Abstract
Continuous Passive Motion (CPM) has been widely used in rehabilitation, yet its effectiveness compared to conventional physical therapy (PT) following elbow contracture release remains unclear. This retrospective cohort study evaluated the effectiveness of home-based immersive CPM training versus manual PT in promoting functional recovery of the elbow. Clinical records of 40 patients with moderate to severe elbow osteoarthritis who underwent standardized arthroscopic release between 2020 and 2022 were reviewed. Among them, 20 patients received home-based CPM rehabilitation, and 20 underwent conventional PT. After a 3-month follow-up, the CPM group demonstrated superior improvements in range of motion (ROM), with an estimated increase of \(13.5^{\circ }\) (95% CI, 7 to 20; p = 0.005), and a higher percentage increase in ROM (83.03% vs 61.29%, p = 0.01). The likelihood of attaining functional ROM was 35% greater in the CPM group (risk ratio 1.35; 95% CI, 1.02 to 1.78; p = 0.03), and Mayo Elbow Performance Score (MEPS) scores were significantly higher, with a 6-point difference (95% CI, 2 to 10; p = 0.02). Furthermore, CPM was more cost-efficient, with monthly rehabilitation costs of 500 RMB compared to 2850 RMB for PT. The primary outcome was ROM improvement, and secondary outcomes included MEPS scores, functional ROM attainment, and rehabilitation cost. As this was a retrospective study based on existing clinical records, trial registration was not required. This study was approved by the Medical Ethics Committee of Cangzhou Fifth Hospital (Approval No. QXRMYY202003). In conclusion, home-based immersive CPM rehabilitation was associated with greater ROM improvements, better pain management, and enhanced functional recovery compared to conventional PT in patients recovering from elbow surgery.
Similar content being viewed by others
Introduction
Degenerative elbow stiffness is a common clinical condition and is one of the main causes of elbow joint stiffness. Its pathological features include joint space narrowing, extensive lip-like osteophyte proliferation, and obstruction of elbow movement1,2. The prevalence of degenerative elbow stiffness in the general population is approximately 2%3, particularly affecting middle-aged and elderly men engaged in heavy upper limb labor, such as construction workers, Chinese chefs, and upper limb athletes4. Elbow stiffness can be classified into four levels based on the extension-flexion arc: an arc of \(\le 30^\circ\) indicates extremely severe stiffness, \(31^\circ\) to \(60^\circ\) represents severe stiffness, \(61^\circ\) to \(90^\circ\) is considered moderate, and an arc greater than \(90^\circ\) is classified as mild stiffness5. Limitations exceeding 50\(^{\circ }\) in elbow flexion or rotation result in an 80% loss of daily functional abilities6. To effectively treat these significant functional impairments, surgical intervention has become an important consideration.
The complex anatomy of the elbow joint, combined with its high stability requirements and the relatively lax joint capsule, makes it prone to stiffness due to osteophyte formation, loose bodies, and joint capsule contracture7. To address this issue, surgical intervention, particularly arthroscopic release, has become a key treatment strategy8. Arthroscopic release allows thorough treatment of intra-articular and periarticular pathological tissue, achieving comprehensive release with minimal trauma9. Given its safety, efficacy, and minimal invasiveness, arthroscopic elbow release techniques have gained significant attention and are gradually becoming the preferred approach over open surgery10. Following surgical intervention, appropriate rehabilitation is essential to maximize recovery outcomes.
Rehabilitation following surgical release of elbow stiffness presents unique challenges due to the difficulty of restoring complete functional movement11. Current rehabilitation methods include Continuous Passive Motion (CPM), Physical Therapy (PT), splinting, or a combination of these approaches12. Preclinical studies suggest that CPM may be more effective than immobilization or intermittent motion, as it promotes fluid clearance from the joint and periarticular tissues, potentially preventing joint stiffness more effectively13. Based on these findings and the demonstrated safety of CPM in clinical use over the past several decades, it has been widely adopted in many institutions as the preferred rehabilitation protocol following elbow contracture release14,15,16. However, there is a lack of robust clinical trials directly comparing CPM with other rehabilitation methods, such as PT, to determine their relative efficacy17,18. To fill this gap, we conducted a randomized controlled trial comparing CPM and PT in patients undergoing arthroscopic release of elbow contracture, hypothesizing that CPM would result in faster recovery and improved range of motion compared to PT19.
Despite the widespread use of CPM and PT in clinical rehabilitation, there is limited high-quality evidence comparing their effectiveness specifically in patients with moderate to severe elbow stiffness following arthroscopic release. Existing studies often focus on knee or shoulder joints, and findings may not be generalizable to the elbow, which has unique anatomical and functional characteristics. Moreover, practical considerations such as treatment cost, accessibility of home-based rehabilitation, and long-term functional outcomes remain underexplored in this context.
Therefore, a targeted clinical evaluation comparing CPM and PT is warranted to guide evidence-based rehabilitation protocols tailored to elbow stiffness recovery. This study aims to provide clinically relevant insights into the comparative effectiveness and cost-efficiency of immersive home-based CPM versus conventional PT, thereby helping optimize postoperative care and improve long-term functional outcomes in patients undergoing arthroscopic release of elbow contracture.
Methods
Participants
We retrospectively selected 60 patients with elbow osteoarthritis (degenerative elbow stiffness) who underwent arthroscopic release in our department, before and after September 1, 2023. Institutional Review Board approval and informed consent were obtained for this study. Based on the inclusion criteria-such as moderate to severe elbow joint stiffness with ineffective conservative treatment for over 3 months, confirmed osteoarthritis through imaging, complete case and follow-up data, and no surgery-related complications-and exclusion criteria-including synovial diseases, post-traumatic adhesions, severe elbow stiffness, local infection, poor compliance, or neuromuscular injuries-40 participants were ultimately selected, as shown in Fig. 1.
To reduce evaluation bias, a single-blind design was implemented, in which outcome assessors were blinded to group allocation, while patients were aware of their treatment assignments due to the nature of the interventions. Since patients with extremely severe elbow joint stiffness have poor preoperative joint function and are few in number, which could introduce data bias, this study focused on patients with moderate to severe elbow joint stiffness. All surgeries were performed by the author, who was well-trained and experienced in elbow arthrolysis. The CPM training group included 14 males and 6 females, with an age range of 42 to 70 years (mean age 57.29 years). There were 13 right elbows and 7 left elbows, with 5 cases accompanied by ulnar nerve symptoms. The duration of the condition ranged from 6 months to 10 years, with an average of 5.5 years. The PT group included 17 males and 3 females, with an age range of 45 to 78 years (mean age 58.13 years). There were 17 right elbows and 3 left elbows, with 4 cases accompanied by ulnar nerve symptoms. The duration of the condition ranged from 3 months to 7 years, with an average of 4.3 years. All patients had restricted elbow joint motion, with or without pain, radiographic findings consistent with degenerative changes of the elbow joint, and a history of more than 3 months without effective conservative treatment.
The participant flow is illustrated in a CONSORT diagram (Fig. 2), which details the screening, enrollment, group allocation, follow-up, and analysis stages. A total of 60 patients were initially assessed for eligibility. Among them, 20 were excluded (15 did not meet the inclusion criteria and 5 declined to participate). The remaining 40 patients were randomly assigned to either the CPM group or the manual PT group, with 20 patients in each arm. All participants completed the intervention and follow-up protocols, and no loss to follow-up or treatment interruptions occurred.
Surgical technique
The patient was placed in the lateral decubitus position under general anesthesia with a tourniquet. After routine disinfection and draping, a small incision of approximately 4 cm was made along the ulnar nerve path based on surface landmarks, to isolate and protect the ulnar nerve. Following O’Driscoll’s four-step method20, the procedure involved: establishing the approach, creating space, removing osteophytes, and excising the joint capsule. Through the proximal anteromedial and anterolateral approaches, the anterior compartment of the elbow was treated, involving synovectomy, osteophyte grinding, removal of loose bodies, and joint capsule excision21. Both medial and lateral approaches were alternated to expose the anterior muscular tissues of the elbow.
Subsequently, the posterior compartment was accessed via posterolateral, posteromedial, and soft spot approaches to comprehensively observe the olecranon fossa, posteromedial groove, posterolateral groove, and the dorsum of the radiocapitellar joint under arthroscopy. The posterior capsule was released, osteophytes were removed, and the posterior bundle of the medial collateral ligament was released. One or two drainage tubes were placed, and the incision was sutured. The elbow was fixed in an extended position using a polymer splint.
Postoperation treatment
After the operation, all patients received immediate local cold compress on the elbow joint, along with indomethacin (25 mg TID) or celecoxib (40 mg BID) for pain relief and to reduce the occurrence of heterotopic ossification, continuing for 4 to 8 weeks postoperatively. Follow-up included X-ray and CT scans to assess the extent of surgical release, as well as examinations of the median, ulnar, and radial nerve functions. We now provide a detailed description of the rehabilitation protocols for both the PT and CPM groups, highlighting the differences in their approaches.
PT Group: Starting from the first postoperative day, patients were guided through a gradual functional exercise program. This included both active and passive flexion-extension exercises of the elbow joint, as well as finger spreading, finger pinching, and gripping exercises. Passive flexion-extension was performed by a rehabilitation therapist, adhering strictly to a gradual progression principle, with each session reaching the maximum tolerance of the patient. Training was conducted once daily, followed immediately by cold compress for 20 minutes. On the fourth postoperative day, if the incision showed no signs of exudation, patients were discharged and instructed to visit our hospital or a local rehabilitation facility daily for manual training conducted by a rehabilitation therapist, including massage and manipulation.
CPM Group: Four hours post-surgery, the plaster cast was removed, and patients began gradual functional training using CPM. The initial range of motion was set at 0-15\(^\circ\) or the maximum angle tolerated by the patient, with incremental increases once pain subsided. During training, intermittent cold therapy was provided every three hours for 20 minutes to alleviate pain and swelling.
Evaluation index
The effectiveness of the CPM rehabilitation plan will be assessed using three key evaluation indices: Range of Motion (ROM), Mayo Elbow Performance Score (MEPS), and Visual Analog Scale (VAS) for pain. Each of these indices provides a comprehensive measure of the patient’s progress in joint mobility, functionality, and pain management.
-
Range of Motion (ROM): ROM measures the degree of movement in the elbow joint, including flexion, extension, pronation, and supination of the elbow joint22. An improvement in ROM indicates greater flexibility and mobility of the joint, which is one of the primary goals of the CPM rehabilitation. Regular measurements will be taken at specific intervals (e.g., 2 weeks, 1 month, and 2 months post-surgery) to monitor the progress in joint movement.
-
Mayo Elbow Performance Score (MEPS): The MEPS is a scoring system that evaluates elbow function based on four domains: pain, range of motion, stability, and elbow function23. The total score ranges from 0 to 100 points, with higher scores indicating better elbow performance. A score between 90 and 100 is considered excellent, 75 to 89 is good, 60 to 74 is fair, and less than 60 is classified as poor. The Minimal Clinically Important Difference (MCID) for the MEPS is 15 points, meaning that a change of at least 15 points is required to reflect a clinically meaningful improvement24. This index will be used to gauge the improvement in overall elbow health and functionality.
-
Visual Analog Scale (VAS) for Pain Assessment: Postoperative pain intensity was assessed using the VAS, a validated and widely used instrument in clinical pain evaluation25. Patients were asked to rate their subjective pain levels on a scale ranging from 0 (no pain) to 10 (worst imaginable pain). VAS scores were recorded at 2 weeks, 1 month, and 3 months postoperatively during scheduled follow-up visits. This quantitative assessment enabled the evaluation of pain reduction trends over time and between groups, thereby facilitating objective analysis of the analgesic effectiveness of CPM versus PT interventions.
By using these three evaluation indices-ROM, MEPS, and VAS-the rehabilitation plan’s impact on joint mobility, overall function, and pain management can be systematically measured and analyzed, ensuring a comprehensive understanding of the patient’s recovery progress.
Home-based CPM rehabilitation plan
On the fourth postoperative day, if the incision showed no signs of exudation, patients were discharged to continue their rehabilitation at home using CPM. To facilitate recovery from elbow stiffness or surgery, a comprehensive home-based CPM rehabilitation plan was developed as shown in Fig. 3. This plan outlines a step-by-step approach to safely and effectively use CPM machines at home, promoting long-term improvement in joint mobility, pain reduction, and overall recovery.
The effectiveness of this rehabilitation plan will be regularly evaluated using key metrics such as ROM, MEPS, and VAS for pain. Data will be systematically collected at specific intervals-2 weeks, 1 month, and 2 months post-surgery-to monitor progress, ensuring that rehabilitation goals are consistently achieved and sustained, as summarized in Table 1.
CPM training was performed using a motorized device set at a standard passive flexion–extension frequency of approximately 45 cycles per minute. Each training session lasted up to 4 hours per cycle, after which the device would automatically pause. Patients could manually pause the session at any time for rest or to attend to physiological needs. While the recommended daily training duration was approximately 20 hours, this was not mandatory. The 20-hour suggestion was based on observed high-frequency use among real-world patients in our department, where patients voluntarily extended training time to alleviate morning rebound stiffness. Some patients chose to continue CPM training during nighttime hours, although it was not enforced. Patients were encouraged to adjust CPM usage based on comfort and sleep quality. No unified guidelines currently exist regarding optimal CPM duration for postoperative elbow rehabilitation; thus, our recommendation reflects practical experience from clinical implementation.
Rehabilitation interventions
The CPM protocol involved the use of a home-based device that provided passive elbow joint mobilization at a frequency of 45 cycles per minute. To ensure patient safety and avoid fatigue, the device was programmed to stop automatically after 4 hours of continuous operation, with patients free to manually pause the device for rest or physiological needs. Although a total daily duration of up to 20 hours was recommended, this was not mandatory. The suggested duration was based on cumulative clinical experience and real-world observations, where certain patients voluntarily adopted high-frequency CPM usage for symptom relief-particularly to mitigate early morning stiffness. Conversely, others discontinued nighttime use when it interfered with sleep. This flexible, patient-centered protocol allowed for individualized adjustments according to pain tolerance, comfort, and rehabilitation goals. At present, no standardized clinical guidelines define the optimal daily CPM dosage for elbow rehabilitation; thus, this approach reflects an adaptive and pragmatic solution developed in clinical practice.
In contrast, the manual PT protocol consisted of therapist-guided active and passive ROM exercises, progressive stretching, soft tissue mobilization, and functional task training. Patients received two sessions per day during hospitalization and continued with three outpatient sessions per week after discharge, for a total duration of up to 12 weeks. Each session lasted approximately 60 minutes. Therapists dynamically adjusted treatment intensity based on patient-specific factors such as pain sensitivity, joint stiffness, and tissue responsiveness. The early rehabilitation phase focused on inflammation control and ROM restoration, whereas later phases emphasized neuromuscular re-education, proprioception, and strength training. Home exercises were prescribed for non-clinic days, and adherence was monitored through rehabilitation logs and weekly therapist consultations. This protocol followed current evidence-based recommendations for postoperative elbow rehabilitation and was individually tailored by licensed rehabilitation professionals.
Statistical analysis
This section outlines the procedures for data collection, statistical tests for evaluating outcome changes over time, and the strategy used to address missing data. Additionally, a cost-effectiveness analysis (CEA) was conducted to compare the financial efficiency of CPM and PT rehabilitation.
Data collection and follow-up schedule
Postoperative follow-up was scheduled at 2 weeks, 1 month, and 3 months after surgery. Follow-ups were conducted either in person or via online consultations. Imaging data, including computed tomography (CT) and 3D reconstructions of the elbow joint, were acquired from local hospitals and reviewed collaboratively by the surgical team.
Statistical methods for outcome comparison
Statistical analyses were conducted using SPSS version 26.0. Continuous variables were presented as means ± standard deviations (\(x \pm s\)). Repeated-measures analysis of variance (ANOVA) was used to evaluate outcome changes across the three time points. Mauchly’s test was applied to assess the assumption of sphericity. If sphericity was violated, the Greenhouse-Geisser correction was employed to adjust the degrees of freedom. Bonferroni post-hoc tests were used for pairwise comparisons. Levene’s test was used to evaluate homogeneity of variance. A p-value of less than 0.05 was considered statistically significant.
Missing data management
Missing data from follow-up visits were handled using the Last Observation Carried Forward (LOCF) method. This imputation technique carried forward the last available measurement for any missing time point, thereby maintaining data continuity for repeated-measures ANOVA and reducing attrition-related bias.
Cost-effectiveness analysis
To evaluate the cost-effectiveness of home-based CPM rehabilitation versus conventional PT, we conducted a cost-effectiveness analysis (CEA) over a 30-day postoperative rehabilitation period. The analysis was carried out from the patient’s perspective, focusing on direct medical expenses.
The total monthly cost for the PT group was calculated based on the average outpatient rehabilitation fees (200–300 RMB per session) obtained from representative hospitals across different provinces in China. Assuming one session per day, the estimated cost was no less than 2,850 RMB. Transportation expenses and opportunity costs (e.g., time off work) were not included. For the CPM group, the primary cost was the fixed monthly rental fee of the device (500 RMB), with minimal or no additional expenses.
Cost-effectiveness was assessed by calculating the cost-effectiveness ratio (CER), defined as the cost required to achieve one unit of functional improvement. Two CERs were calculated, based on improvements in range of motion (ROM) and Mayo Elbow Performance Score (MEPS), respectively. The CER was defined by the following formula:
In this formula, \(C_{\text {total}}\) denotes the total cost of rehabilitation over one month, and \(\Delta \text {Effectiveness}\) represents the change in outcome (either ROM or MEPS) from baseline to 3 months:
These formulas allowed us to compare the relative efficiency of CPM and PT rehabilitation strategies in terms of clinical improvement per unit cost. This pragmatic analysis provides contextually relevant economic information for clinical decision-making, particularly in resource-constrained settings.
This study was designed as a retrospective cohort analysis. Therefore, formal randomization and allocation concealment were not applicable. Group assignments (CPM vs. PT) were based on post-discharge rehabilitation records, reflecting real-world clinical decisions. Despite the non-randomized design, the two groups demonstrated comparable baseline characteristics, which helped reduce selection bias. To evaluate whether the sample size was sufficient, a post hoc power analysis was performed based on the between-group difference in ROM at postoperative day 2. Using the formula for Cohen’s d and the observed group means and standard deviations, the calculated effect size was \(d = 3.93\), yielding a statistical power of over 99% at a significance level of \(\alpha = 0.05\). This confirms that the available sample size (n = 40) was adequate to detect clinically meaningful differences. Regarding measurement tools, ROM was assessed using a standard goniometer by two independent orthopedic surgeons. Pain was measured using the VAS, and functional recovery was evaluated with the MEPS. All three instruments are validated and widely accepted in orthopedic clinical research for their reliability and sensitivity.
Results
This section presents the postoperative outcomes comparing patients who received home-based CPM rehabilitation with those who underwent conventional PT. The analysis includes five key domains: surgical safety and follow-up adherence, improvements in elbow ROM, functional recovery as measured by the MEPS, postoperative pain assessed using the VAS, and a comprehensive comparison of rehabilitation costs. Statistical comparisons between groups are provided at multiple postoperative time points to evaluate the efficacy and cost-effectiveness of the two rehabilitation approaches.
ROM result
Firstly, all patients underwent successful surgeries and were discharged. The ROM of patients in the PT and CPM groups was compared before surgery and at follow-up (Table 2). Preoperatively, both groups had similar ROM values (69.75\(^\circ\) for PT and 69.25\(^\circ\) for CPM). At two weeks postoperatively, the CPM group showed a significantly greater improvement (105.05\(^\circ\)) compared to the PT group (94.05\(^\circ\)), with a statistically significant difference (\(P = 0.001\)). At three months postoperatively, the CPM group achieved a mean ROM of 126.75\(^\circ\), which was significantly higher than the PT group’s mean ROM of 112.50\(^\circ\) (\(P = 0.00\)).
As shown in Table 2, the difference in ROM between the CPM and PT groups at three months postoperatively was 14.25\(^\circ\), which could have a significant impact on the patients’ daily lives. An increased range of elbow motion, particularly for flexion, can greatly enhance the ability to perform activities such as eating, grooming, and using a computer keyboard comfortably. For example, tasks like holding a phone to the ear or reaching for objects in the kitchen become easier with greater elbow flexion. Therefore, the additional 14.25\(^\circ\) of ROM gained by the CPM group compared to the PT group provides noticeable improvements in daily functional activities, contributing to a better quality of life for the patients.
At three months postoperatively, all patients in both groups showed significant improvement in elbow joint ROM, and the ROM continued to improve over time. The overall ROM of the experimental group was significantly better than the control group, and there was a significant difference in the ROM changes between the two groups (P < 0.001). The experimental group showed more significant ROM improvements after surgery. The interaction effect indicated that the intervention effect of the grouping enhanced with time, with the greatest intergroup difference observed at three months postoperatively (see Table 2). These results suggest that CPM training can improve elbow joint mobility in patients (Table 3).
MEPS result
Subsequently, we compared the elbow joint MEPS scores (points) for the PT group and the CPM group at different time points: before operation (preoperative), 2 weeks after operation (2W), and 3 months after operation (3M) in Table 4. Both groups showed improvement in MEPS scores over time. Specifically, the PT group’s mean score increased from 72.50 ± 6.19 pre-operatively to 83.25 ± 3.35 at 2 weeks and 90.50 ± 5.60 at 3 months. Similarly, the CPM group’s mean score improved from 74.00 ± 11.07 pre-operatively to 86.75 ± 3.35 at 2 weeks and 96.50 ± 4.90 at 3 months.
As shown in Table 4, a paired t-test analysis showed significant improvements within each group from Pre-op to 3 months, with t-values of -13.08 (P = 0.00) for the PT group and -8.82 (P = 0.00) for the CPM group, indicating marked recovery in both groups. However, comparisons between the two groups revealed significant differences in the 2-week and 3-month intervals, with t-values of -3.30 (P = 0.002) and -3.61 (P = 0.001), respectively. This suggests that the CPM Group had a significantly higher improvement in MEPS scores compared to the PT Group during these post-operative periods (Table 5).
VAS pain score analysis
Postoperative pain levels were systematically evaluated using the Visual Analog Scale (VAS) at eight critical time points: pre-operation (baseline), 4 hours, 1 day, 2 days, 3 days, 4 days, 2 weeks, and 3 months after surgical intervention.
Table 6 presents the longitudinal VAS score measurements for both treatment groups (PT and CPM). Notably, the groups demonstrated comparable baseline pain levels (PT: \(0.90 \pm 0.64\) vs CPM: \(1.10 \pm 0.97\), \(p > 0.05\)). The immediate postoperative period (4 hours) revealed a paradoxical pain pattern, with the CPM group reporting significantly higher VAS scores (\(3.26 \pm 0.81\)) compared to the PT group (\(1.15 \pm 0.59\), \(p < 0.001\)). This relationship inverted during days 1-2 post-operation, where the PT group exhibited substantially elevated pain levels (\(4.90 \pm 1.08\) and \(4.50 \pm 1.05\) respectively) versus the CPM group (\(1.26 \pm 0.56\) and \(1.00 \pm 0.67\), both \(p < 0.001\)).
The subsequent recovery phase (days 3-4) showed progressive pain reduction in the PT group, while the CPM group maintained consistently low pain scores. By week 2, both groups achieved significant pain relief, though residual differences persisted (PT: \(1.45 \pm 0.86\) vs CPM: \(0.47 \pm 0.51\), \(p = 0.003\)). At the 3-month follow-up, pain levels converged to minimal values (PT: \(0.50 \pm 0.61\) vs CPM: \(0.11 \pm 0.32\), \(p = 0.082\)), indicating comparable long-term outcomes.
Table 7 demonstrates significant main effects for both time (F(4.98,184.23)=88.95, \(p < 0.001\), \(\eta ^2\)=0.946) and treatment group (F(1,37)=101.44, \(p < 0.001\), \(\eta ^2\)=0.733), with the CPM group showing overall lower pain scores (\(1.06 \pm 0.11\)) compared to PT (\(2.54 \pm 0.10\)).
Table 8 reveals a significant time\(\times\) group interaction (F(4.98,184.23)=100.75, \(p < 0.001\), \(\eta ^2\)=0.940), confirming the differential temporal pain patterns between groups. Post-hoc analysis with Bonferroni correction confirmed the CPM group maintained superior pain control during the acute phase (days 1-4, all \(p < 0.001\)).
All analyses employed Greenhouse-Geisser correction where appropriate. The CPM group (n=20) demonstrated significantly better acute pain control compared to PT (n=20), though long-term outcomes were equivalent. All reported p-values are Bonferroni-adjusted.
Cost comparison between CPM and PT rehabilitation
We have also counted the daily recovery costs for patients in the PT group. Based on the patient’s residential area, we have calculated the daily recovery costs, as shown in Table 9.
Finally, we compare the approximate rehabilitation costs for patients using CPM machines versus conventional PT during the recovery period in Table 10. The CPM group has a relatively low and fixed monthly cost of 500 RMB, which only covers the rental of the CPM machine. Based on hospital costs (Table 9), the average daily cost across all listed hospitals is approximately 283.64 RMB. The lowest-cost hospital is Qing County People’s Hospital, with an estimated cost range of 80-110 RMB per day. Taking the midpoint value of 95 RMB, the cost for a one-month recovery (30 days) would be 2,850 RMB. Additionally, the PT group may face extra transportation costs for daily hospital visits, making the CPM method a more affordable and convenient rehabilitation option for patients.
Finally, we compared the cost-effectiveness of CPM and PT interventions by calculating the cost-effectiveness ratio (CER), defined as the cost required to achieve one unit of functional improvement. As shown in Table 11, the CPM group achieved a \(\Delta\)ROM of 57.5\(^{\circ }\) and a \(\Delta\)MEPS of 22.5 points, resulting in CER-ROM and CER-MEPS values of 8.70 RMB/\(^{\circ }\) and 22.22 RMB/pt, respectively. In contrast, the PT group showed a \(\Delta\)ROM of 42.75\(^{\circ }\) and a \(\Delta\)MEPS of 18.0 points, corresponding to CERs of 66.67 RMB/\(^{\circ }\) and 158.33 RMB/pt. These results indicate that CPM rehabilitation is markedly more cost-effective in terms of both joint mobility and functional score improvements.
Discussion
After elbow arthrolysis, although the physical barriers to joint movement have been removed, the surrounding muscles and ligaments still remain shortened26. It requires long-term exercise to gradually stretch them back to their normal length27,28. Currently, the most common post-operative rehabilitation for orthopedic surgery is passive training, primarily conducted in rehabilitation departments or hospitals under the guidance of rehabilitation physicians. This implies that all rehabilitation exercises can only be performed intermittently, with the physician’s guidance or assistance, leading to severe pain during the initial and progressive phases of training, as shown in Table 6. This intense pain can affect the patient’s rest, reduce their motivation for rehabilitation, and lead to negative or resistant emotions, ultimately impacting the training process and the surgical outcome, sometimes even causing failure29. Additionally, the inconvenience of prolonged hospital stays or frequent hospital visits, combined with the significant time and financial costs, gradually wears down the patient’s resolve.
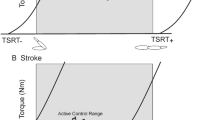
Therefore, painless or minimally painful postoperative rehabilitation training is a prerequisite for elbow joint functional recovery30,31. CPM refers to the continuous passive movement of the joint under the influence of external mechanical forces32. By promoting blood circulation and lymphatic return in the limbs, CPM reduces limb swelling and also promotes the circulation and metabolism of joint fluid33, facilitating the regeneration of fibrocartilage and preventing adhesions, thereby increasing the pain threshold. Its safety, efficacy, and pain-free nature are its greatest advantages. The joint capsule regenerates during continuous elbow motion, preventing re-contracture, making CPM highly suitable for postoperative rehabilitation following elbow release. Two rehabilitation modes are shown in Fig. 4.
Based on the ROM (Table 2), MEPS scores (Table 4), VAS scores (Table 6), and rehabilitation costs (Table 10) of the two patient groups, our study demonstrated that CPM significantly improved elbow joint flexibility and reduced pain in postoperative patients compared to conventional PT. To further illustrate the practical benefits of CPM, we present two cases involving middle-aged men: one who underwent CPM training, as shown in Fig. 5, and another who received conventional PT training, as depicted in Fig. 6.
Table 12 shows a significant difference in total rehabilitation costs between Case 1 (PT training) and Case 2 (CPM training). Case 1 assumed 60 days of PT at Qingxian People’s Hospital (Table 10) at a minimum cost of RMB 95 per day, totaling RMB 5700. In contrast, Case 2 involved 2 months of CPM training at RMB 500 per month, totaling RMB 1000. The hospitalization costs were similar: RMB 13540 for Case 1 and RMB 13620 for Case 2. The total cost for Case 1 was RMB 19780, while for Case 2 it was RMB 14620. Therefore, CPM training in Case 2 is more cost-effective, mainly due to the lower rehabilitation costs. Case 2 saved RMB 5160 compared to Case 1, which is a cost reduction of approximately 26%.
This study has several limitations that should be noted: (1) As a retrospective study, the findings are susceptible to selection bias. (2) The sample size (n=40), while comparable to than similar studies, may not be sufficient to detect smaller, yet clinically meaningful effects, which limits the generalizability of the results to a wider population with varied characteristics. (3) The unequal distribution of genders between groups may introduce biases related to gender-specific factors, such as anatomical and hormonal differences, which could affect rehabilitation outcomes.
Conclusion
This single-blind retrospective cohort study involving 40 patients with elbow osteoarthritis compared the efficacy of home-based CPM rehabilitation to conventional PT following arthroscopic release of degenerative elbow stiffness. Blinding was applied to outcome assessors, while patients were aware of their assigned interventions. At the 3-month follow-up, the CPM group showed superior outcomes in terms of range of motion (ROM), functional recovery, and pain control, along with higher patient-reported satisfaction and faster recovery. CPM was also associated with significantly lower rehabilitation costs, highlighting its economic advantage over conventional PT.
In conclusion, home-based immersive CPM rehabilitation offers a clinically meaningful and cost-effective strategy for managing postoperative elbow stiffness. Given its affordability (500 RMB/month), ease of implementation, and demonstrated benefits in ROM and functional outcomes, CPM provides evidence-based guidance for clinicians to optimize postoperative care. These findings support prioritizing CPM in rehabilitation protocols to improve recovery efficiency and enhance the overall patient experience.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.
References
Siemensma, M. F., van der Windt, A. E., van Es, E. M., Colaris, J. W. & Eygendaal, D. Management of the stiff elbow: A literature review. EFORT Open Rev. 8, 351–360. https://doi.org/10.1530/EOR-23-0039 (2023).
Masci, G. et al. The stiff elbow: Current concepts. Orthop. Rev. 12, 8661 (2020).
Morrey, B., Askew, L. & Chao, E. A biomechanical study of normal functional elbow motion. J. Bone Jt. Surg. 63, 872–877. https://doi.org/10.2106/00004623-198163060-00002 (1981).
Nakayama, K. et al. Prevalence and associated factors of primary elbow osteoarthritis in the Japanese general elderly population: A Japanese cohort survey randomly sampled from a basic resident registry. J. Shoulder Elbow Surg. 31, 123–132. https://doi.org/10.1016/j.jse.2021.07.015 (2022).
Kim, S.-J., Moon, H.-K., Chun, Y.-M. & Chang, J.-H. Arthroscopic treatment for limitation of motion of the elbow: The learning curve. Knee Surg. Sports Traumatol. Arthrosc. 19, 1013–1018. https://doi.org/10.1007/s00167-010-1334-7 (2011).
Sivakumar, R., SomaSheker, V., Shingi, P. K., Vinoth, T. & Chidambaram, M. Treatment of stiff elbow in young patients with interpositional arthroplasty for mobility: case series. J. Orthop. Case Rep. 6, 49. https://doi.org/10.13107/jocr.2250-0685.566 (2016).
Martinez-Catalan, N. & Sanchez-Sotelo, J. Primary elbow osteoarthritis: Evaluation and management. J. Clin. Orthop. Trauma 19, 67–74. https://doi.org/10.1016/j.jcot.2021.05.002 (2021).
Pettersen, P. M. et al. Increased rom and high patient satisfaction after open arthrolysis: A follow-up-study of 43 patients with posttraumatic stiff elbows. BMC Musculoskelet. Disord. 17, 1–6. https://doi.org/10.1186/s12891-016-0928-8 (2016).
Kukreja, M., Kang, J., Curry, E. J. & Li, X. Arthroscopic lysis of adhesions and anterior interval release with manipulation under anesthesia for severe post-traumatic knee stiffness: A simple and reproducible step-by-step guide. Arthrosc. Tech. 8, e429–e435. https://doi.org/10.1016/j.eats.2019.01.005 (2019).
Gallay, S., Richards, R. & O’Driscoll, S. Intraarticular capacity and compliance of stiff and normal elbows. Arthrosc. J. Arthrosc. Relat. Surg. 9, 9–13. https://doi.org/10.1016/S0749-8063(05)80336-6 (1993).
Everding, N. G., Maschke, S. D., Hoyen, H. A. & Evans, P. J. Prevention and treatment of elbow stiffness: A 5-year update. J. Hand Surg. 38, 2496–2507. https://doi.org/10.1016/j.jhsa.2013.06.007 (2013).
Richter, M., Trzeciak, T. & Kaczmarek, M. Effect of continuous passive motion on the early recovery outcomes after total knee arthroplasty. Int. Orthop. 46, 549–553. https://doi.org/10.1007/s00264-021-05245-5 (2022).
Knapik, D. M. et al. The basic science of continuous passive motion in promoting knee health: A systematic review of studies in a rabbit model. Arthrosc. J. Arthrosc. Relat. Surg. 29, 1722–1731 (2013).
Tille, E. et al. Early functional improvements using continuous passive motion therapy after angular-stable plate osteosynthesis of proximal humerus fractures-results of a prospective, randomized trial. J. Orthop. Surg. Res. 19, 1–10. https://doi.org/10.1186/s13018-024-04804-x (2024).
Viveen, J. et al. Continuous passive motion and physical therapy (CPM) versus physical therapy (PT) versus delayed physical therapy (DPT) after surgical release for elbow contractures; a study protocol for a prospective randomized controlled trial. BMC Musculoskelet. Disord. 18, 1–7. https://doi.org/10.1186/s12891-017-1854-0 (2017).
Wolf, J. M. Does CPM improve outcomes after elbow contracture release?. J. Bone Joint Surg. 104, 1–2. https://doi.org/10.2106/JBJS.21.01410 (2022).
Jia, Z., Zhang, Y., Zhang, W., Xu, C. & Liu, W. Efficacy and safety of continuous passive motion and physical therapy in recovery from knee arthroplasty: A systematic review and meta-analysis. J. Orthop. Surg. Res. 19, 1–9. https://doi.org/10.1186/s13018-024-04536-y (2024).
Ammerman, B. M., Updegrove, G., Ponnuru, P. & Armstrong, A. Analysis of long-term outcomes following surgical contracture release of the elbow: A case series. Cureus 13, 1–10. https://doi.org/10.7759/cureus.14691 (2021).
O’Driscoll, S. W. et al. Prospective randomized trial of continuous passive motion versus physical therapy after arthroscopic release of elbow contracture. J. Bone Jt. Surg. 104, 430–440. https://doi.org/10.2106/JBJS.21.00685 (2022).
Blonna, D. et al. Prevention of nerve injury during arthroscopic capsulectomy of the elbow utilizing a safety-driven strategy. J. Bone Jt. Surg. 95, 1373–1381. https://doi.org/10.2106/JBJS.K.00972 (2013).
Isa, A. et al. Arthroscopic debridement for primary elbow osteoarthritis with and without capsulectomy: A comparative cohort study. Shoulder Elbow 10, 223–231. https://doi.org/10.1177/1758573217726429 (2018).
Khalil, L. S. et al. The relationship between shoulder range of motion and elbow stress in college pitchers. J. Shoulder Elbow Surg. 30, 504–511. https://doi.org/10.1016/j.jse.2020.06.016 (2021).
Bodian, C. A., Freedman, G., Hossain, S., Eisenkraft, J. B. & Beilin, Y. The visual analog scale for pain: Clinical significance in postoperative patients. J. Am. Soc. Anesthesiol. 95, 1356–1361. https://doi.org/10.1097/00000542-200112000-00013 (2001).
Tashjian, R. Z., Deloach, J., Porucznik, C. A. & Powell, A. P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J. Shoulder Elbow Surg. 18, 927–932. https://doi.org/10.1016/j.jse.2009.03.021 (2009).
Mark, M., Au, T., Choi, Y. & Wong, T. The minimum clinically significant difference in visual analogue scale pain score in a local emergency setting. Hong Kong J. Emerg. Med. 16, 233–236. https://doi.org/10.1177/102490790901600406 (2009).
Sun, Z. et al. Determining the effective timing of an open arthrolysis for post-traumatic elbow stiffness: A retrospective cohort study. BMC Musculoskelet. Disord. 20, 1–9. https://doi.org/10.1186/s12891-019-2506-3 (2019).
Varadhan, K. K. et al. The enhanced recovery after surgery (eras) pathway for patients undergoing major elective open colorectal surgery: A meta-analysis of randomized controlled trials. Clin. Nutr. 29, 434–440. https://doi.org/10.1016/j.clnu.2010.01.004 (2010).
Joshi, G. P. & Kehlet, H. Enhanced Recovery Pathways: Looking into the Future https://doi.org/10.1213/ANE.0000000000003746 (2019).
Dueñas, M., Ojeda, B., Salazar, A., Mico, J. A. & Failde, I. A review of chronic pain impact on patients, their social environment and the health care system. J. Pain Res. 9, 457–467. https://doi.org/10.2147/JPR.S105892 (2016).
Higgs, Z. et al. Outcomes of open arthrolysis of the elbow without post-operative passive stretching. J. Bone Jt. Surg. 94–B, 348–352. https://doi.org/10.1302/0301-620X.94B3.27278 (2012).
Leach, W., Reid, J. & Murphy, F. Continuous passive motion following total knee replacement: A prospective randomized trial with follow-up to 1 year. Knee Surg. Sports Traumatol. Arthrosc. 14, 922–926. https://doi.org/10.1007/s00167-006-0042-9 (2006).
Pope, R. et al. Continuous passive motion after primary total knee arthroplasty. J. Bone Jt. Surg. 79, 914–917. https://doi.org/10.1302/0301-620X.79B6.0790914 (1997).
O’Driscoll, S. & Giori, N. Continuous passive motion (CPM): Theory and principles of clinical application. J. Rehabil. Res. Dev. 37, 179–188 (2000).
Funding
This work was supported in part by the Cangzhou Science and Technology Bureau under Grant No. 204106140.
Author information
Authors and Affiliations
Contributions
MHaibin Li performed the surgical procedures on the participants involved in the experiment. The manuscript was primarily written by Haibin Li and Ming Wang, while Guangming Deng prepared all the figures. Hongrui Fu and Bingbing Chen were responsible for data collection and analysis. Xueqiao Yang contributed to the conceptualization, supervision, investigation, and methodology of the study. Additionally, all authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
We confirmed that the written informed consent to publish this manuscript was obtained from the study participants.
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki. Approval was obtained from the Medical Ethics Committee of Cangzhou Fifth Hospital (Qingxian People’s Hospital) (Approval No. QXRMYY202003), and all procedures were carried out following relevant guidelines and regulations. Informed consent for publication of identifying information/images in an online open-access publication was obtained from all participants and/or their legal guardians.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, H., Wang, M., Deng, G. et al. Effectiveness of home based continuous passive motion compared with conventional physical therapy after arthroscopic release of degenerative elbow stiffness. Sci Rep 15, 30570 (2025). https://doi.org/10.1038/s41598-025-16337-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-16337-2