Abstract
Ceramic materials have gained prominence as advanced alternatives to metals and polymers in total hip prosthesis, owing to their superior wear resistance, chemical inertness, and minimal ion release. Among ceramic biomaterials, aluminum oxide (Al2O2) is particularly favored for its exceptional hardness, high compressive strength, and excellent tribological performance, outperforming other candidates such as zirconium dioxide (ZrO₂) and silicon nitride (Si2N4). However, the inherently brittle nature of ceramics necessitates careful stress analysis to mitigate fracture risks in ceramic-on-ceramic bearing systems. This study investigates the influence of radial clearance as a key geometric parameter on the mechanical safety of Al2O2-on-Al2O3 bearings by analyzing Tresca stress distributions under physiologically representative loading conditions. A 2D axisymmetric finite element model was developed to simulate the internal stress behavior of the bearing components during a full gait cycle. Six radial clearance values, ranging from 0.03 to 0.3 mm, were systematically evaluated to determine their effect on internal shear stress patterns. The simulation results demonstrate that a radial clearance of 0.03 mm yields the lowest Tresca stress, indicating a more favorable stress distribution and reduced risk of shear-induced fracture. Conversely, larger clearances were associated with elevated shear stresses, which could compromise the mechanical integrity of the ceramic components over time. These findings highlight the importance of precise control over radial clearance during the design and manufacturing of ceramic-on-ceramic hip implants. The study provides foundational insights for optimizing implant geometry to enhance the structural reliability and clinical longevity of ceramic-bearing total hip prostheses.
Similar content being viewed by others
Introduction
Total hip prosthesis remains one of the most effective orthopedic solutions for restoring mobility1 and alleviating pain2 in patients with degenerative3, traumatic4, or congenital5 hip joint conditions. The total hip prosthesis helps millions of patients around the world regain functional independence and enhance their quality of life by substituting biomechanical parts such as the femoral stem, femoral head, acetabular cup, and acetabular shell for the natural hip joint6. The mechanical articulation between the femoral head and the acetabular cup functions as the central bearing interface, accommodating complex joint motion7 and withstanding substantial biomechanical loads8 during routine activities. Achieving long-term prosthesis durability and reducing the risk of revision surgery necessitates the use of optimal materials and structural designs capable of enduring physiological stress over extended periods.
The tribological and mechanical performance of total hip prosthesis components is critically dependent on the biomaterials used. Traditional bearing surfaces have employed polymers9, metals10, and more recently, advanced ceramics11. While polymers offer low friction12 and good biocompatibility13, they tend to produce wear debris that can trigger osteolysis14, chronic inflammation15, and eventual implant loosening16, leading to revision surgeries17. Metals, though mechanically robust18 and widely used19, but can corrode over time20 and release metallic ions into surrounding tissues21, potentially causing metallosis22 and systemic toxicity23. In contrast, ceramic materials particularly aluminum oxide (Al2O2), zirconium dioxide (ZrO₂), and silicon nitride (Si2N4) exhibit superior wear resistance24, excellent biocompatibility25, and high corrosion resistance26. Among these, Al2O2 stands out as a preferred material for ceramic-on-ceramic bearings due to its exceptional hardness27, high compressive strength28, chemical inertness29, and outstanding scratch resistance30 under high contact stress conditions. Its low coefficient of friction31 and minimal wear generation32 further enhance its clinical appeal by reducing the risk of osteolysis. Compared toZrO2, which may undergo phase transformation under stress33, and Si2N4, which presents challenges in fabrication34 and long-term in vivo and in vitro validation35, Al2O2 offers a well-documented history of clinical success36 and material stability37.
A critical design parameter influencing the functional performance of ceramic-on-ceramic bearings in total hip prosthesis is radial clearance, which defined as the intentional gap between the femoral head and the acetabular cup illustrated in Fig. 1. This clearance significantly affects contact mechanics by altering the distribution and peak values of contact pressure38, which in turn influence wear behavior39, lubrication regimes40, and localized stress patterns41 at the articulating surfaces. Alongside radial clearance, other geometric parameters such as femoral head diameter and acetabular cup thickness also play key roles in defining the load-bearing capacity and mechanical response of the joint. Larger femoral head diameters are generally associated with improved joint stability42 and a reduced risk of dislocation43, but may introduce greater frictional torque44 and altered stress paths45. Conversely, acetabular cup thickness contributes to structural integrity46 and resistance to fracture47, particularly under cyclic loading. However, among these parameters, radial clearance remains especially critical in ceramic-on-ceramic systems where wear is minimal and fracture becomes the dominant failure mode due to the brittle nature of ceramic materials like Al2O2. Both excessive and insufficient clearances can lead to unfavorable outcomes ranging from micromotion48, edge loading49, and instability50 to increased stress concentrations that may precipitate crack initiation51. Therefore, precise optimization of radial clearance is essential for achieving biomechanically favorable conditions that minimize the risk of catastrophic failure and enhance the long-term performance of ceramic hip implants.
Illustration of radial clearance parameter on the bearing of total hip prosthesis (with part of the figure has been adapted from Hansen137. The figure was drawn by the authors using Microsoft Visio Professional 2019 (Microsoft Corporation, https://www.microsoft.com).
In the context of total hip prosthesis biomechanics, stress analysis is essential for evaluating implant safety, understanding failure mechanisms, and guiding design optimization. Classical failure theories based on yield criteria are commonly employed to assess the mechanical integrity of prosthetic components under physiological loading. Among these, von Mises stress is widely utilized due to its applicability to isotropic materials under complex stress states, and has been adopted in numerous hip prosthesis studies, including those by Ismail et al.52, Göktaş et al.53, and Chethan et al.54. In contrast, the Tresca criterion, which is based on maximum shear stress offers a more conservative assessment by defining a smaller allowable stress zone55, making it particularly valuable in safety–critical applications. Although its use in total hip prosthesis research has been relatively limited, Tresca stress has been effectively applied in other medical implant-related investigations, as reported by Moser et al.56, Mabrouk et al.57, and Farroukh et al.58. While Tresca stress is traditionally associated with ductile materials59,60,61, its application in the analysis of ceramic components is justified when used for comparative stress evaluation. This is especially relevant for Al2O2 as commonly used ceramic in hip bearings, which possesses high compressive strength62, but comparatively low shear resistance63. Mapping regions of elevated shear stress through Tresca analysis can provide valuable insight into areas prone to crack initiation, thereby contributing to the early identification of mechanical risk in brittle ceramic components and informing safer prosthesis design.
Advancements in computational modeling have significantly transformed the way complex engineering and biomedical problems are investigated. Among the various numerical techniques, finite element analysis has emerged as a powerful and widely utilized method for assessing the mechanical behavior of structures under various loading64, material65, and geometry66 conditions. Its ability to replicate conditions that are difficult or impractical to reproduce experimentally makes it particularly valuable for evaluating design alternatives67, identifying critical stress concentrations68, and predicting mechanical failure modes69. In the field of orthopedic implant research, especially total hip prosthesis, finite element analysis has been extensively used to analyze the mechanical performance of bearing components under physiological loads. While 3D models offer detailed representations of joint anatomy, triaxial motion, and complex contact behavior as done by Hidayat et al.70, Wibowo et al.71, and Alpkaya and Mihcin72, they require significant computational resources and time. To address this challenge, many studies have employed 2D axisymmetric models that simplify the ball-in-socket geometry of total hip prostheses performed by Saputra et al.73, Jamari et al.74, and Lestari et al.75. This approach enables efficient simulation of symmetric loading conditions, such as those encountered during normal gait, while maintaining accuracy in stress evaluation.
This study aims to investigate the influence of radial clearance on Tresca stress distribution in Al2O2-on-Al2O3 bearings used in total hip prosthesis, where is a continuation of our previous work investigating various ceramic materials for ceramic-on-ceramic bearing that can be found on Ammarullah et al.76. Using a 2D axisymmetric finite element model, the authors simulate the mechanical behavior of the bearing system under a physiologically representative walking cycle comprising 32 load phases. Six radial clearance values (0.03 mm, 0.05 mm, 0.075 mm, 0.1 mm, 0.15 mm, and 0.3 mm) are examined to identify the configuration that minimizes maximum Tresca stress and thereby reduces the risk of fracture. The outcomes of this work provide critical insights into stress-based performance optimization for Al2O2-on-Al2O3 hip bearings and contribute toward the development of safer, more reliable implant designs.
Materials and methods
Geometry parameters
The geometric configuration used in this study was based on widely adopted design standards bearings in total hip prosthesis, as reported in Ramadhoni et al.77. These parameters were selected to ensure relevance to clinically used implant designs and to facilitate comparison with existing literature78. The baseline model consists of a femoral head with a radius of 14 mm articulating against an acetabular cup with a wall thickness of 5 mm. To investigate the effect of radial clearance on mechanical safety from the perspective of Tresca stress distribution, six clearance values were adopted from Shankar and Nithyaprakash79 were examined: 0.03 mm, 0.05 mm, 0.075 mm, 0.1 mm, 0.15 mm, and 0.3 mm, as summarized in Table 1.
The implementation of these clearances in the finite element model was carried out by systematically modifying the internal radius of the acetabular cup, while keeping the femoral head radius constant at 14 mm for all cases. This approach allowed for precise control over the radial clearance without altering the overall geometry or dimensions of the femoral component. Furthermore, the outer diameter of the acetabular cup was adjusted accordingly to maintain a constant cup thickness of 5 mm across all simulations. This ensured structural consistency and comparability among the models, allowing the observed stress variations to be attributed solely to differences in radial clearance.
Material properties
In this study, the mechanical behavior of Al2O2 used in the ceramic-on-ceramic bearing components was modeled under the assumptions of homogeneous, isotropic, and linear elastic referred from Gutmann et al.80. A Young’s modulus and a Poisson’s ratio were applied for Al2O2 acetabular cup and femoral head taken from Shankar et al.81. These parameters reflect the material’s ability to resist elastic deformation under compressive loads, which is critical in load-bearing applications such as total hip prostheses. The constant coefficient of friction between the articulating surfaces Al2O2 femoral head and Al2O2 acetabular cup adopted from Uddin and Zhang82. Detailed computational simulation input for modelling materials behaviour presented in Table 2.
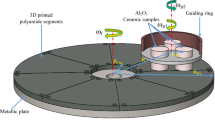
Finite element simulation of Al2O3-on-Al2O3bearing
The finite element analysis conducted in this study focused exclusively on the articulation between the Al2O2 femoral head and Al2O2 acetabular cup, which together form the core load-bearing interface in total hip prostheses. To achieve computational tractability while preserving geometrical relevance, a 2D axisymmetric model was developed based on a ball-in-socket configuration, simplifying the inherently 3D joint into a rotationally symmetric quarter-circle geometry presented in Fig. 2. This modeling approach has been validated in prior studies and is particularly suitable for symmetric loading conditions such as those reported from the previous study76.
Finite element model of Al2O2-on-Al2O3 bearing with varying radial clearance(with part of the figure has been adapted from Hansen137). The figure was drawn by the authors using Microsoft Visio Professional 2019 (Microsoft Corporation, https://www.microsoft.com).
Simulations were performed using ABAQUS CAE 6.14-1 (Dassault Systèmes, Vélizy-Villacoublay, France) employing a static loading scheme with implicit solver routines83. The contact between the femoral head and acetabular cup was modeled under dry conditions, reflecting the low-lubrication behavior of ceramic-on-ceramic interfaces84. Contact modeling was defined through surface-to-surface interactions using a master–slave algorithm, with the acetabular cup designated as the master surface85. An adiabatic contact process was assumed to capture time-independent interaction behavior, adopting Alpkaya and Mihçin86. Regarding boundary conditions, the outer surface of the acetabular cup was fully constrained in all directions to replicate its fixation within the pelvic bone as referred from Alpkaya et al.87. The femoral head was subjected to an axial compressive load applied at the lower edge of the axisymmetric boundary to represent gait-induced forces during normal walking. Lateral displacements were restricted, allowing only vertical translation to simulate physiological load transfer through the femoral stem88.
A detailed mesh convergence study (see Section "Mesh convergence study") was conducted to ensure numerical stability and solution accuracy. The final mesh configuration consisted of approximately 5500 four-node axisymmetric elements (CAX4) that have been used in several previous study from Močilnik et al.89, Esmaeili and Rizvi90, and Han et al.91, with 2000 elements assigned to the femoral head and 3500 elements to the acetabular cup. Mesh density was refined at the articulating surfaces to improve the resolution of contact stresses and ensure convergence of peak stress values across all simulated conditions.
Mesh convergence procedure
To ensure the reliability and accuracy of the finite element simulations, a mesh convergence study was conducted using the h-refinement technique, as described by Ramlee et al.92. This method involves systematically increasing the number of elements in the model to evaluate how solution outputs, specifically Tresca stress that stabilize with finer discretization. The convergence study was performed on the Al2O2-on-Al2O3 bearing model configured with a radial clearance of 0.3 mm, selected to represent a worst-case scenario in terms of potential stress amplification. Across all models, boundary conditions, loading (derived from the peak stance phase of the gait cycle), material definitions, and contact properties were kept constant to isolate the influence of mesh density on the computed stress field.
Six levels of mesh density were applied, ranging from an initial coarse mesh of 13 total elements to an ultra-refined mesh of 550,000 elements. Element refinement was performed independently in the femoral head and acetabular cup, with additional emphasis on the contact interface, where high stress gradients are expected. The purpose of this procedure was to determine the minimum mesh density required to achieve convergence without incurring excessive computational cost.
Human gait cycle
To simulate physiologically relevant loading conditions representative of daily activities, this study incorporated a quasi-static loading profile based on the human gait cycle referred from Saputra et al.93. Normal walking is the most frequent and clinically relevant activity performed by patients following total hip replacement surgery94, and thus serves as a valuable framework for evaluating stress behavior in implant components95. The loading data were adapted from Shankar et al.96, who modelled the hip joint forces during a complete gait cycle. The cycle was discretized into 32 load phases, capturing the full range of biomechanical loading experienced throughout a single step, which is a common values that can be found in an established study by Yu and Zhang97, Nithyaprakash et al.98, and Liu et al.99. The cycle is conventionally divided into two primary phases: the stance phase, comprising 60% of the cycle, during which the limb bears weight; and the swing phase, accounting for the remaining 40%, when the limb is in motion without ground contact100. The peak loading phase occurs at the 7th phase, where the hip joint is subjected to a maximum force of 2326.09 N, corresponding to approximately 3.5 times the body weight of an average adult.
Due to the geometric constraints of the 2D axisymmetric ball-in-socket model, dynamic joint kinematics such as rotation, flexion–extension, and femoral offset were not incorporated in this study. Instead, the analysis focused exclusively on axial loading conditions, which dominate during mid-stance and allow for meaningful stress evaluations under symmetric and repeatable load application. This modeling decision enables clear isolation of radial clearance effects on internal stress behavior without the added variability of joint orientation. The applied gait cycle used in the simulation is presented in Fig. 3, illustrating the temporal distribution and magnitude of joint reaction forces throughout the cycle.
Gait cycle loading profile adapted from Shankar et al.96 (with part of the figure has been adapted from Hansen137). The figure was drawn by the authors using Microsoft Visio Professional 2019 (Microsoft Corporation, https://www.microsoft.com).
Results and discussion
Mesh convergence study
The results of the mesh convergence analysis demonstrated that mesh density had a significant influence on the calculated Tresca stress values up to a certain threshold. Beyond this point, further refinement resulted in only marginal changes. Among the six mesh configurations tested, a model with 5,500 CAX4 elements (comprising 3500 elements in the acetabular cup and 2000 elements in the femoral head) was identified as optimal. This configuration exhibited less than 2% variation in maximum Tresca stress compared to the densest model (550,000 elements), indicating satisfactory numerical convergence (see Fig. 4). This mesh resolution provided a balance between computational efficiency and accuracy, ensuring that subsequent stress evaluations were not significantly influenced by discretization artifacts. Therefore, all further simulations involving radial clearance variations were conducted using this validated mesh configuration.
Tresca stress investigation
This study examined Tresca stress distributions in Al2O2-on-Al2O3 hip bearings under physiological loading, with a specific focus on the influence of radial clearance throughout a complete gait cycle consisting of 32 phases. Tresca stress, based on maximum shear stress theory, offers a conservative measure of mechanical safety and is especially relevant for brittle ceramics such as Al2O2, which are more susceptible to failure under shear and tensile stresses than under compression.
As illustrated in Fig. 5a, Tresca stress varies across the gait cycle, with the 7th phase consistently corresponding to the peak stress for all configurations. This phase represents maximum joint loading during the mid-stance phase of normal walking, and the observed trend reinforces prior literature identifying this as the most mechanically demanding condition for hip implants. The stress values were further summarized in Fig. 5b, which reports the minimum, average, and maximum Tresca stress values for each radial clearance. A progressive increase in all three metrics was observed as clearance increased from 0.03 to 0.3 mm. The average Tresca stress rose from 45.42 MPa at 0.03 mm to 185.76 MPa at 0.3 mm, while the maximum stress spiked from 58.12 to 234.1 MPa, representing a fourfold increase. This trend can be attributed to reduced conformity between articulating surfaces at higher clearances, which concentrates contact loads into smaller areas, increasing localized shear stress101.
Figure 6 displays Tresca stress contours at phases 1, 7, and 32, showing that peak loading significantly increases both the magnitude and extent of the stress field. With increasing radial clearance, these contours expand inward into the acetabular cup, indicating a deeper penetration of stress into the bulk material. Importantly, the model’s axisymmetric and centrally loaded configuration prevented edge loading, a known driver of catastrophic stress localization in ceramic components102.
To explore deeper into the internal stress behavior, Tresca stress was evaluated along a radial line across the acetabular cup thickness at phase 7 as shown in Fig. 7. This analysis reveals a striking pattern: the maximum Tresca stress does not occur at the articulating surface, but instead within the subsurface layers of the cup, typically at 20–40% of the wall thickness from the surface. This pattern becomes more pronounced with increasing radial clearance. At 0.03 mm clearance, the stress profile shows a relatively gentle gradient, peaking modestly below the surface and decaying toward the outer radius. However, as the clearance increases, the profiles become more nonlinear and peaked, with larger stress gradients and deeper stress concentrations. For example, at 0.3 mm clearance, the Tresca stress remains elevated well into the bulk material, with localized maxima that could serve as critical zones for crack nucleation, especially under cyclic loading. This behavior reflects the mechanical interplay between contact pressure distribution and structural constraint within the cup. While the articulating surface absorbs initial loading, internal constraint forces redistribute the load inward, leading to hoop stresses103 and shear interactions104 within the mid-thickness zone. These zones are particularly vulnerable in ceramics, which lack plastic deformation mechanisms to blunt internal stress peaks105.
Comparison with previous studies
To contextualize and validate the findings of this study, a comparative analysis was conducted against key previous investigations involving ceramic-on-ceramic hip bearing systems. The results from Ammarullah et al.76 are particularly relevant, as their finite element analysis investigated the influence of ceramic material types, starting from Al2O2, Si2N4, and ZrO2 on Tresca stress values under similar loading and geometrical conditions, using a fixed radial clearance of 0.05 mm. Their study reported a maximum Tresca stress of 78.29 MPa for Al2O2-on-Al2O3, 68.92 MPa for Si2N4-on-Si2N4, and 56.97 MPa for ZrO2-on-ZrO2. Ammarullah et al.76 findings indicate that while all ceramic materials remained structurally safe, which is under respective yield strengths (580 MPa for Al2O2106, 950–1200 MPa for Si2N4107, and 1000–1200 MPa for ZrO2108) under simulated gait loading, Al2O2 exhibited relatively higher internal stress, attributable to its lower toughness and higher elastic modulus compared to the others.
The present study extends this understanding by systematically varying radial clearance while keeping the material (Al2O2) constant. Notably, the maximum Tresca stress of 78.29 MPa was replicated at a 0.05 mm clearance, closely matching the value reported by Ammarullah et al.76. This consistency validates the numerical modeling approach and affirms the reliability of Tresca stress as a conservative safety metric. However, by further expanding the analysis across radial clearances ranging from 0.03 to 0.3 mm, the current study reveals a significant increase in Tresca stress with increasing clearance, culminating in a maximum value of 234.1 MPa at 0.3 mm, which is nearly three times higher than at 0.05 mm. Conversely, reducing the clearance to 0.03 mm yielded a substantial decrease in stress to 58.12 MPa, suggesting an optimal clearance threshold for minimizing internal shear and tensile stress in ceramic bearings.
Complementary insights are drawn from the work of Shankar109, who investigated the effect of radial clearance on contact pressure presented in Table 3. Their results similarly demonstrated that increasing radial clearance leads to a proportional rise in peak contact pressure from 72.53 MPa at 0.03 mm to 292.41 MPa at 0.3 mm. Although contact pressure and Tresca stress represent different mechanical metrics, the parallel trends reinforce the hypothesis that larger clearances exacerbate mechanical stresses at the articulating interface, reducing the conformity and distributing forces over smaller areas. Importantly, the correlation between Shankar’s peak contact pressure and the Tresca stress values obtained in this study explains a mechanistic linkage: higher contact pressures at the surface likely translate into more severe internal shear stresses.
Engineering and clinical discussion
The finite element analysis revealed that across all examined radial clearances, the computed Tresca stress values remained well below the static yield strength of Al2O2, reported at 580 MPa106. This finding confirms that, under modeled physiological gait loading, the Al2O2-on-Al2O3 bearing configurations are mechanically safe in terms of static structural integrity. The lowest maximum Tresca stress of 58.12 MPa occurred at a radial clearance of 0.03 mm, while the highest, 234.1 MPa, was observed at a clearance of 0.3 mm, which is still within the allowable material limits. These margins are reassuring from a short-term safety perspective, yet they highlight an important design consideration there are minimizing radial clearance not only reduces the magnitude of shear stress but also widens the safety margin against potential failure.
From an engineering standpoint, these results emphasize the critical role of manufacturing precision and dimensional control. Even minor deviations in radial clearance, whether due to fabrication tolerances110, thermal expansion during sterilization111, or wear-in effects112 can significantly alter the internal stress distribution. Higher clearances lead to increased contact pressures113, reduced conformity114, and elevated Tresca stress76, especially within the subsurface bulk of the acetabular cup. These stresses, though below the material’s yield limit, could initiate fatigue-driven damage over prolonged use115. Therefore, maintaining sub-millimeter tolerances, particularly within the range of 0.03–0.05 mm, is vital for ensuring long-term mechanical stability and mitigating fracture risk. Engineering teams involved in the production of ceramic bearings must therefore prioritize tight tolerance control, surface finish accuracy, and post-processing verification, potentially utilizing advanced inspection methods such as 3D metrology116 and laser scanning117.
From a clinical perspective, the findings provide valuable insights into the role of radial clearance as a modifiable factor in implant longevity. Although no stress exceeded Al2O2’s yield limit, the progressive increase in Tresca stress with clearance and its localization within the bulk material suggest a higher susceptibility to sub-surface damage in patients implanted with bearings manufactured at or beyond the upper range of allowable clearances. Such stress concentrations may not lead to immediate failure118, but under cyclic loading and in vivo microseparation events, they could contribute to long-term degradation119 or spontaneous fracture120. These concerns are particularly relevant for younger, more active patients, who exert higher mechanical demands on their implants121. Thus, the results advocate for stringent quality assurance in component production, pre-implantation verification of dimensional accuracy, and where feasible, personalized prosthesis selection based on patient-specific biomechanics. Additionally, they underline the need for continued post-market surveillance and longitudinal clinical studies that correlate radial clearance specifications with real-world implant performance and revision rates.
Study limitations and future directions
Despite offering valuable insights into the mechanical behavior of Al2O2-on-Al2O3 bearings, several limitations inherent to this study must be acknowledged to ensure appropriate interpretation and to guide future improvements. First and foremost, the absence of experimental validation limits the direct clinical applicability of the finite element simulation results. While numerical analyses provide powerful approximations of physical phenomena, validation through in vitro testing as conducted by Kotta et al.122 or comparison with in vivo data preformed by Hung and Wu123 is essential to confirm the accuracy and reliability of the model predictions.
Secondly, the coefficient of friction between the Al2O2 femoral head and acetabular cup was modeled as a constant value. In reality, this coefficient can vary significantly over time due to evolving surface roughness124, wear117, fluid-film lubrication effects125, and third-body particle interactions126. A time-dependent work, like Rebenda et al.127 would improve the predictive fidelity of future simulations.
Third, the study employed a 2D axisymmetric ball-in-socket model, which, while computationally efficient, does not fully capture the complex 3D motion and multi-axial loading experienced in real human hip joints. Important biomechanical phenomena such as edge loading128, femoral anteversion129, pelvic tilt130, and non-symmetric gait forces131 are not addressed in the current framework. Incorporating 3D geometries and physiological loading conditions in future work would yield more anatomically and biomechanically representative insights.
Fourth, although Tresca stress was selected in this study to provide a conservative estimate of mechanical safety due to its sensitivity to maximum shear stress and smaller yield surface, it may not be the most suitable criterion for predicting brittle failure in ceramic materials. Al2O2 ceramics primarily fail under tensile loading rather than shear, making maximum principal stress a more appropriate predictor. As shown by Moga et al.132 and Fischer-Cripps133, tensile-based criteria better reflect crack initiation behavior in brittle materials, where tensile strength is considerably lower than compressive or shear strength. Additionally, the current model omits the femoral stem taper, which in practice induces significant tensile and hoop stresses in the femoral head, particularly under microseparation and dynamic loading. Nevelos et al.134 demonstrated that these stresses are critical in the initiation and propagation of ceramic fractures. Excluding this anatomical feature may lead to an underestimation of localized tensile stress and fracture risk. Future models should incorporate the stem taper and adopt maximum principal stress analysis to improve failure prediction accuracy and clinical relevance.
In addition, the simulation assumes idealized boundary conditions by excluding the mechanical constraints and interactions associated with the pelvic bone and implant fixation. This simplification may underestimate stress transfer dynamics at the bone–implant interface, which are crucial for assessing implant longevity and bone remodeling behavior. As noted by Ali135, such assumptions limit the accuracy of load transmission and can mask potential risks like stress shielding or micromotion. Furthermore, the material properties of Al2O2 were modeled as homogeneous, isotropic, and linearly elastic. However, ceramics exhibit microstructural variability and are susceptible to damage accumulation, particularly under cyclic loading or subcritical stress. According to Wan136, using linear-elastic models can underpredict crack initiation and progression, while nonlinear or damage-based models better capture real-world fracture behavior. Future studies should incorporate both realistic anatomical constraints and advanced constitutive models to enhance the biomechanical relevance and clinical applicability of finite element simulations.
Conclusions
This study investigated the influence of radial clearance on Tresca stress distribution in Al2O2-on-Al2O3 hip prosthesis bearings using finite element analysis under physiologically relevant gait cycle loading. The results demonstrate that radial clearance plays a critical role in determining the internal stress distribution of ceramic bearings, with smaller clearances (0.03–0.05 mm) yielding significantly lower Tresca stress values. All simulated configurations produced maximum Tresca stress well below the yield strength of Al2O2 (580 MPa), affirming their mechanical safety under static loading conditions. However, higher radial clearances substantially increased the peak Tresca stress, potentially amplifying the risk of subsurface crack initiation due to the ceramic’s susceptibility to tensile and shear stresses. These findings highlight the importance of tight manufacturing tolerances and precise quality control in the production of ceramic hip implants. From an engineering perspective, optimizing radial clearance is essential for mechanical efficiency and ensuring long-term durability and reducing the likelihood of fatigue-induced failure. Clinically, this research highlights the relevance of component design and fit in minimizing internal stresses that could compromise implant longevity.
Data availability
All data generated or analyzed during this study are included in this published article. No additional datasets were generated or analyzed beyond the contents of the manuscript.
References
Vișan, R., Mihajlov, M., Luminița, M. A. & Baușic, A. I. G. Muscle deflection used as an assessment indicator of the rehabilitation quality after total hip joint arthroplasty (THA). J. Clin. Med. 14, 3728. https://doi.org/10.3390/jcm14113728 (2025).
Tian, Y. et al. The effect of pericapsular nerve group block and lateral femoral cutaneous nerve block on postoperative recovery after hip arthroplasty. Sci. Rep. 15, 19913. https://doi.org/10.1038/s41598-025-04699-6 (2025).
Tanaka, H. et al. High risk of postoperative complications in dialysis patients undergoing total hip arthroplasty: a database study of Japanese nationwide medical claims. Sci. Rep. 15, 24211. https://doi.org/10.1038/s41598-025-02829-8 (2025).
O’Driscoll, C. S. et al. Total hip arthroplasty in the setting of post-traumatic arthritis following acetabular fracture: A systematic review. Arthroplast. Today. 19, 101078. https://doi.org/10.1016/j.artd.2022.101078 (2023).
Zeroual, M.-A., Nassiri, M., El Kasseh, M., Achkoun, A. & Chafik, R. Outcomes of total hip arthroplasty for congenital hip dislocation: A retrospective study. Cureus. https://doi.org/10.7759/cureus.84797 (2025).
Drobniewski, M. et al. High risk of revision associated with the l-cup titanium alloy porous coated acetabular component in primary total hip arthroplasty: minimum follow-up of 14 years. J. Clin. Med. 14, 1301. https://doi.org/10.3390/jcm14041301 (2025).
Fukunaga, M. How to graphically represent the whole range of motion of a hip joint?. Lect. Notes Data Eng. Commun. Technol. 218, 28–34. https://doi.org/10.1007/978-3-031-71013-1_3 (2025).
Allcca, D., Nacarino, A., Sanchez, B., Castro, R., La-Rosa, A., Cornejo, J., Palomares, R., Vargas, M. Mechatronics bio-design of hip prosthesis using mechanic of materials analysis and finite element method: A proof of concept. In: 2024 5th International Conference on Recent Trends in Computer Science and Technology (2024). https://doi.org/10.1109/ICRTCST61793.2024.10578526.
Rasheed, M. E. H., Sweeney, J., Youseffi, M., Sefat, F. & Javid, S. A. Towards a standardised fatigue test for ultra high molecular weight polyethylene (UHMWPE) material used in total joint replacements (TJRs). J. Phys. Conf. Ser. 3027, 012084. https://doi.org/10.1088/1742-6596/3027/1/012084 (2025).
Liu, S. et al. Imaging and speciation of intracellular metallic implant debris using synchrotron-based X-ray fluorescence micro-spectroscopy: A study of two cases. Sci. Rep. 15, 12467. https://doi.org/10.1038/s41598-025-94231-7 (2025).
Stefan, C., Moldovan, C., Marsavina, L., Hurmuz, M. & Stefan, I. A case report on a fractured ceramic bearing surface following total hip replacement and a short review on the mechanisms of liner fracture. Reports. 7, 117. https://doi.org/10.3390/reports7040117 (2024).
Fouly, A. et al. Developing artificial intelligence models for predicting the tribo-mechanical properties of HDPE nanocomposite used in artificial hip joints. IEEE Access. 12, 14787–14799. https://doi.org/10.1109/ACCESS.2024.3352448 (2024).
Sathishkumar, S., Jawahar, P. & Chakraborti, P. Numerical Investigation of Polymer-based Biomaterials for Artificial Hip Joint with diverse boundary conditions. Recent Patents Eng. https://doi.org/10.2174/0118722121315250240822091850 (2025).
Efe, G. Ç., Yener, T., Zor, M. S., Türk, S. & Bİndal, C. Characterization of enhanced UHMWPE-Hap composites manufactured by hot pressing. Polym. Compos. https://doi.org/10.1002/pc.30116 (2025).
Hasegawa, M., Tone, S., Naito, Y. & Sudo, A. Ultra-high-molecular-weight polyethylene in hip and knee arthroplasties. Materials (Basel). 16, 2140. https://doi.org/10.3390/ma16062140 (2023).
Morano, C. et al. A comprehensive literature review of total hip arthroplasty (THA): Part 1—biomaterials. J. Funct. Biomater. 16, 179. https://doi.org/10.3390/jfb16050179 (2025).
Nikam, N. et al. Advancements in surface coatings for enhancing longevity in hip implants: A review. Prosthesis. 7, 21. https://doi.org/10.3390/prosthesis7010021 (2025).
Nappi, S., Gargale, L., Naccarata, F., Valentini, P. P. & Marrocco, G. A fractal-RFID based sensing tattoo for the early detection of cracks in implanted metal prostheses. IEEE J. Electromagn. RF Microwaves Med. Biol. 6, 29–40. https://doi.org/10.1109/JERM.2021.3108945 (2022).
Davis, T. P. Metal-on-metal hip arthroplasty: A comprehensive review of the current literature. Cureus. https://doi.org/10.7759/cureus.48238 (2023).
Ghadirinejad, K. et al. Fretting wear and corrosion-related risk factors in total hip replacement: A literature review on implant retrieval studies and national joint replacement registry reports. Prosthesis. 5, 774–791. https://doi.org/10.3390/prosthesis5030055 (2023).
Khandelwal, G., Roychoudhury, A., Bhutia, O. & Shariff, A. Longitudinal surveillance of serum titanium ion levels in patients with indigenous 3D printed total temporomandibular joint replacement. Sci. Rep. 13, 7275. https://doi.org/10.1038/s41598-023-33229-5 (2023).
Imada, A. O., Painter, B. M., Clinger, B. & Decker, M. M. A rare case of metallosis co-occurring with chronic prosthetic joint infection in total hip arthroplasty. Cureus https://doi.org/10.7759/cureus.21515 (2022).
Fan, W. & Guo, M. Research progress on nanotoxicity and detoxification of cobalt in metal-based implants. Ann. Med. https://doi.org/10.1080/07853890.2025.2532120 (2025).
Lee, A. C. et al. Nanopowder processing of ultrafine Si 3 N 4 with improved wear resistance. J. Asian Ceram. Soc. 3, 6–12. https://doi.org/10.1016/j.jascer.2014.09.004 (2015).
Priyadarshini, B., Rama, M., Chetan, & Vijayalakshmi, U. Bioactive coating as a surface modification technique for biocompatible metallic implants: a review. J. Asian Ceram. Soc. 7, 397–406. https://doi.org/10.1080/21870764.2019.1669861 (2019).
Hashim, A. A., Anaee, R. & Nasr, M. S. Improving the mechanical, corrosion resistance, microstructural and environmental performance of recycled aggregate concrete using ceramic waste powder as an alternative to cement. Ceramics. 8, 11. https://doi.org/10.3390/ceramics8010011 (2025).
Qizi, N. R. K. & Turabayevich, Y. A. The mechanical andthermal properties ofceramic materials. Am. J. Appl. Sci. Technol. 5, 98–101. https://doi.org/10.37547/ajast/Volume05Issue04-21 (2025).
Chandan, P. B. & Sankar, M. R. Extrusion-based additive manufacturing of alumina ceramics through controlled extrusion pressure. Int. J. Appl. Ceram. Technol. https://doi.org/10.1111/ijac.14935 (2025).
Žmak, I., Jozić, S., Ćurković, L. & Filetin, T. Alumina-based cutting tools—a review of recent progress. Materials (Basel). 18, 2813. https://doi.org/10.3390/ma18122813 (2025).
Jahanshahi, M., Mofidian, R., Hosseini, S. S. & Miansari, M. Investigation of mechanical properties of granular γ-alumina using experimental nano indentation and nano scratch tests. SN Appl. Sci. 5, 164. https://doi.org/10.1007/s42452-023-05388-7 (2023).
Kaushal, S., Saloni, Zeeshan, M., Imran Ansari, M. & Sharma, D. Progress in tribological research of Al2O3 ceramics: A review. Mater. Today Proc. 82, 163–167. https://doi.org/10.1016/j.matpr.2022.12.116 (2023).
Szymański, M., Przestacki, D. & Szymański, P. Tool wear and surface roughness in turning of metal matrix composite built of Al2O3 sinter saturated by aluminum alloy in vacuum condition. Materials (Basel). 15, 8375. https://doi.org/10.3390/ma15238375 (2022).
Gorelov, V. P., Belyakov, S. A. & Abdurakhimova, R. K. Phase transitions in monoclinic ZrO-=SUB=-2-=/SUB=-. Phys. Solid State. 65, 461. https://doi.org/10.21883/PSS.2023.03.55589.541 (2023).
Hummam, Z., Vahed, H. & Pourziad, A. Investigating the influence of material composition and design parameters on optical loss in hollow core fibers at 9.5 µm. Opt. Quantum Electron. 57, 174. https://doi.org/10.1007/s11082-025-08096-1 (2025).
Kong, X., Hu, X. & Chai, W. In vitro & in vivo investigation of the silicon nitride ceramic hip implant’s safety and effectiveness evaluation. J. Orthop. Surg. Res. 17, 87. https://doi.org/10.1186/s13018-021-02884-7 (2022).
Rahman, H. S. A. et al. In vivo and in vitro outcomes of alumina, zirconia and their composited ceramic-on-ceramic hip joints. J. Ceram. Soc. Japan. 121, 382–387. https://doi.org/10.2109/jcersj2.121.382 (2013).
Santavirta, S. et al. Alternative materials to improve total hip replacement tribology. Acta Orthop. Scand. 74, 380–388. https://doi.org/10.1080/00016470310017668 (2003).
Affatato, S., Merola, M. & Ruggiero, A. Development of a novel in silico model to investigate the influence of radial clearance on the acetabular cup contact pressure in hip implants. Materials (Basel). 11, 1–11. https://doi.org/10.3390/ma11081282 (2018).
Nikam, N., Shenoy, S., Keni, L. G., Shetty, S. & KN, C. Computational analysis of hip prosthesis: Impact of shape and material on mechanical performance. J. Appl. Eng. Sci. https://doi.org/10.5937/jaes0-55883 (2025).
Nitish Prasad, K. & Ramkumar, P. Effect of geometrical, operational and material parameters in the lubrication regime of hard-on-hard hip implants. Mater. Chem. Phys. 317, 129171. https://doi.org/10.1016/j.matchemphys.2024.129171 (2024).
Dantas, P. et al. Guimarães Consciência Hip joint contact pressure and force: a scoping review of in vivo and cadaver studies. Bone Joint Res. 12, 712–721. https://doi.org/10.1302/2046-3758.1212.BJR-2022-0461.R2 (2023).
Tigani, D., Banci, L., Valtorta, R. & Amendola, L. Hip stability parameters with dual mobility, modular dual mobility and fixed bearing in total hip arthroplasty: an analytical evaluation. BMC Musculoskelet. Disord. 23, 373. https://doi.org/10.1186/s12891-022-05280-2 (2022).
Kobayashi, S. et al. Factors associated with dislocation after total hip arthroplasties performed for nontraumatic osteonecrosis of the femoral head: a multicenter cohort study of 5,983 hips. Acta Orthop. https://doi.org/10.2340/17453674.2025.43473 (2025).
Clegg, B. A. et al. Effects of physiological loading from patient-derived activities of daily living on the wear of metal-on-polymer total hip replacements. Bioengineering 12, 663. https://doi.org/10.3390/bioengineering12060663 (2025).
Kluess, D., Martin, H., Mittelmeier, W., Schmitz, K.-P. & Bader, R. Influence of femoral head size on impingement, dislocation and stress distribution in total hip replacement. Med. Eng. Phys. 29, 465–471. https://doi.org/10.1016/j.medengphy.2006.07.001 (2007).
Ruhr, M., Baetz, J., Pueschel, K. & Morlock, M. M. Influence of acetabular cup thickness on seating and primary stability in total hip arthroplasty. J. Orthop. Res. 40, 2139–2146. https://doi.org/10.1002/jor.25232 (2022).
Solarino, G. et al. Outcomes of ceramic composite in total hip replacement bearings: A single-center series. J. Compos. Sci. 5, 320. https://doi.org/10.3390/jcs5120320 (2021).
Bologna, F. A., Putame, G., Audenino, A. L. & Terzini, M. Understanding the role of head size and neck length in micromotion generation at the taper junction in total hip arthroplasty. Sci. Rep. https://doi.org/10.1038/s41598-024-57017-x (2024).
Shankar, S., Nithyaprakash, R., Selvamani, K. A. & Kumar, R. N. Effect of radial clearance, ellipsoidal and corner radius on contact mechanics of metallic and ceramic implants under fixed micro-lateralization: A finite element analysis. Trends Biomater Artif. Organs. 35, 247–254 (2021).
Tiwari, M., Gupta, K. & Prakash, O. Effect of radial internal clearance of a ball bearing on the dynamics of a balanced horizontal rotor. J. Sound Vib. 238, 723–756. https://doi.org/10.1006/jsvi.1999.3109 (2000).
Choudhari, A. et al. Wear and friction mechanism study in knee and hip rehabilitation: A comprehensive review. Appl. Biotribology Biomed. Syst. https://doi.org/10.1007/978-3-031-58327-8_13 (2024).
Ismail, R. et al. Numerical study of salat movements for total hip replacement patient. Appl. Mech. Mater. 493, 426–431. https://doi.org/10.4028/www.scientific.net/AMM.493.426 (2014).
Göktaş, H. et al. Optimization of hip implant designs based on its mechanical behaviour. Lect. Notes Networks Syst. 328, 37–43. https://doi.org/10.1007/978-3-030-86297-8_4 (2022).
Chethan, K. N., Mohammad, Z., Shyamasunder Bhat, N. & Satish Shenoy, B. Optimized trapezoidal-shaped hip implant for total hip arthroplasty using finite element analysis. Cogent Eng. 7, 1–14. https://doi.org/10.1080/23311916.2020.1719575 (2020).
Budynas, R. G. & Nisbett, J. K. Shigley’s Mechanical Engineering Design, 10th editi (McGraw-Hill Education, 2015).
Moser, A.-C. et al. Freeze drying and Lugol staining of human menisci reveal circumferential fibre volumes to guide meniscus implant design and virtual simulation. Sci. Rep. 15, 22798. https://doi.org/10.1038/s41598-025-05004-1 (2025).
Mabrouk, M. S., Marzouk, S. Y. & Afify, H. M. A biomechanical analysis of prosthesis disc in lumbar spinal segment using three-dimensional finite element modelling. Int. J. Biomed. Eng. Technol. 39, 1. https://doi.org/10.1504/IJBET.2022.123256 (2022).
Farroukh, H., Kaddah, F. & Wehbe, T. Numerical investigation of the optimal porosity of titanium foam for dental implants. Heliyon. 10, e28063. https://doi.org/10.1016/j.heliyon.2024.e28063 (2024).
Li, W. & Jing, Y. A simple calibrated ductile fracture model and its application in failure analysis of steel connections. Buildings 12, 1358. https://doi.org/10.3390/buildings12091358 (2022).
Zhu, X.-K., Wiersma, B. Sindelar, R. Johnson, W.R. New strength theory and its application to determine burst pressure of thick-wall pressure vessels, In: Vol. 4B Mater. Fabr., (American Society of Mechanical Engineers, 2022). https://doi.org/10.1115/PVP2022-84902.
Moga, R.-A., Olteanu, C. D. & Delean, A. G. Investigating the ability of the tooth and surrounding support tissues to absorb and dissipate orthodontic loads during periodontal breakdown—finite elements analysis. Appl. Sci. 14, 1041. https://doi.org/10.3390/app14031041 (2024).
Chub-uppakarn, T. et al. Influence of partial substitution of metakaolin by palm oil fuel ash and alumina waste ash on compressive strength and microstructure in metakaolin-based geopolymer mortar. Case Stud. Constr. Mater. 19, e02519. https://doi.org/10.1016/j.cscm.2023.e02519 (2023).
Singh, G., Yu, Y., Ernst, F. & Raj, R. Shear strength and sliding at a metal–ceramic (aluminum–spinel) interface at ambient and elevated temperatures. Acta Mater. 55, 3049–3057. https://doi.org/10.1016/j.actamat.2007.01.008 (2007).
Saputra, E., Anwar, I. B., Jamari, J. & Van Der Heide, E. Finite element analysis of artificial hip joint movement during human activities. Procedia Eng. 68, 102–108. https://doi.org/10.1016/j.proeng.2013.12.154 (2013).
Gutmann, C. et al. Wear estimation of hip implants with varying chamfer geometry at the trunnion junction: a finite element analysis. Biomed. Phys. Eng. Express. 9, 035004. https://doi.org/10.1088/2057-1976/acb710 (2023).
Saputra, E., Anwar, I. B., Ismail, R., Jamari, J. & Van Der Heide, E. Study of unipolar and bipolar hip prostheses using finite element simulation: Contact stress analysis. Key Eng. Mater. 739, 96–102. https://doi.org/10.4028/www.scientific.net/KEM.739.96 (2017).
Akbar, I. et al. Analysis of the effect of tortuosity porous heatsink on force convection heat transfer. J. Adv. Res. Numer. Heat Transf. 16, 57–69. https://doi.org/10.37934/arnht.16.1.5769 (2024).
Basri, H. et al. The effect of tortuosity on wall shear stress of porous scaffold. CFD Lett. 15, 61–73. https://doi.org/10.37934/cfdl.15.7.6173 (2023).
Buechel, F. F. & Pappas, M. J. Failure modes. Princ. Hum. Jt. Replace. https://doi.org/10.1007/978-3-642-23011-0_2 (2011).
Hidayat, T. et al. Study of lubrication fluid pressure in artificial hip joint during bowing (Ruku’). Lect. Notes Mech. Eng. https://doi.org/10.1007/978-981-19-3179-6_56 (2022).
Wibowo, B. S., Wijaya, P. N., Tauviqirrahman, M., Ismail, R. & Muchammad, J. A 3-dimensional computational fluid-structure interaction analysis in the hip-joint prosthesis during solat (Prayer) activity. Jurnal Tribologi. 20, 125–141 (2019).
Alpkaya, A. T. & Mihcin, S. Sensitivity analysis of wear on metal-on-metal bearing couples via verification of numeric and analytic methods. Hittite J. Sci. Eng. 11, 57–67. https://doi.org/10.17350/HJSE19030000332 (2024).
Saputra, E., Anwar, I. B., Ismail, R., Jamari, J. & Van Der Heide, E. Finite element study of contact pressure distribution on inner and outer liner in the bipolar hip prosthesis. AIP Conf. Proc. 1725, 1–6. https://doi.org/10.1063/1.4945529 (2016).
Jamari, J., Lie, H. A., Saputra, E., Anwar, I. B. & Van Der Heide, E. The effect of additional layer between liner and PMMA on reducing cracks of cement mantle hip joints. Int. J. Eng. Technol. Innov. 8, 99–106. https://doi.org/10.1051/e3sconf/20187312013 (2018).
Lestari, W. D. et al. Investigation the effect of clearance and body weight on the contact pressure of metal on PCU hip prosthesis using finite element method. E3S Web Conf. 328, 07014. https://doi.org/10.1051/e3sconf/202132807014 (2021).
Ammarullah, M. I. et al. Minimizing risk of failure from ceramic-on-ceramic total hip prosthesis by selecting ceramic materials based on Tresca stress. Sustain. 14, 1–12. https://doi.org/10.3390/su142013413 (2022).
Ramadhoni, T. S. et al. The analysis of wear on artificial hip joint with dimple on femoral surface. J. Phys. Conf. Ser. 1500, 1–8. https://doi.org/10.1088/1742-6596/1500/1/012021 (2020).
Hidayat, T. et al. Short communication: Running-in behavior on single-mobility total hip arthroplasty Med. Eng. Phys. 104, 103806. https://doi.org/10.1016/j.medengphy.2022.103806 (2022).
Shankar, S. & Nithyaprakash, R. Effect of radial clearance on wear and contact pressure of hard-on-hard hip prostheses using finite element concepts. Tribol. Trans. 57, 814–820. https://doi.org/10.1080/10402004.2014.915072 (2014).
Corda, J. V., Chethan, K. N., Shetty, S., Shenoy, S. & Zuber, M. Finite element analysis of elliptical shaped stem profile of hip prosthesis using dynamic loading conditions. Biomed. Phys. Eng. Express. 9, 65028. https://doi.org/10.1088/2057-1976/acfe14 (2023).
Shankar, S. & Nithyaprakash, R. Predicting the wear of soft-on-hard bearing couples for human hip prosthesis using finite element concepts. J. Mech. Med. Biol. 16, 1–17. https://doi.org/10.1142/S0219519416500202 (2016).
Uddin, M. S. & Zhang, L. C. Predicting the wear of hard-on-hard hip joint prostheses. Wear 301, 192–200. https://doi.org/10.1016/j.wear.2013.01.009 (2013).
Dassault Systèmes, ABAQUS Analysis User’s Guide Volume IV: Elements, (2016).
Shankar, S., Nithyaprakash, R., Sugunesh, A. P. & Uddin, M. S. Long-term wear prediction of zirconia on alumina ceramic for hip prosthesis. Int. J. Surf. Sci. Eng. 14, 192–206. https://doi.org/10.1504/IJSURFSE.2020.110534 (2020).
Al-saffar, A. Modelling of Metal on Metal Hip Prostheses, Cardiff University, (2015). https://orca.cardiff.ac.uk/id/eprint/79514/.
Alpkaya, A. T. & Mihçin, Ş. The computational approach to predicting wear: Comparison of wear performance of CFR-PEEK and XLPE liners in total hip replacement. Tribol. Trans. 66, 59–72. https://doi.org/10.1080/10402004.2022.2140727 (2023).
Alpkaya, A. T., Yılmaz, M., Şahin, A. M. & Mihçin, D. Ş. Investigation of stair ascending and descending activities on the lifespan of hip implants. Med. Eng. Phys. 126, 104142. https://doi.org/10.1016/j.medengphy.2024.104142 (2024).
Jamari, J., Saputra, E., Anwar, I. B. & Van Der Heide, E. Study of an additional layer of cement mantle hip joints for reducing cracks. J. Funct. Biomater. 10, 1–8. https://doi.org/10.3390/jfb10030040 (2019).
Gubeljak, N., Predan, J. & Močilnik, V. Time dependent load capacity of the press fit. Teh. Glas. 19, 434–441. https://doi.org/10.31803/tg-20250115224222 (2025).
Esmaeili, H. & Rizvi, R. Indentation-driven machine learning approach for estimating rate-dependency in cohesive-frictional materials. Multifunct. Mater. Struct. https://doi.org/10.1117/12.3051536 (2025).
Han, G., Yoon, Y. & Lee, H. Evaluation of polymer viscoelasticity by integrated micro-indentation test with optical flow algorithm. Polym. Test. 145, 108750. https://doi.org/10.1016/j.polymertesting.2025.108750 (2025).
Ramlee, M. H., Zainudin, N. A. & Abdul Kadir, M. R. Finite element analysis of different pin diameter of external fixator in treating tibia fracture. Int. J. Integr. Eng. 13, 133–140. https://doi.org/10.30880/ijie.2021.13.04.012 (2021).
Saputra, E. et al. The effect of layer variation between liner and cement mantle on reducing cracks of PMMA material hip joints. E3S Web Conf. 73, 3–7. https://doi.org/10.1051/e3sconf/20187312013 (2018).
Bakry-Elmalik, A. Rehabilitation strategies of total hip replacement surgery. Clin. Orthop. Trauma Care. 6, 01–07. https://doi.org/10.31579/2694-0248/077 (2024).
Bounoua, N. et al. Three-Dimensional finite element analysis of cement-cup junction in total hip prosthesis: Mechanical stress distribution, crack initiation and rupture dynamics. NANO https://doi.org/10.1142/S1793292024500929 (2025).
Shankar, S., Siddarth, R., Nithyaprakash, R. & Uddin, M. S. Wear prediction of hard carbon coated hard-on-hard hip implants using finite element method. Int. J. Comput. Aided Eng. Technol. 10, 440–456. https://doi.org/10.1504/IJCAET.2018.092844 (2018).
Yu, Z. & Zhang, L. Design of low wear artificial hip joint considering 3D physiological loading and motion. Wear 523, 204744. https://doi.org/10.1016/j.wear.2023.204744 (2023).
Nithyaprakash, R., Shankar, S. & Uddin, M. S. Computational wear assessment of hard on hard hip implants subject to physically demanding tasks. Med. Biol. Eng. Comput. 56, 899–910. https://doi.org/10.1007/s11517-017-1739-2 (2018).
Liu, F., Leslie, I., Williams, S., Fisher, J. & Jin, Z. Development of computational wear simulation of metal-on-metal hip resurfacing replacements. J. Biomech. 41, 686–694. https://doi.org/10.1016/j.jbiomech.2007.09.020 (2008).
Asif, M. et al. Analysis of human gait cycle with body equilibrium based on leg orientation. IEEE Access. 10, 123177–123189. https://doi.org/10.1109/ACCESS.2022.3222859 (2022).
Johns-Rahnejat, P. M., Dolatabadi, N. & Rahnejat, H. Analytical elastostatic contact mechanics of highly-loaded contacts of varying conformity. Lubricants. 8, 89. https://doi.org/10.3390/lubricants8090089 (2020).
Shankar, S., Nithyaprakash, R., Sugunesh, A. P., Selvamani, K. A. & Uddin, M. S. Experimental and finite element wear study of silicon nitride against alumina for hip implants with bio-lubricant for various gait activities. SILICON https://doi.org/10.1007/s12633-020-00462-w (2020).
Anderson, I. A., Bowden, M. & Wyatt, T. P. Stress analysis of hemispherical ceramic hip prosthesis bearings. Med. Eng. Phys. 27, 115–122. https://doi.org/10.1016/j.medengphy.2004.09.018 (2005).
Rahaman, M. N., Yao, A., Bal, B. S., Garino, J. P. & Ries, M. D. Ceramics for prosthetic hip and knee joint replacement. J. Am. Ceram. Soc. 90, 1965–1988. https://doi.org/10.1111/j.1551-2916.2007.01725.x (2007).
Clayton, J. D. Modeling deformation and fracture of boron-based ceramics with nonuniform grain and phase boundaries and thermal-residual stress. Solids 3, 643–664. https://doi.org/10.3390/solids3040040 (2022).
Shankar, S., Prakash, L. & Kalayarasan, M. Finite element analysis of different contact bearing couples for human hip prosthesis. Int. J. Biomed. Eng. Technol. 11, 66–80. https://doi.org/10.1504/IJBET.2013.053712 (2013).
Shankar, S. et al. Effect of radial clearance, corner radius and micro-lateralization on contact stress of metallic and ceramic hip prosthesis—a finite element analysis. Def. Sci. J. 72, 441–449. https://doi.org/10.14429/dsj.72.1648310.14429/dsj.72.16483 (2022).
Bal, B. S. et al. Fabrication and Testing of Silicon Nitride Bearings in Total Hip Arthroplasty. Winner of the 2007 “HAP” PAUL Award. J. Arthroplasty. 24, 110–116. https://doi.org/10.1016/j.arth.2008.01.300 (2009).
Shankar, S. Predicting wear of ceramic–ceramic hip prosthesis using finite element method for different radial clearances, Tribol. - Mater. Surfaces. Interfaces 8, 194–200. https://doi.org/10.1179/1751584X14Y.0000000077 (2014).
Sriram, S. & Reddy, B. S. Analysis and develop a novel multi-piece-split-cavity mold for the fabrication of bipolar femoral head. Mater. Today Proc. 56, 1391–1398. https://doi.org/10.1016/j.matpr.2021.11.438 (2022).
Gu, J. Bearing surfaces for total hip arthroplasty. Princ. Prim. Total Hip Arthroplast. https://doi.org/10.1007/978-981-19-3606-7_4 (2022).
Merfort, R. et al. Head, acetabular liner composition, and rate of revision and wear in total hip arthroplasty: A Bayesian network meta-analysis. Sci. Rep. 13, 20327. https://doi.org/10.1038/s41598-023-47670-z (2023).
Czerniec, M. & Zubrzycki, J. Study of contact pressures in total hip replacement. Adv. Sci. Technol. Res. J. 15, 176–183. https://doi.org/10.12913/22998624/136178 (2021).
Li, J., Hua, X., Jin, Z., Fisher, J. & Wilcox, R. K. Influence of clearance on the time-dependent performance of the hip following hemiarthroplasty: A finite element study with biphasic acetabular cartilage properties. Med. Eng. Phys. 36, 1449–1454. https://doi.org/10.1016/j.medengphy.2014.05.014 (2014).
Guo, F., Cheng, G. & Yuan, X. Fatigue life and reliability analysis of a parallel hip joint simulator. Robotica 39, 2079–2093. https://doi.org/10.1017/S0263574721000151 (2021).
Zanini, F., Carmignato, S., Savio, E. & Affatato, S. Uncertainty determination for X-ray computed tomography wear assessment of polyethylene hip joint prostheses. Precis. Eng. 52, 477–483. https://doi.org/10.1016/j.precisioneng.2018.02.009 (2018).
Bennett, W. B. & Zou, M. Small laser-textured dimples for improved tribological performance of CoCrMo in artificial hip joints. Lubricants. 13, 158. https://doi.org/10.3390/lubricants13040158 (2025).
Corda, J. V., Chethan, K. N., Shenoy, S., Shetty, S. & Zuber, M. Fatigue life evaluation of different hip implant using finite element analysis. J. Appl. Eng. Sci. 21, 896–907. https://doi.org/10.5937/jaes0-44094 (2023).
Fernández-Fairén, M. et al. Early short-term postoperative mechanical failures of current ceramic-on-ceramic bearing total hip arthroplasties. Materials (Basel). 13, 5318. https://doi.org/10.3390/ma13235318 (2020).
Entezari, A., Roohani-Esfahani, S.-I., Zhang, Z., Zreiqat, H., Dunstan, C.R. & Li, Q. Fracture behaviors of ceramic tissue scaffolds for load bearing applications. Sci. Rep. 6, 28816. https://doi.org/10.1038/srep28816 (2016).
Wang, T., Sun, J.-Y., Zhao, X.-J., Liu, Y. & Yin, H. Ceramic-on-ceramic bearings total hip arthroplasty in young patients. Arthroplast. Today. 2, 205–209. https://doi.org/10.1016/j.artd.2016.04.004 (2016).
Kottan, N., Gowtham, N. H. & Basu, B. Development and validation of a finite element model of wear in UHMWPE liner using experimental data from hip simulator studies. J. Biomech. Eng. https://doi.org/10.1115/1.4052373 (2022).
Hung, J.-P. & Wu, J.S.-S. A comparative study on wear behavior of hip prosthesis by finite element simulation. Biomed. Eng. Appl. Basis Commun. 14, 139–148. https://doi.org/10.4015/S1016237202000218 (2002).
Nečas, D. et al. Frictional behaviour and surface topography evolution of DLC-coated biomedical alloys. Biosurface Biotribol. https://doi.org/10.1049/bsb2.70004 (2025).
Mittal, V. K. & Gupta, V. Dry and wet lubrication analysis for multi-material hip assembly. Int. J. Automot. Mech. Eng. 19, 9606–9622. https://doi.org/10.15282/ijame.19.1.2022.22.0741 (2022).
Kumar, G. B. V., Balasubramanya, H. S., Kumar, T. A., Pramod, R. & Aradhya, S. M. Tribological behavior of Co–Cr–Mo alloy on ultra high molecular polyethylene with and without third body particles used in hip implant application. Lect. Notes Mech. Eng. https://doi.org/10.1007/978-981-19-4606-6_10 (2023).
Rebenda, D., Odehnal, L., Uhrová, S., Nečas, D. & Vrbka, M. On the friction and lubrication of 3D Printed Ti6Al4V Hip joint replacement. Tribol. Lett. https://doi.org/10.1007/s11249-025-02002-2 (2025).
Elkins, J. M., Kruger, K. M., Pedersen, D. R., Callaghan, J. J. & Brown, T. D. Edge-loading severity as a function of cup lip radius in metal-on-metal total hips—a finite element analysis. J. Orthop. Res. 30, 169–177. https://doi.org/10.1002/jor.21524 (2012).
Heller, M. O. et al. Influence of femoral anteversion on proximal femoral loading: measurement and simulation in four patients. Clin. Biomech. 16, 644–649. https://doi.org/10.1016/S0268-0033(01)00053-5 (2001).
Hasegawa, K. et al. The influence of pelvic tilt on stress distribution in the acetabulum: Finite element analysis. BMC Musculoskelet. Disord. 22, 764. https://doi.org/10.1186/s12891-021-04500-5 (2021).
Wareńczak, A. & Lisiński, P. Does total hip replacement impact on postural stability?. BMC Musculoskelet. Disord. 20, 229. https://doi.org/10.1186/s12891-019-2598-9 (2019).
Moga, R. A., Olteanu, C. D., Daniel, B. M. & Buru, S. M. Finite elements analysis of tooth—a comparative analysis of multiple failure criteria. Int. J. Environ. Res. Public Health. 20, 4133. https://doi.org/10.3390/ijerph20054133 (2023).
Fischer-Cripps, A. C. A partitioned-problem approach to microstructural modelling of a glass-ceramic. MRS Proc. 578, 345. https://doi.org/10.1557/PROC-578-345 (1999).
Nevelos, J. et al. Microseparation of the centers of alumina-alumina artificial hip joints during simulator testing produces clinically relevant wear rates and patterns. J. Arthroplasty. 15, 793–795. https://doi.org/10.1054/arth.2000.8100 (2000).
Ali, M. Computational and theoretical contact modelling of hip implant devices with the application of wear simulations, University of Warwick, (2013). https://wrap.warwick.ac.uk/id/eprint/58399/.
Wan, B. Computational Modeling of Fracture Failure in Mineralized and Prosthetic Biomaterials, The University of Sydney, (2022). https://ses.library.usyd.edu.au/handle/2123/32069.
Hansen, E.. Total Hip Replacement for Hip Arthritis. Arthritis Heal. URL https://www.arthritis-health.com/surgery/hip-surgery/total-hip-replacement-hip-arthritis (2022).
Acknowledgements
The authors acknowledge the funded by World Class Research Universitas Diponegoro number 222-765/UN7.D2/PP/IV/2025.
Statement of originality
The authors declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere. The authors confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. The authors further confirm that the order of authors listed in the manuscript has been approved by all of us. The authors understand that the Corresponding Author is the sole contact for the Editorial process. The corresponding author is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
Funding
This research was funded by World Class Research Universitas Diponegoro number 222-765/UN7.D2/PP/IV/2025.
Author information
Authors and Affiliations
Contributions
Muhammad Imam Ammarullah: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, and Writing—original draft preparation. Abdulfatah Abdu Yusuf: Writing—review and editing and Project administration. Muhammad Kozin: Writing—review and editing and Project administration. Mohamad Izzur Maula: Writing—review and editing and Project administration. M. Danny Pratama Lamura: Writing—review and editing and Project administration. Hasyid Ahmad Wicaksono: Writing—review and editing and Project administration. Athanasius Priharyoto Bayuseno: Funding acquisition, Supervision, and Writing—review and editing. Jamari Jamari: Funding acquisition, Supervision, and Writing—review and editing. Muhammad Hanif Ramlee: Supervision and Writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study did not involve human participants or animals, and no ethical approval was required. All research procedures adhered to relevant ethical guidelines and best practices for non-human and non-animal research.
Informed consent
Not applicable.
Consent for publication
The authors consent for the publication of this manuscript.
Declaration of AI use
The authors declare the use of generative artificial intelligence (AI) and AI-assisted technologies in the preparation of this manuscript. Specifically, ChatGPT (version GPT-4, OpenAI) was used to improve the readability and language of the article. The AI tool was not used for data analysis, interpretation of results, or drawing scientific conclusions. All content has been reviewed and verified by the authors to ensure accuracy and integrity.
Transparency statement
The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ammarullah, M., Yusuf, A., Kozin, M. et al. Influence of radial clearance on Tresca stress in Al2O2-on-Al2O3 bearings for total hip prosthesis evaluated using finite element analysis. Sci Rep 15, 33091 (2025). https://doi.org/10.1038/s41598-025-16850-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16850-4