Abstract
The first month of life is the most vulnerable period for child survival. Newborns who are born too soon or too small, or sick, are at the greatest risk of death. Objective of the study was to delve into neonatal mortality and low birth weight (LBW) survival at hospitals in Indonesia. It was a retrospective cohort on the neonates cared at 12 hospitals in various islands of Indonesia during August-October 2021. Inclusion criteria were singleton and age 0–28 days, whereas exclusion criteria were incomplete medical records and gestational age ≥ 42 weeks. Of 2726 neonates, 2017 were eligible for the study. Multivariate logistic regression analysis exhibited LBW had the highest mortality risk, followed by referral neonates. The highest mortality risks at birth were asphyxia and major congenital abnormalities, subsequently. During the early neonatal period, the highest mortality risks were respiratory distress and feeding problem, consecutively. At 7–28 days of life, the feeding problem was the highest mortality risk. Kaplan Meier analysis suggested early neonatal death in LBW and Normal Birth Weight (NBW) infants was almost similar at aged 6 days. At neonatal period, however, the average age of neonatal death in LBW infants was 21 days, whereas in NBW 26 days.
Similar content being viewed by others
Introduction
The first month of life is the most vulnerable period for child survival, which is among the most vulnerable periods of life and requires intensified quality of intrapartum and newborn care1. Current trends indicate that 63 countries are not on track to achieve the 2030 Sustainable Development Goals target of a neonatal mortality rate ≤ 12 per 1000 live births, with 55 needing to double the annual rate of decline in neonatal mortality to do so2,3.
Newborns who are born too soon or too small, or who become sick, are at the greatest risk of death and disability. Every year, an estimated 2.5 million newborns die during the first 28 days of life. It had been estimated that as many as 80% of all neonatal deaths in the world occurred in LBW infants, of whom two-thirds are probably preterm and one-third SGA4. In addition, a further estimated 1 million small and sick newborns survive with a long-term disability4,5. The fact that every fourth baby in the world is born too soon or born too small is a concern for human rights, public health, national economy and development. By not addressing this priority, we are jeopardising our collective future6.
There have not been any published multicentre studies on LBW and neonates conducted at hospitals in Indonesia. The objective was to delve into at birth, early neonatal, late neonatal, neonatal mortality, and LBW survival at hospitals in Indonesia.
Methods
It was a retrospective cohort study on the neonates taken care at 12 hospitals in various islands of Indonesia from August to October 2021. The inclusion criteria were singleton and age 0–28 days, whereas exclusion criteria were incomplete medical records and gestational age ≥ 42 weeks.
The dependent variable was the neonatal mortality occurring while the neonates were being cared for at the hospitals; the independent variable was LBW; while confounding variables included mothers’ and infants’ conditions. Infants’ conditions included sex, place of birth, method of delivery, gestational age, condition at birth, condition at early neonatal (EN) < 7 days old, and condition at late neonatal (LN) 7–28 days of age. Mothers’ conditions covered mothers’ ages, parity, antenatal care (ANC), mothers’ medical problems, and current obstetric problems.
The data were extracted from the medical records of each hospital. Neonatal mortality was classified into “yes” and “no”. Birth weight was declared with LBW (birth weight < 2500 gram) “yes” and “no”. Sex was determined by the physical examination and was categorized into boy and girl. Place of birth referred to the settings where the infants were delivered, which were divided into born at the hospitals and outside the hospitals or referral infants. Methods of delivery were defined as vaginal delivery or caesarean section. Gestational age was recorded from the medical records and was measured based on antenatal ultrasonography or estimated gestational age by Dubowitz score or sick or weak neonates declared in complete weeks by Ballard score.
Conditions at birth included asphyxia, major congenital anomaly, and birth trauma. Asphyxia was a condition in which an infant was born breathless or he/she required a resuscitation with positive pressure ventilation or umbilical cord blood PH < 7.2; which was classified into “yes” and “no”. Major congenital anomalies or life threatening syndromes were stated in “yes” and “no”. Birth trauma referred to the trauma that occurred during the delivery process and was declared in “yes” and “no”.
Some conditions found in the neonates at EN or at LN may take the forms of respiratory distress, sepsis, jaundice, seizure, haemorrhage, and feeding problem. Respiratory distress referred to a condition in which neonates breathed at higher or lower than normal frequency, did not breathe at all, or developed cyanosis by Downes score with ≥ 4; which was divided into “yes” and “no”. Sepsis was a systemic infection in neonates and was clinically stated by at least 4 symptoms and signs present in general condition, cardiovascular, respiration, haematology, central nervous system, and gastrointestinal, which was categorized into “yes” and “no”. Jaundice was characterized by yellowish skin or mucous membrane with bilirubin level higher than normal, and was stated in “yes” and “no”. Seizure was defined as neonates’ rhythmic movements, which was divided into “yes” and “no”. Haemorrhage referred to visible or invisible bleeding such as in periventricular bleeding and was categorized into “present” or “none”. Feeding problem was defined as troubled enteral feeding which may have been caused by feeding difficulties or feeding intolerance characterized by abdominal distention or vomit or the presence of abdominal residual as much as ⅓ of being fed7; it was declared in “present” and “none”.
Mother’s age was classified into < 20 years (high risk), 20–34 years (low risk), and ≥ 35 years (high risk); which was divided into “yes” and “no”. Parity refers to a situation in which the mother had previously given birth, which was categorized into high risk if there was 1 parity or ≥ 5 and no high risk if there were 2–4 parities. The ANC was defined as care of a pregnant mother at the health facility for at least 4 times during her pregnancy, which was then classified into “yes” and “no”. Mother’s medical problem referred to the problem that the mother suffered during her pregnancy, and this was divided into present and none. Obstetric problem was defined as the pregnancy and delivery-related case that the mother encountered; which was stated as present and none.
The characteristics of the data of each variable were presented in the univariate table. Bivariate analyses among the independent variable, confounding variable, and dependent variable were considered to have a significant difference if p < 0.05; calculated by Odds Ratio (OR) with confidence interval (CI) 95%. The analysis of multivariate logistic regression was obtained from the variable whose bivariate result was p < 0.25. Kaplan Meier survival curve was used to observe the mean survival time with the CI 95% of both LBW and NBW infants at EN and neonatal period.
All methods were carried out in accordance with relevant guidelines and regulations of each hospital participating in this study, even though the operational definition was the same. The protocol of diagnosis recording at every hospital was in line with the national guideline. The management of the missing data and different methods of diagnosis recording in various hospitals is presented.
Results
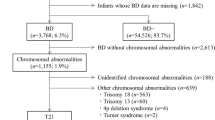
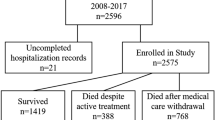
There were 2726 neonates collected, 2017 of whom were eligible for our study. Incomplete medical records, which were dominated by unclear time of death, were the reason for exclusion. Of 2017 neonates, 765 (38%) were LBW and 1252 (62%) were NBW (Fig. 1).
We found 323 (16%) neonatal deaths and 1694 (84%) survivors among the eligible neonates. Among NBW, there were 97 (7.7%) neonatal deaths and 1155 (92.3%) survivors, whereas among the LBW infants there were 226 (29.5%) neonatal deaths and 539 (70.5%) survived until 28 days (Table 1).
The mortality among the total neonates in neonatal period was 323 (16%), in EN period 182 (9%) and in LN period showed 141 (7%). Meanwhile, the mortality among LBW, in the neonatal period was 226 (29.5%), in EN period 133 (17.4%), and in LN 93 (12.1%).
Mother’s characteristics of death of the neonates who lived until 28 days included mother’s age, parity, ANC at least 4 times during pregnancy, mother’s medical problem, and current obstetric problem (Table 2).
Bivariate analysis showed referral birth place, LBW, preterm, mother’s age with risks, mother’s current medical problem that posed mortality risks. Meanwhile, conditions at birth which potentially resulted in death included asphyxia, major congenital anomalies, and birth trauma, respectively. Some conditions that were likely to bring the risks to infants at EN mortality were feeding problem, haemorrhage, respiratory distress, seizure, sepsis, and jaundice, successively. The risks of LN mortality included seizure, feeding problem, haemorrhage, respiratory distress, sepsis, and jaundice, consecutively (Table 3).
The multivariate logistic regression analysis exhibited LBW had the highest mortality risk, followed by referral birth place, whereas gestational age showed insignificant difference. The highest mortality risks at birth were asphyxia and major congenital abnormalities, subsequently. During the EN period, the highest mortality risks were respiratory distress and feeding problem, consecutively. Meanwhile, sepsis, seizure, and haemorrhage posed insignificant differences in mortality risks. At LN period, feeding problem was the highest mortality risk in infants; however, we did not find any significant difference among respiratory distress, seizure, and haemorrhage as the mortality risks (Table 3).
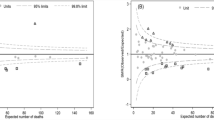
Kaplan Meier analysis suggested EN mortality in LBW and NBW infants was almost similar, approximately at 6 days of life (Fig. 2). At neonatal period, however, the average age of mortality of LBW infants was 21 days, whereas in NBW was 26 days (Fig. 3).
Discussion
The present study showed that the proportion of neonatal mortality was 16%. A similar result was found at the Neonatal Intensive Care Unit (NICU) in western Ethiopia8. The neonatal mortality in our study, however, was lower than that of the NICU-based study conducted in Nigeria and Kenya, which was 18,7%9 and it was also lower than Desalev’s in eastern Ethiopia, which was 20%. Greater efforts are needed to address the very high burden of illnesses and mortality in hospitalized newborns10. Our study reported neonatal mortality among LBW in the EN period was 17.4% and in LN period 12.1%, whereas Debere recounted that, among birthweight < 2000 gram in 5 hospitals in Ethiopia, the neonatal mortalities during the EN and LN period were 23.02% and 6.68%, respectively11.
Neonatal factors
Our study found 29.5% of LBW infants death, and a mortality risk with OR 2.56. The mortality risk in our study was lower than that in Eyebaru’s study, which reported neonatal mortality risk in LBW with adjusted OR 4.0112. Eshete reported 42.3% of the LBW neonates died during the first week of life13. Other studies mentioned that LBW infants with complications were one of the causes of neonatal death at hospitals14. A quality improvement intervention was associated with decreased mortality among infants with birth weight between 1500 and 2499 g. Further efforts are needed to improve the prognosis in very low birth weight infants15. Woelile also reported 2 of 7 LBW infants died during the observation period. Therefore, the health personnel and policy makers need to know the early diagnosis and management of LBW infants with complications16. The lower neonatal mortality risk in our study may have been caused by the fact that we included the infants with birth weight < 2500 g only. Future studies need to classify the birth weight in detail.
A community-based study recounted, according to mother’s perception of baby’s size, neonates that mothers perceived to be small had 3.46 times more risks of dying compared with average size neonates17. From Indonesia Demographic and Health Survey (IDHS) 2012–2017, Titaley revealed the strong association among LBW, preterm birth, and EN mortality18.
In this study, the bivariate analysis on gestational age was significant with OR 2.67; however, the multivariate analysis did not show the mortality risk. It was different from the result of the study conducted in 14 European countries, which found wide neonatal mortality rate disparities with varying patterns by gestational age19.
Referral neonates in our study had mortality risk with OR 2.06, which was similar to the result of the other studies. The place of delivery was one of the neonatal mortality risks. It was reported that the neonates delivered at the health centres had the mortality risk with adjusted OR 5.0512. Nevertheless, health facility delivery is found to reduce the risk of neonatal mortality by 29% in low and middle income countries (LMIC). Desalev reported that a well-structured referral to the hospital with NICU was required in order to reduce neonatal mortality10. It is recommended that the government emphasize accessible healthcare services and develop educational programs that focus on facility-based deliveries, prenatal care, and postnatal care for expectant mothers20.
There were 54.49% boys in our study with the total proportion of mortality 76.23%. In the analysis, however, it did not reveal the mortality risk. This result was different from that of the study on neonatal mortality at the tertiary and secondary hospitals in Indonesia, which reported that boys had hazard ratio risk of 1.1621. The analysis of IDHS 201722 and a secondary analysis of demographic and health surveys conducted between 2015 and 2022 in 43 LMIC reported that male newborns had higher mortality risk significantly23. Khadam explained the significant predictors of neonatal mortality was male (p = 0.004)24.
Our study did not present the difference in neonatal mortality between caesarean and vaginal delivery. It was similar to Spung, which reported that caesarean delivery performed for very preterm neonates is associated with decreased risk for death in the delivery room or within 24 h of delivery but was not associated with improvement in the overall morbidity or mortality25. However, Nugraha found that preterm infants born through caesarean would decrease neonatal mortality26.
The proportion of asphyxia at birth in our study was 16.61% of total neonates, and multivariate analysis unveiled the highest mortality risk with OR 3.80. It was similar to Eyebaru’s study, which reported asphyxia with mortality risk of adjusted OR 3.8512. In our study, the proportion of asphyxia was lower than in Desalew’s (22.45%), which was a NICU-based study10. Hospitals and health care workers should pay attention to neonates admitted to NICU by strengthening early detection and treatment of health problems12. The magnitude of ENM is considerable and most of the determinants are preventable. Neonatal resuscitation as per national standard within the first golden hour is a key. Ahmed showed newborn resuscitation had a protective effect and reduced early newborn death by 70% with Adjusted OR 0.327.
Cross sectional, community-based study using adapted verbal and social autopsy instruments showed the causes of neonatal death in two districts in Indonesia was intrapartum-related infant, mainly birth asphyxia (39%)28.
Neonatal mortality caused by major congenital anomalies in our study was 6.7%, which was higher than in Desalew’s, reporting 4.08% at the NICU in Eastern Ethiopia10. Our study showed mortality risks by multivariate analysis was OR 2.08. Another study reported the mortality risk due to congenital abnormalities with OR 4.939. Our mortality risk was, however, lower than that in Nabwera’s study. This might have been induced by the fact that 95% of the hospitals in our multicentre study were tertiary hospitals, to which the infants with major congenital abnormalities were commonly referred. The hospitals were equipped with more adequate facilities and availability of surgeons and other related specialists.
In this study, the proportion of respiratory distress during EN period was 18.5% with the mortality risk OR 2.58, whereas during the LN period it was 7.73% with OR 1.23 without significance. Desalew in his study in Ethiopia reported that respiratory distress was 16.3%10. Meanwhile, Nabwera discovered that respiratory conditions posed the mortality risk of 1.469. The result of our study was slightly higher because most of the hospitals where our study took place were tertiary referral and/or teaching hospitals where most severe medical problems were managed. Haksari recounted respiratory distress posed the highest hazard ratio in early and neonatal mortality21. Preterm-small for gestational age (SGA) had the highest risk of respiratory distress with complications of length of hospital stay and ventilator use. We should therefore be alert when dealing with preterm-SGA infants29. In order to reduce the number of neonatal mortality, WHO recommends every district have 80% of level 2 health facilities equipped with respiratory support such as continuous positive airway pressure to take care of small and/or sick infants2,3,30,31.
In our study, sepsis occurring at < 7 days by bivariate analysis showed OR 5.81; however, multivariate analysis exhibited OR 1.2 without significant difference. In the LN period, the mortality risk was only found by bivariate analysis with OR 3.88. The result was different from that of another study which revealed early sepsis with adjusted OR 3.93 was the factor significantly associated with neonatal mortality11. One study on Mother and Child Hospital in Aceh reported that sepsis was the most associated factor with neonatal mortality32. The different result may have been induced by the fact that our study reported clinical sepsis.
Seizure during EN period, by bivariate analysis, showed mortality risk with OR 6.36; however, by multivariate analysis the mortality risk was OR 1.5 without a significant difference. In the LN period, the bivariate analysis unveiled OR 9.55, whereas multivariate analysis found OR 1.38 without a significant difference. Another study reported high seizure burdens with OR 4.33 were associated with increased odds of death. In a cohort of neonates with seizures, death occurred predominantly after decisions to withdraw or withhold life-sustaining intervention(s)33. Heiljic reported that the mortality rate in the first year of infants with seizures during the neonatal period was 23%. The most common causes of seizures were birth asphyxia with hypoxic ischemic encephalopathy for full-term were birth asphyxia with hypoxic ischemic encephalopathy and intra periventricular haemorrhage for preterm infants. Death was more common in preterm than in term infants (p < 0,005). In this cohort of neonates with seizures, asphyxia requiring neonatal resuscitation was the primary risk factor for death34.
The haemorrhage proportion in our study during EN period was 1.8%, with mortality risk by bivariate analysis OR 12.42. During LN period, the proportion of haemorrhage was 2.78%, with mortality risk by bivariate analysis OR 8.8. Meanwhile, multivariate analysis revealed the EN mortality risk with OR 1.95 and LN mortality risk with OR 1.77, although there was no significant difference between the two. The haemorrhage proportion on death in this study was smaller than in Khadam’s study, which reported the mortality rate among the Intraventricular Haemorrhage (IVH) preterm neonates was 38.9%24. This happened because our study involved preterm and full-term infants and did not focus merely on the IVH. Additionally, increased severity of IVH, early gestational age, and LBW were associated with mortality in preterm neonates with IVH24.
Feeding problem in our study had a mortality risk during the EN period with OR 2.9 and during LN period with OR 2.3. It was similar to the result of other studies which revealed a high incidence of mortality among LBW neonates with feeding problems. Furthermore, factors such as birth weight, trophic feeding initiation, low Apgar score, and oedematous malnutrition were identified as predictors for mortality among LBW receiving enteral feeding. Therefore, the priority of optimizing enteral feeding practices and enhancing the quality of care provided to LBW neonates should be optimized10,35,36. Feeding problems are a major issue in neonatology, which may take the forms of feeding difficulties and/or feeding intolerance, either which frequently brings clinicians to withhold, decrease, or discontinue enteral feeds. Thus, they may hamper the establishment of an adequate enteral nutrition and lead to a prolonged duration of both parenteral nutrition and central lines, with increased risks of such complications as liver cholestasis or sepsis37. The future study should focus on LBW infants only.
Mother’s factors
Mother’s age with risks (< 20 years and ≥ 35 years) by bivariate analysis was 1.54, whereas the multivariate analysis showed OR 1.13, but without a significant difference. It was different from the result of the study based on IDHS 2017, which reported that the mother’s age with risks was associated with neonatal mortality22. Kim also stated that mothers ≥ 40 years may become a risk factor for their EN mortality. This finding suggests public health efforts should be taken to improve care for reproductive age of 25–34 years in order to reduce EN mortality38.
Parity in our study was not a risk factor for neonatal mortality, which was different from Siahaan’s study that used the IDHS data 2017. He revealed that parity ≥ 4 was significantly associated with neonatal mortality in Indonesia. The more children are born to mothers, the higher the risk of neonatal death will be. While nulliparity did not have a significant relationship with neonatal mortality, it was recommended that family planning programs be increased to reduce parity and to avoid the risk of neonatal death39. Another study reported the large sample from diverse settings, nulliparity was independently associated with both lower birthweight and weight for age Z scores as well as higher neonatal mortality compared with multiparity. Nulliparous women < 18 years of age had the highest odds of adverse neonatal outcomes such as preterm, SGA, or death. Higher odds of adverse outcomes were also seen among parity ≥ 3 or age ≥ 35 mothers40.
The proportion of ANC visits < 4 times in our study was 21.8%, but without the mortality risk. The result was different from that of the IDHS data-based study, reporting that the ANC visit < 4 times was associated with neonatal mortality24. A study conducted at the NICU of a university referral hospital in western Ethiopia found that lack of ANC visits affected neonatal mortality7.
The proportion of maternal medical problems in our study was 33.42%. The mortality risk by bivariate analysis showed OR 1.3; however, multivariate analysis did not present a significant difference. This study did not discuss the detailed maternal medical problem during pregnancy. Valadbeigi reported that undiagnosed underlying diseases were related to neonatal mortality, which highlighted the importance of caring for and counselling about, screening, and controlling blood sugar levels before and during pregnancy to prevent neonatal mortality by all means possible41. One study from India suggested that the maternal history of neonatal death is a potentially useful risk factor to identify women and neonates who may need extended and enhanced pregnancy care42. Dev, using maternal birth histories from the Indonesia Family Life Survey panel data, established previous adverse outcomes such as neonatal deaths and stillbirth could help identify high-risk pregnancies during prenatal care, inform interventions, and improve health policy43.
Our study found 16% neonatal deaths in mothers with obstetric problems, which was not a risk factor for neonatal mortality. It was different from the result of the study which was based on IDHS 2017, reporting that there was a significant correlation between the complications during delivery and neonatal mortality after controlling by variables of age, ANC visits, baby’s birth weight, and baby’s sex on neonatal mortality with prevalence ratio 3.9022.
Mortality survival of LBW infants in our study was 21 days, which was higher than Woelie’s which reported 17 days16. Debere, using the birth weight < 2000 gram, recounted that the overall incident rate of neonatal mortality was 16.17/100011. The study did not, however, clarify the classification of the LBW infants. An analysis by Kaplan Meier revealed that the increased survival age of NBW is more likely to improve their life expectancy.
Limitation and strength of study
Our study was a cohort-retrospective study which was dependent much on completeness of the medical records at each hospital. Also, it did not specify the classifications of LBW, very low birth weight, and extreme low birthweight infants. The things pertaining to undivided sepsis into early and late, no separation of indirect and direct bilirubin, absence of detailed feeding problems, absence of information on the presence of NEC, respiratory distress with or without ventilation, and absence of detailed information on mothers’ medical and obstetric problems will be analysed in my future study. In addition, we only observed the neonates while they were at the hospitals. It was a multicentre study which became the strength of our study since there have not been any published reports on neonatal mortality in LBW infants at hospitals in Indonesia extracted from multi-centre data.
Conclusion
The highest neonatal mortality risks at hospitals in Indonesia were LBW and referral infants, respectively. At birth, asphyxia and major congenital anomalies might serve as the highest mortality risks consecutively. EN mortality risks included respiratory distress and feeding problem. Meanwhile, LN mortality risk at ages 7–28 days was feeding problem.
Kaplan Meier observation revealed EN mortality in LBW and NBW infants occurred approximately at 6 days old, whereas an observation on the neonates for 28 days unveiled neonatal death in LBW at 21 days and NBW at 26 days.
Hospitals and health care workers should pay attention to the neonates admitted to the NICU. Health care providers should particularly be aware of whether mothers have given birth at the hospitals according to the conditions of their fetus and neonates, know how to stabilize referral neonates, perform neonatal resuscitation and identify and manage congenital anomalies, respiratory distress, and feeding problem. Also, they should perform early detection and strengthen the quality improvement of the small newborns. All of the above require improvement of the health service system from the government.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
antenatal care
- CI:
-
confidence interval
- EN:
-
early neonatal
- IDHS:
-
indonesian demographic health surveillance
- IVH:
-
intraventricular haemorrhage
- LBW:
-
low birth weight
- LMIC:
-
low medium income countries
- LN:
-
late neonatal
- NBW:
-
normal birth weight
- NICU:
-
neonatal intensive care unit
- OR:
-
odd ratio
- SGA:
-
small for gestational age
- WHO:
-
world health organization
References
World Health Organization (WHO). Newborn mortality https://www.who.int/news-room/fact-sheets/detail/newborn-mortality (2024).
World Health Organization, United Nations Children Fund (UNICEF). Ending preventable newborn deaths and stillbirths by 2030. https://www.unicef.org/reports/ending-preventable-newborn-deaths-stillbirths-quality-health-coverage-2020-2025 (2020).
World Health Organization (WHO). World Health Organization Recommendations for Care of the Preterm or Low Birth Weight Infant (Geneva, 2022).
Blencowe, H. et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Global Health. 7, e849–e860. https://doi.org/10.1016/s2214-109x(18)30565-5 (2019).
World Health Organization (WHO). Survive and Thrive: Transforming Care for Every Small and Sick Newborn (Geneva, 2019).
Ashorn, P. et al. Small and vulnerable newborns an executive summary for the lancet’s series. Preprint at (2023). https://www.thelancet.com/series-do/small-vulnerable-newborns (2023)
Corvaglia, L. & Martini, S. Feeding difficulties during the neonatal period. Ital. J. Pediatr. 41, A21. https://doi.org/10.1186/1824-7288-41-S2-A21 (2015).
Tolossa, T. et al. Survival status and predictors of neonatal mortality among neonates admitted to neonatal intensive care unit (NICU) of Wollega university referral hospital (WURH) and Nekemte specialized hospital, Western ethiopia: a prospective cohort study. PLoS One. 17, e0268744. https://doi.org/10.1371/journal.pone.0268744 (2022).
Nabwera, H. M. et al. Burden of disease and risk factors for mortality amongst hospitalized newborns in Nigeria and Kenya. PLoS One. 16, e0244109. https://doi.org/10.1371/journal.pone.0244109 (2021).
Desalew, A. et al. Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in Eastern ethiopia: a facility-based prospective follow-up study. BMC Pediatr. 20, 160. https://doi.org/10.1186/s12887-020-02051-7 (2020).
Debere, M. K., Mariam, D. H., Ali, A., Mekasha, A. & Chan, G. J. Survival status and predictors of mortality among low-birthweight neonates admitted to KMC units of five public hospitals in ethiopia: frailty survival regression model. PLoS One. 17, e0276291. https://doi.org/10.1371/journal.pone.0276291 (2022).
Eyeberu, A., Shore, H., Getachew, T., Atnafe, G. & Dheresa, M. Neonatal mortality among neonates admitted to NICU of Hiwot Fana specialized university hospital, Eastern ethiopia, 2020: a cross-sectional study design. BMC Pediatr. 21, 125. https://doi.org/10.1186/s12887-021-02598-z (2021).
Eshete, A., Alemu, A. & ZerfuT. A. Magnitude and risk of dying among low birth weight neonates in rural ethiopia: a community-based cross-sectional study. Int. J. Pediatr. 2019 (9034952). https://doi.org/10.1155/2019/9034952 (2019).
Taye, K., Kebede, Y., Tsegaw, D. & Ketema W. Predictors of neonatal mortality among neonates admitted to the neonatal intensive care unit at Hawassa university comprehensive specialized hospital, Sidama regional state, Ethiopia. BMC Pediatr. 24, 237. https://doi.org/10.1186/s12887-024-04689-z (2024).
Pietravalle, A. et al. Impact of quality improvement bundle on neonatal mortality in a district hospital in Tanzania. Children 9 (1060). https://doi.org/10.3390/children9071060 (2022).
Woelile, T. A. et al. Survival status and predictors of mortality among low-birth-weight neonates admitted to the neonatal intensive care unit at Felege Hiwot comprehensive specialized hospital, Bahir dar, ethiopia, 2020. Pediatr. Health Med. Ther. 12, 451–466. https://doi.org/10.2147/PHMT.S323526 (2021).
Limaso, A. A., Dangisso, M. H. & Hibstu, D. T. Neonatal survival and determinants of mortality in Aroresa district, Southern ethiopia: a prospective cohort study. BMC Pediatr. 20, 33. https://doi.org/10.1186/s12887-019-1907-7 (2020).
Titaley, C. R., Mu’asyaroh, A., Que, B. J., Tjandrarini, D. H. & Ariawan, I. Determinants of early neonatal mortality: secondary analysis of the 2012 and 2017 Indonesia demographic and health survey. Front. Pediatr. 12, 1288260. https://doi.org/10.3389/fped.2024.1288260 (2024).
Sartorius, V. et al. For the Euro-Peristat network. Neonatal mortality disparities by gestational age in European countries. JAMA Netw. Open. 7, e2424226. https://doi.org/10.1001/jamanetworkopen.2024.24226 (2024).
Asim, A. N., Kiani, M. M. L., Ali, J., Sheraz, A. & Zafar, R. Impact of place of delivery on neonatal mortality in pakistan: challenges and pathways toward achieving the sustainable development goals. Global Health Econ. Sustain. 10 https://doi.org/10.36922/ghes.5089 (2025).
Haksari, E. L., Hakimi, M. & Ismail, D. Neonatal mortality in small for gestational age infants based on reference local newborn curve at secondary and tertiary hospitals in Indonesia. BMC Pediatr. 23, 214. https://doi.org/10.1186/s12887-023-04023-z (2023).
Anisa, N., Astuti, A. W. & Hakimi, M. Correlation between complications during delivery and neonatal mortality: data analysis of Indonesia demographic and health survey (IDHS) 2017. Jurnal Kedokteran Dan. Kesehatan Indonesia. 13, 125–138. https://doi.org/10.20885/JKKI.Vol13.Iss2.art5 (2022).
Tamir, T. T. Neonatal mortality rate and determinants among births of mothers at extreme ages of reproductive life in low and middle income countries. Sci. Rep. 14, 12596. https://doi.org/10.1038/s41598-024-61867-w (2024).
Kadam, M., Trivedi, A. & Sachede, V. Intraventricular hemorrhage on mortality and neurological outcomes in premature infants. Int. J. Contemp. Pediatr. 11, 296–302. https://doi.org/10.18203/2349-3291.ijcp20240347 (2024).
Zahedi-Spung, L. D., Raghuraman, N., Macones, G. A., Cahill, A. G. & Rosenbloom, J. I. Neonatal morbidity and mortality by mode of delivery in very preterm neonates. Am. J. Obstet. Gynecol. 226, 114. https://doi.org/10.1016/j.ajog.2021.07.013 (2022).
Nugraha, G. B. A. & Anggraini, N. W. P. Mode of delivery and neonatal outcomes in preterm pregnancy metode persalinan Dan Luaran neonatus Pada Kehamilan prematur. Indones J. Obstet. Gynecol. 11, 2. https://doi.org/10.32771/inajog.v11i2.1803 (2023).
Ahmed, A. T., Farah, A. E., Ali, H. N. & Ibrahim, M. O. Determinants of early neonatal mortality (hospital based retrospective cohort study in Somali region of Ethiopia). Sci. Rep. 13, 1114. https://doi.org/10.1038/s41598-023-28357-x (2023).
Deviany, P. E. et al. Neonatal mortality in two districts in indonesia: findings from neonatal verbal and social autopsy (VASA). PLoS One. 17, e0265032. https://doi.org/10.1371/journal.pone.0265032 (2022).
Haksari, E. L., Hakimi, M. & Ismail, D. Respiratory distress in small for gestational age infants based on local newborn curve prior to hospital discharge. Front. Pediatr. 10, 986695. https://doi.org/10.3389/fped.2022.986695 (2022).
World Health Organization-United Nations Children Fund (UNICEF) Expert and Country Consultation on Small and/or Sick Newborn Care Group. A comprehensive model for scaling up care for small and/or sick newborns at district level–based on country experiences presented at a WHO-UNICEF expert consultation. J. Glob Health. 13, 03023. https://doi.org/10.7189/jogh.13.03023 (2023).
World Health Organization (WHO). Born too soon: decade of action on preterm birth. Geneva, (2023).
Nurhayati, N., Abdullah, A., Maidar, M., Hermansyah, H. & Zakaria, R. Determinants of neonatal death in Aceh mother and child hospital. J. Community Health. 10, 86–95. https://doi.org/10.25311/keskom.Vol10.Iss1.1510 (2024).
Belachew, A. & Tewabe, T. Neonatal sepsis and its association with birth weight and gestational age among admitted neonates in ethiopia: systematic review and meta-analysis. BMC Pediatr. 20, 55. https://doi.org/10.1186/s12887-020-1949-x (2020).
Lemmon, M. E. et al. Neonatal seizure registry. Characterization of death in infants with neonatal seizures. Pediatr. Neurol. 113, 21–25. https://doi.org/10.1016/j.pediatrneurol.2020.08.002 (2020).
Heljic, S., Uzicanin, S., Catibusic, F. & Zubcevic, S. Predictors of mortality in neonates with seizures; a prospective cohort study. Med. Arch. 70, 182–185. https://doi.org/10.5455/medarh.2016.70.182-185 (2016).
Mislu, E., Arage, M. W., Kumsa, H. & Terefe, A. Mortality among low birth weight neonates on parenteral feeding: a prospective follow-up study. Res. Rep. Neonatology. 14, 67–84. https://doi.org/10.2147/RRN.S450572 (2024).
Banait, N. et al. Feeding of low birth weight neonates. J. Neonatology. 34, 28–51. https://doi.org/10.1177/0973217920938522 (2020).
Kim, Y-N., Choi, D-W., Kim, D. S., Park, E-C. & Kwon, J-Y. Maternal age and risk of early neonatal mortality: a National cohort study. Sci. Rep. 11, 814. https://doi.org/10.1038/s41598-021-80968-4 (2021).
Siahaan, A. & Ariawan, I. The effect of parity on neonatal mortality in indonesia. Jurnal Ilmu Kesehatan Masyarakat. 12, 250–262. https://doi.org/10.26553/jikm.2021.12.3.250-262 (2021).
Garces, A. et al. Association of parity with birthweight and neonatal death in five sites: the global network’s maternal newborn health registry study. Reprod. Health. 17, 182. https://doi.org/10.1186/s12978-020-01025-3 (2020).
Valadbeigi, T. et al. Evaluating the association between neonatal mortality and maternal high blood pressure, heart disease, and gestational diabetes: a case control study. J. Res. Med. Sci. 25, 23. https://doi.org/10.4103/jrms.jrms_814_18 (2020).
Kapoor, M. et al. Association of maternal history of neonatal death with subsequent neonatal death in India. JAMA Netw. Open. 3, e202887. https://doi.org/10.1001/jamanetworkopen.2020.2887 (2020).
Dev, A. Risk of recurrent stillbirth and neonatal mortality: mother-specific random effects analysis using longitudinal panel data from Indonesia (2000–2014). BMC Pregnancy Childbirth. 22, 524. https://doi.org/10.1186/s12884-022-04819-4 (2022).
Acknowledgements
We would like to thank The Indonesian Society of Perinatology (Perinasia) for the opportunity to conduct this study and for its funding support. Our gratitude is also addressed to Agus Herwindo, Ananta, Hariyati, Khairunissaa’, Sari, Tony, and Wawan Yunanto for their remarkable help and support so that this manuscript could be ready for publication.
Funding
This work was financially supported by Perinasia.
Author information
Authors and Affiliations
Contributions
All authors participated in the study design and interpretation of data. ELH, ND conceptualized and designed the study, coordinated and supervised data collection, acquisition of data, analysis and interpretation of data, as well as drafted the article. TW, RW, and S conceptualized and designed the study, analysed and interpreted the data, and conducted a critical review. EA, MB, and PR designed the data collection instruments, coordinated and supervised the data collection, acquired the data, and drafted the article. AY, RE carried out the initial analysis of the study, coordinated and supervised data collection and acquisition of data. GI, SDL, PS, and AP conceptualized and designed the study, carried out analysis and interpretation of the data, and drafted the initial article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical clearance was obtained from the Medical and Health Research Ethics Committee (MHREC). Faculty of Medicine, Public Health and Nursing Universitas Gadjah Mada- Dr Sardjito General Hospital. Ref No: KE/FK/0895/EC/2021.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Haksari, E.L., Irawan, G., Lusyati, S.D. et al. Neonatal mortality and survival of low-birth-weight infants at hospitals in indonesia, a multi center study. Sci Rep 15, 31607 (2025). https://doi.org/10.1038/s41598-025-16401-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16401-x