Technologies, CA, USA), as described previously25. Urinary creatinine concentrations were measured using colorimetric method using commercial kits (Cayman Chemical, MI, USA). Urinary biomarker concentrations were normalized by creatinine concentration.
Land use regression (LUR) model
To stratify the PM exposure levels of the study participants for PM load in AM and biomarker analysis, we developed a LUR model based on the methodology described earlier by our group26 to improve air pollution exposure assessments in MCMA. Earlier LUR models for six criteria air pollutants were developed using the least absolute shrinkage and selection operator (LASSO) method and hourly Google Traffic data. In the current study, the LASSO method with enhanced PM observation data was applied to improve the performance of earlier LUR model using R software (version 4.1.3) with the lmmlasso package27. The current study improved the previous LUR model by adding PM2.5 monitoring data at the participants’ homes (n = 21, red stars in Fig. 1) in addition to the MCMA compliance monitoring sites (n = 37, black dots in Fig. 1).
Ambient PM2.5 concentrations were obtained from the Red Automática de Monitoreo Atmosférico (RAMA) stations over the 2011–2018 period (37 stations across the MCMA). The compliance monitoring stations provide hourly PM2.5 concentrations determined by the beta-attenuation monitors. Quality of the compliance monitoring data was assured by standard operation procedures28. In addition, we obtained daily ambient PM2.5 concentrations on the roof sites of the homes of our MexAir study participants (n = 21). For that purpose, the MexAir sampling suitcase containing air quality monitoring instruments (Supplementary Fig. S2) was placed for a day on the roof of the study participant houses. A Sioutas cascade impactor (SKC, PA, USA) with Teflon filter (0.5 μm, 25 mm, Zefluor supported PTFE, Pall, NY, USA) and SKC Leland Legacy sampling pump (9 LPM, SKC, PA, USA) were used to measure daily PM2.5 concentrations. For gravimetric analysis of the Teflon filters, filters were weighed before and after PM sampling in a clean, temperature (20–23 °C) and humidity (30–40%) controlled weighing facility at the UAM. The sampling pump flow rate was calibrated following a recommended procedure by manufacturer for quality control. Measured daily PM2.5 concentrations across over three years periods on the rooftops of the homes of 21 MexAir study participants were between 6.3 and 86.5 µg/m3 with a moderate correlation with nearby compliance monitoring sites (R2 = 0.38). The daily ambient PM2.5 data provided improved spatial coverage for the LUR model around the focused area (Fig. 1).
Other LUR model variables were collected from the RAMA, the meteorology and solar radiation monitoring network (Red de Meteorología y Radiación Solar; REDMET, n = 21) and the atmospheric deposition monitoring network (Red de Depósito Atmosférico, REDDA, n = 16) stations for hourly temperature (T), relative humidity (RH), and wind speed (WS). Google Traffic data was used for typical hourly traffic density information (TD). Land use information and elevation were downloaded from the United States Geological Survey (USGS). Traffic density, land use, and elevation variables within 500 m diameter circular buffer around the PM2.5 monitoring locations (i.e., 37 RAMA and 21 MexAir participant home sites) were selected. All hourly variables were averaged to daily time resolution to develop LUR model.
Statistical analysis
Descriptive statistics for participant demographics, PM load in AM markers, PM2.5 exposures using our LUR model, and biomarker concentrations for BALF, plasma, and urine were estimated. Chi-square and t-tests were used to compare the measurements between low, medium, and high AMPM load groups. Associations between %AMPM, plasma biomarkers, and estimated average PM2.5 concentrations over different periods (1 day to 6 months) were analyzed using linear regression. Regression analyses were also conducted to study the relationship between short-term PM concentrations (1–7 days before urine sample collection) and urinary oxidative stress markers.
Results
Study participants
The characteristics of the 53 study participants (25 male and 28 female, age range: 21–60 years) are described in Table 1. Mean age and body mass index (BMI) were 29.6 years and 26.2 weight [Kg]/height [m2], respectively. 92% of the participants had received a college or higher education. 60% of the participants were college students at the time of the study. 26% of the participants’ houses had mechanical ventilation systems (e.g., mechanical range hood). Eighteen participants indicated that they had smokers in their households.
PM load in AM and biomarker levels
PM load in AM was estimated in 53 participant samples (Fig. 2) using the automated image analysis method. Overall, a median of 183 (interquartile range [IQR] 134–263) AM cells were identified on each participant’s cytospin image (61–71 images per participant). PM was detected in 62.4% (50.0–73.0%) of AM (%AMPM), and the median and interquartile range of the PM area in AM was 1.082 µm2 (0.607–1.855 µm2).
Brightfield microscopy (magnification x 1000) of alveolar macrophages (AM) with particulate matter (PM) inclusions. (a) Overview of a typical BAC cytospin preparation with AM. (b) and (c) Magnified AM details from panel (a). Perimeters of AM objects are shown as light blue solid lines. Perimeters of PM objects are shown with red lines.
Table 2 shows PM load in AM results, mean LUR-estimated ambient PM2.5 concentrations at different periods prior to the BAL date and basic demographics. PM load groups were categorized into tertiles using %AMPM estimates: low (n = 18, < 33 percentile), medium (n = 17, 33–66 percentile), and high (n = 18, > 66 percentile). Participants with higher %AMPM had larger PM areas in AM. In the lowest tertile, 46.2% of AM had PM with a median PM area of 0.427 µm2, while in the highest tertile 77.7% of AM contained PM with a median area of 2.274 µm2 (t-test, p = 0.00). PM2.5 exposure estimated using the LUR model on BAL date (0-day) showed slightly higher concentrations in the AM with high PM load group than in the low PM load group (t-tests, p > 0.33). Age, BMI, and AM size were within similar ranges in the different PM load groups. The medium PM load group included more female participants (70.5% female) than other groups (Chi-Square, p = 0.49).
Correlation analysis results between the PM load in AM markers and bronchoalveolar lavage fluid (BALF), plasma, and serum biomarker levels are shown in Fig. 3. von Willebrand factor (vWF, correlation coefficient [ρ] = 0.42, p = 0.002), Lactate dehydrogenase (LDH, ρ = 0.19, p = 0.045), fibrinogen (ρ = 0.19, p = 0.188), and C-Reactive Protein (CRP, ρ = 0.14, p = 0.336) showed weak to moderate positive correlations with %AMPM (ρ = 0.14–0.42). PM area with AM showed weaker positive correlations with vWF, LDH, fibrinogen, and CRP than %AMPM (ρ = 0.13–0.28). The two biomarkers, vWF and LDH, showed a high correlation with PM load in AM markers were known to indicate inflammation and cardiovascular disease29,30. Other markers correlated with PM load in AM markers including fibrinogen, CRP and serum glutamic pyruvic transaminase (TGP) were also31,32,33. Interestingly, AM size were negatively correlation with the inflammation and cardiovascular disease markers (i.e., fibrinogen, vWF, and CRP), but the mechanism is unknown.
Correlation matrix between PM load in AM and other biomarkers measured in this study. %AMPM: Fraction of AM containing PM; PM area in AM: absolute PM area within AM; AM size: absolute size of AM; BALF: bronchoalveolar lavage fluid; MDAf: free malondialdehyde level; P-selectin: plasma type-1 Transmembrane Protein (CD62P); CRP: C-Reactive Protein; vWF: von Willebrand factor level; PT: Prothrombin time; PTT: Partial thromboplastin time; TGO: Serum glutamic oxaloacetic transaminase; TGP: Serum glutamic pyruvic transaminase; LDH: Lactase dehydrogenase.
Associations between ambient PM2.5 concentrations and PM load in AM
This study refined the LUR model developed in our previous study26. The current model included additional RAMA compliance monitoring stations and daily ambient PM2.5 monitoring data measured on the rooftops of the homes of 21 MexAir study participants. Compared to the previous study, the LUR model for this study improved its performance from R2 = 0.49 to R2 = 0.81 (Supplemental Figure S3, Table S1). The addition of the data from the rooftops of the homes of 21 MexAir study participants slightly improved overall fit of the LUR model (R2 from 0.79 to 0.81) by capturing spatial variation of PM sources and distributions. Mean ambient PM2.5 concentrations were estimated using the refined LUR model to measure its association with PM load in AM.
Associations between %AMPM and mean LUR-estimated ambient PM2.5 concentrations (µg/m3) are shown in Fig. 4. Considering the lifetime of AM, we estimated the PM2.5 concentrations on BAL dates (0 days [0D]) and their averages at 7-day (7D), 1-month (1 M), 3-months (3 M), and up to 6-months (6 M) prior to the BAL date34. Medium and high PM loads in AM groups did not show a significant association between %AMPM and estimated ambient PM2.5 concentrations. Low PM load in AM group with less than 1-month PM2.5 averaging time did not show significant associations (p = 0.14–0.88). Averaged PM2.5 concentrations over longer than a 3-month period, however, showed a significant association with %AMPM (p < 0.005). Increments of 10 µg/m3 of 6-month averaged PM2.5 concentrations in the low PM load group were associated with increased the %AMPM by 8.06% (p = 0.000, 95% confidence interval = 6.78–9.36%).
Associations between PM load in AM and biomarkers
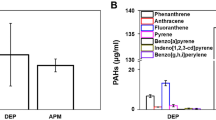
Figure 5 shows associations between %AMPM and vWF [von Willebrand factor, marker of inflammation-related thrombosis35, µg/ml], LDH (U/L), fibrinogen (µg/ml), and CRP (C-Reactive Protein, µg/ml) concentrations from all participants. The three plasma and a serum biomarker showed positive associations with %AMPM. The vWF (p = 0.016) and LDH (p = 0.026) concentrations showed a statistically significant relationship with %AMPM. BALF Malondialdehyde and plasma p-selectin showed negative associations with the levels of %AMPM (Table 3). Other biomarker analysis results are tabulated in Supplementary Table S2. Two urinary oxidative stress markers (Malondialdehyde and 8OHdG) didn’t show clear trends with AMPM load levels. However, %AMPM load levels altered the associations between PM2.5 and urinary oxidative stress markers (Supplementary Table S3).
Associations between the fraction of PM containing AM (%AMPM [%]) and plasma and serum biomarker levels, (a) plasma vWF (µg/ml), (b) serum LDH (U/L), (c) plasma fibrinogen (µg/ml), and (d) plasma CRP (µg/ml) concentrations. The blue lines and shades indicate the regression lines and confidence intervals.
Discussion
Household and ambient PM exposure is known to cause a multitude of adverse health outcomes1. Identifying biomarkers of PM exposures and their roles within the biological processes of the exposed persons is a topic of great research effort. This study explored correlations between ambient PM exposures and PM load in AM and the consequences of PM accumulation in human AM on various biomarkers. To our knowledge, this study is the first to explore associations between PM load in AM, exposure to LUR-estimated ambient PM2.5 exposure levels, and biomarkers in the BALF, plasma, and urine samples of healthy adult residents of the MCMA. Assessment of the PM load in alveolar macrophages (AM) provides a direct, cellular-level indicator of chronic PM exposure in the lower respiratory tract. This enables quantification of PM burden within AM and facilitates investigation of the biological mechanisms underlying air pollution-related immune dysfunction and disease risk. Unlike traditional immune cell function biomarkers, which often lack exposure specificity, PM load in AM serves as a highly representative and specific biomarker of particulate exposure.
In addition, we obtained daily ambient PM2.5 concentrations on the roof sites of the homes of our MexAir study participants (n = 21). Being able to add additional PM level data points obtained from the roof sites of our study participant’s residences, we were able to develop a further refined LUR model that dramatically improved compared with its earlier usage in performance26. The model accuracy was improved from R2 = 0.41 to R2 = 0.81 (see Supplementary Table S1). This study, also for the first time, demonstrates utilization of the CellProfiler image analysis software for automatic assessment of PM load in human AM.
PM2.5 exposure was assessed by averaging PM2.5 concentrations for 6-month period prior to each study participant’s BAL dates. The 6-month averaged PM2.5 concentrations were positively correlated with %AMPM in the low PM load group (p = 0.000). Our findings are supported by a study of type 1 or 2 diabetic patients in Leuven, Belgium, in which a positive correlation was found between modeled 6-month average PM10 exposure and PM area in AM22. In another study in Leicester, United Kingdom, children (n = 22, 3 months to 16 years) without respiratory symptoms who resided near primary roads with dense traffic had higher %AMPM (10%) than those who lived on quiet residential streets (%AMPM = 3%)36. In other studies, indoor biomass burning increased PM load in AM37,38. In a study assessing the longevity of PM load in AM, AMPM clearance half-lives were 54 days on average in persons who had moved from a highly polluted location (mean annual PM10 108 µg/m3) to Leuven, Belgium (mean annual PM10 23 µg/m3)39. In that study, persons with high AMPM load (90th percentile) needed a longer time (mean 116 days) to clear PM deposited in AM.
Our findings suggest that high ambient PM2.5 levels in the MCMA underlie the various degrees of PM loads in AM. Interestingly, in the medium and high PM load groups no associations between the estimated ambient PM2.5 concentrations and %AMPM were observed. Lacking correlation between PM exposure and PM load in the medium and high PM load groups may result from PM exposure saturation effects, or different AM ages and maturity stages. To the best of our knowledge, the processes of PM accumulation in and clearance from AM are still poorly understood.
Previous studies have used absolute PM area within the AM to assess PM load in AM22,38,39,40,41. Our findings indicate that the %AMPM is a useful biological marker of long-term PM exposure and likely related to adverse health impacts. The current study showed a stronger correlation between %AMPM and plasma biomarkers than absolute PM size in AM. We observed a significant positive correlation between %AMPM and plasma inflammation biomarker vWF (p = 0.016) and serum cardiovascular marker LDH (p = 0.026). %AMPM showed trends toward positive associations with CRP (p = 0.182) and fibrinogen (p = 0.405). These observations provide biological plausibility toward a recent EPA report that stated a causal relationship between PM2.5 exposure and cardiovascular disease1. The %AMPM was negatively correlated with P-selectin, and other markers were positively correlated.
This study observed that %AMPM positively correlated with plasma vWF levels (p = 0.016). In other studies, vWF and fibrinogen levels were associated with short-term air pollution exposures. Short-term PM2.5 exposure (< 7 days) significantly increased plasma vWF by 0.41% (95%CI: 0.11–0.71) per 10 µg/m3 increments42. In a murine study, sub-chronic exposure (25–26 days) to tunnel air pollutants increased vWF levels43. Plasma vWF is a predictor of adverse cardiac events and is closely related to systemic inflammation and cardiovascular disease30,35,44. In addition to vWF, our data also showed a positive relationship between %AMPM and serum LDH (p = 0.026). LDH is known marker of cardiovascular disease29. Plasma LDH levels shown to be higher in diabetes patients than the general public45. A previous study showed positive correlations between PM load in AM and diabetes20.
In our study, %AMPM was not correlated with plasma fibrinogen levels (p = 0.405). In other studies, short-term PM exposures (< 7 days) showed strong positive associations with fibrinogen levels46,47, while long-term exposures (1 year) to air pollutants did not affect fibrinogen levels46,48,49. Fibrinogen is a known marker of cardiovascular disease50. This study observed positive correlations between %AMPM and plasma CRP levels (p = 0.182). Others showed that plasma CRP levels were significantly correlated with long-term PM exposures49,51. CRP is related to tissue damage, systemic inflammation, respiratory (e.g., COPD)52, and cardiovascular disease53.
In contrast to vWF, fibrinogen and CRP, which were positively correlated with %AMPM in this study, were negatively correlated with %AMPM and P-selectin. The impact of air pollution exposures on P-selectin levels is not well understood. P-selectin is a cellular adhesion molecule strongly associated with cardiovascular disease (CVD)54,55 development and varies by age group55. Further study will be needed to understand better the relationships between air pollution exposure, P-selectin levels, and CVD risk.
The findings of this study indicate that %AMPM is more strongly correlated with biomarkers than PM area in AM. This is consistent with our earlier findings in human BAC and PBMC, in which BAC with greater %AMPM more strongly suppressed IL-1β, a key antimycobacterial cytokine, than BAC with lower %AMPM5. Small amounts of PM within AM were shown to alter AM functions such as antigen presentation56. As shown before by our group5, the PM load of individual AM can vary widely both within individual BAC samples of study participants and between study participants.
Our findings provide new insights into short-term (< 1 week) PM exposure effects in humans. Urinary biomarkers are indicators of shorter-term environmental exposures that include PM24,57. Here, we observed increasing significance between PM exposures and urinary oxidative stress markers with higher %AMPM. Even though the relationships were not significant, the results support our earlier findings that %AMPM results in the suppression of key cytokine response to Mtb for the high AMPM load group5.
A limitation of the current study is the relatively small participant group and its limited demographic diversity from a single urban municipality with its specific PM exposure environment. Most study participants were students at the UAM with similar air pollution exposure (i.e., urban PM), behaviors, lifestyles, and mobility radii. The ‘relative homogeneity’ of the study population may have impacted our findings. Previous studies have shown that traffic-related PM exposure is positively associated with cardiovascular events (i.e., increased CRP and vWF) in healthy adults58,59, whereas the association between wildfire PM exposure and cardiovascular disease remains inconclusive60. Given the urban source of PM examined in this study, transferability of our results to varied PM sources and exposures in rural locations may be limited. Indeed, our prior research showed that PM effects on immune function vary by particle size and season, with larger particles and certain seasonal PM samples inducing greater cytotoxicity and impaired immune responses to Mtb10. These findings highlight the importance of PM source and composition in shaping biological responses and exposure-related health risks. Further, the cytospin images analyzed here were prepared using standardized processes that may miss PM spots in AM due to the limitations of two-dimensional images. AM and PM size could have been altered during cytospin preparations.
Regardless of these limitations, this study observed significant correlations between long-term, low-level urban PM2.5 exposures and %AMPM, as well as between %AMPM and biomarkers such as vWF and LDH. Interestingly, despite reports of similar behavioral patterns among participants (Supplemental Table S4), their alveolar macrophages often carried widely varying PM loads. Although PM load measurement in AM is not yet widely feasible in large-scale studies due to sampling constraints, it may offer unique advantages, including direct quantification of chronic PM exposure at the cellular level in the lower respiratory tract. Our previous study demonstrated that PM-induced impairments in AM function compromise innate immune responses to respiratory pathogens and revealed a segregation in constitutive cytokine production between individuals with high versus low PM burdens. These findings suggest a potential dose–response relationship and support the use of PM load as a specific and biologically relevant biomarker of exposure.
Future research may further identify the mechanisms by which PM exposure and PM load in AM induce adverse health effects. Such studies may also investigate the role of chemical and physical composition differences of PM from different sources (e.g., urban, traffic vs. biomass burning) in the various cellular responses and health outcomes of interest. Future studies could also consider using three-dimensional (3D) cell image analysis61. The 3D cell imaging techniques with automated cell image analysis processes used in this study provide opportunity for further research studies of PM effects on cellular processes. Studies of dose-response relationships between PM load and AM function, as well as AM phenotypes are needed to follow up on our observations.
Conclusion
This study explored associations between PM load in AM, PM2.5 exposure, and biomarkers among residents of a large urban area (MCMA). The results provide novel insights indicating that urban PM deposited in AM might have altered physiological functions of AM, such as signaling molecule production (e.g., inflammatory cytokines), causing increased systemic inflammation and cardiovascular disease risk. The study results also suggest that even low-level urban PM exposures lead to uptake of AM by PM, which might increase inflammatory and cardiovascular disease risks. Our findings emphasize the importance of World Health Organization (WHO)’s new air quality recommendation to work towards an annual ambient PM2.5 concentration of 5 ug/m362,63 to protect public health.
%AMPM: Fraction of AM containing PM; PM area in AM: absolute PM area within AM; Estimated ambient PM2.5: ambient PM2.5 concentrations were estimated for the date of BAL, 3- and 6-month averages prior to BAL date; BMI: Body Mass Index; a, b: statistical significance at α = 0.05 level.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
US EPA., Supplement to the 2019 Integrated Science Assessment for Particulate Matter (Final Report, 2022). U.S. Environmental Protection Agency, Washington, DC. EPA/635/R-22/028. (2022).
Mukherjee, A. & Agrawal, M. World air particulate matter: sources, distribution and health effects. Environ. Chem. Lett. 15, 283–309 (2017).
Molina, M. J. & Molina, L. T. Megacities and atmospheric pollution. J. Air Waste Manag. Assoc. 54 (6), 644–680 (2004).
Molina, L. T., Retama, A. & Zavala, M. Diagnosis of Current Knowledge of the Scientific Bases for Air Quality Management in the Megalopolis (Molina Center for Strategic Studies in Energy and the Environment. Boston, 2023).
Torres, M. et al. Urban airborne particle exposure impairs human lung and blood Mycobacterium tuberculosis immunity. Thorax 74 (7), 675–683 (2019).
Brauer, M. et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet 403 (10440), 2162–2203 (2024).
Popovic, I. et al. A systematic literature review and critical appraisal of epidemiological studies on outdoor air pollution and tuberculosis outcomes. Environ. Res. 170, 33–45 (2019).
Dimala, C. A. & Kadia, B. M. A systematic review and meta-analysis on the association between ambient air pollution and pulmonary tuberculosis. Sci. Rep. 12 (1), 11282 (2022).
Ibironke, O. et al. Urban air pollution particulates suppress human T-cell responses to Mycobacterium tuberculosis. Int. J. Environ. Res. Public Health. 16 (21), 4112 (2019).
Sarkar, S. et al. Season and size of urban particulate matter differentially affect cytotoxicity and human immune responses to Mycobacterium tuberculosis. PloS One. 14 (7), e0219122 (2019).
Rivas-Santiago, C. E. et al. Air Pollution Particulate Matter Alters Antimycobacterial Respiratory Epithelial Innate Immunity. Infection and Immunity, : p. IAI. 03018-14. (2015).
Sarkar, S. et al. Suppression of the NF-κB pathway by diesel exhaust particles impairs human antimycobacterial immunity. J. Immunol. 188 (6), 2778–2793 (2012).
Sarkar, S. et al. Exposure to urban air pollution particulate matter modifies Th1/Th2 Mtb immunity in the human lung. Am. J. Respir. Cell Mol. Biol. 72 (2), 222–225 (2025).
Glencross, D. A. et al. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 151, 56–68 (2020).
Paarwater, B. A. et al. Inhaled particulate matter affects immune responsiveness of human lung phagocytes to mycobacteria. Am. J. Physiology-Lung Cell. Mol. Physiol., 321(3): p. (2021). L566-L575.
Rylance, J. et al. Household air pollution causes dose-dependent inflammation and altered phagocytosis in human macrophages. Am. J. Respir. Cell Mol. Biol. 52 (5), 584–593 (2015).
Miyata, R. & van Eeden, S. F. The innate and adaptive immune response induced by alveolar macrophages exposed to ambient particulate matter. Toxicol. Appl. Pharmcol. 257 (2), 209–226 (2011).
Sada-Ovalle, I. et al. Macrophage exposure to polycyclic aromatic hydrocarbons from wood smoke reduces the ability to control growth of Mycobacterium tuberculosis. Front. Med. 5, 309 (2018).
Moller, W. et al. Mucociliary and long-term particle clearance in the airways of healthy nonsmoker subjects. J. Appl. Physiol. 97 (6), 2200–2206 (2004).
Bai, Y. et al. Carbon loading in airway macrophages as a biomarker for individual exposure to particulate matter air pollution—A critical review. Environ. Int. 74, 32–41 (2015).
Brugha, R. E. et al. Carbon in airway macrophages from children with asthma. Thorax p. thoraxjnl-2013-204734 (2014).
Jacobs, L. et al. Traffic air pollution and oxidized LDL. PloS One. 6 (1), e16200 (2011).
Stirling, D. R. et al. CellProfiler 4: improvements in speed, utility and usability. BMC Bioinform. 22, 1–11 (2021).
Cui, X. et al. Relationship between free and total malondialdehyde, a well-established marker of oxidative stress, in various types of human biospecimens. J. Thorac. Disease. 10 (5), 3088 (2018).
Day, D. B. et al. Association of Ozone exposure with cardiorespiratory pathophysiologic mechanisms in healthy adults. JAMA Intern. Med. 177 (9), 1344–1353 (2017).
Son, Y. et al. Land use regression models to assess air pollution exposure in Mexico City using finer Spatial and Temporal input parameters. Sci. Total Environ. 639, 40–48 (2018).
Schelldorfer, J. et al. Estimation for High-Dimensional linear Mixed‐Effects models using ℓ1‐Penalization. Scand. J. Stat. 38 (2), 197–214 (2011).
SIMAT. Mexico City Atmospheric Monitoring System (Sistema de Monitoreo Atmosférico). (2018).
Zhu, W. et al. Serum level of lactate dehydrogenase is associated with cardiovascular disease risk as determined by the Framingham risk score and arterial stiffness in a health-examined population in China. Int. J. Gen. Med. 15, 11–17 (2022).
Roldán, V. et al. Plasma von Willebrand factor levels are an independent risk factor for adverse events including mortality and major bleeding in anticoagulated atrial fibrillation patients. J. Am. Coll. Cardiol. 57 (25), 2496–2504 (2011).
Wroblewski, F. & Ladue, J. S. Serum glutamic pyruvic transaminase in cardiac and hepatic disease. Proceedings of the Society for Experimental Biology and Medicine, 91(4): pp. 569–571. (1956).
Ernst, E. & Resch, K. L. Fibrinogen as a cardiovascular risk factor: a meta-analysis and review of the literature. Ann. Intern. Med. 118 (12), 956–963 (1993).
Pepys, M. B. & Hirschfield, G. M. C-reactive protein: a critical update. J. Clin. Investig. 111 (12), 1805–1812 (2003).
Parihar, A., Eubank, T. D. & Doseff, A. I. Monocytes and macrophages regulate immunity through dynamic networks of survival and cell death. J. Innate Immun. 2 (3), 204–215 (2010).
Kawecki, C., Lenting, P. & Denis, C. von Willebrand factor and inflammation. Journal of Thrombosis and Haemostasis, 15(7): pp. 1285–1294. (2017).
Bunn, H. et al. Ultrafine particles in alveolar macrophages from normal children. Thorax 56 (12), 932–934 (2001).
Fullerton, D. G. et al. Domestic smoke exposure is associated with alveolar macrophage particulate load. Tropical Med. Int. Health. 14 (3), 349–354 (2009).
Whitehouse, A. L. et al. Use of cleaner-burning biomass stoves and airway macrophage black carbon in Malawian women. Sci. Total Environ. 635, 405–411 (2018).
Bai, Y. et al. Carbon load in airway macrophages as a biomarker of exposure to particulate air pollution; a longitudinal study of an international panel. Part. Fibre Toxicol. 15 (1), 1–10 (2018).
Steenhof, M. et al. In vitro toxicity of particulate matter (PM) collected at different sites in the Netherlands is associated with PM composition, size fraction and oxidative potential - the RAPTES project. Part. Fibre Toxicol. 8, 1–15 (2011).
Yin, G. et al. Evaluating carbon content in airway macrophages as a biomarker of personal exposure to fine particulate matter and its acute respiratory effects. Chemosphere 283, 131179 (2021).
Liang, Q. et al. Short-term PM2. 5 exposure and Circulating von Willebrand factor level: a meta-analysis. Sci. Total Environ. 737, 140180 (2020).
Emmerechts, J. et al. Thrombogenic changes in young and old mice upon subchronic exposure to air pollution in an urban roadside tunnel. Thromb. Haemost. 108 (10), 756–768 (2012).
Spiel, A. O., Gilbert, J. C. & Jilma, B. Von Willebrand factor in cardiovascular disease: focus on acute coronary syndromes. Circulation 117 (11), 1449–1459 (2008).
Dmour, H. H. et al. Assessment of lactate dehydrogenase levels among diabetic patients treated in the outpatient clinics at King Hussein medical center, Royal medical services, Jordan. Med. Archives. 74 (5), 384 (2020).
Lee, H. et al. Short-and long-term exposure to ambient air pollution and Circulating biomarkers of inflammation in non-smokers: A hospital-based cohort study in South Korea. Environ. Int. 119, 264–273 (2018).
Hildebrandt, K. et al. Short-term effects of air pollution: a panel study of blood markers in patients with chronic pulmonary disease. Part. Fibre Toxicol. 6, 1–13 (2009).
Viehmann, A. et al. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup. Environ. Med. 72 (9), 656–663 (2015).
Hoffmann, B. et al. Chronic residential exposure to particulate matter air pollution and systemic inflammatory markers. Environ. Health Perspect. 117 (8), 1302–1308 (2009).
Collaboration, F. S. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. Jama 294 (14), 1799–1809 (2005).
Pilz, V. et al. C-reactive protein (CRP) and long-term air pollution with a focus on ultrafine particles. Int. J. Hyg. Environ Health. 221 (3), 510–518 (2018).
Karadag, F. et al. The value of C-reactive protein as a marker of systemic inflammation in stable chronic obstructive pulmonary disease. Eur. J. Intern. Med. 19 (2), 104–108 (2008).
De Ferranti, S. & Rifai, N. C-reactive protein and cardiovascular disease: a review of risk prediction and interventions. Clin. Chim. Acta. 317 (1–2), 1–15 (2002).
Bielinski, S. J. et al. P-selectin and subclinical and clinical atherosclerosis: the Multi-Ethnic study of atherosclerosis (MESA). Atherosclerosis 240 (1), 3–9 (2015).
Barbaux, S. C. et al. Association between P-selectin gene polymorphisms and soluble P-selectin levels and their relation to coronary artery disease. Thromb. Vascular Biology. 21 (10), 1668–1673 (2001). Arteriosclerosis.
Shapouri-Moghaddam, A. et al. Macrophage plasticity, polarization, and function in health and disease. J. Cell. Physiol. 233 (9), 6425–6440 (2018).
Calderon-Garciduenas, L. et al. 8-hydroxy-2 ‘-deoxyguanosine, a major mutagenic oxidative DNA lesion, and DNA strand breaks in nasal respiratory epithelium of children exposed to urban pollution. Environ. Health Perspect. 107 (6), 469–474 (1999).
Riediker, M. Particulate matter exposure in cars is associated with cardiovascular effects in healthy young men. Am. J. Respir. Crit Care Med. 169 (8), 934–940 (2004).
Riediker, M. Cardiovascular effects in patrol officers are associated with fine particulate matter from brake wear and engine emissions. Part. Fibre Toxicol. 1 (1), 2 (2004).
Wang, Y. Associations of wildfire-derived particulate matter with hospitalization, emergency department visits and mortality: A systematic review and meta-analysis. Environ. Res. 273, 121221 (2025).
Jiang, M. et al. Application of artificial intelligence in quantifying lung deposition dose of black carbon in people with exposure to ambient combustion particles. J. Expo. Sci. Environ. Epidemiol. 34 (3), 1–9 (2023).
Chen, J. & Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: a systematic review and meta-analysis. Environ. Int. 143, 105974 (2020).
Velasco, R. P. & Jarosińska, D. Update of the WHO global air quality guidelines: systematic reviews–An introduction. Environ. Int. 170, 107556 (2022).
Acknowledgements
We thank all study participants for their contribution to this work. We would also like to thank the leadership of the Universidad Autónoma Metropolitana (UAM) and of the Instituto Nacional de Enfermedades Respiratorias (INER) for their support of research work.
Author information
Authors and Affiliations
Contributions
Son, Y.: Data curation, Formal analysis, Methodology, Investigation, Validation, Visualization, Writing – original draft, review, & editing; Carranza, C., Subramhanya, S., Torres, M., and Zhang, J.: Data curation, Formal analysis, Methodology, Investigation, Validation, Writing – review & editing; Gardner, C., Jones, L., Meng, Q., Osornio-Vargas, A., and Orman-Strickland, P.: Investigation, Validation, Writing – review & editing, O’Neill, M.: Investigation, Validation; Black, C.: Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Writing – review & editing; and Schwander, S.: Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Writing – original draft, review, & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Son, Y., Carranza, C., Subramhanya, S. et al. Correlations between human alveolar macrophage particulate matter load, air pollution particulate matter levels, and systemic inflammation markers in Mexico City. Sci Rep 15, 29903 (2025). https://doi.org/10.1038/s41598-025-15878-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-15878-w