Abstract
Hypertension can lead to hypertensive heart disease (HHD). Genetically hypertensive Schlager (BPH/2J) mice are valuable models for hypertension research. However, comprehensive sex- and age-related differences in cardiovascular phenotype and HHD progression in this model are currently lacking. Here, we aimed to investigate age- and sex-related changes in blood pressure and cardiac parameters in hypertensive BPH/2J mice and normotensive BPN/3J controls. We utilized adult (4-months) and middle-aged (10-months) mice and non-invasively assessed their blood pressure using a tail cuff method and cardiac parameters through echocardiography. Elevated mean arterial pressure (mmHg ± SD) was observed in both male (BPH/2J: 158 ± 26 versus BPN/3J: 117 ± 9) and female mice (BPH/2J:129 ± 10 versus BPN/3J: 105 ± 14) compared to their normotensive counterparts, starting at adulthood, and persisting through middle-age. Echocardiographic analysis revealed significant cardiac dysfunction in adult hypertensive males, including reductions in ejection fraction (%±SD) (BPH/2J: 41 ± 4 versus BPN/3J: 61 ± 8), and fractional shortening (%±SD) (BPH/2J: 20 ± 3 versus BPN/3J: 32 ± 6), indicating the progression of HHD. In contrast, hypertensive females showed preserved cardiac function despite elevated blood pressure, suggesting sex-based differences in how chronic hypertension affects cardiac health. There was no cardiac fibrosis or pleural effusion in either hypertensive or normotensive mice, regardless of age and sex. In conclusion, this study highlights the BPH/2J mouse as an important model for investigating sex-based cardiovascular differences in the context of hypertension.
Similar content being viewed by others
Introduction
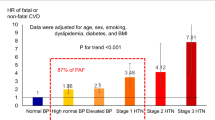
Chronically elevated blood pressure or hypertension can cause hypertensive heart disease (HHD)1,2. HHD is a constellation of structural and functional changes in the heart atria, ventricles, and coronary blood vessels. HHD is the second leading cause of heart failure (HF)3. HF patients have either a preserved (≥ 50%) left ventricular ejection fraction (HFpEF), a reduced (< 40%) ejection fraction (HFrEF), or a mid-range (40–49%) ejection fraction (HFmrEF)4. The risk of cardiovascular mortality doubles with every 20mmHg increase in systolic and 10mmHg increase in diastolic pressure above the baseline blood pressure5. The prevalence of HHD and HF is high in the elderly population6,7. According to the American Heart Association, 70% males and 78% females, between the ages of 65 and 75 were diagnosed with hypertension6. Research exploring the molecular mechanisms of HHD using preclinical models is essential for reducing the morbidity and mortality in hypertensive as well as aging patients. Therefore, we carried out this study to identify the suitability of hypertensive Schlager (BPH/2J) mice as a model for HHD.
Currently available preclinical HHD models are either surgery- or drug-induced. These HHD models do not capture the complete clinical phenotype i.e., spontaneous development of hypertension, systolic dysfunction, ventricular dilation, and heart failure. Other animal models that also develop HF include the spontaneously hypertensive, heart failure-prone (SHHF) rats and the Dahl salt-sensitive (DSS) rats. The SHHF rats develop hypertension induced cardiomyopathy and HFrEF8 at 10 months of age, whereas, the DSS rats develop hypertension mediated cardiac hypertrophy and HFpEF at 4 months of age9. Rat models of HHD that require pharmacological investigations are expensive due to higher body weight of rats compared to mice. Genetic manipulation in rats is also limited compared to mice and underscores the need for using cost effective mouse models to study HHD10. Mohammed et al., previously reported that the transverse aortic constriction (TAC) surgery along with deoxycorticosterone acetate or DOCA treatment moderately increased blood pressure and caused HFpEF development9. Available animal models have some limitations and require either surgical intervention or drug administration to develop HHD11,12. Therefore, we propose here a potential animal model to study the age- and sex-related changes in cardiovascular phenotype prevalent in HHD.
The genetically hypertensive strain of mice also known as Schlager mice (BPH/2J) is a widely used mouse model for hypertension research13. BPH/2J is an inbred strain developed by selective breeding for around 30 generations based on a high blood pressure phenotype. Blood pressure (BP) was measured in these mice using both tail- cuff and radiotelemetry devices. BPH/2J mice were reported to have higher BP compared to their normotensive counterparts (BPN/3J) starting from 5 weeks of age14,15,16. In neurogenic hypertension, peptide hormone angiotensin II increases peripheral sympathetic nerve activity17, vasomotor tone, BP, and thereby increases cardiac afterload18. The BPH/2J mice is a well characterized model of human neurogenic hypertension19 with increase sympathetic nerve activity15,16. In addition, studies by Sharma and colleagues have reported that the diabetic hypertensive male BPH/2J mice of 4.5 month of age have an increase in isovolumic relaxation time (IVRT) indicating relaxation impairment of their left ventricle10.To the best of our knowledge, our study is the first to look at the HHD phenotype in 4 M and 10 M BPH/2J male and female mice. Our goal in this study was to understand whether BPH/2J is an ideal model to study age- and sex-related differences in HHD as seen in clinics.
Methods
Animals
The experimental protocol involving animals were all approved by the Indian Institute of Technology Madras, Chennai’s Institutional Animal Ethics Committee (IITM/IAEC/6/NAJ/2020) and Indian Institute of Science, Bangalore. All experiments were performed as per the Animal in Research: Reporting In Vivo Experiments (ARRIVE) guidelines and the Guide for the care and use of laboratory animals. The breeding pairs were obtained from the Jackson Laboratory (Bar Harbor, Maine, USA). After inbreeding mice were maintained in cages with a light/dark cycle of 12 h each. The mice were given ad libitum normal chow diet (ATNT Labs, Mumbai, India) and water. In the current study, 4-month (4 M) old adult mice and 10-month (10 M) old middle-aged mice were used (5–6/group). At the end of the study protocol, mice were anesthetized using isoflurane and euthanized by cervical dislocation to assure euthanasia. The tissues were collected, snap-frozen in liquid nitrogen, and stored (-80 °C) for further analysis. Heart samples were fixed in 10% buffered formalin and paraffin embedded for sectioning and histological analysis.
Non-invasive blood pressure measurement (NIBP)
The non-invasive blood pressure system (CODA, Kent Scientific, Torrington, USA) was used for BP measurement as described previously (16, 17). In brief, all the animals were acclimatized to the holder for 5 days before actual blood pressure recording. The mice were gently placed in holders and were kept on the heating platform maintained at ~ 38℃. The tail temperature was maintained between 32–35℃ during the BP recording of the mice. Each recording session consisted of 25 cycles with 5 “acclimatizing cycles,” and 20 “recording cycles,” and each cycle duration was for 20 s. The mean arterial pressure (MAP), systolic blood pressure (SBP), and diastolic blood pressure (DBP) data were automated by CODA software 4.2. The hemodynamic parameters with standard deviation (SD) of > 30mmHg were eliminated.
Echocardiography
We performed the transthoracic echocardiography as per the protocol described earlier (18). Briefly, mice were anesthetized using 1–2% isoflurane and transthoracic echocardiography (VisualSonics Vevo 1100, Toronto, Canada) was performed. Two-dimensional echocardiography images were obtained using the MS-400 transducer. The data for fractional shortening (FS), ejection fraction (EF), cardiac output (CO), left ventricular posterior wall thickness during systole (LVPWs) and diastole (LVPW; d), left ventricular internal diameter during systole (LVIDs) and diastole (LVIDd), diameter of interventricular septum during systole (IVSs) and diastole (IVSd), were obtained from the echocardiography M-mode recording. Mitral valve (MV) function (E/A) ratio was obtained from PW mode from the ratio of average of three consecutive E (velocity of blood when MV opens) and A (velocity of blood during atrial contraction) values.
Measurement of pleural effusion
Gravimetric assessment of pulmonary edema20 was used to determine the status of pleural effusion in the lungs. The body weight (BW) as well as the lung wet weight (LW) of mice were measured on the day of tissue collection. In the BPH/2J as well as control BPN/3J mice, the calculated LW/BW ratio was compared to the lung size to evaluate the presence of lung injury. After air drying the lung tissue for around 60 h, the lung dry weight was measured and the lung wet weight/lung dry weight (W/D) ratio was calculated to look at the change in lung dry mass as an indicator for the level of pleural effusion in these mice20,21.
RT-qPCR
The frozen heart tissue (~ 50 mg) from the mice was used for total RNA isolation using TRIzol (Sigma-Aldrich #T9424, St. Louis, MO) reagent. Purity and concentration of the total RNA was measured using nanodrop (Denovix DS 11, FX+, Wimington, USA). Isolated RNA was DNase treated before cDNA synthesis using the manufacturer’s protocol (Roche, cat #4716728001, Germany). For the cDNA synthesis, 1µg of total RNA was taken and the iScript cDNA synthesis kit from Bio-Rad (#1708891, Hercules, CA) was used. Takara protocol (Takara #RR820A, Shiga, Japan) was followed to study the level of gene expression using SYBR green master mix for the primers atrial natriuretic peptide (ANP), alpha myosin heavy chain (α-MHC), alpha smooth muscle actin (α-SMA), brain derived natriuretic peptide (BNP), and the internal control glyceraldehyde phosphate dehydrogenase (GAPDH). For quantitative real time PCR (#Qiaquant 96 5 plex, Qiagen, Germany) 10 ng cDNA, and 5 picomoles of both forward primer and reverse primer were utilized. The initial denaturation was at 95°C for 30s, followed by 95℃ for 5s, and 60℃ for 34s for 40 cycles. Melt curve was also included to confirm amplified product specificity. The Ct values were normalized to GAPDH. The fold change was calculated using the 2ΔΔCT method. Nucleotide sequences for primers were as follows: MCP-1 forward primer (FP)-5’-TGCATCTGCCCTAAGGTCTTC-3’ and reverse primer (RP)-5’AAGTGCTTGAGGTGGTTGTGG-3’; ANP FP- 5’-CCTGTGTACAGTGCGGTGTC-3’ and RP- 5’-CCTCATCTTCTACCGGCATC-3’; α-MHC FP- 5’-TAAAATTGAGGACGAGCAGGC-3’ and RP- 5’-TCCAGCTCCTCGATGCGT-3’; α-SMA FP- 5’-CTGACAGAGGCACCACTGAA-3’ and RP- 5’-CATCTCCAGAGTCCAGCACA-3’; BNP FP- 5,-AAGGGAGAATACGGCATCATTG-3’ and RP- 5’-ACAGCACCTTCAGGAGATCCA-3’; GAPDH FP- 5’-TGGCAAAGTGGAGATTGTTGCC-3’ and RP- 5’-AAGATGGTGATGGGCTTCCCG-3’22.
Western blotting
Protein extraction from heart tissue was performed as described previously23. Briefly, heart tissue (~ 80 mg) was homogenized and a 200 µl lysis buffer was added. Lysate was centrifuged at ~ 14,000 g for 15 min at 4 °C. The bicinchoninic acid (BCA) assay was used for protein concentration measurement according to the manufacturer’s protocol (Thermofisher scientific, 23225). SDS PAGE (10% gel) was run at 80 V for ~ 2 h and kept for transferring overnight using activated poly vinylidene fluoride (PVDF) membrane at 20 V. The blot was washed 3 times with 1X tris buffered saline added with tween 20 (TBST) for 3 min each. Subsequently, blocking was performed with 5% skim milk (SRL #28582, New Mumbai, India) for 1 h at room temperature in a rocker with gentle shaking. After blocking, the membrane was washed and probed with primary antibody (1:1000) overnight at 4 °C (anti-natriuretic peptide A antibody, Abcam, Cat. #ab126149, Boston, MA)24. On the next day, the membrane was washed and probed with HRP conjugated secondary antibody (1:1000) (anti-rabbit IgG, Cell Signaling Technology, Cat. #7074S, Danvers, MA) for 1 h at room temperature. Then the blot was washed and the membrane was developed using an ECL substrate in a chemiluminescence imager (Bio-Rad, Singapore). Later, the blot was stripped and probed with anti-GAPDH primary antibody (1:10,000) (Abcam, Cat # ab8245) and corresponding secondary antibody-HRP conjugated (1:1000) (anti-mouse IgG, Cell Signaling Technology, Cat. # 7076 S) followed by washing and imaging.
Hematoxylin and Eosin staining
H and E staining for heart tissue was performed as per the previously published protocol25 with some modifications. Briefly, Formalin fixed paraffin embedded samples were sectioned using microtome (Leica, histocore multicut, semi motorized). Sectioned (5 μm thick) heart samples were kept at 60 °C for 60 min and allowed to cool down. Then the samples were deparaffinized with three changes of xylene for 5 min each. Then the samples were hydrated with decreasing order of alcoholic gradient as follows, 100% ethanol for 3 min three times, and 95% ethanol for 3 min followed by tap water for 3 min. The hydrated sections were incubated with Mayer’s hematoxylin (HiMedia #S058, Mumbai, India) staining for 3 min. The slides were then washed with running tap water for 4 min. Then, the sections were dipped in 1% acid alcohol (20 s) for differentiation and washed immediately with tap water (3 min). This was followed by addition of 2% eosin (Qualigens #Q38613, Mumbai, India) for 1 min followed by washed and hydration using a series of steps (95% ethanol for 1 min and 100% ethanol thrice for 45 s each). The slides were cleared with xylene (SRL #89159, New Mumbai, India) (thrice for 2 min each). Later, slides were dried and mounted using DPX mountant (Qualigens #Q18404, Mumbai, India). An optical microscope (Leica DM750, Leica Microsystems, Wetzlar, Germany) was used to visualize and acquire images. The cardiomyocyte size and area were measured using the ImageJ analysis tool. Using a single blinded method, inflammation scoring of the H and E-stained images was performed by the pathologist. Based on the inflammatory mononuclear cell infiltration in the samples, scoring was done from 0 to 4. Normal heart samples were given a score of 0 and the samples with different grade of inflammation were scored from 1 to 4.
Trichrome staining
The protocol from the Abcam trichrome staining kit (Abcam #ab150686, Danvers, MA) was used for performing trichrome staining in paraffin embedded formalin fixed heart samples. Microtome was used to obtain 5 μm thick heart sections. Slides containing the heart sections were deparaffinized, hydrated, and stained with Weigert’s iron hematoxylin solution. Then the samples were differentiated with acid alcohol and washed with running tap water. Later, Biebrich scarlet/acid fuchsin and phosphomolybdic/phosphotungstic acid were added to the slides as per the manufacturer’s protocol. After distilled water wash, acetic acid and alcohol were added to the slides as per the protocol. The xylene treated slides were mounted using DPX mountant before imaging. The Leica DM750 microscope was used for imaging the slides.
Picrosirius staining
Picrosirius red staining was performed using Abcam kit (Abcam#245887, Danvers, MA)26. Sectioned samples were kept at 60 °C for 60 min and allowed to cool down. The samples were then deparaffinized with two changes of xylene for 7 min and 30 s each, followed by a decreasing gradient of alcohol (100% ethanol, 96% ethanol, 80% ethanol, and 70% ethanol). Then, samples were hydrated with deionized water for 1 min. After hydration, samples were treated with phosphomolybdic and phosphotungstic acid for 5 min and then washed with distilled water. Picrosirius red was added and slides were incubated for 60 min at room temperature. After this, samples were treated with 0.5% acetic acid twice for 1 min and 30 s each. Then the samples were dehydrated with a series of alcohol (70% ethanol, 80% ethanol, 96% ethanol, & 100% ethanol). After xylene treatment, the slides were mounted with DPX to visualize fibrosis.
Statistics
Two-way ANOVA was used for the statistical analysis of hemodynamic parameters (MAP, SBP, DBP), echocardiography data, cardiomyocyte area, fibrosis, lung pathology, mRNA expression, and protein expression data. Statistical analysis and Tukey post hoc test were performed using GraphPad Prism version 9.5.1 for Windows, GraphPad Software, San Diego, California USA. A value of p < 0.05 was considered statistically significant.
Results
Blood pressure levels in male and female BPH/2J mice
The hemodynamic parameters (MAP, SBP, DBP) in BPN/3J and BPH/2J revealed significantly higher mean arterial pressure in 4 M old adult male BPH/2J mice compared to their normotensive adult counterparts. In female normotensive mice, blood pressure increased with aging. Furthermore, both 4 M and 10 M old female BPH/2J mice were hypertensive compared to the normotensive adult mice (P < 0.05; Table 1).
Cardiac structural and functional characteristics
The heart weight (mg) and body weight (g) were measured and represented in Fig. 1A, B for males and in Fig. 1D, E for females. In female normotensive mice there was an age mediated increase in both heart weight and body weight.
Cardiac structure of mice heart. (A) Heart weight with insert showing the representative heart images, (B) body weight, and (C) heart weight to body weight ratio (HW/BW) of 4-month (M) BPN adult, 10 M (middle age) BPN, 4 M BPH and 10 M BPH male mice. (D) Heart weight with insert showing the representative heart images, (E) body weight, and (F) heart weight to body weight ratio (HW/BW) of 4 M BPN, 10 M BPN, 4 M BPH and 10 M BPH female mice. (n = 5–6/group). Data was analyzed by Two-way ANOVA and Tukey post hoc test. *=p < 0.05.
The heart weight to body weight ratio (Fig. 1C for males; Fig. 1F for females) and heart weight to tibia length ratio (Figure S1) were also calculated. In males, compared to the adult normotensive BPN/3J, the adult BPH/2J animals have significantly higher HW/BW ratio indicating increased heart weight in hypertensive mice (Fig. 1C). We observed a similar pattern in HW/BW ratio in female BPH/2J mice (Fig. 1F) indicating sex independent effects of hypertension on heart weight in BPH/2J adult mice.
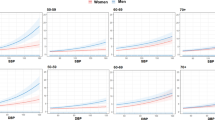
Echocardiography data revealed that in hypertensive adult and middle-aged male mice, the ejection fraction (Fig. 2A), fractional shortening (Fig. 2B), and E/A ratio (Table 2) were significantly lower than the normotensive animals. Also, the LVID during systole was higher in both hypertensive adult and middle-aged male mice as compared to normotensive adults (Table 2). However, in female mice, there was no difference in ejection fraction and fractional shortening in the adult and middle aged BPH/2J mice compared to the BPN/3J controls (Fig. 2C and D). However, there is a significantly lower E/A ratio in middle aged female mice as compared to both adult BPN/3J and BPH/2J mice, which indicates a decline in diastolic function in hypertensive females with aging (Table 2). In females, even though LVID during systole (Table 2) did not change significantly in hypertensive adults compared to normotensive adults, middle aged hypertensive females showed a higher systolic LVID in comparison with normotensive adults.
Echocardiography analysis of BPH/2J male and female mice. (A) Ejection fraction, and (B) fractional shortening in 4 M BPN, 10 M BPN, 4 M BPH and 10 M BPH male mice. (C) Ejection fraction, and (D) fractional shortening in 4 M BPN, 10 M BPN, 4 M BPH and 10 M BPH female mice. (n = 5–6/group). Data was analyzed by Two-way ANOVA and Tukey post hoc test. *=p < 0.05.
Fibrosis marker, ANP levels, and histological analysis of heart
The heart H & E revealed the cardiomyocyte histopathology, and trichrome staining and picrosirius red staining estimated the percentage of fibrosis. Figure 3A for male and Fig. 3D for females show the representative heart histology images. The inflammation score (Fig. 3B, E), cardiomyocyte area (Figure S1C, F) and collagen content or percent fibrosis (Fig. 3C, F) were not different in the BPH/2J mice, irrespective of the sex of the animals, compared to controls.
Histological analysis of normotensive and hypertensive male and female mice cardiac tissue. Images representing heart tissue sections stained with (A) H and E, trichrome staining and picrosirius red staining, (B) inflammation score, and (C) percentage of fibrosis in 4 M BPN, 10 M BPN, 4 M BPH, and 10 M BPH male mice. (D) H and E, trichrome staining and picrosirius red staining, (E) inflammation score, and (F) percentage of fibrosis in 4 M BPN, 10 M BPN, 4 M BPH, and 10 M BPH female mice (n = 3–5/group).
Atrial natriuretic peptide (ANP), alpha myosin heavy chain (α-MHC), brain natriuretic peptide (BNP), and α-smooth muscle actin (α-SMA) transcript levels were not significantly different from their normotensive counterparts in males (Figure S2). The inflammatory chemokine MCP-1 expression did not change with sex and age of mice (Figure S3). The ANP protein expression levels in BPN/3J and BPH/2J mice were also similar irrespective of the sex of the animals (Figure S4).
Pleural effusion status
The lung weight in male and female BPN/3J and BPH/2J mice was similar (Fig. 4A, D). Lung weight to body weight ratio and lung wet weight (W) to lung dry weight (D) ratio as a measure of pleural effusion were compared among adult normotensive, adult, and middle-aged hypertensive mice. The LW/BW and W/D ratio in male (Fig. 4B, C) hypertensive mice were like the normotensive control group. The LW/BW in female (Fig. 4E) normotensive and hypertensive mice showed an effect of age on body weight increase and therefore decrease in the LW/BW ratio. The W/D ratio in female (Fig. 4F) hypertensive mice were like the normotensive control group.
Determination of pulmonary effusion in the lungs of male and female Schlager mice. (A) Lung weight, (B) Lung weight to body weight ratio (LW/BW), and (C) Lung wet weight to dry weight ratio (W/D) compared among 4 M BPN, 10 M BPN, 4 M BPH and 10 M BPH male mice. (D) Lung weight, (E) Lung weight to body weight ratio (LW/BW), and (F) Lung wet weight to dry weight ratio (W/D) compared among 4 M BPN, 10 M BPN, 4 M BPH and 10 M BPH female mice. (n = 3–5/group).
The summary Fig. 5 shows the main finding of this study. The hypertensive adult and middle-aged male Schlager mice show a decrease in ejection fraction and fractional shortening whereas the female adult and middle-aged mice show no change in EF and FS compared to the normotensive control mice.
Graphical abstract. Based on our study, EF and FS decreased in adult and middle-aged hypertensive males. However, EF and FS remained unchanged in hypertensive females with respect to their normotensive counterparts. Pleural effusion remained the same in hypertensive adult and middle aged BPH/2J male and female mice compared to normotensive BPN/3J counterparts.
Discussion
Our results demonstrate that the adult and middle-aged male Schlager (BPH/2J) mice exhibit increased blood pressure, but lower ejection fraction and fractional shortening. In contrast to males, normal ejection fraction and fractional shortening were seen in adult and middle-aged female BPH/2J mice, indicating an impact of sex on cardiac functional characteristics in the hypertensive mice.
Cardiac structural and functional changes in male and female hypertensive mice
The hypertensive Schlager mice or BPH/2J and their normotensive controls, the BPN/3J mice are an established model for investigating the mechanisms of neurogenic hypertension15,16. As expected and evident from previous publications which used both telemetry and NIBP, the BPH/2J mice displayed higher blood pressure compared to BPN/3J mice14,15,16. As a confirmation tool, NIBP was used in this study to check the hypertensive and normotensive state of our mice. We chose not to do telemetry-based BP recording in this study to avoid surgery mediated change in the inflammation profile. To the best of our knowledge this is the first study to explore the hypertension induced heart failure phenotype in aging male and female BPH/2J mice.
Previous studies reported that young BPH/2J male mice displayed a slight increase in left ventricular weight normalized to tibial length and found no difference in the diastolic function in male BPH/2J mice compared to the control mice10. In another study, two-dimensional echocardiography in older spontaneously hypertensive rats (SHR) revealed a significant increase in end diastolic volume and end systolic volume, decrease in ejection fraction, and heart failure27. In the normotensive mice, with age, we saw no change in ejection fraction and fractional shortening, similar to the reports in 12 M old C57Bl/6 male28 and female29 mice, a close relative of BPN/3J mice. Our data in adult as well as middle-aged male Schlager mice showed a decrease in the ejection fraction and fractional shortening which could be due to a spontaneous and sustained increase in blood pressure in this mouse model.
Our echocardiographic analysis revealed a decrease in E/A ratio in male BPH/2J mice compared to normotensive BPN/3J. The normal mice (C57/BL6) have E/A ≥ 130. Li. et al., reported a decrease in E/A ratio in the transthoracic aortic constriction (TAC) model of heart failure in mice30. There are reports in literature on the pathological diastolic and/or systolic dysfunction with reduced E/A ratio30. Another study by Yuan et al., suggests reduction in E/A ratio as an indication of early diastole dysfunction due to impaired ventricular relaxation31. However, in adult and middle aged BPH/2J females, along with increased heart size, we also found that there was a decrease in interventricular septum thickness during diastole in adults, and an increase in left ventricular inner diameter during systole and diastole in middle aged females. These findings suggest that, as female BPH/2J mice age, their hearts undergo structural remodeling despite preserved cardiac function. This structural remodeling may represent early signs of hypertension-induced cardiac dysfunction, which warrants further investigation over time to assess the progression toward heart failure in female mice.
Aligning with previous studies10our study showed no change in inflammation, percent fibrosis or alteration in expression of fibrotic and hypertrophic markers in aged BPH/2J mice when compared to their normotensive counterparts in males. In the female mice, the cardiac inflammation was moderate to extensive in 4 M BPH/2J mice and mild to moderate in 10 M BPH/2J mice indicating hypertensive cardiac damage. In contrast to the increase in cardiomyocyte area in young BPH/2J male mice, no change in the cardiomyocyte area was observed in our study in the aging male and female BPH/2J mice. However, previous studies have reported the development of fibrosis and hypertrophy during old age (24-months) in C57BL/6 mice32. Thus, the possibility of fibrosis and hypertrophy in older BPH/2J mice needs to be explored.
Pulmonary effusion is a hallmark of HF33 with interstitial accumulation of pathological extracellular fluid in HFpEF as well as HFrEF patients34,35. In our study, we checked for lung water content in the hypertensive BPH/2J mice to assess pleural effusion. However, there was not a significant difference in lung weight and lung water content in BPH/2J strain in comparison with its normotensive controls in both males and females. Our data in the BPH/2J mice model (where the mice develop hypertension spontaneously) is supported by the data by Bing. et al., where they observed in old spontaneously hypertensive rats with heart failure that there was no significant difference in lung weight and water weight27. However, contradictory to our report and others, a previous study in middle aged angiotensin II treated Balb/c mice showed an increased lung weight to tibial length ratio (significant lung congestion) compared to vehicle controls36. Based on our observation and reports from other researchers, pleural effusion measurement in older Schlager mice, with and without pharmacological stressors is warranted.
In human patients, HF with reduced EF is characterized by eccentric left ventricular hypertrophy, cardiac stiffening, systolic dysfunction, fibrosis, atrial dilation, endothelial dysfunction, and/or inflammation37. Whereas, HF with preserved EF is characterized by concentric left ventricular hypertrophy, cardiac stiffening, diastolic dysfunction, fibrosis, atrial dilation, endothelial dysfunction, or inflammation38. Our study in hypertensive BPH/2J mice revealed reduced EF in male mice and preserved EF in female mice. The functional similarity between human HF patients and the BPH/2J mice could make this a potential model to study HHD.
There are a few limitations in our current study. First, we have only looked at the sex differences in the HHD characteristics in adult and middle aged genetically hypertensive BPH/2J mice and compared it with adult and middle aged normotensive BPN/3J mice. We have not included an older group of hypertensive mice due to the non-availability of older mice. Studies have already reported HHD and HF as a disorder of aging39 and thus understanding the possibility of an older age group (~ 18-24-months) of BPH/2J mice developing HHD will be useful to provide individualized care to hypertensive older populations. Second, our study lacks the motor activity assessment and exercise intolerance study data to confirm whether the adult genetically hypertensive BPH/2J mice model shows signs of exercise intolerance which is reported in HHD and HF40. Future studied could explore these questions.
In conclusion, we have used data from normotensive and hypertensive Schlager mice to assess the cardiac structural and functional characteristics, lung function, hypertrophic and inflammatory genes expression, protein expression, and collagen content. We conclude that first, there is significant reduction in the cardiac function and changes in the cardiac structures indicating hypertension- induced structural remodeling in male BPH/2J mice. Second, this model characterization study will be useful for researchers who plan to use Schlager mice in their cardiovascular research. In the future, administration of drugs or physiological stressors41 may be required for clear understanding of heart failure development in the hypertensive Schlager mice.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Ponikowski, P. et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 1(1), 4–25. https://doi.org/10.1002/ehf2.12005 (2014).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am. Coll. Cardiol. 22(25), 2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010 (2020).
Bragazzi, N. L. et al. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. Eur J. Prev. Cardiol. 29(15), 1682–1690. https://doi.org/10.1093/eurjpc/zwaa147 (2021).
Ueda, T. et al. Left ventricular ejection fraction (EF) of 55% as cutoff for late transition from heart failure (HF) with preserved EF to HF with mildly reduced EF. Circ. J. 79(10), 2209–2215. https://doi.org/10.1253/circj.CJ-15-0425 (2015).
Lewington, S. et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 14(9349), 1903–1913. https://doi.org/10.1016/s0140-6736(02)11911-8 (2002).
Benjamin, E. J. et al. Heart disease and stroke Statistics-2019 update: A report from the American heart association. Circulation 05(10), e56–e528. https://doi.org/10.1161/CIR.0000000000000659 (2019).
Chang, A. Y., Skirbekk, V. F., Tyrovolas, S., Kassebaum, N. J. & Dieleman, J. L. Measuring population ageing: an analysis of the global burden of disease study 2017. Lancet Public. Health 4(3), e159–e167. https://doi.org/10.1016/S2468-2667(19)30019-2 (2019).
Fellmann, L., Nascimento, A. R., Tibiriça, E. & Bousquet, P. Murine models for Pharmacological studies of the metabolic syndrome. Pharmacol. Ther. 137(3), 331–340. https://doi.org/10.1016/j.pharmthera.2012.11.004 (2013).
Doi, R. et al. Development of different phenotypes of hypertensive heart failure: systolic versus diastolic failure in Dahl salt-sensitive rats. J. Hypertens. 18(1), 111–120. https://doi.org/10.1097/00004872-200018010-00016 (2000).
Sharma, A. et al. Cardiovascular characterisation of a novel mouse model that combines hypertension and diabetes co-morbidities. Sci. Rep. 30(1), 8741. https://doi.org/10.1038/s41598-023-35680-w (2023).
Gomes, A. C., Falcão-Pires, I., Pires, A. L., Brás-Silva, C. & Leite-Moreira, A. F. Rodent models of heart failure: an updated review. Heart Fail. Rev. 18(2), 219–249. https://doi.org/10.1007/s10741-012-9305-3 (2013).
Mohammed, S. F. et al. Mineralocorticoid accelerates transition to heart failure with preserved ejection fraction via nongenomic effects. Circulation 27(4), 370–378. https://doi.org/10.1161/CIRCULATIONAHA.109.915215 (2010).
Schlager, G. Biometrical genetic analysis of blood pressure level in the genetically hypertensive mouse. Clin Exp. Hypertens. 16(6), 809–824. https://doi.org/10.3109/10641969409078027 (1994).
Schlager, G. & Sides, J. Characterization of hypertensive and hypotensive inbred strains of mice. Lab Anim. Sci. 47(3), 288–292 (1997).
Davern, P. J., Nguyen-Huu, T. P., La Greca, L., Abdelkader, A. & Head, G. A. Role of the sympathetic nervous system in schlager genetically hypertensive mice. Hypertension 54(4), 852–859. https://doi.org/10.1161/HYPERTENSIONAHA.109.136069 (2009).
Asirvatham-Jeyaraj, N. et al. Renal denervation and Celiac ganglionectomy decrease mean arterial pressure similarly in genetically hypertensive schlager (BPH/2J) mice. Hypertension 02(2), 519–528. https://doi.org/10.1161/HYPERTENSIONAHA.119.14069 (2021).
Lamptey, R. N. L., Sun, C., Layek, B. & Singh, J. Neurogenic hypertension, the Blood-Brain barrier, and the potential role of targeted nanotherapeutics. Int J. Mol. Sci. 22(3). https://doi.org/10.3390/ijms24032213 (2023).
Kassan, A., Ait-Aissa, K. & Kassan, M. Hypothalamic miR-204 induces alteration of heart electrophysiology and neurogenic hypertension by regulating the sympathetic nerve activity: potential role of microbiota. Cureus 13(10), e18783. https://doi.org/10.7759/cureus.18783 (2021).
DiBona, G. F. & Esler, M. Translational medicine: the antihypertensive effect of renal denervation. Am J. Physiol. Regul. Integr. Comp. Physiol. 298(2), R245–R253. https://doi.org/10.1152/ajpregu.00647.2009 (2010).
Parker, J. C. & Townsley, M. I. Evaluation of lung injury in rats and mice. Am J. Physiol. Lung Cell. Mol. Physiol. 286(2), L231–L246. https://doi.org/10.1152/ajplung.00049.2003 (2004).
Ma, X. et al. A mouse model of heart failure exhibiting pulmonary edema and pleural effusion: useful for testing new drugs. J. Pharmacol. Toxicol. Methods. 96, 78–86. https://doi.org/10.1016/j.vascn.2019.02.001 (2019).
Sarikhani, M. et al. SIRT2 deacetylase represses NFAT transcription factor to maintain cardiac homeostasis. J. Biol. Chem.. 06(14), 5281–5294. https://doi.org/10.1074/jbc.RA117.000915 (2018).
Ravi, V., Jain, A., Mishra, S. & Sundaresan, N. R. Measuring protein synthesis in cultured cells and mouse tissues using the Non-radioactive sunset assay. Curr Protoc. Mol. Biol. 133(1), e127. https://doi.org/10.1002/cpmb.127 (2020).
Su, F., Shi, M., Zhang, J., Li, Y. & Tian, J. Recombinant high–mobility group box 1 induces cardiomyocyte hypertrophy by regulating the 14–3–3η, PI3K and nuclear factor of activated T cells signaling pathways. Mol Med. Rep. 23(3). https://doi.org/10.3892/mmr.2021.11853 (2021).
Hay, A., Lapointe, J. M., Lewis, A., Moreno Quinn, C. & Miranda, E. Optimization of RNA extraction from laser captured microdissected glomeruli from formalin-fixed paraffin-embedded mouse kidney samples for Nanostring analysis. Histol. Histopathol.. 35(1), 57–68. https://doi.org/10.14670/HH-18-135 (2020).
Wang, H. et al. Natural cardiac regeneration conserves native biaxial left ventricular biomechanics after myocardial infarction in neonatal rats. J Mech. Behav. Biomed. Mater. 126, 105074. https://doi.org/10.1016/j.jmbbm.2022.105074 (2022).
Bing, O. H. et al. The spontaneously hypertensive rat as a model of the transition from compensated left ventricular hypertrophy to failure. J Mol. Cell. Cardiol. 27(1), 383–396. https://doi.org/10.1016/s0022-2828(08)80035-1 (1995).
Kang, R. et al. Age-Related shift in cardiac and metabolic phenotyping linked to inflammatory cytokines and antioxidant status in mice. Int J. Mol. Sci. 31(21). https://doi.org/10.3390/ijms242115841 (2023).
Kiper, C., Grimes, B., Van Zant, G. & Satin, J. Mouse strain determines cardiac growth potential. PLoS One. 8(8), e70512. https://doi.org/10.1371/journal.pone.0070512 (2013).
Li, L. et al. Assessment of cardiac morphological and functional changes in mouse model of transverse aortic constriction by echocardiographic imaging. J. Vis. Exp. 21(112). https://doi.org/10.3791/54101 (2016).
Zhang, Q. et al. Chloroquine differentially modulates coronary vasodilation in control and diabetic mice. Br. J. Pharmacol. 177(2), 314–327. https://doi.org/10.1111/bph.14864 (2020).
Achkar, A., Saliba, Y. & Fares, N. Differential Gender-Dependent patterns of cardiac fibrosis and fibroblast phenotypes in aging mice. Oxid. Med. Cell. Longev. 2020, 8282157. https://doi.org/10.1155/2020/8282157 (2020).
Cleland, J. G. F. et al. The struggle towards a universal definition of heart Failure-how to proceed? Eur. Heart J. 21(24), 2331–2343. https://doi.org/10.1093/eurheartj/ehab082 (2021).
Valero-Muñoz, M., Backman, W. & Sam, F. Murine models of heart failure with preserved ejection fraction: a fishing expedition. JACC Basic. Transl. Sci. 2(6), 770–789. https://doi.org/10.1016/j.jacbts.2017.07.013 (2017).
Gladysheva, I. P., Sullivan, R. D. & Pellicori, P. Editorial: Edema in heart failure with reduced ejection fraction. Front. Cardiovasc. Med. 10, 1141937. https://doi.org/10.3389/fcvm.2023.1141937 (2023).
Peng, H. et al. Angiotensin II-induced dilated cardiomyopathy in balb/c but not C57BL/6J mice. Exp. Physiol. 96(8), 756–764. https://doi.org/10.1113/expphysiol.2011.057612 (2011).
Noll, N. A., Lal, H. & Merryman, W. D. Mouse models of heart failure with preserved or reduced ejection fraction. Am J. Pathol. 190(8), 1596–1608. https://doi.org/10.1016/j.ajpath.2020.04.006 (2020).
Oktay, A. A., Rich, J. D. & Shah, S. J. The emerging epidemic of heart failure with preserved ejection fraction. Curr Heart Fail. Rep. 10(4), 401–410. https://doi.org/10.1007/s11897-013-0155-7 (2013).
Mosterd, A. & Hoes, A. W. Clinical epidemiology of heart failure. Heart 93(9), 1137–1146. https://doi.org/10.1136/hrt.2003.025270 (2007).
Del Buono, M. G. et al. Exercise intolerance in patients with heart failure: JACC State-of-the-Art review. J. Am. Coll. Cardiol. 73(17), 2209–2225. https://doi.org/10.1016/j.jacc.2019.01.072 (2019).
Fujita, K., Ellis, M. W. & Sheikh, F. Calcium stress adds a third hit in driving heart failure with preserved ejection fraction. Am J. Physiol. Heart Circ. Physiol . 01(4), H414–H416. https://doi.org/10.1152/ajpheart.00075.2023 (2023).
Acknowledgements
The authors would like to thank the Indian Institute of Technology Madras animal house core facility for help with shared equipment for the study. A special thanks to Dr. Priya Balasubramanian for editorial contributions to the manuscript.
Funding
The study was supported by the Core Research Grant CRG/2020/002228 from the Anusandhan National Research Foundation (Science and Engineering Research Board), India (to N.A.J. and N.R.S). N.A.J is a recipient of the Har-Gobind Khorana Innovative Young Biotechnologist Fellowship (IYBF) from the Department of Biotechnology, Government of India. DS would like to acknowledge the support by the Department of Biotechnology, Ministry of Science and Technology, Government of India.
Author information
Authors and Affiliations
Contributions
D.S. carried out the experiments and performed data analysis; G.S. and S.S performed staining experiments; B.S maintained the mice and carried out echocardiography experiment; S.P.T and G.J. performed blood pressure data collection; M.P, M.B.M.S, and K.V. carried out the RT-PCR studies; A.B.P standardized the experimental protocol; D.S. and G.S. wrote the manuscript; A.P-M provided inflammation score; N.R.S approved the final version of the manuscript; N.A.J conceived the idea, designed the study, supervised analysis of data, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sunil, D., Subramaniam, G., Shivanaiah, B. et al. Sex based cardiovascular differences in adult and middle-aged hypertensive schlager mice. Sci Rep 15, 31679 (2025). https://doi.org/10.1038/s41598-025-16459-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-16459-7