Abstract
Lost to follow-up (LTFU), defined as interrupting anti-TB treatment for ≥ 8 consecutive weeks or missing anti-retroviral therapy (ART) appointments for > 90 days, is a barrier to TB/HIV coinfection management. Poor treatment adherence, a driver of multidrug resistance in TB/HIV, poses critical challenges to case management. Overestimating effect sizes when considering mutually exclusive events, like LTFU from ART and anti-TB treatment, can occur if sources of error are not properly accounted for in competing events. However, studies estimating the effect sizes of predictors of time to LTFU using competing risk analysis are scarce. Hence, this study aimed to investigate the predictors of time to LTFU among adults with TB/HIV coinfection. We conducted a multicenter facility-based retrospective follow-up study. We randomly selected 471 TB/HIV coinfected adults. Data were extracted using standardised checklists. The LTFUs from ART and anti-TB treatment were events of interest and competing events, respectively, and others were censored. The data were entered into Epi data and then exported to Stata and Rstudio. Statistical differences were tested by Gray’s test, and the cumulative incidence of each event was estimated by a cumulative incidence function. Bivariable and multivariable competing risk regression models were fitted, and variables with p values < 0.05 were considered significant predictors. Incidence rates of LTFU for ART and TB treatment were 3.90 and 19.17 per 1000 person-months of observation (PMOs), respectively. The predictors of ART LTFU included rural residence (adjusted subdistribution hazard ratio (SDHR): 3.39), WHO stage IV (SDHR: 2.88), haemoglobin < 11 g/dl (SDHR: 3.56), and opportunistic infections (OIs) (SDHR: 3.65). For TB treatment LTFU, significant predictors were rural residence (SDHR: 0.11), divorced (SDHR: 2.81), widowed (SDHR: 5.92), BMI < 18.5 (SDHR: 0.41), ambulatory functional status (SDHR: 2.59), adverse drug effects (SDHR: 2.87), and poor ART adherence (SDHR: 5.72). Considering errors in competing events, ART LTFU was higher among rural dwellers, individuals with advanced disease, nutritional deficits, or adverse drug effects requiring prioritised, multifaceted interventions. Targeted strategies such as intensified monitoring, adherence counselling, nutritional support, proactive management of drug-related side effects, marital instability, OIs and poor ART adherence should be integrated into the existing ART/TB program to mitigate LTFU.
Similar content being viewed by others
Introduction
The coinfection of tuberculosis (TB) and human immunodeficiency virus (HIV) poses significant challenges in treatment and case management1,2, with coinfected adults facing higher risks of poor outcomes compared to single infections3. Contributing factors include drug interactions between anti-TB and antiretroviral therapy (ART) that reduce efficacy, increase toxicity, and exacerbate inflammatory syndromes4,5. To address these challenges, the World Health Organization (WHO)recommends careful medication selection, dosing adjustments6,7, and integrated strategies such as patient education, counselling, and comprehensive support services8, alongside close monitoring and collaboration between HIV and TB clinicians to ensure coordinated care9. Treatment adherence remains critical but is complicated by polypharmacy, overlapping side effects, and drug-drug interactions10. Despite global successes, such as an estimated 53 million deaths averted through treatment, significant gaps in care and prevention persist, particularly in high-burden regions like Ethiopia, which reports a TB incidence rate of 140/100,000 people11.
Lost to follow-up (LTFU)rates vary widely across regions: ART LTFU ranges from 4.5 to 42% in Sub-Saharan Africa (SSA)12,13,14,15,16,17,18,19,20,21,22, 18.2% in Latin America23, and 4.5–10.22/1000 person-Years of observation [PYOs] in Ethiopia24,25,26,27,28, while TB treatment LTFU spans 3.6% in Namibia29 to 21.2% in Ethiopia30. Key predictors of LTFU include sociodemographic factors (e.g., rural residence, male sex, divorced/widowed marital status)21,25, clinical indicators [e.g., advanced HIV disease18,31, CD4 count < 200 cells/µL, anaemia (haemoglobin ≤ 11.0 g/dl)and OIs)18,25,32, and systemic barriers (e.g., poor adherence, adverse drug reactions, food insecurity, and fragmented TB/HIV services)33,34,35. Paradoxically, adverse drug events may reduce LTFU risk by necessitating closer clinical oversight25.
Analysing competing risk data, where patients may experience mutually exclusive outcomes such as LTFU from ART or TB treatment, is complex and susceptible to error. Competing risk analysis is essential to avoid bias and overestimation of predictor effects on time to LTFU from ART or TB treatment. These models appropriately account for mutually exclusive events, where the occurrence of one event precludes others36. For instance, a patient who becomes LTFU from ART cannot subsequently become LTFU from TB treatment.
Unlike the Kaplan-Meier method, which treats other events as censored and may thus lead to effect estimates, competing risk models, specifically subdistribution hazard regression models (SDHRMs), utilise the subdistribution hazard function (SDHF) and estimate the cumulative incidence function for each event17. This approach provides more accurate estimates of predictor effects related to time to LTFU, aiding in clinical and policy decisions37,38. Many prior studies have employed the Kaplan-Meier method, which neglects competing risks and can lead to biased conclusions. The use of SDHRMs is crucial to mitigate such biases and improve prognostic modelling17.
This study investigated predictors of time to LTFU among adults with TB/HIV coinfection in Ethiopia using a competing risk framework. In addition to previously studied predictors, it incorporated novel variables, such as occupation, viral load, pain assessment and management, and fluconazole preventive therapy (FPT), which were often omitted in earlier survival analyses.
Methods
Study design, study area and period
This retrospective follow-up study utilised data from multiple health facilities in Bahir Dar, Ethiopia, spanning 28 June 2017 to 27 June 2022. Bahir Dar is the capital of the Amhara National Regional State, located 565 km northwest of Addis Ababa. According to the 2022 population projection by the Ethiopian Statistical Agency (ESA)39, the city has a population of 422,850, including 215,654 females. The study area comprises 13 governmental health facilities (3 hospitals, 10 health centres) and 4 private hospitals, alongside over 20 private clinics. Among these, 9 health centres and 3 public hospitals operate as ART centres. Five health centres and two public hospitals were selected for inclusion based on their initiation of ART services by or before 28 June 2017. These facilities provide primary, secondary, and tertiary care, including specialised HIV/AIDS and TB management and treatment services. The study sites serve a diverse population within the city and outside the city administration, such as West Gojjam, East Gojjam, Awi, South Gondar, and Central Gondar zones, as well as neighbouring regions.
Source, study population, and eligibility criteria
The source population comprised all adult patients (aged 15 years or older) with TB/HIV coinfection receiving both anti-TB treatment and ART follow-up at TB/ART clinics within public health facilities in Bahir Dar City. The study population included adults (≥ 15 years) with TB/HIV coinfection who underwent treatment at selected TB/HIV clinics in these facilities between June 28, 2017, and June 27, 2022. The study unit consisted of individual patient follow-up records (folders). Inclusion criteria required patients to be aged ≥ 15 years, confirmed TB/HIV-coinfected, and receiving both ART and anti-TB treatment at the selected facilities during the study period. Patients were excluded if they had incomplete medical records, undocumented treatment outcomes (e.g., unknown transfer status or final disposition), and concurrent ART and TB LTFU outcomes. Concurrent ART and TB LTFU outcomes are excluded to avoid the potential overlapping of events of interest (ART LTFU) and competing events (TB LTFU).
Study variables
Outcomes
This study evaluated time to LTFU from ART and anti-TB treatment as competing outcome variables. LTFU from ART was defined as missing clinic follow-ups for ≥ 3 consecutive months, while LTFU from anti-TB treatment was defined as missing treatment for ≥ 8 consecutive weeks. The events of interest (ART LTFU) and competing events (TB LTFU) are considered if the occurrence of the two events is not simultaneous (if an individual experiences ART LTFU, but s/he no longer experiences TB LTFU at the same time point during our follow-up period). Outcomes were categorised as follows: 1 (LTFU from ART, the event of interest), 2 (LTFU from anti-TB treatment, the competing event), or 0 (censored, including death, treatment completion, cure, or other discontinuations).
Predictors
The study included three categories of predictors: (1) socioeconomic factors (sex, age, religion, education, occupation, residence, marital status); (2) baseline clinical characteristics (BMI, functional status, WHO HIV/AIDS stages, CD4 count, haemoglobin level); and (3) diagnosis- and treatment-related factors (adverse drug events, opportunistic infections (OIs), TB category, TB treatment completion, isoniazid preventive therapy (IPT), cotrimoxazole preventive therapy (CPT), baseline viral load, pain assessment/management, ART adherence, and fluconazole preventive therapy (FPT). These variables were analysed to identify their associations with competing risks of LTFU in TB/HIV coinfected adults.
Operational definitions
TB/HIV coinfection
Refers to the concurrent presence of HIV and TB infections (40).
Lost to follow-up (LTFU)
Was defined as interrupting anti-TB treatment for ≥ 8 consecutive weeks after ≥ 4 weeks of therapy40or missing ART appointments for > 90 days41.
Adherence to ART
Was categorized as good (> 95% adherence: <2 missed doses/30 or < 3/60 doses), fair (85–94%: 2–4 missed/30 or 4–9/60 doses), or poor (< 85%: ≥5 missed/30 or ≥ 10/60 doses), as documented by clinicians41.
Opportunistic infections (OIs) included
Any diagnosed OI other than TB.
Haemoglobin levels
Were classified as anaemic (≤ 11.0 g/dl) or normal (> 11.0 g/dl), irrespective of sex or pregnancy25.
Time to LTFU
Was calculated in months from ART or anti-TB initiation until discontinuation. Events: was LTFU from ART or anti-TB treatment during the study period (June 28, 2017–June 27, 2022).
Censored
Patients were censored if they died, remained in care, or were transferred to other facilities.
Survival status
Was categorised as LTFU or censored based on clinical records.
Sample size determination
The required sample size was calculated using the Freedman method of proportional event allocation42, which accounts for the probability of the event as 1− (ps1 (t) + qs2 (t)), where n denotes the sample size, Zα/2 (1.96 at α = 5%), and β (1.282 for 90% power). Assuming equal allocation between groups (p = q = 0.5), hazard ratios (HRs) from prior studies were incorporated. Using Stata version 14’s power log-rank command with parameters including a hazard ratio of 0.451, 90% power, and a withdrawal probability of 0.1, separate sample sizes were computed for five predictors (haemoglobin, adverse drug events, opportunistic infections, TB treatment completion, and isoniazid preventive therapy (IPT) identified as statistically significant in earlier research25. The largest calculated sample size (214) was selected, adjusted for a design effect of 2 to accommodate multistage sampling variability, and increased by 10% to account for incomplete records, yielding a final sample size of 471.
Sampling techniques
We employed a multistage stratified random sampling technique to select participants from seven public health facilities in Bahir Dar City. Medical registration numbers (MRNs) of patients enrolled in ART or TB follow-up programs were compiled from facility registries spanning June 28, 2017, to June 27, 2022. All eligible MRNs within each facility were catalogued, and proportional sample sizes were allocated to each health facility to ensure representative sampling. Using Microsoft Excel’s randomisation function, MRNs were randomly selected from these stratified lists. A total of 471 medical records were included in the study, distributed as follows: 135 from Felege Hiwot Comprehensive Specialised Hospital (FHCSH), 82 from Bahir Dar Health Centre (HC), 72 from Han HC, 69 from Addis Alem Primary Hospital (APH), 54 from Shimbet HC, 39 from Abay HC, and 20 from Tis-Abay HC. This approach ensured geographic and institutional diversity while maintaining methodological rigour in participant selection (Fig. 1).
Data extraction procedures
We developed structured checklists aligned with the variables of interest to systematically extract data from TB/ART patient charts and Smart Care registries. Trained healthcare professionals external to the selected facilities conducted the data extraction using a standardised tool. The manuscript’s corresponding authors supervised the process daily, verifying completeness, consistency, and accuracy through cross-verification. To mitigate data gaps, records lost during tracing or patients with undetermined ART/TB status were systematically replaced with nearby records, maintaining the integrity of the dataset.
Data quality control
Data quality was ensured throughout tool development, data extraction, coding, entry, cleaning, and analysis. A structured checklist based on the data elements to be recorded on patient charts, registries and follow-up forms was prepared before data extraction. The data extractors and supervisors received one day of training on the data extraction methods. Health professionals with experience in TB and/or ART clinics were recruited. Each day, completed checklists were reviewed for completeness, accuracy, and clarity, with necessary corrections provided the following morning.
Data processing and analysis
The extracted data were initially coded, cleaned, and entered into EPI-data version 4.643. To address missing data, multiple imputation techniques were employed because we had 12.3% missing data across the dataset of our key variables, including critical laboratory parameters such as viral load and CD4 count.Specifically, we directly compared results from the imputed dataset with those from a complete case analysis (CCA). The CCA approach, which excluded participants with missing data (n = 413), yielded less precise estimates (e.g., wider confidence intervals) and demonstrated clinically meaningful differences in effect sizes for key predictors. Descriptive statistics were conducted using Stata version 1444, while RStudio(We adjusted the version (starting from 4.3.0, then 4.3.1, 4.3.2, and so on) to accommodate the dependencies required by different packages)45 software was utilised for estimating cumulative incidence curves and performing multivariable analysis.
In the presence of competing risks, standard survival methods such as the Kaplan-Meier estimator are inadequate, as they inherently censor competing events and overestimate the probability of the event of interest. Instead, cumulative incidence functions (CIFs) were utilised to account for the interdependence of event types, where the occurrence of one event (e.g., anti-TB treatment LTFU) alters the probability of observing the primary event (ART LTFU). The CIF quantifies the probability of an individual experiencing a specific event (e.g., ART LTFU) by time “t”, conditional on not having experienced any prior event. This approach explicitly acknowledges that individuals experiencing competing events remain in the risk set for the primary event, ensuring unbiased estimation.
Given the study’s focus on ART LTFU as the primary outcome, with anti-TB treatment LTFU as a competing risk, the Fine and Gray subdistribution hazard regression model (FGSDHRM) was used to directly model the CIF. Unlike cause-specific hazard models, FGSDHRM accounts for the cumulative effect of covariates on the subdistribution hazard function (SDHF), which reflects the instantaneous risk of the primary event among those who have not yet experienced it or are still at risk despite competing events. This is critical in settings where competing events are informative and non-negligible.
After checking the proportional subdistribution hazard assumption via the cumulative sum of residuals, CIF plots, and modified Schoenfeld residuals, we fitted a multivariable Fine-Gray subdistribution hazard regression model (FGSDHRM) to assess the impact of covariates, age, sex, residence, marital status, religion, occupation, baseline BMI, functional status, WHO stage, CD4 count, haemoglobin level, adverse drug events, pain management, opportunistic infections, TB type, TB treatment completion, IPT, ART adherence, and viral load, on the subdistribution hazard for LTFU from ART versus anti-TB treatment. Covariates with bivariable p ≤ 0.25 were entered into the multivariable model, and those with p < 0.05 were deemed significant.
Model fit was assessed via cross-validated calibration curves, which showed close agreement between predicted and observed CIFs, and discrimination was quantified by an AUC of 0.888 (88.8%). A low Brier score of 3.4% further indicated excellent overall performance46. Finally, subdistribution hazard ratios with 95% confidence intervals were reported as statistically significant predictors of time to LTFU in the final FGSDHRM.
Results
Baseline sociodemographic characteristics and LTFU rates of participants
We included 471 co-infected adults, with a median age of 38 years (an interquartile rangeof 32–47) and an age range of 16 to 78 years. Females constituted slightly more than half of the participants, and approximately seven in ten experienced the event of interest (Table 1).
Baseline clinical, diagnosis and treatment characteristics of participants
Among the participants, 88.3% had a baseline BMI below the national threshold for adequate nutrition (BMI < 18.5 kg/m2), and 83.08% of these individuals experienced the event of interest. Out of the participants, 435 (92.36%) reported no adverse drug effects, and 10(15.38%) experienced the event of interest (Table 2).
The incidence and median survival time for LTFU from anti-TB treatment or ART among coinfected adults
Among the participants, 13.80% experienced ART LTFU as the primary event of interest, while 11.04% encountered anti-TB treatment LTFU as a competing event. The incidence of ART LTFU was 3.90 cases per 1000 person-months of observation (PMOs), and the incidence of anti-TB treatment LTFU was approximately 19.17 cases per 1000 PMOs. Additionally, 70.77% of the LTFU cases occurred among females, with an incidence rate of 5.62 new cases per 1000 PMOs.
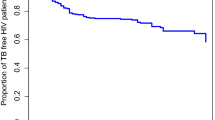
We recorded a total of 16,666.86 PMOs for ART and 2,724.43 PMOs for anti-TB treatment follow-up. The duration of ART follow-up ranged from 0.93 to 69.6 months, whereas the anti-TB treatment was from 0.4 to 8 months. Due to significant censoring, the median survival time was indeterminable. To prevent underestimating survival time, we used the restricted mean survival time (RMST), which offers a more precise estimate. The overall RMST was 59.97 months (95% CI 57.29–62.64) for ART LTFU patients and 7.41 months (95% CI 7.26–7.57) for anti-TB treatment LTFU. The RMST to ART LTFU was longer for males (64.69 months) than for females (51.31 months) (Table 3).
Cumulative incidence differences among categorical covariates among adult TB/HIV-coinfected patients
The statistical analysis revealed significant differences between categories of sex, residence, marital status, BMI, functional status, WHO clinical stages, CD4 counts, Hgb levels, viral load, pain management, presence of OIs other than TB, TB type, TB treatment completion, IPT, adverse drug effects, and ART drug adherence. However, no significant differences were found in the categories of religion, educational level, occupational status, CPT, and FPT (Table 3).
The cumulative incidence of ART LTFU was estimated to be 5.4, 8.2, 11.2, 15.6, and 28.9% at 12, 24, 36, 48, and 60 months of follow-up, respectively. In contrast, the cumulative incidence of anti-TB treatment LTFU was estimated to be 3.7, 5.5, 7.5, 12.5, and 23.6% at the same follow-up intervals. These estimates indicate a persistent increase in the probability of experiencing both events over time among Coinfected adults.
We use the CIF curve to compare the CIF differences between categories of covariates using Gray’s test. The overall incidence of the event of interest exceeded that of the competing event. Both events began to rise at the study’s onset, with the expected incidence of both events increasing from the start-up to 60 months, after which it remained stable until the end of the final follow-up period (Fig. 2a).
There was a significant difference in the incidence of LTFU between rural and urban settings for both treatments. Specifically, the incidence of experiencing the event of interest was higher in rural areas than in urban areas. Conversely, the incidence of competing events was higher in urban areas than in rural areas (Fig. 2b).
Concerning anti-TB treatment, there were significant differences in LTFU incidence based on baseline BMI. Compared with their counterparts, individuals with a BMI < 18.5 kg/m² had a lower incidence of experiencing competing events, although there was no statistically significant difference in LTFU from ART (Fig. 2c).
Significant differences in LTFU incidence were observed between categories of baseline haemoglobin (Hgb) levels for ART. Individuals with baseline Hgb levels < 11 g/dl had a greater incidence of experiencing the event of interest than those with higher Hgb levels. However, there was no significant difference in LTFU from anti-TB treatment based on baseline Hgb levels (Fig. 2d).
There was a notable difference in LTFU incidence between categories of adverse drug effects from ART. Individuals with a history of adverse drug effects had a higher incidence of the event of interest than those without such a history. However, no significant difference in LTFU incidence was observed for patients receiving anti-TB treatment because of adverse drug effects (Fig. 2e).
Additionally, there was a significant difference in LTFU incidence between categories of OIs from ART. Individuals with a history of at least one OI other than TB experienced a higher incidence of the event of interest than those with no history of OIs. No significant difference in LTFU incidence was found for anti-TB treatment based on OI history (Fig. 2f).
Predictors of time to LTFU from ART and anti-TB treatment among adults with TB/HIV coinfections in the final SDHRM
We applied the Fine and Gray subdistribution hazard regression model (FGSDHRM) to analyse the competing risks of LTFU among TB/HIV co-infected adults. This approach allowed us to account for the presence of competing events, providing a more accurate estimation of the cumulative incidence of LTFU.
Our analysis identified four variables as significant prognostic factors for LTFU from ART. These factors were determined based on their SHRs and corresponding 95% CIs, indicating their impact on the risk of ART LTFU over time. Similarly, seven variables were found to be significant predictors of LTFU from anti-TB treatment. These variables demonstrated statistically significant associations with the risk of LTFU, as evidenced by their SHRs and 95% CIs.
The identification of these prognostic factors through FGSDHRM underscores the importance of considering competing risks in survival analysis, particularly in the context of TB/HIV co-infection, where patients are at risk of multiple, mutually exclusive events. For ART LTFU, significant predictors included a rural residence, WHO clinical stage IV, Hgb level < 11 g/dl and a history of opportunistic infections other than TB were associated with an increased incidence of ART LTFU. For anti-TB treatment LTFU, significant predictors were age, rural residence, and baseline BMI < 18.5 kg/m², which are associated with a decreased incidence, whereas marital status (divorced and widowed), baseline functional status (ambulatory), adverse drug effects, and ART drug adherence are associated with an increased incidence ant-TB treatment LTFU.
Table 4 presents the SDH ratios, P values, and 95% confidence intervals for the selected covariates derived from the FGSDHRM for different types of treatment, LTFU.
The analysis revealed that the SDHR for coinfected adults residing in rural areas is 3.39 times that of those living in urban areas, indicating that the cumulative incidence of ART LTFU is significantly higher among rural dwellers (SDHR = 3.39, 95% CI: 1.56–7.41). Furthermore, the SDHR indicates that coinfected adults with a baseline WHO HIV/AIDS clinical stage IV have a 2.88 times higher cumulative incidence of ART LTFU compared to those with a baseline stage I, suggesting that individuals with stage IV disease are at significantly higher risk of LTFU (SDHR = 2.88, 95% CI 1.01–8.26).
Additionally, coinfected adults with a baseline Hgb level of less than 11 g/dl is 3.56 times higher than those with a baseline Hgb level of 11 g/dl or higher, indicating that the cumulative incidence of ART LTFU is significantly higher among those with Hgb levels less than 11 g/dl (SDHR = 3.56, 95% CI 1.75–7.24).
Finally, the SDHR for coinfected adults with opportunistic infections (OIs) other than tuberculosis is 3.65 times higher than that for those without OIs other than TB, indicating that the `cumulative incidence of ART LTFU is significantly higher among individuals with OIs other than TB (SDHR = 3.65, 95% CI 1.77–7.53).
Based on the analysis, the effects of age were found to be similar for both types of failures (ART and anti-TB treatment LTFU), with no significant impact on LTFU for either treatment (SDHR = 0.98, 95% CI 0.95–1.0, p = 0.19 and SDHR = 0.97, 95% CI 0.94–1.00, p = 0.047, respectively). Compared to their urban counterparts, adults with coinfection residing in rural areas have an 89% lower cumulative incidence of LTFU during anti-TB treatment. This suggests a significantly reduced cumulative incidence of LTFU in rural settings (SHR = 0.11, 95% CI 0.04–0.32).
Adults with coinfection who were divorced or widowed experienced a significantly higher cumulative incidence of LTFU during anti-TB treatment compared to those who were married. Specifically, the SDHR indicated that divorced individuals had a 2.81 times higher risk (95% CI: 1.01–7.82](of LTFU, and widowed individuals had a 5.92 times higher risk (95% CI: 2.17–16.15) of LTFU during TB treatment.
Individuals with a baseline BMI of less than 18.5 kg/m² have a 59% lower SDH of LTFU during anti-TB treatment compared to those with a BMI of 18.5 kg/m² or greater. This indicates a lower cumulative incidence of LTFU among those with lower BMIs, as reflected by an SDHR of 0.41(95% CI: 0.20–0.82). Individuals with an ambulatory baseline functional status are 2.59 times more likely to experience LTFU from anti-TB treatment compared to those with a working baseline functional status. This indicates a higher cumulative incidence of anti-TB treatment LTFU among those with ambulatory functional status, as reflected by an SDHR of 2.59 (95% CI: 1.19–5.69).
Poor ART drug adherence was associated with a 5.72-fold greater likelihood of experiencing LTFU from anti-TB treatment compared to good ART drug adherence, indicating a significantly higher cumulative incidence of anti-TB treatment LTFU (SHR = 5.72,95% CI: 2.36–13.84). Finally, Individuals who experienced adverse drug effects were 2.87 times more likely to be LTFU on anti-TB treatment compared to those who did not experience adverse drug effects. This indicates a higher incidence of LTFU among individuals with adverse drug effects. This suggests that the association is statistically significant and that adverse drug effects are a substantial risk factor for LTFU (SDHR = 2.87, 95% CI 1.23–6.73) (Table 4).
Discussion
In our study, we identified the predictors of time to LTFU from ART and TB treatment using LTFU from TB treatment as competing events and the cumulative incidence of time to LTFU from ART, the event of interest. Accordingly, individuals residing in rural areas, those classified as WHO stage IV, those with haemoglobin levels below 11 g/dl, and those with opportunistic infections were identified as statistically significant prognostic predictors of ART LTFU. Similarly, rural residence, being divorced or widowed, ambulatory functional status, adverse drug effects, and poor ART adherence were significant prognostic predictors of TB treatment LTFU.
Our analysis accounted for drawbacks or failures of the conventional time-to-event survival analysis method, which were addressed in the literature47, and studies show that conventional survival hazard regression models fail to account for multiple competing events when estimating the effect sizes of predictors38,48.
The median survival time for LTFU from anti-TB or ART among adults with TB/HIV-coinfected patients is undetermined; however, the RMST of ART LTFU and anti-TB treatment LTFU among coinfected adult patients were estimated and found to be 59.97 and 7.41 months, respectively, but these findings could not be compared with those of other studies because other studies reported median survival time.
The incidence of ART LTFU was 3.9 LTFU cases per 1000 PMOs or 4.7/100 PYOs (95% CI: 3–5), which is lower than that reported in studies conducted in Zimbabwe (5.75 per 100 PYOs)49, Uganda (7.5 per 100 PYOs)50 and Ethiopia (10.9 per 100 PYOs)27. These differences could be attributed to variations in sample sizes, follow-up durations, study environments, and the characteristics of the populations involved. In this context, the follow-up periods of the Ugandan50 and previous Ethiopian studies27 were three and four years, respectively. The follow-up period of our study was five years. In addition, in our study, we used a competing risk analysis approach, which prevents upward estimation of the standard survival analysis estimates. The incidence rate of LTFU during anti-TB treatment was 19.17 per 1000 PMOs (95% CI: 14.6–25.2). This result is lower than a study conducted in the Sheka Zone health centres, in southern Ethiopia, which reported incidence rates of 27.3 per 1000 PMOs but higher than findings in the same place in a general hospital, which reported incidence rates of 9.6 per 1000 PMOs51. It is also higher than the rate observed in a study from Gondar, Ethiopia, where the incidence rate was 6.47 per 1000 PMOs52. The above variations might be due to differences in sample sizes, study settings, and population characteristics52. In this context, the sample size and population characteristics in the previous study included 332 individuals with drug-resistant tuberculosis but 471 TB/HIV Coinfected adults, and the previous study was performed at a specialised hospital, whereas our study was done in both hospitals and health centres. Therefore, there may be health service delivery differences across settings.
Residence in rural areas, baseline WHO clinical stage IV, baseline haemoglobin levels less than 11 g/dl, and a history of opportunistic infections other than TB have been identified as potential prognostic factors for ART LTFU. Our study revealed that rural residency significantly increases the risk of ART LTFU, a finding that is consistent with research conducted in sub-Saharan Africa, including Debre Markos and Oromiya in Ethiopia53,54,55. This association may be attributed to the extended travel times required for rural residents to access healthcare facilities, which can hinder regular clinic visits and medication pickups, thereby increasing the risk of LTFU25,53. Additionally, rural populations often experience lower income levels, limited employment opportunities, and undernutrition, which can further impact their ability to access and maintain care. Furthermore, the lack of strong community-based support systems in rural areas may negatively influence treatment adherence and retention in care25,53,56.
In this study, patients with a baseline WHO clinical stage IV disease were at a higher risk of ART LTFU. This result is supported by research carried out in Ethiopia’s Oromia region, along with studies from Tanzania and Uganda50,54,57. These studies suggest that individuals with advanced HIV/AIDS (WHO clinical stage IV) may experience more severe symptoms and treatment side effects, which can affect their adherence to ART and ongoing engagement in care. Additionally, patients with advanced disease often require more intensive healthcare support. Those residing in rural areas or with limited access to healthcare facilities may encounter difficulties in obtaining necessary care, leading to increased instances of LTFU58,59. Furthermore, patients with advanced HIV/AIDS may face heightened social and economic challenges, such as discrimination, stigma, poverty, and insufficient social support, which can exacerbate their difficulties in maintaining care and adhering to treatment60. Advanced disease status is also associated with a risk of mortality and can contribute to ART LTFU due to adverse effects such as drug toxicity, treatment failure, and drug resistance, ultimately compromising patient survival25.
Coinfected adult patients with a baseline haemoglobin level of less than 11 g/dl are at increased risk of LTFU from ART. This result aligns with studies carried out in Ethiopia’s Tigray region25. Low haemoglobin levels are often indicative of disease severity, disability, and overall impairment12,61. They may also signal a serious illness, contributing to symptoms that complicate adherence to ART and the continuation of care. Additionally, low haemoglobin is a common comorbidity among ART patients, exacerbating symptoms such as weakness and fatigue31. For patients coinfected with TB/HIV, the need for multiple medications to address HIV, TB, and anaemia can result in a significant treatment burden. This burden, coupled with the complex side effects of these drugs, may adversely impact a patient’s ability to adhere to ART and maintain engagement in care, potentially increasing the incidence of LTFU25.
Patients who have experienced OIs other than TB tend to have a higher incidence of LTFU from ART. This result is in line with studies carried out in the Tigray region of Ethiopia25. Despite the availability of ART62, OIs continue to be a significant cause of hospitalisation and advanced disease, potentially leading to increased LTFU and higher healthcare utilisation. OIs can undermine adherence to treatment and raise concerns about adverse effects, thereby increasing the risk of LTFU. Evidence suggests that the presence of OIs during ART follow-up may indicate therapy failure or poor response, contributing to LTFU by exacerbating the overall burden of illness and increasing the frequency of medical visits. Furthermore, poor treatment adherence associated with OIs is linked to the incidence of LTFU and challenges in managing drug adherence61,63,64,65.
Age, residence (rural), marital status (divorced and widowed), baseline BMI (BMI < 18.5 kg/m²), baseline functional status (ambulatory), the presence of adverse drug effects, and poor ART drug adherence have been identified as potential prognostic factors for LTFU from anti-TB treatment. In our study, age appeared to have a comparable effect on the incidence of LTFU across both treatments. However, this finding contrasts with existing scientific evidence suggesting that age can positively influence the risk of LTFU in anti-TB treatment among adults. For example, a retrospective cohort study conducted in Ethiopia indicated that older TB patients experienced higher rates of LTFU than their younger counterparts did51. Similarly, another Ethiopian study reported that TB patients aged 55–64 years were four times more likely to experience LTFU66. Furthermore, a global analysis of LTFU in multidrug-resistant TB (MDR-TB) patients across 22 countries revealed that HIV-positive individuals aged 36–50 years face the highest risk of LTFU67.
An increased incidence of LTFU for anti-TB treatment has been observed among coinfected adults, who are divorced or widowed, a finding that is consistent with a study conducted in Central Kenya (40). Prior research on healthcare utilisation and marital status in the Netherlands68 has highlighted differences based on marital status. This association may be attributed to several factors, including social support, economic stability, psychological impact, and healthcare access, which are often less favourable for individuals who are divorced or widowed69,70,71. Additionally, studies in Northwest Ethiopia and India have indicated a significant link between single or divorced marital status and poorer adherence to TB treatment72.
A Coinfected adult whose baseline BMI is less than 18.5 kg/m2 (undernutrition) has a decreased incidence of anti-TB treatment LTFU. Research conducted in Taiwan, Peru, Guinea, South Africa, and Ethiopia has demonstrated that underweight patients with TB face a higher risk of LTFU than those with a normal BMI73,74,75,76,77. This elevated risk may be attributed to a combination of factors, including the severity of the disease, economic instability, comorbid health conditions, and treatment adherence69,70,71. Among coinfected adults, an ambulatory baseline functional status is associated with an increased incidence of LTFU for anti-TB treatment. This observation is consistent with results from a competing risk study carried out in Gondar27. The relationship between ambulatory functional status and lost of follow-up for TB treatment is multifaceted, encompassing factors such as disease severity, adherence to treatment, and access to and support from healthcare services25,73.
Patients with coinfection who have a history of adverse drug events are at a higher risk of LTFU during anti-TB treatment. The increase in treatment LTFU can be linked to a range of interconnected factors, including adherence to treatment, economic stability, psychological effects, and the availability of healthcare and support services70,71,75,78,79. Furthermore, having to manage multiple medications can lead patients to stop taking some drugs, focusing instead on continuing others to lessen the overall medication burden, especially if they perceive one condition as less severe than the other.
Finally, a coinfected patient with poor adherence to ART is at increased risk of LTFU from anti-TB treatment. The factors contributing to this increased risk may include adverse drug effects, forgetfulness in medication adherence, prolonged absences from home, missed appointments, lack of transportation, insufficient social support, conflicts with religious beliefs, demands on traditional healers, fear of stigma and discrimination, feelings of hopelessness regarding treatment, inadequate communication between patients and healthcare providers, and interruptions in the availability of medications38,80.
Conclusion
This study investigates the time to lost to follow-up and its predictors among adults co-infected with tuberculosis (TB) and HIV. While the median survival time was undetermined, the restricted mean survival time was 59.97 months. The incidence rates of LTFU were 3.90 and 19.17 per 1,000 PMOs for ART and anti-TB treatment, respectively. The cumulative incidence of LTFU was 13.8% for ART and 11.04% for anti-TB treatment. Notably, the ART LTFU rate (3.9 per 1000 PMOs) was lower than that reported in a previous Ethiopian study (9.1 per 1000 PMOs), while the anti-TB treatment LTFU rate (19.17 per 1,000 PMOs) was higher than that reported in Gondar, Ethiopia (6.47 per 1,000 PMOs).
The risk of ART LTFU was significantly higher among individuals living in rural areas, those at WHO stage IV, with haemoglobin levels below 11 g/dl, and those with opportunistic infections. TB treatment LTFU was more prevalent among rural residents, divorced or widowed individuals, and those with ambulatory functional status, adverse drug effects, and poor ART adherence.
These findings underscore the need for enhanced care, close monitoring, and regular follow-ups for TB/HIV co-infected adults, particularly those at higher risk of LTFU. Healthcare systems should implement structured counselling, integrated follow-up mechanisms, and intensified monitoring strategies. Strengthening adherence counselling, coordinating multidisciplinary case teams, and ensuring regular supervision and mentoring of health facilities are vital. Collaboration with nongovernmental organisations to align adherence programs with ART and TB services is also recommended.
Strengths and limitations of the study
The study on lost to follow-up from ART and anti-TB treatment was conducted as a multicenter analysis utilising a competing risk framework with the Fine and Gray subdistribution hazard regression model. This approach is advantageous because it mitigates the overestimation commonly associated with Kaplan‒Meier estimates and provides interpretable risk estimates. The Fine and Gray model effectively manages competing risks and aligns with the cumulative incidence of each event type. The analysis accounts for informative censoring and dependent events. This study is pioneering in evaluating the time to LTFU from ART and anti-TB treatment and identifying predictors among coinfected adults using a competing risk analysis.
However, the study’s findings should be considered within the context of certain limitations. The use of secondary data precluded the inclusion of significant predictors such as distance from the facility, income level, disclosure status, treatment regimens, and other clinical factors due to inadequate recording. Additionally, the study faced a substantial level of censorship (75.2%), which may affect model stability. However, similar studies have been published with comparable levels of censorship25,27,55. It is recommended that future researchers conduct prospective or retrospective follow-up studies by including important predictors of ART LTFU that were not addressed in this study, such as income level, distance from a health facility, disclosure status, treatment regimen, and substance use.
Data availability
All the data are available within the manuscript. If additional datasets are required, they can be obtained from the corresponding author upon a reasonable request.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- ART:
-
Anti-retroviral therapy
- BMI:
-
Body mass index
- CD4:
-
Cluster of differentiation 4
- CI:
-
Confidence interval
- CIF:
-
Cumulative incidence function
- CPT:
-
Cotrimoxazole preventive therapy
- FGSDHRM:
-
Fine-gray subdistribution regression hazard model
- FPT:
-
Fluconazole preventive therapy
- Hgb:
-
Haemoglobin
- HIV:
-
Human immunodeficiency virus
- HR:
-
Hazard ratio
- IPT:
-
Isoniazid prophylactic therapy
- LTFU:
-
Lost to follow-up
- OI(s):
-
Opportunistic infection(s)
- PMOs:
-
Person months of observation
- PYOs:
-
Person years of observation
- RMST:
-
Restricted mean survival time
- SDHF/R:
-
Subdistribution hazard function/ratio
- TB:
-
Tuberculosis
- WHO:
-
World health organisation
References
Lawn, S. D. & Zumla, A. I. Tuberculosis. Lancet 378 (9785), 57–72. (2011).
WHO G. Global tuberculosis report 2020. Glob. Tuberc. Rep. (2020).
Organization, W. H. Global Tuberculosis Report 2021: Supplementary Material (World Health Organization, 2022).
Gurumurthy, P. et al. Decreased bioavailability of Rifampin and other antituberculosis drugs in patients with advanced human immunodeficiency virus disease. Antimicrob. Agents Chemother. 48 (11), 4473–4475 (2004).
McIlleron, H., Meintjes, G., Burman, W. J. & Maartens, G. Complications of antiretroviral therapy in patients with tuberculosis: drug interactions, toxicity, and immune reconstitution inflammatory syndrome. J. Infect. Dis. 196 (1), S63–75 (2007).
Organization, W. H. Consolidated Guidelines on HIV Prevention, Diagnosis, Treatment and Care for Key Populations (World Health Organization, 2016).
Tadokera, R. et al. Hypercytokinaemia accompanies HIV–tuberculosis immune reconstitution inflammatory syndrome. Eur. Respir. J. 37 (5), 1248–1259 (2011).
Mills, E. J. et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North america: a meta-analysis. Jama 296 (6), 679–690 (2006).
Harries, A. D., Zachariah, R. & Lawn, S. D. Providing HIV care for co-infected tuberculosis patients: a perspective from sub-Saharan Africa. Int. J. Tuberc Lung Dis. 13 (1), 6–16 (2009).
CDC. Managing drug interactions in the treatment of HIV-related tuberculosis. http://www.cdc.gov/tb/TB_HIV_Drugs/default.htm (2013).
MoH Ethiopia. Guidelines for Clinical and Programmatic Management of TB, TB/HIV, DR-TB and Leprosy in Ethiopia 2021.
Arnesen, R., Moll, A. P. & Shenoi, S. V. Predictors of lost to follow-up among patients on ART at a rural hospital in KwaZulu-Natal, South Africa. PLoS One. 12 (5), e0177168 (2017).
Haas, A. D. et al. Retention and mortality on antiretroviral therapy in sub-Saharan africa: collaborative analyses of HIV treatment programmes. J. Int. AIDS. Soc. 21 (2), e25084 (2018).
Joseph Davey, D. et al. Same-day antiretroviral therapy is associated with increased lost to follow‐up in South African public health facilities: a prospective cohort study of patients diagnosed with HIV. J. Int. AIDS. Soc. 23 (6), e25529 (2020).
Khumalo, P. G., Chou, Y. J. & Pu, C. Antiretroviral treatment attrition in swaziland: a population-based study. Epidemiol. Infect. 144 (16), 3474–3482 (2016).
Legesse, T. et al. Trends of tuberculosis treatment outcomes of notified cases in three refugee camps in sudan: a four-year retrospective analysis, 2014–2017. Sudan. J. Med. Sci. 16 (2), 259–275 (2021).
Mugisha, V. et al. Determinants of mortality and lost to follow-up among adults enrolled in HIV care services in Rwanda. PLoS One. 9 (1), e85774 (2014).
Nacarapa, E. et al. Predictors of attrition among adults in a rural HIV clinic in Southern mozambique: 18-year retrospective study. Sci. Rep. 11 (1), 17897 (2021).
Nansera, D. et al. Mortality and lost to follow-up among tuberculosis and HIV co-infected patients in rural Southwestern Uganda. Int. J. Tuberc. Lung Dis. 16 (10), 1371–1376 (2012).
Ntabanganyimana, D., Rugema, L., Omolo, J., Nsekuye, O. & Malamba, S. S. Incidence and factors associated with being lost to follow-up among people living with HIV and receiving antiretroviral therapy in nyarugenge the central business district of Kigali city, Rwanda. PLoS One. 17 (10), e0275954 (2022).
Wekesa, P., McLigeyo, A., Owuor, K., Mwangi, J. & Ngugi, E. Survival probability and factors associated with time to lost to follow-up and mortality among patients on antiretroviral treatment in central Kenya. BMC Infect. Dis. 22 (1), 522 (2022).
Zürcher, K. et al. Outcomes of HIV-positive patients lost to follow‐up in African treatment programmes. Tropical Med. Int. Health. 22 (4), 375–387 (2017).
Carriquiry, G. et al. Mortality and lost to follow-up among HIV-infected persons on long-term antiretroviral therapy in Latin America and the Caribbean. J. Int. AIDS Soc. 18 (1), 20016 (2015).
Dessu, S., Mesele, M., Habte, A. & Dawit, Z. Time until lost to follow-up, incidence, and predictors among adults taking ART at public hospitals in Southern Ethiopia. HIV/AIDS-Res. Palliative Care 205 – 215. (2021).
Gezae, K. E., Abebe, H. T. & Gebretsadik, L. G. Incidence and predictors of LTFU among adults with TB/HIV co-infection in two governmental hospitals, mekelle, ethiopia, 2009–2016: survival model approach. BMC Infect. Dis. 19 (1), 107 (2019).
Mekonnen, N., Abdulkadir, M., Shumetie, E., Baraki, A. G. & Yenit, M. K. Incidence and predictors of lost to follow-up among HIV infected adults after initiation of first line anti-retroviral therapy at university of Gondar comprehensive specialized hospital Northwest ethiopia, 2018: retrospective follow up study. BMC Res. Notes. 12 (1), 111 (2019).
Teshale, A. B., Tsegaye, A. T. & Wolde, H. F. Incidence and predictors of lost to follow up among adult HIV patients on antiretroviral therapy in university of Gondar comprehensive specialized hospital: A competing risk regression modeling. PLoS One. 15 (1), e0227473 (2020).
Tola, H. H., Azar, T., Shojaeizadeh, D. & Garmaroudi, G. Tuberculosis treatment non-adherence and lost to follow up among TB patients with or without HIV in developing countries: a systematic review. Iran. J. Public. Health. 44 (1), 1 (2015).
Kibuule, D. et al. Predictors of lost to follow-up of tuberculosis cases under the DOTS programme in Namibia. ERJ Open. Res. 6 (1). (2020).
Mekonnen, H. S. & Azagew, A. W. Non-adherence to anti-tuberculosis treatment, reasons and associated factors among TB patients attending at Gondar town health centers, Northwest Ethiopia. BMC Res. Notes. 11 (1), 691 (2018).
Shroufi, A. et al. Risk of death among those awaiting treatment for HIV infection in zimbabwe: adolescents are at particular risk. J. Int. AIDS Soc. 18 (1), 19247 (2015).
Oni, T. et al. High prevalence of subclinical tuberculosis in HIV-1-infected persons without advanced immunodeficiency: implications for TB screening. Thorax 66 (8), 669–673 (2011).
Balcha, T. T. & Jeppsson, A. Outcomes of antiretroviral treatment: a comparison between hospitals and health centers in Ethiopia. J. Int. Assoc. Physicians AIDS Care (Chic). 9 (5), 318–324 (2010).
Muñoz-Sellart, M., Cuevas, L., Tumato, M., Merid, Y. & Yassin, M. Factors associated with poor tuberculosis treatment outcome in the Southern region of Ethiopia. Int. J. Tuberc. Lung Dis. 14 (8), 973–979 (2010).
Uyei, J., Coetzee, D., Macinko, J. & Guttmacher, S. Integrated delivery of HIV and tuberculosis services in sub-Saharan africa: a systematic review. Lancet. Infect. Dis. 11 (11), 855–867 (2011).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94 (446), 496–509 (1999).
Gooley, T. A., Leisenring, W., Crowley, J. & Storer, B. E. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat. Med. 18 (6), 695–706 (1999).
Putter, H., Fiocco, M. & Geskus, R. B. Tutorial in biostatistics: competing risks and multi-state models. Stat. Med. 26 (11), 2389–2430 (2007).
Bahirdar city health Department. population projection, accounting censuses of 2007 by Ethiopian Statistical Agency (ESA), of Bahirdar city health Department. (2022).
Ministry of Health Ethiopia. Guidelines for management of Tb, Dr-Tb and leprosy in ethiopia. 6 (2017).
WHO Guidelines Approved by the Guidelines Review Committee. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. Geneva: World Health Organization Copyright © World Health Organization (2016).
Ryan, T. P. Sample Size Determination and Power (Wiley, 2013).
Epidata manager. http://www.epidata.dk (2024).
Stata version 14. https://www.stata.com/stata14/
Cran RStudio.
Zhang, Z. et al. Overview of model validation for survival regression model with competing risks using melanoma study data. Ann. Transl Med. 6 (16), 325 (2018).
Haller, B., Schmidt, G. & Ulm, K. Applying competing risks regression models: an overview. Lifetime Data Anal. 19 (1), 33–58 (2013).
Bakoyannis, G. & Touloumi, G. Practical methods for competing risks data: a review. Stat. Methods Med. Res. 21 (3), 257–272 (2012).
Matsena Zingoni, Z., Chirwa, T., Todd, J. & Musenge, E. Competing risk of mortality on lost to follow-up outcome among patients with HIV on ART: a retrospective cohort study from the Zimbabwe National ART programme. BMJ Open. 10 (10), e036136 (2020).
Kiwanuka, J., Mukulu Waila, J., Muhindo Kahungu, M., Kitonsa, J. & Kiwanuka, N. Determinants of lost to follow-up among HIV positive patients receiving antiretroviral therapy in a test and treat setting: A retrospective cohort study in masaka, Uganda. PLoS One. 15 (4), e0217606 (2020).
Shaweno, T., Getnet, M. & Fikru, C. Does time to lost to follow-up differ among adult tuberculosis patients initiated on tuberculosis treatment and care between general hospital and health centers? A retrospective cohort study. Trop. Med. Health. 48 (1), 1–11 (2020).
Kassa, G. M., Teferra, A. S., Wolde, H. F., Muluneh, A. G. & Merid, M. W. Incidence and predictors of lost to follow-up among drug-resistant tuberculosis patients at university of Gondar comprehensive specialized hospital, Northwest ethiopia: a retrospective follow-up study. BMC Infect. Dis. 19 (1), 817 (2019).
Kebede, H. K., Mwanri, L., Ward, P. & Gesesew, H. A. Predictors of lost to follow up from antiretroviral therapy among adults in sub-Saharan africa: a systematic review and meta-analysis. Infect. Dis. Poverty. 10 (1), 33 (2021).
Megerso, A. et al. Predictors of lost to follow-up in antiretroviral treatment for adult patients in the oromia region, Ethiopia. HIV AIDS (Auckl). 8, 83–92 (2016).
Birhanu, M. Y. et al. Incidence and predictors of lost to follow-up among HIV-positive adults in Northwest ethiopia: a retrospective cohort study. Trop. Med. Health. 48, 78 (2020).
Alebel, A., Sibbritt, D., Petrucka, P. & Demant, D. Undernutrition increased the risk of lost to follow-up among adults living with HIV on ART in Northwest ethiopia: a retrospective cohort study. Sci. Rep. 12 (1), 22556 (2022).
Tesha, E-D., Kishimba, R., Njau, P., Revocutus, B. & Mmbaga, E. Predictors of lost to follow up from antiretroviral therapy among adolescents with HIV/AIDS in Tanzania. PloS One. 17 (7), e0268825 (2022).
Berheto, T. M., Haile, D. B. & Mohammed, S. Predictors of lost to follow-up in patients living with HIV/AIDS after initiation of antiretroviral therapy. N Am. J. Med. Sci. 6 (9), 453–459 (2014).
Fisiha Kassa, S., Zemene Worku, W., Atalell, K. A. & Agegnehu, C. D. Incidence of lost to Follow-Up and its predictors among children with HIV on antiretroviral therapy at the university of Gondar comprehensive specialized referral hospital: A retrospective data analysis. HIV AIDS (Auckl). 12, 525–533 (2020).
Fentie, D. T., Kassa, G. M., Tiruneh, S. A. & Muche, A. A. Development and validation of a risk prediction model for lost to follow-up among adults on active antiretroviral therapy in ethiopia: a retrospective follow-up study. BMC Infect. Dis. 22 (1), 727 (2022).
Hibstie, Y. T. et al. Nearly one in every six HIV-infected children lost from ART follow-up at Debre Markos referral hospital, Northwest ethiopia: A 14-year retrospective follow-up study. PLoS One. 15 (9), e0239013 (2020).
Ogyiri, L. et al. Effect of HIV infection on TB treatment outcomes and time to mortality in two urban hospitals in Ghana-a retrospective cohort study. Pan Afr. Med. J. 32 (1). (2019).
Alebel, A., Demant, D., Petrucka, P. & Sibbritt, D. Effects of undernutrition on opportunistic infections among adults living with HIV on ART in Northwest ethiopia: using inverse-probability weighting. PLoS One. 17 (3), e0264843 (2022).
Mushy, S. E. et al. Predictors of the observed high prevalence of lost to follow-up in ART-experienced adult PLHIV: a retrospective longitudinal cohort study in the Tanga region, Tanzania. BMC Infect. Dis. 23 (1), 92 (2023).
Núñez, I. et al. Late-onset opportunistic infections while receiving anti-retroviral therapy in Latin america: burden and risk factors. Int. J. Infect. Dis. 122, 469–475 (2022).
Birhane, M., Mekonnen, S., Dingeta, T. & Teklemariam, Z. Lost to follow-up tuberculosis treatment and associated factors among adults attending at public health facilities in warder district, Somali regional state, Eastern Ethiopia. Front. Public. Health. 11, 1151077 (2023).
Walker, I. F. et al. Analysis of lost to follow-up in 4099 multidrug-resistant pulmonary tuberculosis patients. Eur. Respir. J. 54 (1). (2019).
Joung, I. M., van der Meer, J. B. & Mackenbach, J. P. Marital status and health care utilization. Int. J. Epidemiol. 24 (3), 569–575 (1995).
Mengesha, M. M., Gebremichael, M. A., Watumo, D., Hallström, I. K. & Jerene, D. Poor adult tuberculosis treatment outcome and associated factors in Gibe woreda, Southern ethiopia: an institution-based cross-sectional study. PLOS Glob Public. Health. 2 (3), e0000161 (2022).
Mishra, P. et al. Reasons for lost to follow-up (LTFU) of pulmonary TB (PTB) patients: A qualitative study among saharia, a particularly vulnerable tribal group of Madhya pradesh, India. PLoS One. 16 (12), e0261152 (2021).
Soedarsono, S. et al. Determinant factors for lost to follow-up in drug-resistant tuberculosis patients: the importance of psycho-social and economic aspects. BMC Pulm Med. 21 (1), 360 (2021).
Gashu, K. D., Gelaye, K. A. & Tilahun, B. Adherence to TB treatment remains low during continuation phase among adult patients in Northwest Ethiopia. BMC Infect. Dis. 21 (1), 1–10 (2021).
Adamashvili, N. et al. Low BMI increases all-cause mortality rates in patients with drug-resistant TB. Int. J. Tuberc Lung Dis. 26 (4), 326–333 (2022).
Aibana, O. et al. Nutritional status and tuberculosis risk in adult and pediatric household contacts. PLoS One. 11 (11), e0166333 (2016).
Jiang, Y. et al. Factors associated with lost to follow-up before and after treatment initiation among patients with tuberculosis: A 5-year observation in China. Front. Med. (Lausanne). 10, 1136094 (2023).
Lai, H. H., Lai, Y. J. & Yen, Y. F. Association of body mass index with timing of death during tuberculosis treatment. PLoS One. 12 (1), e0170104 (2017).
Wondimu, W., Dube, L. & Kabeta, T. Factors affecting survival rates among adult TB/HIV Co-Infected patients in Mizan Tepi university teaching hospital, South West Ethiopia. HIV AIDS (Auckl). 12, 157–164 (2020).
Michael, O. S., Sogaolu, O. M., Fehintola, F. A., Ige, O. M. & Falade, C. O. Adverse events to first line anti-tuberculosis drugs in patients co-infected with HIV and tuberculosis. Ann. IB. Postgrad. Med. 14 (1), 21–29 (2016).
Sant Anna, F. M. et al. Impact of adverse drug reactions on the outcomes of tuberculosis treatment. PLoS One. 18 (2), e0269765 (2023).
Manosuthi, W., Wiboonchutikul, S. & Sungkanuparph, S. Integrated therapy for HIV and tuberculosis. AIDS Res. Ther. 13, 22 (2016).
Acknowledgements
First, I am very grateful to GOD, who always helped me throughout the entire process.Second, I am grateful to Bahir Dar University College of Medicine and Health Sciences School of Public Health for allowing me to perform this research.Third, We would like to appreciate Hossana College of Health Sciences for financial and material support. Finally, I extend my deepest gratitude to the lecturers, families, friends, data extractors, supervisors and Bahir Dar City health department and selected public health facility staff for their valuable support and cooperativeness throughout my thesis work.
Funding
Hossana College of Health Sciences, which is a scholarship grantor, funded the study. The funder has no role in the design, conduct or analysis of the study.
Author information
Authors and Affiliations
Contributions
DR conceived the idea, wrote and presented the proposal, supervised the field work, curated the data, formally analysed the data, drafted and revised the manuscript.HG and AT reviewed the proposal, participated in the data analysis, reviewed the final report and reviewed the draft manuscript.HY reviewed the proposal, participated in the data analysis, reviewed the final report and reviewed the draft manuscript.AZ, TA, and ND reviewed the proposal, participated in the data analysis, reviewed the draft manuscript, and approved it for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Due to the retrospective nature of the study, the need to obtain the informed consent was waived by the Institutional Review Board (IRB) of the College of Health Sciences of Bahir Dar University approved the study, with study protocol number 730/2023. The IRB performs following the Declaration of Helsinki, the International Conferences on Harmonisation (ICH) Good Clinical Practice, the WHO Operating Guidelines for Ethical Review Committee and the National Guideline for Research Ethics in Ethiopia. The Amhara Public Health Institute (APHI) reviewed the ethical approval protocols and requested that the selected hospitals and health centres provide records of TB/HIV treatment follow-up data to the authors. Accordingly, the health facilities’ patient charts or ART follow-up forms were used. The name of the patient was not included in the checklist. The data of any patient were not used for other purposes other than for the aim of this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Demelash, R., Hailu, G., Abuhay, T. et al. A competing risk analysis of predictors of time to lost to follow-up among adults with TB/HIV coinfection in Bahir Dar. Sci Rep 15, 30362 (2025). https://doi.org/10.1038/s41598-025-15985-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15985-8