Abstract
Mild cognitive impairment (MCI) is a pre-dementia phase preceding dementia of the Alzheimer’s type (DAT). Despite numerous studies exploring the risk factors for the conversion from MCI to DAT, the results have been heterogeneous. This study aimed to investigate the incidence of the conversion from MCI to DAT and the risk factors contributing to DAT conversion in Korean patients with MCI. A 12-year nationwide retrospective study was conducted. We enrolled patients with MCI aged ≥ 40 years between 2009 and 2015 and followed them up until 2020. The incidence of DAT conversion based on age at MCI diagnosis and its risk factors were analyzed using Cox proportional hazards regression. The conversion rate of DAT in patients with MCI increased during the age range of 70 to 90 years, and approached a plateau near the age of 100 years. Being underweight (hazard ratio [HR] 1.279, 95% confidence interval [CI] 1.223–1.338) was associated with a higher risk of DAT conversion. Cardiometabolic diseases (diabetes, HR 1.373, 95% CI 1.342–1.406; coronary heart disease, HR 1.047, 95% CI 1.015–1.079; and hemorrhagic stroke, HR 1.342, 95% CI 1.296–1.390;) increased the risk of DAT conversion, whereas hypertension, ischemic stroke, and dyslipidemia did not. Depression (HR 1.736, 95% CI 1.700–1.773) and physical inactivity (HR 1.193, 95% CI 1.161–1.227) were related to the increased risk. Mild (HR 0.860, 95% CI 0.830–0.891) to moderate (HR 0.880, 95% CI 0.837–0.926) alcohol consumption, high income (HR 0.947, 95% CI 0.925–0.970), and urban residence (HR 0.889, 95% CI 0.872–0.907) were associated with the decreased risk of DAT conversion. Multiple modifiable risk factors were closely associated with an increased risk of DAT conversion. Our results may help in designing preventive strategies to mitigate the risk of DAT conversion in patients with MCI.
Similar content being viewed by others
Introduction
Mild cognitive impairment (MCI) is an intermediate state between normal aging and dementia, with cognitive decline greater than expected for an individual’s age and education level; however, it does not affect independence in daily life1. Therefore, identifying the incidence rate of dementia conversion and effective strategies to delay dementia conversion are important for planning public health care policies. According to the population-based studies, 5–30% of patients with MCI progress to dementia annually2. However, the considerable variations in conversion rates may be influenced by factors, such as study design, population characteristics (including race/ethnicity), and various risk factors3,4,5,6,7.
Numerous studies have explored and evaluated the risk factors predictive of the conversion from MCI to dementia of the Alzheimer’s type (DAT), which accounts for the largest proportion of dementia cases. Among immutable risk factors, old age was strongly related to DAT conversion and female sex and low education levels showed heterogenous result8,9. Among modifiable risk factors, diabetes, low body weight, and depression are usually associated with an increased risk of DAT conversion9,10. However, hypertension, stroke, and cardiac disease were not always associated with the increased risk9,10,11,12,13. Moreover, dyslipidemia showed wide variation, from protective to worse outcome14,15. Smoking and alcohol consumption were not always associated with an increased risk. Alcohol consumption showed protective effect in some studies14,16,17.
Race/ethnicity affects DAT conversion18,19 and modulates the effects of cardiometabolic syndromes on brain health20. Specifically, Asians are more likely to develop cardiometabolic syndrome-related complications, including coronary artery disease21, stroke22, dementia23,24, or mortality25. Therefore, it is important to identify modifiable risk factors in European as well as Asian populations. However, only few longitudinal large-cohort studies have evaluated the risk factors for the conversion from MCI to DAT in Asian populations.
In the present study, we investigated the incidence of MCI to DAT conversion in Korean population based on the Korea National Health Insurance System (KNHIS) data and explored the risk factors contributing to DAT conversion.
Methods
Data source
We used a customized dataset from the KNHIS, which encompasses more than 99% of Koreans population (approximately 50 million individuals) (http://nhiss.nhis.or.kr). The KNHIS database includes personal information, health insurance claim codes (procedures and prescriptions), diagnostic codes from the Korean Standard Classification of Diseases, 7th Revision based on the International Classification of Diseases, 10th Revision (ICD-10), death records from the Korean National Statistical Office, and general health screening examination data for each participant from 2002 to 2019.
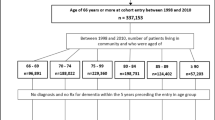
Study participants
Patients aged ≥ 40 years with MCI first diagnosed between 2009 and 2015 were enrolled using ICD-10 codes (F06.8 or R41.3). In total, 642,954 eligible candidates were identified. We excluded patients who had following conditions: 27,477 patients with a prior history of dementia, 15,239 patients with a dementia diagnosis within 6 months after MCI diagnosis, 11 patients who died at baseline, and 263,914 patients without information on risk factors at baseline (body mass index [BMI], 253,124; smoking status, 253,749; alcohol consumption, 254,356; physical activity, 253,816; income, 14,332; residential area, 169). The study was reviewed and approved by the Institutional Review Board of Korea University Guro Hospital. Due to the retrospective nature of the study, Institutional Review Board of Korea University Guro Hospital waived the need of obtaining informed consent. All procedures performed in human studies were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Assessment of risk factors
Hypertension, diabetes, dyslipidemia, coronary heart disease, ischemic stroke, hemorrhagic stroke, depression, and osteoporosis were considered as risk factors. The presence of hypertension was defined according to the ICD-10 code (I10-13, I15) and prescription of antihypertensive medication. The presence of diabetes was defined according to the ICD-10 code (E10-14) and prescription of antidiabetic medication. The presence of dyslipidemia was defined according to the ICD-10 code (E78) and prescription of lipid-lowering medication. The presence of coronary heart disease was defined according to the ICD-10 code (I20-25) and prescription of antiplatelet or anticoagulation agents. The presence of ischemic stroke was defined according to the ICD-10 code (I63-66) and prescription of antiplatelet or anticoagulation agents. Hemorrhagic stroke (I60-62), depression (F32-34), and osteoporosis (M80-82) were defined using at least one ICD-10 code.
The BMI, smoking status, alcohol consumption, and physical activity data were obtained from a health screening examination database. Obesity, overweight, and underweight were defined as BMI ≥ 25 kg/m2, 23 ≤ BMI < 25, and BMI < 18.5 kg/m2, respectively. For male and female patients, heavy alcohol consumption was defined as drinking > 60 g and > 40 g alcohol per day, respectively, moderate consumption was defined as drinking between 20–60 g and 10–40 g alcohol per day, respectively, and mild consumption was defined as drinking < 20 g and < 10 g alcohol per day, respectively26. Smoking status was defined as none, ex-smoker, and current smoker. Physical activity was defined as none and active. Specifically, active exercise was defined as high-intensity exercise ≥ 3 times a week or moderate-intensity exercise ≥ 5 times a week during the past week. Income level and residential area were obtained from personal information. Income level was categorized by percentile: ≤ 30th and > 30th. The residential areas were classified as urban or rural. Urban areas were defined as Seoul, six other large cities, and cities with a population > 300,000.
Definition of outcome and follow-up
The outcome of the study was DAT conversion (participants with newly diagnosed dementia who received dementia medication among patients with MCI), which was defined according to ICD-10 codes (F00, F02, F03, G30, and G31), and simultaneous prescription of dementia medications, including donepezil, rivastigmine, galantamine, and memantine. The patients were followed-up from the date of MCI diagnosis (baseline) to the date of DAT diagnosis, date of death, or until the end of the study period (December 31, 2020).
Statistical analysis
Baseline characteristics are presented as mean ± standard deviation (SD) and frequency (%). The incidence of DAT conversion was calculated per 1,000 person-years, and trends by age group of MCI diagnosis were analyzed using the Cochrane–Armitage and linearity tests. The cumulative incidence of DAT conversion was calculated using Kaplan–Meier curves. Univariable and multivariable Cox proportional hazard regression analyses were performed to identify the factors associated with DAT conversion. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using the models. The multivariable analysis included factors such as age, sex, BMI, baseline comorbidities (hypertension, diabetes, dyslipidemia, coronary heart disease, ischemic stroke, hemorrhagic stroke, depression, and osteoporosis), alcohol consumption, physical activity, income, and residential area, which were statistically significant in the univariable analysis.
All reported p-values were two-sided and the significance level was set at 0.05. All analyses were performed using SAS Enterprise Guide 7.1 (SAS Institute Inc., Cary, NC, USA).
Results
Demographic and clinical characteristics
The demographics and clinical characteristics of the patients are presented in Table 1. In total, 336,313 patients with MCI were enrolled in this study. The mean age of patients was 67.5 ± 9.3 years and 67.7% were female. Of all patients, 10,062 (3.0%), 117,061 (34.8%), 88,752 (26.4%), and 120,438 (35.8%) were underweight (BMI < 18.5 kg/m2), normal weight (18.5 ≤ BMI < 23), overweight was (23 ≤ BMI < 25), and obese (≥ 25 kg/m2), respectively. The prevalence of hypertension, diabetes, dyslipidemia, coronary heart disease, ischemic stroke, and hemorrhagic stroke was 51.2%, 17.0%, 29.8%, 8.9%, 8.5%, and 11.6%, respectively. The proportion of patients with depression, osteoporosis, current smoking, heavy drinking, and physical inactivity was 20.7%, 28.5%, 8.0%, 1.4%, and 80.6%, respectively. The median follow-up duration was 6.7 years.
Conversion and conversion rate of DAT
The total number of DAT cases were 102 in the 40 s, 1453 in the 50 s, 7,863 in the 60 s, 23,290 in the 70 s, and 8,967 in those over 80. The DAT conversion rate per 1000 person-year increased with age (p for trend = 0.025) (Table 2). The conversion of DAT was lower in individuals aged 40–60 years, but increased in those aged 70–90 years and reached a plateau near the age of 100 years (Fig. 1).
Conversion rate from MCI to DAT according to the age at diagnosis. The conversion rate from MCI to DAT varies according to the age at diagnosis. The conversion of DAT is lower in individuals aged 40–60 years, but rises in individuals aged 70–90 years and reaches a plateau near the age of 100 years. DAT, dementia of the Alzheimer’s type; MCI, mild cognitive impairment.
DAT conversion according to age and sex
Older age was independently related to DAT conversion (HR, 1.107; 95% CI 1.106–1.109). Female sex was associated with the decreased risk of DAT conversion (HR 0.932; 95% CI 0.910–0.954). After stratification of age group, females in the young age group (< 65 years) (HR, 0.587; 95% CI 0.537–0.642) were less likely to undergo DAT conversion, whereas those in the old age group (≥ 65 years) (HR, 1.007; 95% CI 0.980–1.035) were not associated with a decreased risk of DAT conversion (Fig. 2, Table 3).
Risk factors for DAT conversion
Compared with normal weight, underweight was associated with an increased risk (HR, 1.279; 95% CI 1.223–1.338), and overweight (HR, 0.856; 95% CI 0.835–0.877) or obese (HR, 0.802; 95% CI 0.783–0.821) were associated with a decreased risk of DAT conversion. Among cardiometabolic syndromes and related complications, the presence of diabetes (HR, 1.373; 95% CI 1.342–1.406), coronary heart disease (HR, 1.047; 95% CI 1.015–1.079), and hemorrhagic stroke (HR, 1.342; 95% CI 1.296–1.390) independently increased the risk of DAT conversion. However, the presence of hypertension (HR, 0.994; 95% CI 0.974–1.015) and ischemic stroke (HR 1.024; 95% CI 0.983–1.066) were not associated with the risk of DAT conversion. Dyslipidemia was related to a decreased risk of DAT conversion (HR, 0.887; 95% CI 0.867–0.907). Depression was independently related to an increased risk of DAT (HR, 1.736; 95% CI 1.700–1.773), whereas osteoporosis was not related. In addition, smoking status was not associated with the risk of DAT conversion. Mild (HR, 0.860; 95% CI 0.830–0.891) and moderate (HR, 0.880; 95% CI 0.837–0.926) alcohol consumption was related to a decreased risk of DAT conversion compared with no alcohol consumption. Heavy alcohol consumption was not associated with an increased or decreased risk of DAT conversion. Physically inactivity was associated with an increased risk of DAT conversion (HR, 1.193; 95% CI 1.161–1.227). High income (HR, 0.947; 95% CI 0.925–0.970) and residence in urban areas (HR, 0.889; 95% CI 0.872–0.907) were related to a decreased risk of DAT conversion (Table 3).
Discussion
In this study, we evaluated the incidence of conversion from MCI to DAT and the associated risk factors using large cohort data from the KNHIS. Our major findings are as follows. First, the conversion rate of DAT in patients with MCI increased at the age of 70 years and approached a plateau near the age of 100 years. Second, underweight status was associated with an increased rate of DAT conversion. Third, cardiometabolic syndromes, except for hypertension, ischemic stroke, and dyslipidemia, increased the risk of DAT conversion. Fourth, depression and physical inactivity were associated with an increased risk of DAT conversion. Finally, mild-to-moderate alcohol consumption, high income, and residence in an urban area were associated with a decreased risk of DAT conversion. Our findings suggest that multiple modifiable risk factors are closely associated with an increased risk of DAT conversion. Furthermore, our results may help in designing preventive strategies to mitigate the risk of DAT conversion in patients with MCI.
Age is the most significant risk factor of dementia27,28. We replicated the finding that age is related to an increased risk of DAT conversion in patients with MCI. However, there have been conflicting results regarding the incidence of dementia, which continuously increases with age or plateaus at some point29. In the present study, DAT conversion was increased as age at diagnosis increased before the age of 100 years. It was approximately 1% (1.2 per person-year) in patients in their 40’s and more than 30% (59.5 per person-year) in > 80’s. However, this rate plateaued at approximately 100 years of age. The number of patients aged > 100 years was insufficient, and further studies, especially longitudinal studies of the oldest-old, are needed to verify the relationship between extreme aging and DAT conversion.
Male sex was associated with a higher risk of DAT conversion, although there was a relatively high proportion of female patients with MCI. The finding that females accounted for a large proportion of patients with MCI were consistent with the findings of many epidemiologic studies. However, the vulnerability of males to DAT conversion is conflicting. After stratification by age, the association was evident only in the younger age group (< 65 years old). Several studies have shown similar trends: a higher incidence of DAT in women than in men after the 80’s and vice versa before the 80’s30,31. In addition, the rate of progression from MCI to DAT was higher in males in their 70’s but higher in female aged > 80 years32. Previous studies, that aimed to identify the exact mechanism of gender-based difference in the prevalence of DAT have reported that tau pathology, a core feature of Alzheimer’s disease (AD), accumulated at a faster rate in females compared to males33. However, despite comparable levels of pathology and neurodegeneration in the early stages of DAT, males tended to exhibit lower cognitive performance than females, suggesting that males may possess a lower cognitive reserve than females34,35. In other words, these findings may be related to lower cognitive function and faster cognitive decline in males than females in the presence of comparable AD pathological burden36,37, which may have contributed to our findings.
Being underweight was associated with the risk of DAT conversion. This finding is consistent with previous studies. Specifically, being underweight in late life is associated with accelerated neurodegeneration38 and an increased risk of DAT39,40. Additionally, individuals who are underweight in late life are associated with an increased risk of β-amyloid (Aβ) deposition41.
Among cardiometabolic syndromes, diabetes, coronary heart disease, and hemorrhagic stroke increased the risk of dementia conversion. Several epidemiological studies have found that the incidence of DAT is higher in patients with diabetes that in patients without diabetes32,33,34. Additionally, high blood glucose variability or insulin resistance was associated with Aβ deposition42,43. Coronary heart disease is associated with an increased risk of dementia44 and contribute to neuropathology associated with DAT45. In terms of hemorrhagic stroke, lobar hemorrhage, part of hemorrhagic stroke, is known to be a clinical manifestation of cerebral amyloid angiopathy (CAA) which involves cerebrovascular deposition of Aβ. Given that CAA and DAT often overlap due to the shared role of Aβ, patients with MCI with hemorrhagic stroke were more likely to have Aβ deposition, which in turn increased the risk of DAT conversion. In fact, patients with DAT are likely to have a higher risk of hemorrhagic stroke, but not of ischemic stroke, compared to controls46.
Hypertension and ischemic stroke were not related to the risk of DAT conversion. Hypertension is related to vascular dementia; however, its relationship with DAT seems controversial47. In addition, since the patients with hypertension in our study were prescribed anti-hypertensive medication, well-controlled hypertension might not be related to cognitive decline in patients with MCI48. Ischemic stroke is a risk factor for vascular dementia49,50,51,52; however, its relationship with DAT is not consistent. Thus, after controlling for other risk factors, the independent effect of ischemic stroke on progression from MCI to DAT may not be significant.
We also found that dyslipidemia was associated with a decreased risk of DAT in patients with MCI. This may be related to the definition of dyslipidemia in our study. Dyslipidemia was defined according to the ICD-10 code (E78) and the prescription of lipid-lowering medications. Higher LDL was related to an increased Aβ burden53,54; however, DAT risk may be lower in patients treated with statin54,55. Thus, dyslipidemia itself may be related to an increased risk of DAT; however, treatment with statins could modify the consequences.
Physical inactivity 56,57,58 and depression59,60 are related to the risk of DAT conversion in patients with MCI, which is consistent with the findings of previous studies. In particular, the effect size of depression on conversion to DAT was higher than that of the other evaluated risk factors. Mild to moderate alcohol consumption was associated with a decreased risk of dementia compared with abstinence. However, studies on the relationship between alcohol consumption and cognitive impairment have yielded conflicting results. Several studies have shown that there may be a J-shaped relationship between alcohol consumption and developing DAT17,61,62.
Urbanization was associated with a decreased risk of AD after adjusting for age, sex, education, comorbidities, and lifestyle factors. These findings are consistent with previous studies63,64,65. In addition, the prevalence of MCI was higher in urban areas, and urbanization was associated with a decreased risk of developing DAT. This may be attributed to the lower likelihood of MCI diagnosis in rural areas than that in urban areas. Reduced opportunities to encounter healthcare providers and a more monotonous lifestyle in rural areas may lead to individuals being diagnosed with MCI less frequently and at later stages of the condition. Low socioeconomic status (SES) is a risk factor for the development of DAT66,67,68. However, most studies that have assessed SES in patients with dementia were predominantly based on educational and occupational categories. Only few studies have measured SES based on household income, as in our study68. Household income may be a more appropriate marker for assessing SES in retired older adults. Education is typically attained early in life. Based on findings regarding urbanization and high income, policies aimed at caring for patients with cognitive impairment should prioritize low-income individuals residing in rural areas.
The present study had some limitations. First, because only modifiable risk factors that patients with MCI had at baseline were included, we did not consider changes in the status of modifiable risk factors after MCI diagnosis. Second, due to the limitation of data that were not originally aimed at studying cognitive impairment and AD, we could not assess patients’ exact cognitive performance, years of education, apolipoprotein E genotype, and biomarkers including Aβ. Although the operational definition of DAT conversion was based on both ICD-10 codes and concurrent dementia medications, the lack of neuropsychological test scores or biomarker data may have led to diagnostic heterogeneity and potential misclassification. This may especially be relevant for distinguishing DAT from other types of dementia such as vascular dementia, dementia with Lewy bodies, and frontotemporal dementia. These limitations should be considered when interpreting our findings. Third, the presence of cardiometabolic syndromes was determined based on the patient’s history of diagnosis or medications, rather than clinical examinations. Nevertheless, the strengths of this study are the large number of patients with MCI and the long follow-up duration based on a nationwide cohort. Additionally, our study was based on Korean patients with MCI, who may be influenced by cultural and genetic factors that are different from those in Western countries.
Conclusions
In conclusion, we verified that older age, male sex, low body weight, diabetes, coronary heart disease, hemorrhagic stroke, depression, abstaining from alcohol, and physical inactivity were risk factors for the progression from MCI to DAT in a large-scale cohort study. It is important to understand the trend of the DAT conversion rate and modifiable risk factors in patients with MCI to establish optimal strategies for mitigating the risk of DAT conversion. Considering that the restricted treatment alternatives are available for AD, there is a pressing need to prioritize prevention strategies, particularly through strict blood glucose control, encouraging physical activity, and caring for depression among patients with MCI who are at a heightened risk of DAT.
Data availability
The datasets used and/or analyses during the current study available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- Aβ:
-
β-Amyloid
- BMI:
-
Body mass index
- CAA:
-
Cerebral amyloid angiopathy
- CI:
-
Confidence interval
- DAT:
-
Dementia of the Alzheimer’s type
- HR:
-
Hazard ratio
- ICD-10:
-
International Classification of Diseases, 10th Revision
- KNHIS:
-
Korea National Health Insurance System
- MCI:
-
Mild cognitive impairment
- SD:
-
Standard deviation
- SES:
-
Socioeconomic status
References
Gauthier, S. et al. Mild cognitive impairment. Lancet 367, 1262–1270 (2006).
Ward, A., Tardiff, S., Dye, C. & Arrighi, H. M. Rate of conversion from prodromal Alzheimer’s disease to Alzheimer’s dementia: A systematic review of the literature. Dement. .Geriatr Cognit. Disord. Extra 3, 320–332 (2013).
Thaipisuttikul, P., Jaikla, K., Satthong, S. & Wisajun, P. Rate of conversion from mild cognitive impairment to dementia in a Thai hospital-based population: A retrospective cohort. Alzheimer’s Dement. Transl. Res. Clin. Interv. 8, e12272 (2022).
Farias, S. T., Mungas, D., Reed, B. R., Harvey, D. & DeCarli, C. Progression of mild cognitive impairment to dementia in clinic-vs community-based cohorts. Arch. Neurol. 66, 1151–1157 (2009).
Mitchell, A. J. & Shiri-Feshki, M. Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatr. Scand. 119, 252–265 (2009).
Manly, J. J. et al. Frequency and course of mild cognitive impairment in a multiethnic community. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 63, 494–506 (2008).
Mitchell, A. & Shiri-Feshki, M. Temporal trends in the long term risk of progression of mild cognitive impairment: A pooled analysis. J. Neurol. Neurosurg. Psychiatr. 79, 1386–1391 (2008).
Visser, P. J., Kester, A., Jolles, J. & Verhey, F. Ten-year risk of dementia in subjects with mild cognitive impairment. Neurology 67, 1201–1207 (2006).
Li, J.-Q. et al. Risk factors for predicting progression from mild cognitive impairment to Alzheimer’s disease: A systematic review and meta-analysis of cohort studies. J. Neurol. Neurosurg. Psychiatry 87, 476–484 (2016).
Cooper, C., Sommerlad, A., Lyketsos, C. G. & Livingston, G. Modifiable predictors of dementia in mild cognitive impairment: A systematic review and meta-analysis. Am. J. Psychiatry 172, 323–334 (2015).
Mauri, M., Sinforiani, E., Zucchella, C., Cuzzoni, M. G. & Bono, G. Progression to dementia in a population with amnestic mild cognitive impairment: Clinical variables associated with conversion. Funct. Neurol. 27, 49 (2012).
Artero, S. et al. Risk profiles for mild cognitive impairment and progression to dementia are gender specific. J. Neurol. Neurosurg. Psychiatry 79, 979–984 (2008).
Viticchi, G. et al. Framingham risk score and the risk of progression from mild cognitive impairment to dementia. J. Alzheimers Dis. 59, 67–75 (2017).
Xue, H. et al. Risk factors of transition from mild cognitive impairment to Alzheimer’s disease and death: a cohort study. Compr. Psychiatry 78, 91–97 (2017).
Ng, T. P. et al. Metabolic syndrome and the risk of mild cognitive impairment and progression to dementia: follow-up of the Singapore longitudinal ageing study cohort. JAMA Neurol. 73, 456–463 (2016).
Koch, M. et al. Alcohol consumption and risk of dementia and cognitive decline among older adults with or without mild cognitive impairment. JAMA Netw. Open 2, e1910319–e1910319 (2019).
Solfrizzi, V. et al. Alcohol consumption, mild cognitive impairment, and progression to dementia. Neurology 68, 1790–1799 (2007).
Mehta, K. M. & Yeo, G. W. Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimers Dement. 13, 72–83 (2017).
Nianogo, R. A. et al. Risk factors associated with Alzheimer disease and related dementias by sex and race and ethnicity in the US. JAMA Neurol. 79, 584–591 (2022).
Kang, S. H. et al. Different effects of cardiometabolic syndrome on brain age in relation to gender and ethnicity. Alzheimer’s Res. Ther. 15, 68. https://doi.org/10.1186/s13195-023-01215-8 (2023).
McKeigue, P. M., Miller, G. J. & Marmot, M. G. Coronary heart disease in south Asians overseas: A review. J. Clin. Epidemiol. 42, 597–609. https://doi.org/10.1016/0895-4356(89)90002-4 (1989).
Eastwood, S. V., Tillin, T., Chaturvedi, N. & Hughes, A. D. Ethnic differences in associations between blood pressure and stroke in South Asian and European men. Hypertension (Dallas, Tex: 1979) 66, 481–488. https://doi.org/10.1161/hypertensionaha.115.05672 (2015).
Park, J. E. et al. Decline in the incidence of all-cause and Alzheimer’s disease dementia: A 12-year-later rural cohort study in Korea. J. Korean Med. Sci. 34, e293. https://doi.org/10.3346/jkms.2019.34.e293 (2019).
Niu, H., Álvarez-Álvarez, I., Guillén-Grima, F. & Aguinaga-Ontoso, I. Prevalence and incidence of Alzheimer’s disease in Europe: A meta-analysis. Neurologia (Barcelona, Spain) 32, 523–532. https://doi.org/10.1016/j.nrl.2016.02.016 (2017).
Wild, S. H., Fischbacher, C., Brock, A., Griffiths, C. & Bhopal, R. Mortality from all causes and circulatory disease by country of birth in England and Wales 2001–2003. J. Public Health (Oxf.) 29, 191–198. https://doi.org/10.1093/pubmed/fdm010 (2007).
Fernandez-Sola, J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat. Rev. Cardiol. 12, 576–587 (2015).
Nichols, E. et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 88–106 (2019).
Wahl, D. et al. Aging, lifestyle and dementia. Neurobiol. Dis. 130, 104481 (2019).
van der Flier, W. M. & Scheltens, P. Epidemiology and risk factors of dementia. J. Neurol. Neurosurg. Psychiatry 76, v2–v7 (2005).
Miech, R. et al. Incidence of AD may decline in the early 90s for men, later for women: The Cache county study. Neurology 58, 209–218 (2002).
Ott, A., Breteler, M. M., Harskamp, F. V., Stijnen, T. & Hofman, A. Incidence and risk of dementia: The Rotterdam study. Am. J. Epidemiol. 147, 574–580 (1998).
Roberts, R. et al. The incidence of MCI differs by subtype and is higher in men: The Mayo clinic study of aging. Neurology 78, 342–351 (2012).
Buckley, R. F. et al. Sex differences in the association of global amyloid and regional tau deposition measured by positron emission tomography in clinically normal older adults. JAMA Neurol. 76, 542–551 (2019).
Sundermann, E. E. et al. Better verbal memory in women than men in MCI despite similar levels of hippocampal atrophy. Neurology 86, 1368–1376. https://doi.org/10.1212/wnl.0000000000002570 (2016).
Digma, L. A. et al. Women can bear a bigger burden: ante- and post-mortem evidence for reserve in the face of tau. Brain communications 2, fcaa025. https://doi.org/10.1093/braincomms/fcaa025 (2020).
Koran, M. E. I., Wagener, M. & Hohman, T. J. Sex differences in the association between AD biomarkers and cognitive decline. Brain Imaging Behav. 11, 205–213. https://doi.org/10.1007/s11682-016-9523-8 (2017).
Altmann, A., Tian, L., Henderson, V. W. & Greicius, M. D. Sex modifies the APOE-related risk of developing Alzheimer disease. Ann. Neurol. 75, 563–573. https://doi.org/10.1002/ana.24135 (2014).
Kim, H. et al. Association between body mass index and cortical thickness: among elderly cognitively normal men and women. Int. Psychogeriatr. 27, 121–130. https://doi.org/10.1017/s1041610214001744 (2015).
Tolppanen, A. M. et al. Midlife and late-life body mass index and late-life dementia: Results from a prospective population-based cohort. J. Alzheimer’s Dis. JAD 38, 201–209. https://doi.org/10.3233/jad-130698 (2014).
Bell, S. P. et al. Late-Life body mass index, rapid weight loss, apolipoprotein E ε4 and the risk of cognitive decline and incident dementia. J. Nutr. Health Aging 21, 1259–1267. https://doi.org/10.1007/s12603-017-0906-3 (2017).
Kang, S. H. et al. Independent effect of body mass index variation on amyloid-β positivity. Front. Aging Neurosci. 14, 924550. https://doi.org/10.3389/fnagi.2022.924550 (2022).
Jang, H. et al. Association of glycemic variability with imaging markers of vascular burden, β-amyloid, brain atrophy, and cognitive impairment. Neurology 102, e207806. https://doi.org/10.1212/wnl.0000000000207806 (2024).
Ekblad, L. L. et al. Midlife insulin resistance, APOE genotype, and late-life brain amyloid accumulation. Neurology 90, e1150–e1157. https://doi.org/10.1212/wnl.0000000000005214 (2018).
Wolters, F. J. et al. Coronary heart disease, heart failure, and the risk of dementia: A systematic review and meta-analysis. Alzheimers Dement. 14, 1493–1504 (2018).
Beeri, M. S. et al. Coronary artery disease is associated with Alzheimer disease neuropathology in APOE4 carriers. Neurology 66, 1399–1404 (2006).
Waziry, R., Chibnik, L. B., Bos, D., Ikram, M. K. & Hofman, A. Risk of hemorrhagic and ischemic stroke in patients with Alzheimer disease: A synthesis of the literature. Neurology 94, 265–272 (2020).
Walker, K. A., Power, M. C. & Gottesman, R. F. Defining the relationship between hypertension, cognitive decline, and dementia: A review. Curr. Hypertens. Rep. 19, 1–16 (2017).
Hoffman, L. et al. Less Alzheimer disease neuropathology in medicated hypertensive than nonhypertensive persons. Neurology 72, 1720–1726 (2009).
Corraini, P. et al. Long-term risk of dementia among survivors of ischemic or hemorrhagic stroke. Stroke 48, 180–186 (2017).
Koton, S. et al. Association of ischemic stroke incidence, severity, and recurrence with dementia in the atherosclerosis risk in communities cohort study. JAMA Neurol. 79, 271–280 (2022).
Honig, L. S. et al. Stroke and the risk of Alzheimer disease. Arch. Neurol. 60, 1707–1712 (2003).
Waziry, R., Claus, J. J. & Hofman, A. Dementia risk following ischemic stroke: a systematic review and meta-analysis of factors collected at time of stroke diagnosis. J. Alzheimers Dis. 90, 1535–1546 (2022).
Williams, D. M., Finan, C., Schmidt, A. F., Burgess, S. & Hingorani, A. D. Lipid lowering and Alzheimer disease risk: A Mendelian randomization study. Ann. Neurol. 87, 30–39 (2020).
Cheng, Y.-W. et al. The contribution of vascular risk factors in neurodegenerative disorders: From mild cognitive impairment to Alzheimer’s disease. Alzheimer’s Res. Ther. 12, 1–10 (2020).
Larsson, S. C. & Markus, H. S. Does treating vascular risk factors prevent dementia and Alzheimer’s disease? A systematic review and meta-analysis. J. Alzheimers Dis. 64, 657–668 (2018).
Santos-Lozano, A. et al. in Mayo Clinic Proceedings. 999–1020 (Elsevier).
Scarmeas, N. et al. Physical activity, diet, and risk of Alzheimer disease. JAMA 302, 627–637 (2009).
Beckett, M. W., Ardern, C. I. & Rotondi, M. A. A meta-analysis of prospective studies on the role of physical activity and the prevention of Alzheimer’s disease in older adults. BMC Geriatr. 15, 1–7 (2015).
Ownby, R. L., Crocco, E., Acevedo, A., John, V. & Loewenstein, D. Depression and risk for Alzheimer disease: Systematic review, meta-analysis, and metaregression analysis. Arch. Gen. Psychiatry 63, 530–538 (2006).
Green, R. C. et al. Depression as a risk factor for Alzheimer disease: The MIRAGE study. Arch. Neurol. 60, 753–759 (2003).
Jeon, K. H. et al. Changes in alcohol consumption and risk of dementia in a nationwide cohort in South Korea. JAMA Netw. Open 6, e2254771–e2254771 (2023).
Xu, G. et al. Alcohol consumption and transition of mild cognitive impairment to dementia. Psychiatry Clin. Neurosci. 63, 43–49 (2009).
Zhao, Y.-L. et al. Environmental factors and risks of cognitive impairment and dementia: A systematic review and meta-analysis. Ageing Res. Rev. 72, 101504 (2021).
Rahman, M., White, E. M., Mills, C., Thomas, K. S. & Jutkowitz, E. Rural-urban differences in diagnostic incidence and prevalence of Alzheimer’s disease and related dementias. Alzheimers Dement. 17, 1213–1230 (2021).
Liu, C.-C. et al. Rural-urban disparities in the prevalence of mild cognitive impairment and dementia in Taiwan: A door-to-door nationwide study. J. Epidemiol. 32, 502–509 (2022).
Rusmaully, J. et al. Contribution of cognitive performance and cognitive decline to associations between socioeconomic factors and dementia: A cohort study. PLoS Med. 14, e1002334 (2017).
Wang, A.-Y. et al. Socioeconomic status and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 39 prospective studies. J. Prev. Alzheimer’s Dis. 10, 83–94 (2023).
Petersen, J. D. et al. Association of socioeconomic status with dementia diagnosis among older adults in Denmark. JAMA Netw. Open 4, e2110432–e2110432 (2021).
Funding
This research was supported by the Korea University Guro Hospital (KOREA RESEARCH-DRIVEN HOSPITAL) and grant funded by Korea University Medicine (K2512601), the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIT) (RS-2025-16066879), and Basic Science Research Program through the National Research Foundation of Korea(NRF) funded by the Ministry of Education(RS-2023-00245506).
Author information
Authors and Affiliations
Contributions
KB, MK, and SHK conceptualized the project and drafted the manuscript. MK and SHK developed the methodology. KB and MK analyzed the data. YJP, SJC, and KO reviewed and edited the manuscript. KO, SBK, and SHK supervised the project. All authors discussed the results, contributed to the final version, and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was reviewed and approved by the Institutional Review Board of Korea University Guro Hospital, and the need for informed consent was waived due to the retrospective design of the study. All procedures performed in human studies were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Baik, K., Kang, M., Park, Y.J. et al. Twelve-year nationwide cohort study identifying risk factors for conversion from mild cognitive impairment to Alzheimer’s disease. Sci Rep 15, 35418 (2025). https://doi.org/10.1038/s41598-025-16620-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16620-2