Abstract
The co-occurrence of central sensitization syndromes (CSS) and post-traumatic symptoms (PTSS) or post-traumatic stress disorder (PTSD) exacerbates impairment, and treatment is unsatisfactory in many cases. This systematic review and meta-analysis examined the effectiveness of psychological therapy in individuals with CSS and comorbid PTSS/PTSD. A search of Medline, PsycInfo, Web of Science, Pubmed, and Scopus databases (2000 to 2023) was conducted following PRISMA guidelines. Nineteen articles were selected, including nine for meta-analysis. The main psychological therapies were pain-focused cognitive-behavioral therapy (P-CBT), and trauma-focused interventions, mainly written emotional disclosure (WED) and emotional awareness and expression therapy (EAET). Both EAET and P-CBT showed potential benefits in improving pain severity (specially EAET), PTSS/PTSD, emotional distress, fatigue, sleep disturbances, CSS-related symptoms, and quality of life. Overall, no significant differences were found between the two interventions. The meta-analysis revealed a large effect size for EAET in reducing pain and emotional distress; however, most comparison were against inactive controls, so results should be interpreted cautiously. These findings underscore the importance of distinguishing CSS patients with PTSS/PTSD. Tailored treatments such as EAET can address the additive impact of these conditions and contribute to improving patients’ quality of life.
Similar content being viewed by others
Introduction
In the field of chronic pain, which is pain that lasts more than 3 months1, there is a relevant set of conditions where medical tests fail to detect abnormalities that can be proven to be their cause. These pain syndromes have been referred to by various term, including unexplained chronic pain or nociplastic pain, although central sensitization syndromes (CSS) is the most widely used term2. Conditions classified as CSS include fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, tension headaches and migraines, and most cases of temporomandibular, pelvic, abdominal and back chronic pain3,4.
In terms of clinical symptoms, CSS conditions show high comorbidity among them and share sleep disturbances, fatigue, cognitive-affective alterations and significative life adversity2. Although the pathogenesis of CSS remains unclear, current research has observed a state of central sensitization (CS) in many of these conditions, defined as hyperexcitability in the pain neuromatrix or increased responsiveness of nociceptive neurons to normal or subthreshold afferent input, resulting in localized and generalized hyperalgesia and allodynia (painful response to non-painful stimuli)5.
The mechanisms that lead to the state of CS are not clear although the relevance of psychosocial factors has been highlighted. The biopsychosocial model proposed by Adam and Turk2 underscores the importance of considering individual pain experiences and identifying the biological, psychological, and social factors influencing how symptoms are experienced. Several cognitive-affective characteristics can act as predisposing and/or maintenance factors of CSS, being pain catastrophizing, depression or anxiety some of the most studied aspect2,6. Furthermore, it has recently been emphasized that the presence of trauma is higher among CSS patients versus healthy controls and other chronic pain patients4,7,8. It is estimated that up to 40% of individuals with CSS could have post-traumatic stress symptoms (PTSS) or post-traumatic stress disorder (PTSD), while up to 75% of individuals with PTSS/PTSD report CSS9. Individuals exposed to childhood trauma are up to two times more likely to develop CSS conditions10. However, estimates vary widely depending on the type of CSS and the context of sample collection. For example, only a 3.8% of veterans in the general US population reported both PTSD and chronic pain11; while in a sample of veterans collected in a healthcare setting, 21.6% of those with chronic pain also had PTSD, and over half (53.2%) of those with PTSD met the criteria for chronic pain12. The co-occurrence of chronic pain and PTSS/PTSD exacerbates pain, affective distress, and disability compared to those with either chronic pain or PTSS/PTSD alone11,12,13, worsening the prognosis and further complicating the treatment of both conditions9,14.
Several theoretical models have been proposed to explain the complex relationships between trauma, PTSD, and chronic pain. The mutual maintenance model focuses on how chronic pain and PTSD are maintained after the conditions develop15. It proposes that symptoms of pain evoke PTSD symptoms and vice versa, each of which is worsened by enhanced attention to threats, reasoning biases, anxiety sensitivity, trauma-related memories of pain, behavioral avoidance, depression, and low activity. In contrast, vulnerability models as the shared vulnerability model16 focus on predispositions that increase the likelihood of developing both conditions in response to trauma. The shared vulnerability model suggests that disability results from individual factors, such as anxiety sensitivity, cognitive biases, selective attention to threat, and a lower alarm threshold due to sympathetic dysregulation16. Reed et al.17 recently highlighted the existential gaps in the current theoretical models and proposed an integrated model of co-occurring chronic pain and PTSD. This model combines Park’s meaning-making model18 with the shared vulnerability model16, and mutual maintenance model15. Both chronic pain and PTSD are often characterized by maladaptive interpretations, attributions, or personal narratives that disrupt, or are incongruent with one’s broader sense of life’s meaning17. Making meaning out of an event is an important component of processing the experience of chronic pain or a potentially traumatic event, and can lead to disability due to co-occurring chronic pain and PTSD. This process is also complicated by other existential factors, as existential anxiety that increases psychological vulnerability and reduce the alarm threshold17. The model outline other several testable hypotheses of the interplay between existential concerns, chronic pain and PTSD.
Comorbidity between chronic pain and PTSS/PTSD poses enormous treatment challenges. Clinical practice guidelines (e.g., fibromyalgia guidelines19,20) recommend a multidisciplinary treatment approach for CSS comprising physical exercise, psychological therapy, and minimal medication. Regarding psychological treatment, both cognitive-behavioral therapy (CBT) and acceptance and commitment therapy (ACT) have demonstrated efficacy and significant benefits compared to other active treatments, although the effect of both therapies on pain relief has been limited21,22. Concerning the treatment of PTSD, trauma-focused therapies such as prolonged exposure, cognitive processing therapy, cognitive therapy for PTSD, and eye movement desensitization and reprocessing therapy (EMDR) are widely recommended and supported by strong evidence23,24. These therapies are considered first-line treatments for managing CSS and PTSD separately, but there are no formal guidelines for treating PTSD and chronic pain together, and there is little evidence on response to treatment for the both conditions9,25. In one study, pain symptoms did not decrease until the PTSD symptoms were addressed and vice versa26; while in other study an intensive, outpatient interdisciplinary pain rehabilitation program focusing on functional restoration (physical recondicioning and activity pacing) combinated with CBT improve pain interference (86.7%) and PTSD outcomes (50.6%), as well as depressive symptoms, physical performance, and medication use, despite the fact that PTSD symptoms were not explicitly targeted as a part of treatment27.
A narrative review of six psychological interventions —mostly uncontrolled—conducted in refugees with PTSS/PTSD and CSS28 concluded that CBT with biofeedback, Narrative Exposure Therapy (NET), manualized trauma psychotherapy, Traditional Chinese Medicine and emotional freedom techniques may yield positive effects on both pain severity and PTSD symptoms. However, heterogeneity between studies prevent comparison between them. An other systematic review29 of seven studies suggest that various multicomponent treatment approaches—including psychoeducation, cognitive restructuring, exposure techniques, muscular progressive relaxation or biofeedback—were effective in reducing PTSS, and improving pain adaptation and quality of life. Nevertheless, most interventions did not result in significant improvements in pain intensity. Importantly, only three of the reviewed studies included a control group, and in most cases, participants received other uncontrolled medical treatment alongside psychological treatment, limiting the ability to isolate the effect of psychological therapy. Lumley et al.25 conducted a narrative highlighting the benefits of Emotional Awareness and Expression Therapy (EAET), an intervention derived from short-term psychodynamic psychotherapies, as well as emotion-focused and exposure-based approaches. EAET was specifically developed for patients with CSS and integrates pain neuroscience education with identification and expression of avoided emotions. In contrast to interventions that address PTSS/PTSD or CSS separately —often yielding limited improvements in pain intensity—, two uncontrolled studies and four randomized controlled trials (RCT) evaluating EAET for the combined treatment of PTSD and pain reported significant reductions in pain intensity and somatic symptoms compared to waitlist controls, psicoeducation or CBT. Although a notable restriction remains in the absence of PTSS/PTSD evaluation in the analyzed studies.
Thus, despite the relevance of underestanding the specific response of individuals with comorbid CSS and PTSS/PTSD to psychological interventions—given the wide range of physical and psychological symptoms they experience and the substantial healthcare burden this population represents9,11,12,13,14—existing reviews suffer from methodological limitations. Previous reviews on CSS and PTSS/PTSD combine predominantly uncontrolled studies with a few RCTs28,29, do not account for the concurrent use of other interventions29, and include studies that group CSS with other types of pain without specifically assessing the presence of PTSS/PTSD25,28,29. Additionally, in some cases, the population studied are restricted to refugees, further limiting genralizability28.
The aim of this systematic review and meta-analysis, as articulated by the Population, Intervention, Comparator, Outcome and Study design (PICOS) statement30, was to analyze, in individuals with comorbid CSS and PTSS/PTSD (P), the efficacy of psychological therapy (I) compared to other interventions or, in their absence, standard medical care (C) in improving physical (pain, fatigue, and sleep) and psychological (anxiety, depression, PTSS/PTSD, and quality of life) variables (O), considering randomized and nonrandomized clinical trials (S).
Results
Characteristics of the included studies
Supplementary Table 1 contains the 19 studies analyzed in this review. The studies are listed in alphabetical order by the first author’s name, along with their main characteristics.
Study context and participants
Studies were conducted in Denmark31, Australia32, Germany33,34, Kosovo35, Norway36, and the United States37,38,39,40,41,42,43,44,45,46,47,48,49.
There was heterogeneity in terms of the type of CSS of the sample. Twelve studies assess and identify the specific type of CSS: fibromyalgia38,40,41,43, chronic urogenital pain or pelvic pain39,44,45, irritable bowel syndrome42,47, chronic back pain31,33, and headache46. Other included somatoform disorders or medically unexplained symptoms (mainly chronic pain)34,49, whiplash-related chronic pain32, and the remaining studies assessed general chronic pain without medical cause35,36,37,48.
Five studies31,32,34,35,37 also included the PTSD diagnostic criteria in their inclusion criteria, one study36 included patients who reported severe PTSD symptoms, and one study33 incorporated exposure to at least one psychologically traumatic event as part of its inclusion criteria. One study48 included war veterans with co-occurring general chronic pain, in which PTSS/PTSD was presumed due to the characteristics of the sample. The remaining studies38,39,40,41,42,43,44,45,46,47,49 did not directly assess PTSS/PTSD but reported a high percentage of traumatic events and/or suspected PTSS/PTSD related to the onset of pain syndromes.
The sample sizes across the studies varied widely, ranging from 26 to 230 participants. A total of 1504 participants were included in the systematic review. The weighted average age of the participants was 42.68 (11.59) years. In terms of sex distribution, a majority of the studies (n = 14) included both male and female participants, four studies38,39,44,45 included exclusively female participants, and one study41 did not specify the sex distribution of the sample. The total percentage of females in the sample was 82.70%, taking into account that four studies had missing data.
Treatments
The majority of the therapies applied in the experimental conditions can be classified into three general categories: pain-focused cognitive-behavioral therapy (P-CBT)32,34,35,36,37; written emotional disclosure (WED)38,40,42,44; and emotional awareness and expression therapy (EAET)39,41,43,46,47,48,49. The remaining studies differed widely in terms of treatment approaches. One study33 used pain-focused eye movement desensitization and reprocessing therapy (P-EMDR), other study31 applied somatic experiencing (SE) therapy, and one study45 applied interpersonal psychotherapy for pain (IPT-P).
Methodological characteristics
All the studies were randomized controlled trials, except one34, which was nonrandomized. Many studies have provided incomplete information regarding the protocol of the treatment applied. The duration of therapy ranged from 3 to 36 weeks, with total therapy hours varying from 1.5 to 28 h distributed across 3 to 20 sessions. Almost all session frequencies were weekly and applied in group-based43,47, individual48,49, or mixed35 formats.
The active control comparison conditions consisted of pain-focused cognitive-behavioral therapy (P-CBT)14,48, written positive emotional experience44, fibromyalgia-education (FM-E)43, and relaxation training (RT)46,47. Passive control conditions consisted of a waitlist (WL) control group32,35,36,46,47, treatment as usual (TAU)31,33,34,38,39,41,45,49, neutral written (NW)38,40,42, and minimum contact comparison group (MCC)37. It is to interest to note that four studies38,43,46,47 were three-arm controlled trials.
A first follow-up assessment was performed in all the studies, within a time frame ranging from 2 weeks to 12 months. A second follow-up assessment was conducted in six studies35,38,40,42,45,47 within a time frame ranging from 3 to 24 months. Two studies35,45 performed a third follow-up assessment at 9 months and at 36 months.
Risk of bias in studies
A summary of the risk of bias assessment for each included study is provided in Supplementary Fig. 1. Concerns about bias were identified in 42% of the studies (n = 8), five of which showed a high risk of bias33,34,37,42,45.
None of the studies included in this systematic review evaluated patients with a comorbid diagnosis of a specific CSS and PTSD. Only Kruse et al.34 evaluated patients with somatoform disorders (mainly pain) and PTSD according to the DSM-IV criteria. Somatoform disorders involves an experience of physical symptoms without a clear physical cause that when it consists of pain, it is indistinguishable from CSS4.
Result of syntheses
Pain
For the analysis of this outcome, we considered only the severity of pain. Four studies did not analyze this component34,44,45,47. Ten studies showed an improvement in pain in the experimental group31,37,38,39,40,41,43,46,48,49. Notably, all the studies evaluating trauma-focused therapy in CSS patients38,39,40,41,43,46,49 reported positive pain outcomes, except for one42. Three studies compared treatment with an active control condition. Lumley et al.43 found no differences between EAET and P-CBT but did find a significant difference between EAET and FM-E. Slavin-Spenny et al.46 reported no difference between AAET and RT, and Yarns et al.48 reported a significant difference between EAET and P-CBT. Among the passive control conditions, five studies showed significant differences between groups: Broderick et al.38 compared WED with TAU and NW; Carty et al.39 compared EAET-I with TAU; Hsu et al.41 compared ASA with TAU; Slavin-Spenny et al.46 compared AAET with WL; and Ziadni et al.49 compared EAET with TAU. Three studies did not find differences between groups: Andersen et al.31 compared SE with TAU; Beck et al.37 compared GCBT with MCC; and Gillis et al.40 compared WED with NW.
PTSS/PTSD
Six studies evaluated PTSS/PTSD31,32,34,35,36,37, and all of which reported improvement in PTSS/PTSD, except for one36 that found no changes. The samples of the studies consisted of war torture victims35, war refugees36, individuals with chronic pain (whiplash) related to a vehicle accident32,37, individuals with low back pain31 and patients with somatoform disorders34. All the treatments applied were trauma-focused therapies (SE31, TF-CBT32, TFP34, IT35, TRT36, GCBT37) and were compared with a passive control condition (TAU31,34, WL32,35,36, MCC37).
Anxiety and depression
Eleven studies have assessed anxiety and depression32,35,37,38,39,43,45,46,47,48,49. Pain diagnostics were CSS38,39,43,45,46,47,48,49, and generalized chronic pain32,35,37. All the studies applied trauma-focused therapies, except for one45 that applied pain-focused therapy. All the studies reported a decrease in anxiety and depression, except for one39 that found no changes. However, among passive control conditions, three studies35,38,47 showed significant differences that were not maintained at follow-up. When compared with active control conditions, Lumley et al.43 found no significant difference between EAET and P-CBT, but EAET differed significantly from FM-E; Thakur et al.47 showed a nonsignificant difference between EAET and RT; Slavin-Spenny et al.46 did not find differences between AAET and RT; and Yarns et al.48 observed a significant reduction in anxiety but not in depression, in EAET compared to P-CBT conditions, at posttreatment, although the differences becomes non-significant at follow-up .
Sleep and fatigue
Two studies assessed fatigue symptoms, and both analyzed the efficacy of trauma-focused therapy in patients with fibromyalgia. Gillis et al.40 observed a not statistically significant reduction in fatigue in WED condition compared with NW condition. Lumley et al.43 reported no differences between EAET and P-CBT, but compared to FM-E, treatment resulted in a significantly lower fatigue score.
Three studies evaluated sleep outcomes38,41,43, and all of which applied trauma-focused therapy (GCBT38, ASA41, EAET43) to patients with fibromyalgia. The results suggested that treatment had a positive effect on sleep quality compared to MCC38, TAU41 and FM-E43 control conditions, but the effect size appeared to be small, and there was no additional benefit compared with pain-focused therapy (P-CBT43).
CSS symptoms
Two studies assessed CSS symptoms, and both examined the efficacy of trauma-focused therapies in patients with irritable bowel syndrome. Thakur et al.47 reported a positive effect of EAET treatment compared to WL passive condition, but the effect size was small and did not differ from the active RT treatment. Laird and Stanton42 did not find a significant difference in CSS symptoms between WED and NW groups; however, statistically significant small-to-medium sized effects were observed over time across groups.
Quality of life
Three studies assessed quality of life, all of which examined the efficacy of trauma-focused therapies in patients with CSS. Broderick et al.38 reported no significant difference of the WED condition compared to the NW passive condition. Thakur et al.47 found a significant difference between EAET treatment compared to WL passive condition, but not compared to the RT condition. Laird and Stanton42 did not observe significant difference between WED condition compared to the NW passive condition; although the quality of life increased over time in both groups.
Meta-analysis
For the quantitative synthesis of the results, studies using the same instruments were selected. The measures considered were pain (Brief Pain Inventory, BPI50) and emotional distress (Brief Symptom Inventory, BSI51).
For pain, seven studies were included36,39,40,41,43,48,49, and for emotional distress, four studies were included39,46,47,49. The Dersemonian and Laird Q tests revealed heterogeneity in both variables, Q (x2) = 131.93, p = 0.000, and Q (x2) = 151.66, p = 0.000, respectively, leading to the adoption of a random-effects model. A significant and large overall effect of psychological treatment was observed for both pain (d = − 1.29, 95% CI − 2.22; − 0.36) and emotional distress (d = − 0.95, 95% CI − 2.86; 0.97). In the domain of pain, the study by Carty et al.39 comparing the EAET-Interview (EAET-I) with the TAU showed the largest effect size (d = − 3.45, large effect). Conversely, for emotional distress, the study by Ziadni et al.49, comparing the EAET-I with the TAU, exhibited the largest effect size (d = − 3.02, large effect) (Figs. 1 and 2, and Table 1).
Sensitivity analysis showed that removing any of the studies did not impact the overall direction of the effect for the analyzed variables (Table 2), although the magnitude was slightly affected. For pain, Begg’s test (z = 1.50, p = 0.133) and Egger’s test (t = − 1.38, p = 0.225) indicated the absence of publication bias, but for emotional distress Begg’s test (z = 1.70, p = 0.090) and Egger’s test (t = − 17.99, p = 0.003) suggested the presence of publication bias.
Discussion
This systematic review and meta-analysis aimed to evaluate the efficacy of psychological therapy in patients with CSS and comorbid PTSS/PTSD, compared to other interventions or passive control conditions, considering randomized and nonrandomized trials. Overall, the systematic review found that psychological treatment significantly improved both chronic pain and PTSS/PTSD. Additionally, psychological therapy also had a positive effect on emotional distress, sleep, fatigue, CSS symptoms and quality of life. The meta-analysis showed a significantly large overall effect of psychological treatment on both pain severity and emotional distress.
Ten of the nineteen studies included in the systematic review showed an improvement in pain severity in the experimental group31,37,38,39,40,41,43,46,48,49. Notably, all the studies evaluating trauma-focused therapy (WED, AAET and EAET), in CSS patients38,39,40,41,43,46,49 reported positive effect on pain, except one using WED in bowel irritable syndrome42. Most of these studies used passive controls, although three included active controls. Among them, Lumley et al. found that EAET is better than psicoeducation, while no differences were observed between EAET and P-CBT in fibromyalgia43, and Slavin-Spenny found no differences between AAET and RT in chronic headache46. In contrast, Yarns et al.48 reported significantly greater improvement in pain severity with EAET compared to P-CBT in war veterans with chronic general pain. Studies that did not report changes in pain severity mostly included samples with unspecified chronic pain conditions and PTSS/PTSD, treated with trauma-focused therapies. It is possible that these unspecified chronic pain conditions may have included aspects that are not typical of CSS and that this has been associated with a worse response. Similarly, the review of Reyes-Pérez et al.29, which also includes general chronic pain conditions, also finds no changes in pain intensity. In addition, the positive effect of trauma-focused therapies, especially EAET, on pain severity in CSS with PTSS/PTSD aligns with Lumley’s25 narrative review, which sowed EAET to outperform waitlist controls, psicoeducation or P-CBT on pain relief21,22.
Concerning PTSS/PTSD, five studies that evaluated PTSS/PTSD in CSS and chronic pain due to whiplash and somatoform disorders, find improvement in these measures with a diversity of interventions as somatic experiencing (SE)31, several approach based on P-CBT32,35,37, and a trauma-focused psychotherapy (TFP; skills training in affect regulation and improvement of interpersonal relationships)34 compared with passive controls. Only one study with war refugees36 found no changes using a multi-component program called Teaching Recovery Techniques (TRT) that includes various TF-CBT techniques. These results are in line with the suggestions of Gilliam et al. study27 who found that a pain rehabilitation program focusing on functional restoration and CBT improve pain interference (but no pain severity), and also PTSD outcomes. Similarly, the reviews of Rometsch-Ogioun El Sount et al.28, and Reyes-Pérez et al.29 concluded that P-CBT or TF-CBT were effective in reducing PTSD symptoms, although the majority did not achieve changes in pain intensity.
In addition to improvements in pain severity and PTSS/PTSD, psychological interventions positively impacted the remaining clinical measures evaluated. Eleven studies assessing anxiety and depression reported reductions with trauma-focused therapies —mainly EAET —and P-CBT in both CSS and general chronic pain samples32,35,37,38,39,43,45,46,47,48,49, except for one study using interpersonal therapy (IPT-P) in chronic pelvic pain45. Only five of these studies included active controls; among them, EAET was superior to psychoeducation43 but not to P-CBT or RT43,46,47,48. Similarly, two studies assessing fatigue40,43, and three evaluating sleep quality38,41,43 in fibromyalgia, found positive effects of trauma-focused therapies (WED and EAET) though not significantly different from P-CBT. Also, two studies examining other CSS symptoms42,47 showed improvement with WED and EAET, with no differences between EAET and RT in the only study with active control47. Three studies assessing quality of life reported improvement with WED and EAET38,42,47, with no differences between EAET and RT in the only study with active control47. These findings are consistent with the narrative review of Lumley et al.25 highlighting the benefits of EAET and related emotion-focused and exposure therapies not only on pain but also on somatic symptoms when compared to waitlist or psicoeducation. Besides, EAET is an approach derived from Short-term psychodynamic psychotherapies (STPP), and there is meta-analytic evidence that STPP outperformed TAU or waitlist controls on somatic symptom measures, and on secondary measures of anxiety, depression, general symptoms, and physical function in patients with functional somatic syndromes —another way of referring to CSS —although this work does not consider comorbidity with PTSS/PTSD4.
Finally, our meta-analysis showed a significant and large overall effect of psychological treatment for both pain (d = − 1.29) and emotional distress (d = − 0.95). The seven studies included that assessed pain severity36,39,40,41,43,48,49, used mainly trauma-focused therapies as WED, ASA and specially EAET, on CSS and general chronic pain, highlighting the large effect size found in the study by Carty et al. 46 (d = − 3.45) who applied EAET-I in chronic pelvic pain. Four studies evaluated emotional distress39,46,47,49, also employing trauma-focused therapies (AAET and AEET), on several conditions of CSS and general chronic pain, drawing attention the study by Ziadni et al.49, comparing the EAET-I with the TAU in medical inexplained symtoms, with the largest effect size (d = − 3.02).
In short, trauma-focused therapy options, mainly EAET, seem to be an effective intervention reducing pain severity in CSS patients and other general chronic pain conditions with PTSS/PTSD. EAET outperformed passive controls, psicoeducation43, and P-CBT48 in one study but not in other43. A diversity of interventions, mainly based on P-CBT, and in one case trauma-focused therapy (TFP), achieve improvement in PTSS/PTSD compared with passive controls. Also, P-CBT approaches but mainly trauma-focused therapies (especially EAET) achieve improvements in emotional distress, fatigue, sleep, CSS symptoms and quality of life, with EAET outperforming passive controls, psicoeducation and, in general, with no differences with P-CBT. Our meta-analysis also reinforces the large overall effect of EAET on pain severity, and of EAET-I on emotional distress in CSS and general chronic pain. The overall positive effects of the treatments were generally maintained during follow-ups compared with passive control groups.
An important limitation of this review is the heterogeneity of the sample in terms of specific CSS and other nonspecific chronic pain conditions as well as the type of trauma and severity of PTSS/PTSD. Considering the shared etiopathogenesis of CSS that emphasizes the impact of trauma on stress regulation systems and on pain processing at the CNS level13,15,17, the meta-analysis included studies with diverse CSS, ensuring that the findings can be generalized to a varied population. However, given such heterogeneity, it would also have been of interest to carry out a subgroup analysis (population or intervention), although it could not be carried out due to not having the number of studies (at least 3) necessary for such an analysis. Another important limitation relates to differences in outcome variables and assessment instruments used between studies. In addition, the applied treatments were diverse, although the majority could be classified as trauma-focused or pain-focused therapy. Trauma-focused therapies show favorable results, however, it must be noted that most of the comparison groups have been waitlist or treatment-as-usual, not active controls. Without more head-to-head trials, the usefulness of this therapeutic approach, although hopeful, must be taken with caution. Trauma-focused therapy in CSS is an emerging area of research that may have great potential to help people with these comorbid conditions. However, as evidenced by our review, there are few studies that to date have addressed this issue, and most of the studies analyzed have included follow-up periods of six months or less, which prevents drawing conclusions about the stability of the improvements over time. Future research is needed to understand the impact of trauma-focused therapy compared to other therapies with proven efficacy in CSS samples and be able to answer questions about the efficiency and stability of treatments over time. Besides, studies are necessary that examine the impact of trauma-focused therapies on central sensitization through objective measures such as electrophysiological and neuroimaging tests.
Both EAET and P-CBT are of interest for achieve improvement in pain severity (specially EAET), PTSS/PTSD, emotional distress, fatigue, sleep, CSS symptoms and quality of life in CSS comorbid with PTSS/PTSD in general, with no differences between them. This raises the question of whether both types of treatments overlap in their therapeutic goal or if they have similar effects on outcomes by targeting different therapeutic objectives due to shared mechanism between CSS and PTSD as proposed by the mutual maintenance model15, the shared vulnerability model16, or the recent model of co-occuring chronic pain and PTSD17.
The results of this systematic review and meta-analysis have important clinical implications. Actually, psychological treatment guidelines often address chronic pain within a unified framework19,20,21,22, without making distinctions between patient profiles. Future studies should consider distinguishing between patients with and without PTSD within the CSS population that may benefit from tailored treatments to address the additive impact of these conditions. Patients with CSS and PTSS/PTSD show significant improvements in pain severity with trauma-focused psychotherapy, which is particularly relevant given their poor therapeutic response to other conventional treatments. Differentiating the effects of pain-focused CBT and trauma-focused therapy in these two subgroups could provide valuable insights into the mechanisms of action of both types of treatments. This specificity can clarify the comprension of the complex relationship between trauma, CSS and PTSS/PTSD, and increase the efficacy, effectiveness and efficiency of treatment, reducing asistential cost, and, most importantly, enhancing quality of life of patients.
Method
For the conduct of this systematic review, the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline was followed52.
Sources of information and search strategy
A rigorous bibliographic search was conducted through electronic databases, including Medline, PsycInfo, Web of Science, Pubmed, and Scopus, spanning from 2000 to 2023. The search algorithm was: (“central sensitization syndrome” OR “fibromyalgia” OR “chronic fatigue syndrome” OR “irritable bowel syndrome” OR “temporomandibular joint disorder” OR “tension-type headache” OR “migraine” OR “chronic pelvic pain” OR “chronic pain”) AND (“trauma” OR “posttraumatic stress disorder”) AND (“therapy” OR “intervention”). Studies identified manually from the reference lists of the selected studies were also included. Additionally, the identification of relevant references was complemented by a comprehensive examination of “gray literature”. The search was conducted during August 2023.
Eligibility criteria
The following eligibility criteria were used for article selection: (EC1) include a primary diagnosis of chronic pain related to central sensitization, that is, chronic pain not directly linked with a clear injury, tissue damage, inflammation, or disease (ICD-1053; ICD-1154); (EC2) have experienced psychosocial trauma and/or exhibited PTSS or comorbid PTSD (DSM-IV55/IV-TR56; DSM-557/5-TR58; ICD-1053; ICD-1154) based on information collected by clinical interviews (e.g., Structured Clinical Interview DSM-IV, SCID) and/or standardized questionnaire that allow to measure both the severity of symptoms and the PTSD diagnosis (e.g., Harvard Trauma Questionnaire); (EC3) focused on analyzing the efficacy of bona fide psychotherapies (based on evidence) and not combined with treatments from other healthcare disciplines (e.g., medicine, physiotherapy, pharmacology, etc.) in order to identify its specific effects; (EC4) to be a randomized or nonrandomized controlled clinical trial; and (EC5) published in Spanish or English.
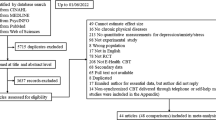
Search process and article selection
The authors CM and JMVL independently searched for and selected the articles. A total of 1534 references were identified, 1516 of which were obtained from electronic databases and 17 from manual searches. After removing duplicates from the database-derived references (n = 735), 799 references were selected for more detailed analysis based on the eligibility criteria. Initially, articles were screened based on title and abstract, with 746 excluded for not meeting the eligibility criteria. Subsequently, 52 articles were subjected to full-text examination to assess relevant information about the methods and results. Among these, 33 articles were excluded for not meeting the established eligibility criteria, resulting in a total of 19 articles being selected for the systematic review (9 randomized controlled trials were included in the meta-analysis). Supplementary Fig. 2 illustrates the process from article identification to the selection of relevant studies.
Results coding
To analyze the information gathered from the selected articles, the following data were compiled: authors, year of publication, main study objectives, research design, sociodemographic information (number of participants, sex, age), clinical characteristics (specific CSS, type of trauma and age when it occurred, PTSS/PTSD or other psychological sequelae), outcome measures, type of intervention (number of participants, content of the therapeutic programme, frequency, duration, and format of sessions), control conditions (number of participants, content, and format of the intervention), and main results.
Risk of bias assessment
The methodological quality of the selected studies was assessed using the Cochrane Collaboration Risk of Bias tool59. This assessment was conducted by CM and JMVL and reviewed by CM, JMVL and MPM. Discrepancies were resolved through consensus.
Data analysis
The meta-analysis was performed when three or more studies included the necessary data on the variables of interest. Analyses were conducted using Epidat 4.2 software60, considering the option of standardized mean differences. The statistical variability between studies was calculated using the DerSimonian and Laird heterogeneity test, which provides the between-study variance, within-study variance, coefficient of variation between studies, and the RI coefficient representing the proportion of total variance due to variance between studies and, therefore, takes values between 0 and 1. A 95% confidence interval was used. To represent the results, a forest plot was generated. The effect size (d) was interpreted according to the recommendation of Cohen61: 0.20, 0.50, and 0.80 indicating small, medium, and large effect sizes, respectively. Publication bias was assessed using the Begg and Egger tests. A sensitivity analysis was performed to assess the influence of each study on the overall effect estimate. The effect sizes of trauma-focused therapies (Anger Awareness and Expression Training -AAET-, Affective Self-Awareness -ASA-, Emotional Awareness and Expression Therapy -EAET-, Emotional Awareness and Expression Interview -EAET-I-, Teaching Recovery Techniques -TRT-, Written Emotional Disclosure -WED-, trauma-focused CBT-TF-CBT), pain-focused therapies (Pain-Focused CBT -P-CBT-, Relaxation Training -RT-) and passive control conditions (Neutral Writing -NW-, Treatment as Usual –TAU-, Waitlist control group -WL-) on pain and emotional distress were compared.
Data availability
The data will be made available on request to the corresponding author: cmaire@correo.ugr.es.
References
Raja, S. N. et al. The revised international association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 161, 1976–1982 (2020).
Adams, L. & Turk, D. Psychosocial factors and central sensitivity syndromes. Curr. Rheumatol. Rev. 11, 96–108 (2015).
Yunus, M. Editorial review (thematic issue: an update on central sensitivity syndromes and the issues of nosology and psychobiology). Curr. Rheumatol. Rev. 11, 70–85 (2015).
Abbass, A. et al. Short-term psychodynamic psychotherapy for functional somatic disorders: A meta-analysis of randomized controlled trials. Psychother. Psychosom. 89, 363–370 (2020).
Den Boer, C. et al. Central sensitization in chronic pain and medically unexplained symptom research: A systematic review of definitions, operationalizations and measurement instruments. J. Psychosom. Res. 117, 32–40 (2019).
Forman, L. S. & Turk, D. Central sensitization and the biopsychosocial approach to understanding pain. J. Appl. Biobehav. Res. 23, e12125 (2018).
Karimov-Zwienenberg, M., Symphor, W., Peraud, W. & Décamps, G. Childhood trauma, PTSD/CPTSD and chronic pain: A systematic review. PLoS ONE 19, e0309332 (2024).
Kleykamp, B. A. et al. The prevalence of psychiatric and chronic pain comorbidities in fibromyalgia: An ACTTION systematic review. Semin. Arthritis Rheum. 51, 166–174 (2021).
Goldstein, E. et al. The impact of psychological interventions on posttraumatic stress disorder and pain symptoms: A systematic review and meta-analysis. Clin. J. Pain 35, 703–712 (2019).
Chandan, J. S. et al. The association between exposure to childhood maltreatment and the subsequent development of functional somatic and visceral pain syndromes. EClinicalMedicine 23, 100392 (2020).
Reed, D. E., Fischer, I. C., Williams, R. M., Na, P. J. & Pietrzak, R. H. Co-occurring chronic pain and PTSD among US military veterans: Prevalence, correlates, and functioning. J. Gen. Intern. Med. 39, 2009–2016 (2024).
Hadlandsmyth, K., Zhuang, C., Driscoll, M. A. & Lund, B. C. Comorbid chronic pain and post-traumatic stress disorder: Current rates and psychiatric comorbidities among U.S. military veterans. Mil. Med. 189, 2303–2306 (2024).
Lehinger, E. et al. An examination of chronic pain indices and the updated posttraumatic stress disorder checklist for diagnostic and statistical manual of mental-disorders-fifth edition. Mil. Med. 186, e1199–e1206 (2021).
Lumley, M. A. & Schubiner, H. Emotional awareness and expression therapy for chronic pain: Rationale, principles and techniques, evidence, and critical review. Curr. Rheumatol. Rep. 21, 30 (2019).
Sharp, T. J. & Harvey, A. G. Chronic pain and posttraumatic stress disorder: mutual maintenance?. Clin. Psychol. Rev. 21, 857–877 (2001).
Reed, D. E., Cobos, B., Nabity, P., Doolin, J. & McGeary, D. D. Comorbid chronic pain and posttraumatic stress disorder: Current knowledge, treatments, and future directions, in Pain Care Essentials and Innovations 211–227 (Elsevier, 2021). https://doi.org/10.1016/B978-0-323-72216-2.00015-6
Reed, D. E., Williams, R. M., Engel, C. C. & Zeliadt, S. B. Introducing the integrated model of co-occurring chronic pain and posttraumatic stress disorder: Adding meaning-making and existential concepts to current theory. Psychol. Trauma Theory Res. Pract. Policy 17, 563–575 (2025).
Park, C. L. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychol. Bull. 136, 257–301 (2010).
The Washington Manual Rheumatology Subspecialty Consult. (Wolters Kluwer, Philadelphia, 2021).
Handa, R. Fibromyalgia, in Clinical Rheumatology 197–199 (Springer, 2021). https://doi.org/10.1007/978-981-33-4885-1_24
Kang, J.-H., Choi, S.-E., Park, D.-J. & Lee, S.-S. Disentangling diagnosis and management of fibromyalgia. J. Rheum. Dis. 29, 4–13 (2022).
Williams, J. R., Cole, V., Girdler, S. & Cromeens, M. G. Exploring stress, cognitive, and affective mechanisms of the relationship between interpersonal trauma and opioid misuse. PLoS ONE 15, e0233185 (2020).
Ackland, P. E. et al. Implementation of evidence-based psychotherapies for posttraumatic stress disorder: A systematic review. Adm. Policy Ment. Health Ment. Health Serv. Res. 50, 792–812 (2023).
Mansour, M. et al. Post-traumatic stress disorder: A narrative review of pharmacological and psychotherapeutic interventions. Cureus https://doi.org/10.7759/cureus.44905 (2023).
Lumley, M. A., Yamin, J. B., Pester, B. D., Krohner, S. & Urbanik, C. P. Trauma matters: Psychological interventions for comorbid psychosocial trauma and chronic pain. Pain 163, 599–603 (2022).
Otis, J. D., Keane, T. M., Kerns, R. D., Monson, C. & Scioli, E. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med. 10, 1300–1311 (2009).
Gilliam, W. P. et al. Examining the effectiveness of pain rehabilitation on chronic pain and post-traumatic symptoms. J. Behav. Med. 43, 956–967 (2020).
Rometsch-Ogioun El Sount, C. et al. Chronic pain in refugees with posttraumatic stress disorder (PTSD): A systematic review on patients’ characteristics and specific interventions. J. Psychosom. Res. 118, 83–97 (2019).
Reyes-Perez, A. et al. Psychological intervention for post-traumatic stress disorder comorbid to chronic musculoskeletal and primary pain: a systematic review. Rev. Mex. Psicol. 37, 77–91 (2020).
Amir-Behghadami, M. & Janati, A. Population, Intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med. J. 37, 387–387 (2020).
Andersen, T. E., Lahav, Y., Ellegaard, H. & Manniche, C. A randomized controlled trial of brief somatic experiencing for chronic low back pain and comorbid post-traumatic stress disorder symptoms. Eur. J. Psychotraumatology 8, 1331108 (2017).
Dunne, R. L., Kenardy, J. & Sterling, M. A randomized controlled trial of cognitive-behavioral therapy for the treatment of PTSD in the context of chronic whiplash. Clin. J. Pain 28, 755–765 (2012).
Gerhardt, A. et al. Eye movement desensitization and reprocessing vs. treatment-as-usual for non-specific chronic back pain patients with psychological trauma: A randomized controlled pilot study. Front. Psychiatry 7, 201 (2016).
Kruse, J., Joksimovic, L., Cavka, M., Wöller, W. & Schmitz, N. Effects of trauma-focused psychotherapy upon war refugees: Psychotherapy With Refugees. J. Trauma. Stress 22, 585–592 (2009).
Wang, S.-J. et al. A novel bio-psycho-social approach for rehabilitation of traumatized victims of torture and war in the post-conflict context: A pilot randomized controlled trial in Kosovo. Confl. Health 10, 1–17 (2017).
Hasha, W. et al. Effect of a self-help group intervention using teaching recovery techniques to improve mental health among Syrian refugees in Norway: A randomized controlled trial. Int. J. Ment. Health Syst. 16, 47 (2022).
Beck, J. G., Coffey, S. F., Foy, D. W., Keane, T. M. & Blanchard, E. B. Group cognitive behavior therapy for chronic posttraumatic stress disorder: An initial randomized pilot study. Behav. Ther. 40, 82–92 (2009).
Broderick, J. E., Junghaenel, D. U. & Schwartz, J. E. Written emotional expression produces health benefits in fibromyalgia patients. Psychosom. Med. 67, 326–334 (2005).
Carty, J. N. et al. The effects of a life stress emotional awareness and expression interview for women with chronic urogenital pain: A randomized controlled trial. Pain Med. 20, 1321–1329 (2019).
Gillis, M. E., Lumley, M. A., Mosley-Williams, A., Leisen, J. C. C. & Roehrs, T. The health effects of at-home written emotional disclosure in fibromyalgia: A randomized trial. Ann. Behav. Med. 32, 135–146 (2006).
Hsu, M. C. et al. Sustained pain reduction through affective self-awareness in fibromyalgia: A randomized controlled trial. J. Gen. Intern. Med. 25, 1064–1070 (2010).
Laird, K. T. & Stanton, A. L. Written expressive disclosure in adults with irritable bowel syndrome: A randomized controlled trial. Complement. Ther. Clin. Pract. 43, 101374 (2021).
Lumley, M. A. et al. Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: A cluster-randomized controlled trial. Pain 158, 2354–2363 (2017).
Norman, S. A., Lumley, M. A., Dooley, J. A. & Diamond, M. P. For whom does it work? Moderators of the effects of written emotional disclosure in a randomized trial among women with chronic pelvic pain. Psychosom. Med. 66, 174–183 (2004).
Poleshuck, E. L. et al. Randomized controlled trial of interpersonal psychotherapy versus enhanced treatment as usual for women with co-occurring depression and pelvic pain. J. Psychosom. Res. 77, 264–272 (2014).
Slavin-Spenny, O., Lumley, M. A., Thakur, E. R., Nevedal, D. C. & Hijazi, A. M. Effects of anger awareness and expression training versus relaxation training on headaches: A randomized trial. Ann. Behav. Med. 46, 181–192 (2013).
Thakur, E. R. et al. Emotional awareness and expression training improves irritable bowel syndrome: A randomized controlled trial. Neurogastroenterol. Motil. 29, e13143 (2017).
Yarns, B. C. et al. Emotional awareness and expression therapy achieves greater pain reduction than cognitive behavioral therapy in older adults with chronic musculoskeletal pain: A preliminary randomized comparison trial. Pain Med. 21, 2811–2822 (2020).
Ziadni, M. S. et al. A life-stress, emotional awareness, and expression interview for primary care patients with medically unexplained symptoms: A randomized controlled trial. Health Psychol. 37, 282–290 (2018).
Cleeland, C. S. & Ryan, K. M. Pain assessment: Global use of the brief pain inventory. Ann. Acad. Med. Singapore 23, 129–138 (1994).
Derogatis, L. R. & Melisaratos, N. The brief symptom inventory: An introductory report. Psychol. Med. 13, 595–605 (1983).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 10, 89 (2021).
The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines (World Health Organization, 1992).
World Health Organization. International Classification of Diseases Eleventh Revision (ICD-11). https://icd.who.int/en (2022).
Diagnostic and Statistical Manual of Mental Disorders, 4th Ed. xxvii, 886 (American Psychiatric Publishing, Inc., 1994).
Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR (American Psychiatric Association, 2000).
Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (American Psychiatric Association, 2013).
Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR (American Psychiatric Association Publishing, 2022).
Higgins, J. P. T. et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928–d5928 (2011).
Consellería de, S., Xunta de, G. España, organización panamericana de la salud (OPS-OMS) & universidad CES, Colombia. Epidat: programa para análisis epidemiológico de datos (2016).
Cohen, J. Statistical power analysis for the behavioral sciences (Academic Press, 1977).
Acknowledgements
This study is part of a broader research project supported by the Spanish Ministry of Science and Innovation and Spanish State Research Agency (project PID2019-109612GB-I00, funded by MCIN/AEI/https://doi.org/10.13039/501100011033).
Funding
This study is part of a broader research project supported by the Spanish Ministry of Science and Innovation and Spanish State Research Agency (project PID2019-109612 GB-I00, funded by MCIN/AEI/https://doi.org/10.13039/501100011033).
Author information
Authors and Affiliations
Contributions
C.M. drafted the protocol, conducted searches, analysed data, and drafted the manuscript. J.M.V.L. conducted searches, analysed data, and drafted and reviewed the manuscript. A.I.S. drafted the protocol, provided supervision, guided the research question, assisted with clinical interpretation of results, and reviewed manuscript drafts. E.M. drafted the protocol, provided supervision, guided the research question, assisted with clinical interpretation of results and reviewed manuscript drafts. M.P.M. drafted the protocol, analysed data, provided supervision, guided the research question, assisted with clinical interpretation of results, and reviewed manuscript drafts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Maire, C., Sánchez, A.I., Ventura-Lucena, J.M. et al. Psychological intervention in patients with central sensitization syndromes and comorbid psychosocial trauma: a systematic review and meta-analysis. Sci Rep 15, 30896 (2025). https://doi.org/10.1038/s41598-025-16074-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-16074-6