Abstract
Oral pathogens contribute to dental caries and other infections affecting oral health. To address concerns related to the adverse effects of chemical mouthwashes like chlorhexidine (CHX), this study introduces a novel herbal mouthwash formulated with green-synthesized zinc oxide nanoparticles (ZnONPs) infused with Cymbopogon citratus essential oil (CEO). Unlike traditional formulations, this herbal mouthwash aims to offer a safer, eco-friendly alternative. Four formulations (F1-F4) with varying concentrations of CEOZnONPs were evaluated for in vitro antibacterial and anti-biofilm activities against Streptococcus mutans, Staphylococcus aureus, and Escherichia coli. The F4 formulation demonstrated superior antibacterial efficacy, with inhibition zones of 64.2 ± 2.6 mm for S. mutans, 43.6 ± 1.0 mm for S. aureus, and 31.8 ± 1.5 mm for E. coli, and achieved 97.12% biofilm inhibition of S. mutans. Additionally, in vivo toxicity was assessed using embryonic zebrafish, showing a high survival rate of 93% for F1 and 82% for F4 after 24 hours, compared to 65% for CHX, indicating lower toxicity. This preclinical study shows that the F4 formulation exhibited promising antibacterial and safety profiles, highlighting its potential as a safe, natural oral care product targeting diverse oral pathogens with reduced toxicity. Further research, including in vivo and clinical trials, is needed to validate its effectiveness and safety for regular dental care use. The herbal mouthwash formulated with CEOZnONPs demonstrates strong antibacterial and anti-biofilm effects with lower toxicity, making it a promising natural alternative for oral hygiene. Its safer profile compared to CHX may reduce side effects in patients, potentially enhancing compliance in oral care regimens.
Similar content being viewed by others
Introduction
Mouthwashes, also known as mouth rinses, are frequently employed in oral care for their deodorizing, refreshing, or antiseptic properties. They are typically divided into two categories: cosmetic and chemotherapeutic1. Chemotherapeutic mouthwashes are designed to prevent and manage gingivitis, oral malodour, and plaque by killing bacteria, whereas cosmetic mouthwashes offer a pleasant flavour and are used temporarily to control or diminish bad breath2. Additionally, mouthwashes can be formulated as analgesic, anti-inflammatory, and antifungal solutions for oral care. The primary active components in mouthwashes are antimicrobial agents, which reduce the number of pathogenic microorganisms in the oral environment3.
The oral flora comprises over 300 recognized bacterial species. The accumulation of bacterial biofilms on tooth surfaces leads to the most common infectious oral diseases4. In the past decade, there has been a surge in oral microbiome studies, highlighting a growing interest in understanding the implications of the oral microbiome on human health and systemic diseases2. Various oral bacteria, including both aerobic and anaerobic species such as Lactobacillus, Actinobacillus, Staphylococcus, and Streptococcus, are linked to numerous oral diseases. The acidogenicity produced by these bacteria reduces the pH in the microenvironment to below 4.0, leading to tooth demineralization5. This underscores the importance of maintaining oral health to prevent dental and systemic diseases.
Numerous mechanical and chemical methods have been proposed for the eradication of various oral diseases, each with its own set of advantages and disadvantages. The daily use of mouthwash is commonly regarded as a straightforward and effective strategy to enhance oral health. However, most commercially available mouthwashes contain alcohol and other chemicals such as chlorhexidine gluconate (CHX) and triclosan6. Concerns have been raised over the years about the inclusion of ethanol and CHX gluconate is widely regarded as the gold standard antiplaque agent in mouthwashes, particularly its impact on the surfaces of composite restorations 7. Furthermore, CHX gluconate rinsing can cause side effects such as staining of the teeth and tongue, disturbances in taste perception, and minor irritation with superficial desquamation of the oral mucosa, which can significantly reduce patient acceptance of CHX mouthwash8. Other chemicals, including hydrogen peroxide, chlorine dioxide, cetylpyridinium, baking soda, and sodium bicarbonate, have been studied for their effectiveness against oral malodor9. Recent studies have also questioned the long-held belief that indiscriminately killing microbes is the primary desirable attribute of an effective antiseptic mouthwash. Instead, it is suggested that the oral microbial ecosystem, or oral microbiome, should be considered integral to both oral and systemic health3. Microbes in the oral cavity exist as a community, with certain bacterial species necessary for good oral health, while others are associated with disease. The side effects linked to the regular use of these chemicals have prompted researchers to seek more effective and safer alternatives for daily use10. This has led to the creation of new alcohol-free formulations containing herbal extracts or natural substances, which are highly attractive due to their potential to mitigate the antimicrobial resistance crisis. These alternatives balance oral health by preserving beneficial microbes and maintaining the overall health of oral tissues.
In the context of green chemistry and sustainable material development, it is crucial to explore green alternative precursors for the production of mouthwashes11. Plant and food products have emerged as valuable sources of natural antimicrobial compounds, many of which have demonstrated potential in preventing dental caries. Examples include neem, propolis, cranberry proanthocyanidins, green tea, grape seed extract, and the natural stilbene piceatannol12. The use of herbal medications has significantly increased recently due to their effectiveness and lack of negative side effects. Numerous researchers worldwide have evaluated and endorsed the antibacterial and anti-inflammatory properties of various herbal medications13. The therapeutic efficacy of herbal-based formulations is associated with secondary metabolites commonly present in plants14. Recently, attention has focused on using nanostructures, which offer advantages over conventional antibiotics due to lower cost, avoidance of resistance, and reduced acute toxicity. Consequently, metal nanoparticles have demonstrated considerable antimicrobial activity and hold promise for delivering various antimicrobial agents15. Zinc oxide nanoparticles (ZnONPs), in particular, are frequently chosen over other metal oxide nanoparticles because they are generally recognized as safe (GRAS) and less toxic16. Our previous study highlighted the potential anti-adherence and anti-biofilm activities of lemongrass (Cymbopogon citratus) essential oil (EO)17. Derived from the family, this essential oil contains a significant number of bioactive compounds, such as carveol, pinene, verbenyl acetate, citral (a mixture of geranial and neral), isoneral, isogeranial, geraniol, geranyl acetate, citronellal, citronellol, germacrene-D, and elemol. It exhibits numerous promising activities, including anti-inflammatory, antibacterial properties, anti-cancer effects, pain relief, and alleviation of common allergies related to dental applications17. Moreover, our previous investigation highlighted the incorporation of C. citratus EO into zinc Ooxide nanoparticle formulations through the green synthesis to eliminate S. mutans from dental caries.
The ideal therapeutic mouthwash should combine biocompatibility and antimicrobial properties to ensure effective disinfection and oral hygiene. This research is designed as a preclinical study, utilizing in vitro assays and zebrafish embryo models to establish a foundational understanding of the antibacterial efficacy and safety of CEOZnONPs-infused mouthwash. These models serve as a critical step in preclinical testing to evaluate the potential of new oral care formulations before advancing to human clinical trials.
Materials and methods
Preparation of herbal mouthwash
The herbal mouthwash was formulated using zinc oxide nanoparticles infused with C. citratus essential oil (CEOZnONPs) synthesized from our previous study. The mouthwash was prepared with varying concentrations of CEOZnONPs: 5 µg/mL (F1), 10 µg/mL (F2), 50 µg/mL (F3), and 80 µg/mL (F4). To optimize stability and dispersion of the formulation, Tween 80 was incorporated as a surfactant. The preparation process involved stirring the ingredients thoroughly (Table 1), heating the mixture to boiling for 10 minutes, followed by cooling and filtration to obtain a clear, refined solution.
Antioxidant activities
The antioxidant activity of the mouthwash formulations was assessed using the DPPH assay to determine their role in mitigating oxidative stress-induced oral inflammation. Antioxidants in mouthwash formulations may reduce inflammatory processes, supporting oral tissue. In this method, 100 µL of the mouthwash was combined with 100 µL of DPPH reagent and incubated for 30 min. The absorbance was then measured at 517 nm. The percentage inhibition was calculated using the following formula: % inhibition = [(Absorbance of control - Absorbance of sample) / Absorbance of control] × 10018.
Physical stability
The visual appearance and physical separation of the formulated mouthwash were evaluated. Four mouthwash formulations were stored at different temperatures, specifically 4 °C, 25 °C, 35 °C, 40 °C for a six-week period. The appearance of the formulations was assessed at these varying temperatures, and the results were documented accordingly. A calibrated pH meter (ESICO model − 1010) was employed to monitor pH stability. To assess any changes in pH, different mouthwash formulations were stored at controlled room temperatures of 27 °C and 35 °C for a duration of six weeks. pH was monitored at the end of this period and compared to determine any variations over the six-week timeframe.
Antimicrobial activity against different pathogens
The antibacterial activity of the prepared herbal mouthwash against three oral pathogens S. mutans MTCC890, S. aureus, and E. coli was assessed using the well diffusion method. A commercial mouthwash (CMW) served as the positive control. Wells were created in the agar plates, and 100 µg/mL concentrations of both the herbal mouthwash and the CMW were added to the respective wells for each bacterial strain. After incubation at 37 °C for 24 hours, the diameters of the inhibition zones surrounding the wells were measured to evaluate the antibacterial efficacy.
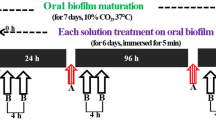
Anti biofilm test
To assess the inhibitory effect of the herbal mouthwash and CMW on biofilm formation by S. mutans MTCC890, S. aureus, and E. coli, an overnight bacterial culture was grown and adjusted to the 0.5 McFarland standard. This culture was then added to a 24-well plate, with each well containing a final volume of 100 µL BHI broth supplemented with 2% w/v sucrose. Various concentrations of the herbal mouthwash and CMW were introduced in two-fold dilutions. The microplate was incubated at 37 °C for 48 hours. Following incubation, the planktonic cells were carefully removed, and the remaining biofilm was washed with sterile phosphate-buffered saline (PBS). Biofilm biomass was quantified using the crystal violet (CV) assay, where the biofilm was stained with 0.01% w/v CV and subsequently eluted with 100 µL of 95% ethanol. The absorbance at 550 nm was measured to determine the biofilm biomass. The percentage of biofilm inhibition was calculated using the following equation:
where AC is the OD value obtained without treatment; AT is the OD value obtained with treatment.
Pre-clinical toxicity assessment using zebrafish embryos
The zebrafish (Danio rerio) embryo model was employed as part of the preclinical evaluation due to its genetic similarity to humans and its effectiveness in early-stage toxicity screening. Zebrafish embryos used in this study were obtained from the Central Inland Fisheries Research Institute (CIFRI), Mumbai, India. Embryos at 24 hours post-fertilization (hpf) were used for the toxicity experiments, with all embryos maintained under 5 days post-fertilization (dpf) to ensure compliance with ethical guidelines for early-stage testing. This model allows for rapid and ethical assessment of biocompatibility, which is critical before proceeding to more complex animal models or human studies. Embryos were maintained in overflow containers filled with conditioned water (E3 solution; 5 mM NaCl, 0.17 mM KCl, 0.33 mM CaCl₂, 0.33 mM MgSO₄; pH 7.2), prepared with double-distilled water.For the experiment, a six-well plate was used, with 10-12 mL of saline water carefully added to each well. Subsequently, 10 embryos were gently placed into each well. The ZnONPs-based mouthwash was then introduced into the wells at 100 µg/mL concentrations of different formulation of herbal mouthwash and CMW. The sixth well served as a control, containing only saltwater and live embryos without any treatment, as described in previous studies19. A comparison was made between the herbal mouthwash and the CMW. The six-well plate was incubated for approximately 24 hours, after which the number of live embryos in each well was recorded. The number of live cells was further assessed after one week. The percentage of live embryos was calculated using the following formula:
Statistical analysis
All experiments were conducted with six independent biological replicates (n = 6) to ensure statistical robustness. Data were expressed as mean ± standard deviation (SD). Statistical analysis was performed using one-way ANOVA followed by Tukey’s post hoc test. A p-value < 0.05 was considered statistically significant. Microsoft Excel and GraphPad Prism were used for data analysis.
Results
Formulation and stability check of mouthwash
Table 1 presents the ingredients and varying concentrations of the developed herbal mouthwashes. Erythritol was selected as a sweetener to mask the spicy flavour, while sodium benzoate was incorporated as a preservative at a concentration of 0.1% w/v. The antioxidant capacity of herbal mouthwash was assessed using DPPH radical scavenging assays, which revealed significant differences (p < 0.05). The CEOZnONPs mouthwash demonstrated moderate DPPH free radical scavenging activity, with values of 34.56%, 44.78%, 50.6%, and 55.90% for F1, F2, F3, and F4 formulations respectively (Table 2).
The pH of all four herbal mouthwash formulations (F1, F2, F3, F4) was measured using a digital pH meter, with the results presented in Fig. 1. Additionally, changes in color, odor, physical separation, and homogeneity were monitored over a six-week period at varying temperatures (4 °C to 40 °C). No significant changes were observed in any of the formulations for at least four weeks. However, slight color changes were noted during the 5th and 6th weeks, particularly when stored at higher temperatures (38 °C to 40 °C), though there were no detectable changes in odor or homogeneity (Table 3). Notably, continued observations have indicated that the formulations have remained stable beyond the initial six-week period, maintaining their physical integrity for several months under ambient conditions. These findings suggest a promising extended shelf-life, although further long-term stability assessments are ongoing to confirm these results.
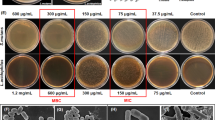
Antibacterial activity of mouthwash
The herbal mouthwashes demonstrated notable antibacterial activity against all three pathogens i.e. S. mutans MTCC890, S. aureus & E. coli (Table 4). Herbal mouthwash with formulation F4 exhibited the highest zone of inhibition (ZOI) with a diameter of 64.2 ± 2.6 mm against S. mutans, followed by S. aureus (43.6 ± 1.0 mm), E. coli (31.8 ± 1.5 mm) (Table 4). In comparison, the CMW exhibited comparatively lower ZOI i.e. 44.7 ± 2.3 mm, 43.6 ± 1.7, 30.5 ± 1.4 against S. mutans, S. aureus and E. coli respectively. These findings indicate that CEOZnONPs, particularly at higher concentrations, enhance antibacterial efficacy.
Anti-biofilm study
Figure 2 illustrates the percentage of inhibition for anti-biofilm activity. The F4 formulation of the herbal mouthwash exhibited a remarkable 97.12 ± 0.44% inhibition of biofilm formation against S. mutans MTCC890. It also showed significant inhibition against S. aureus and E. coli, with values of 74.02 ± 0.2% and 59.98 ± 1.8%, respectively. The F3 formulation inhibited biofilm formation by 92.92%, 68.25 ± 0.4%, and 47.59% against S. mutans, S. aureus, and E. coli, respectively. The other two formulations(F1, F2) with lower concentrations of CEOZnONPs also exhibited considerable anti-biofilm activity against the three pathogens (Table 4). In contrast, the control commercial mouthwash showed comparatively lower inhibition rates, with values of 82.78%, 85.09%, and 71.65% against S. mutans, S. aureus, and E. coli, respectively (Fig. 2).
Pre-clinical toxicity assessment using zebrafish embryos
The cytotoxicity of the ZnONPs-based herbal mouthwash, prepared with C. citratus EO, was assessed in comparison to a commercial mouthwash across various concentrations. The herbal mouthwash F1(lower concentration) containing lowest concentration of CEOZnONPs maintained 93% live embryos in 24 hours. However, formulation F4 (highest concentration) of the herbal mouthwash demonstrated 82% survival rate of live embryos in 24 h, indicating lower toxicity than the commercial mouthwash. The commercial mouthwash containing CHX showed significantly higher toxicity, with only 65% live embryos within 16 hours(Fig. 3). No significant difference is noticed in toxicity level of different mouthwashes in 24 hours and one week within the herbal formulations indicating stable safety profiles over time. Overall, CEOZnONPs formulations exhibited markedly lower toxicity compared to CMW.
Discussion
Dental plaque is recognized as a primary etiological factor in the development of caries, gingivitis, and periodontal disease. Effective control of biofilm is essential to prevent these conditions. Various strategies are currently employed to combat biofilm formation by oral pathogens20. Among these, mouthwashes serve as adjuncts to mechanical plaque control methods, helping to reduce biofilm accumulation. Mouthwashes with antimicrobial properties exert their effects through three primary mechanisms: inducing apoptosis, inhibiting bacterial growth or cellular metabolism, and depending on their concentration, exhibiting either bactericidal or bacteriostatic properties1. Although CHX is widely used for plaque control due to its antimicrobial activity, its long-term use is limited by side effects such as taste alteration, supragingival calculus formation, oral mucosal desquamation, and contraindications in paediatric patients6,7.
Therefore, there is growing interest in safer, plant-based alternatives for effective plaque and biofilm control, such as essential oil-based nanoparticle formulations. Numerous studies have compared CHX with herbal mouthwashes. While herbal formulations may be less effective than chlorhexidine, they offer a safer alternative for oral prophylaxis without adverse effects. Our previous research demonstrated the efficacy of C. citratus EOs as natural anti-biofilm agents, particularly in preventing dental cavities17. The EOs showed significant antimicrobial activity against S. mutans biofilms, highlighting their potential as selective and non-invasive antimicrobial agents. Additionally, ZnONPs synthesized using lemongrass essential oil via green methods exhibited promising antimicrobial activity against oral pathogens. This study aims to formulate and evaluate an herbal mouthwash and compare its efficacy with a commercially available mouthwash. In this study, four mouthwash formulations were prepared, each containing varying concentrations of C. citratus ZnONPs: 5 µg/mL (F1), 10 µg/mL (F2), 50 µg/mL (F3), and 80 µg/mL (F4). The purpose of these variations was to determine the concentration with the most effective antibacterial activity and optimal consistency. The formulation process also involved the use of surfactants like Tween 80 and glycerol, which enhance solubility and reduce surface tension in oil-water solutions by stabilizing the interfacial layers, thus producing a clear and stable mouthwash.
The study evaluated the acidity (pH), stability, irritation potential, and antioxidant properties of the four mouthwash formulations, along with their antibacterial effects against three pathogens. The alcohol-free herbal formulations exhibited a transparent appearance, good water dispersion, and a pleasant aroma. The antioxidant activity, measured using the DPPH free radical scavenging assay, ranged from 34.56 to 55.78%, with the highest scavenging activity observed in the ZnONPs. However, this activity was lower than that reported in previous studies, such as Ulvan-silver nanoparticles at 50 µg/mL or 5% v/v, which exhibited significant antioxidative properties. It is worth considering that higher concentrations might yield enhanced activities21. Moreover, the herbal mouthwash showed greater antibacterial efficacy against S. mutans compared to S. aureus and E. coli, with the highest ZOI of 55 ± 2.5 mm observed against S. mutans across all formulations (F1, F2, F3, F4). This aligns with previous findings on the notable antibacterial activity of lemongrass ZnONPs against oral pathogens. The choice of lemongrass for nanoparticle synthesis reflects the increasing interest in utilizing natural plant properties for therapeutic purposes, as supported by prior studies22,23.
Biofilms serve as protective shelters for microorganisms, promoting pathogen survival. Antimicrobial agents are evaluated for their potency, bacteria-killing rate, and efficacy against biofilms, including their ability to kill bacteria or inhibit biofilm formation24. In this study, a biofilm assay was employed to assess the viability of cells within the biofilm. The F2 concentration of mouthwash effectively killed approximately 80% of biofilm biomass, with significant inactivation of S. mutans,S. aureus and E.coli cells within the biofilm. Furthermore, the highest concentration formulation, F4, nearly eradicated 96% of the biofilm produced by the highly cariogenic S. mutans, demonstrating its potent antibacterial activity. Several studies have reported the effects of different compounds on biofilms but not on planktonic cells, with sub-MIC levels of lemon essential oil and tea extract showing biofilm suppression with minimal impact on planktonic cell growth24,25.
Mouthwashes are a popular oral care product for routine use. This study also included pre-clinical test using zebrafish embryo to investigate potential toxicity. The results indicated that the ZnONPs-mediated mouthwash was less toxic than the commercially available chlorhexidine mouthwash, suggesting its suitability for regular use. The cytotoxic impact was evaluated using a brine shrimp mortality assay, where 80% of live embryo were observed at a concentration of 80 µg/mL, consistent with findings from other studies involving ZnONPs synthesized from coffee bean and xylitol26. In line with this study, research by Shanmugam et al. (2024) also found that ZnONPs synthesized using green methods from lemongrass and mint herbal formulations exhibited promising antimicrobial activity against oral pathogens22.
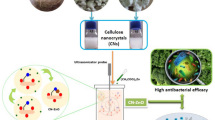
Bacterial adherence to tooth surfaces is primarily facilitated by sucrose-dependent adhesion, which significantly contributes to biofilm formation. This process is accelerated by the enzymatic conversion of sucrose into glucose, catalyzed by genes such as gtfB/C. The quorum sensing (QS) system further enhances biofilm maturation by enabling bacteria to optimize their physiological responses based on population density and environmental stimuli27. C. citratus EO combined with ZnONPs presents a potent antimicrobial herbal mouthwash, particularly effective against pathogens responsible for dental caries in the oral environment. The key bioactive compounds in CEO include carveol, pinene, and verbenyl acetate, each contributing distinctively to this antimicrobial effect17.
Although the molecular pathways were not directly validated in this study, the proposed mechanism illustrated in Fig. 4 is based on literature-supported roles of CEO-derived compounds and ZnONPs. Carveol disrupts bacterial cell membranes by integrating into the lipid bilayer, increasing membrane permeability, leading to the leakage of essential cellular contents, which ultimately results in cell death and inhibition of biofilm formation a critical factor in the development of dental caries28. Pinene enhances this antimicrobial action by further compromising membrane integrity and inhibiting bacterial metabolic processes. Additionally, pinene’s anti-inflammatory properties help mitigate the inflammation commonly associated with dental caries29. This compound specifically targets bacterial adhesion mechanisms and the production of glucosyltransferases (Gtfs), notably gtfB and gtfC. These enzymes synthesize glucans from sucrose, which are crucial components of the biofilm matrix. By inhibiting gtfB and gtfC, verbenyl acetate reduces glucan synthesis, weakening the biofilm structure and diminishing the virulence of S. mutans. Verbenyl acetate also inhibits bacterial enzyme activity and prevents pathogens from adhering to dental surfaces, thereby obstructing the initial stages of biofilm formation and subsequent caries development30.
This study concludes that the observed inhibition of bacterial growth by ZnONPs is attributable to their strong antibacterial efficacy. This remarkable antibacterial effect is largely due to the increased surface area of the smaller nanoparticles and the combined mechanisms described above31. The synergistic action of these compounds, together with ZnONPs, produces a comprehensive antimicrobial effect, making CEOZnONPs mouthwash a promising natural alternative for oral care. Further clinical trials will be required to confirm translational relevance.
Conclusion
This study introduces a groundbreaking strategy for combatting dental caries, employing C. citratus EO to synthesize ZnONPs. The nanoparticles, characterized for stability and uniformity, exhibit potent antioxidant and antibacterial properties against S. mutans, a key contributor to dental caries. In vivo experiments on Wistar rats validate their efficacy in significantly reducing S. mutans CFU, confirming their ability to inhibit caries formation. Mechanistically, these nanoparticles disrupt bacterial cell walls, inhibit biofilm formation, and reduce acid production, offering an eco-friendly solution for oral microbial defence. The proposed mechanism involves the generation of ROS, Zn2+ ion release, and direct interaction with bacterial cell membranes, resulting in cellular damage and death. This study underscores the promising role of green-synthesized ZnO NPs as effective agents against dental caries, providing a sustainable and environmentally friendly alternative to conventional antimicrobial treatments, thereby addressing the global health concern of dental caries and mitigating challenges associated with antimicrobial resistance.
Data availability
All the data are present in the manuscript.
References
Shahidulla, S. M., Begum, S. & Sikora, M. Mouthwash: an advanced perspective. Eur. J. Biomed. 11 (5), 207–214 (2024).
Pawar, S. R., Ahire, M. G. J., Jain, B. V. & Shaikh, M. T. Y. Dynamic formulation of effervescent antimicrobial mouthwash review. Oral Health 4, 12 (2022).
Lee, S. H. et al. Antibacterial and anti-inflammatory potential of mouthwash composition based on natural extracts. Appl. Sci. 11 (9), 4227 (2021).
Colombo, A. P. V., do Souto, R. M., da Silva-Boghossian, C. M., Miranda, R. & Lourenço, T. G. B. Microbiology of oral biofilm-dependent diseases: have we made significant progress to understand and treat these diseases? Curr. Oral Health Rep. 2, 37–47 (2015).
Chattopadhyay, I., Verma, M. & Panda, M. Role of oral microbiome signatures in diagnosis and prognosis of oral cancer. Technol. Cancer Res. Treatment 18, 1533033819867354 (2019).
Maziere, M., Rompante, P., Andrade, J. C. & Rodrigues, C. F. Are mouthwashes really effective against Candida spp.? J. Fungi 10 (8), 528 (2024).
Kamal, D., Hassanein, H., Akah, M., Abdelkawy, M. A. & Hamza, H. Caries preventive and antibacterial effects of two natural mouthwashes vs chlorhexidine in high caries-risk patients: a randomized clinical trial. J. Contemp. Dent. Pract. 21 (12), 1316–1324 (2020).
Kamolnarumeth, K. et al. Effect of mixed chlorhexidine and hydrogen peroxide mouthrinses on developing plaque and stain in gingivitis patients: a randomized clinical trial. Clin. Oral Invest. 25, 1697–1704 (2021).
Radzki, D., Wilhelm-Węglarz, M., Pruska, K., Kusiak, A. & Ordyniec-Kwaśnica, I. A fresh Look at mouthwashes—what is inside and what is it for? In. J. Environ. Res. Public Health 19 (7), 3926 (2022).
Sedghi, L., DiMassa, V., Harrington, A., Lynch, S. V. & Kapila, Y. L. The oral microbiome: role of key organisms and complex networks in oral health and disease. Periodontology 87 (1), 107–131 (2021).
de Moraes, F. M. B., Lopes, L. C. & Kulay, L. Proposals for the redesign of the mouthwash production chain based on environmental performance indicators. J. Clean. Prod. 311, 127679 (2021).
Chen, X. et al. Microbial etiology and prevention of dental caries: exploiting natural products to inhibit cariogenic biofilms. Pathogens 9 (7), 569 (2020).
Tasneem, S., Liu, B., Li, B., Choudhary, M. I. & Wang, W. Molecular Pharmacology of inflammation: medicinal plants as anti-inflammatory agents. Pharmacol. Res. 139, 126–140 (2019).
Ukoroije, R. B. & Otayor, R. A. Review on the bio-insecticidal properties of some plant secondary metabolites: types, formulations, modes of action, advantages and limitations. Asian J. Res. Zool. 3 (4), 27–60 (2020).
Rice, K. M., Ginjupalli, G. K., Manne, N. D., Jones, C. B. & Blough, E. R. A review of the antimicrobial potential of precious metal derived nanoparticle constructs. Nanotechnology 30 (37), 372001 (2019).
Al Jabri, H. et al. Zinc oxide nanoparticles and their biosynthesis: overview. Life 12 (4), 594 (2022).
Pallavi, P., Sahoo, P. P., Sen, S. K. & Raut, S. Comparative evaluation of anti-biofilm and anti-adherence potential of plant extracts against Streptococcus mutans: A therapeutic approach for oral health. Microbial Pathogenesis 188, 106514 (2024).
Sithisarn, P., Rojsanga, P., Sithisarn, P. & Kongkiatpaiboon, S. Antioxidant activity and antibacterial effects on clinical isolated Streptococcus suis and Staphylococcus intermedius of extracts from several parts of Cladogynos orientalis and their phytochemical screenings. Evid.-Based Complement. Altern. Med. 2015(1), 908242 (2015).
Datta, A. et al. Green synthesis of zinc oxide nanoparticles using parthenium hysterophorus leaf extract and evaluation of their antibacterial properties. J. Biotechnol. Biomater. 7 (3), 271–276 (2017).
Cortés, M. E., Bonilla, J. C. & Sinisterra, R. D. Biofilm formation, control and novel strategies for eradication. Sci. Against Microb. Pathog Commun. Curr. Res. Technol. Adv. 2, 896–905 (2011).
Mohandoss, S. et al. Ulvan as a reducing agent for the green synthesis of silver nanoparticles: a novel mouthwash. Inorganics 11 (1), 5 (2022).
Shanmugam, R., Govindharaj, S., Arunkumar, P., Sanjana, G. S. & Manigandan, P. Preparation of a herbal mouthwash with lemongrass and mint-mediated zinc oxide nanoparticles and evaluation of its antimicrobial and cytotoxic properties. Cureus 16, 2 (2024).
Agarwal, H., Nakara, A., Menon, S. & Shanmugam, V. Eco-friendly synthesis of zinc oxide nanoparticles using Cinnamomum Tamala leaf extract and its promising effect towards the antibacterial activity. J. Drug Deliv. Sci. Technol. 53, p.101212 (2019).
Bayramov, D. F. & Neff, J. A. Beyond conventional antibiotics-New directions for combination products to combat biofilm. Adv. Drug Deliv. Rev. 112, 48–60 (2017).
Xu, X., Zhou, X. D. & Wu, C. D. Tea Catechin Epigallocatechin gallate inhibits Streptococcus mutans biofilm formation by suppressing Gtf genes. Arch. Oral Biol. 57 (6), 678–683 (2012).
Pakravanan, K., Rezaee Roknabadi, M., Farzanegan, F., Hashemzadeh, A. & Darroudi, M. Amorphous calcium phosphate nanoparticles-based mouthwash: preparation, characterization, and anti-bacterial effects. Green Chem. Lett. Rev. 12 (3), 278–285 (2019)..
Zhang, Q., Ma, Q., Wang, Y., Wu, H. & Zou, J. Molecular mechanisms of inhibiting glucosyltransferases for biofilm formation in Streptococcus mutans. Int. J. Oral Sci. 13 (1), 30 (2021).
Faleiro, M. L. & Miguel, M. G. Use of essential oils and their components against multidrug-resistant bacteria. In Fighting Multidrug Resistance with Herbal Extracts,Essential Oils and Their Components 65–94 (Academic press, 2013).
Nuă, D. C. et al. Contribution of essential oils to the fight against microbial biofilms-A review. Processes 9 (3), 537 (2021).
Bouzidi, L. E. et al. Chemical composition and anticandidal properties of the essential oil isolated from aerial parts of Cotula cinerea: a rare and threatened medicinal plant in Morocco. Nat. Prod. Commun. 6 (10), 934578X1100601021 (2011).
Sirelkhatim, A. et al. Review on zinc oxide nanoparticles: antibacterial activity and toxicity mechanism. Nano-micro Lett. 7, 219–242 (2015).
Acknowledgements
The authors wish to thank the Management of Centre for Biotechnology, Siksha ‘O’ Anusandhan (Deemed to be University) Bhubaneswar for encouragement and motivation to carry out the research work.
Funding
Open access funding provided by Siksha 'O' Anusandhan (Deemed To Be University)
Author information
Authors and Affiliations
Contributions
Preeti Pallavi: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. Pragnya paramita Sahoo: Data curation, Formal analysis. Adyasha Anapurba Sahoo: Formal analysis, Resources. Sudip Kumar Sen and Sangeeta Raut: Conceptualization, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
This work is approved by ethical committee School of Pharmaceutical Sciences and the project proposal No. IAEC/SPS/SOA/118/2023. Zebrafish embryos used in this study were obtained from the Central Inland Fisheries Research Institute (CIFRI), Mumbai, India. All procedures were conducted in accordance with institutional and national guidelines for the care and use of laboratory animals. This study is reported in accordance with the ARRIVE guidelines (https://arriveguidelines.org) for animal research reporting.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pallavi, P., Sahoo, P.P., Sahoo, A.A. et al. Green synthesized zinc oxide nanoparticles with lemongrass essential oil for the development of an effective herbal mouthwash. Sci Rep 15, 31118 (2025). https://doi.org/10.1038/s41598-025-16877-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-16877-7