Abstract
The COVID-19 pandemic disrupted cardiovascular disease management. This single-center cross-sectional cohort study evaluated cardiopulmonary function changes in acute coronary syndrome (ACS) patients post-percutaneous coronary intervention (PCI) without SARS-CoV-2 infection and explored pandemic-related influencing factors. We analyzed 7,650 ACS patients undergoing complete PCI revascularization and cardiopulmonary exercise testing (CPET) between October 2018 and December 2023, stratified into pre-pandemic (cut-off: February 1, 2020), during-pandemic, and post-pandemic (cut-off: December 31, 2022) groups. Propensity Score Matching (PSM) balanced baseline characteristics, yielding 4,503 patients for analysis. Clinical/laboratory data and CPET results were compared across groups using one-way analysis of variance (ANOVA). The primary CPET parameter, peak oxygen uptake per kilogram (peak VO₂/kg), was significantly lower in the during-pandemic group (15.07 ± 4.09 ml/min/kg) compared to the pre-pandemic group (15.56 ± 3.74 ml/min/kg) and the post-pandemic group (15.69 ± 4.04 ml/min/kg). Machine learning and multivariate logistic regression were used to select key variables related to cardiopulmonary function. The findings indicate that older age, female sex, higher BMI, elevated SYNTAX score, increased NT-pro BNP levels, elevated HbA1c, smoking, anxiety, and higher ACS severity classification were positively correlated with impaired cardiopulmonary function. These results highlight associations between the pandemic and cardiovascular rehabilitation outcomes, emphasizing the need for tailored interventions during healthcare crises.
Similar content being viewed by others
Introduction
Since the onset of the COVID-19 pandemic in late 20191, acute coronary syndrome (ACS) patients had confronted dual challenges in managing cardiovascular conditions and pandemic-related care delays. Prior studies focused on SARS-CoV-2’s direct cardiovascular impacts, including elevated in-hospital mortality rates and worsened pre-existing conditions2,3 while SARS-CoV-2-negative ACS patients may experience impaired cardiopulmonary recovery following percutaneous coronary intervention (PCI) due to pandemic-driven socio-environmental changes.
Cardiorespiratory fitness provides a wealth of information related to health status and prognosis4. Cardiopulmonary Exercise Testing (CPET), as a crucial tool for assessing cardiopulmonary endurance and functional recovery, provides important data to evaluate recovery progress5. In patients with chronic systolic heart failure, a moderate improvement in peak oxygen uptake over three months is associated with improved clinical outcomes6. Studies conducted during the COVID-19 pandemic have indicated that CPET serves as a crucial tool for accurately assessing baseline cardiorespiratory fitness levels, developing personalized exercise training regimens, and tracking rehabilitation progress longitudinally in patients with long COVID7. Therefore, we selected CPET as the primary outcome measure.
Machine learning (ML) algorithms excel at learning complex feature-label relationships, often surpassing human performance in classification tasks, making them ideal for analyzing heterogeneous clinical data to support medical decision-making. The reviews in 2019 and 2023 highlighted ML applications in medicine8,9. In cardiovascular disease prognosis10 ML models like the ECG-based system demonstrate clinical utility by predicting major adverse cardiovascular events. Given the substantial number of observed variables in this study and the requirement to identify critical variables, we employed machine learning algorithms such as Random Forest and XGBoost to conduct variable selection.
The present study retrospectively analyzed the CPET characteristics of ACS patients who underwent PCI between October 2018 and December 2023, focusing specifically on SARS-CoV-2-negative individuals. This research aims to: 1) Characterize changes in CPET parameters among SARS-CoV-2-negative ACS patients post-PCI during the pandemic. 2) Identify pandemic-associated factors for impaired cardiopulmonary function using ML.
Method
Data source and case selection
This cross-sectional study included patients diagnosed with ACS who underwent PCI at the General Hospital of Northern Theater Command between October 2018 and December 2023. The study patients meet the following inclusion criteria: (1) A confirmed diagnosis of ACS and undergoing PCI treatment; (2) Complete revascularization had been achieved; (3) Aged over 18 years old; (4) No history of respiratory diseases affecting ventilatory function; (5) Completion of CPET before discharge; (6) The clinical and CPET data were recorded accurately and completely.
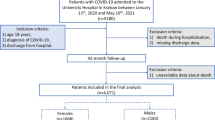
The patients were divided into three groups according to the period of COVID-19 pandemic: pre-pandemic, during-pandemic and post-pandemic. The cut-off points were February 1, 2020 and December 31, 202211 aligned with China’s public health response shifts. It is noteworthy that, in the context of implementing a stringent “dynamic zero-COVID” prevention and control strategy, patients who underwent PCI treatment were confirmed SARS-CoV-2-negative through routine RT-PCR testing of nasopharyngeal swabs. Ultimately, there were a total of 7,650 (2,252 pre-pandemic, 3,878 during-pandemic and 1,520 post-pandemic) eligible participants enrolled in our analysis (Fig. 1).
Clinical information acquisition
Electronic Medical Records (EMR) (including physical examination, laboratory tests and questionnaires, cardiopulmonary evaluation, complete blood counts, ultrasound scans, and biochemical tests, etc.) were collected from the hospital information system and the information first recorded after admission was extracted. Specifically, they include sex, body mass index, and age, whether the patient smokes or drinks alcohol, whether they have comorbid diabetes, hypertension, cerebrovascular disease, arrhythmia, atrial fibrillation, heart failure and chronic kidney disease, as well as any history of myocardial infarction, thyroid disease history, hemoglobin concentration, creatinine, blood urea nitrogen, uric acid, glycosylated hemoglobin, N-terminal pro-brain natriuretic peptide, Hypersensitive C-reactive protein, cardiac troponin T, creatine kinase-MB, Fasting serum glucose, interleukin 6, Serum cholesterol, triglyceride, Homocysteine, Low-Density Lipoprotein Cholesterol, High density lipoprotein cholesterol, the left ventricular ejection fraction, forced vital capacity(FVC), forced expiratory volume in one second (FEV1), FEV1/FVC, maximum vital capacity. Coronary angiography results include the target lesion site and the SYNTAX score. The SYNTAX score, which quantifies the complexity and extent of coronary artery lesions, was assessed by interventional cardiologists during coronary angiography and subsequently documented in the EMR. The target lesion sites include the left anterior descending artery, left main artery, left circumflex artery, and right coronary artery, diagonal. Psychological test data include the Generalized Anxiety Disorder-7 and Patient Health Questionnaire-9 scales.
Cardiopulmonary exercise testing (CPET)
Prior to each CPET, patients undergo static lung function tests, calibrated with reference gases to ensure accuracy. The dynamic function is then assessed using bicycle ergometers (SCHILLER, Baar, Switzerland)12.
After a brief resting period, participants engaged in 2–3 min of unloaded exercise at 60 revolutions per minute. This phase was followed by a gradual increase in load, adjusted by adding 10% of the estimated exercise power, which was calculated based on each participant’s age, height and weight. This increment continued until an equilibrium of oxygen uptake and carbon dioxide excretion was reached13. The exercise was continued until the criteria for test termination, as set by the American Heart Association14 were met. Meanwhile, rehabilitation technicians recorded various CPET test outcomes, including peak oxygen uptake, anaerobic threshold oxygen uptake and other physiological metrics. Metabolic equivalent (MET) is estimated as the energy cost of a given activity divided by resting energy expenditure: 1 MET approximating 3.5 ml/kg/min.
Definitions and preliminary data processing
Acute coronary syndromes are characterized by a sudden reduction in blood supply to the heart and include ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina (UA)15,16.
The Weber classification assesses cardiac function based on Peak VO2 and exercise limitation, objectively reflecting the heart’s efficiency in pumping blood during exercise. The Weber classification system categorizes patients into four groups: A, B, C, and D17. It is considered that patients in A/B have low-risk cardiac function; C/D have high-risk cardiac function18.
The psychological status of the patients was assessed by Generalized Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) self-rating scales before CPET. GAD-7 is a self-rating scale which consists of 7 items, using a 4-level scoring system of 0–3, with an overall score range of 0–21 points. GAD-7 scores of 5, 10 and 15 represented mild, moderate and severe anxiety, respectively19. PHQ-9 is a self-rating scale for diagnosing and assessing depression severity, with scores indicating mild to severe depression. PHQ-9 scores 5, 10, 15, and 20 correspond to mild, moderate, moderately severe, and severe depression20.
For data processing, sex was recorded male = 1 or female = 0. GAD-7 was recorded as normal = 0, mild = 1, moderate = 2 and severe = 3. PHQ-9 was recorded as normal = 0, mild = 1, moderate = 2, moderately severe = 3, and severe = 4. Smoking status and drinking status were recorded as never = 0, former = 1 and active = 2. Lastly, medical history was recorded as yes = 1 or no = 0. Aiming to maintain the largest possible sample size, multiple imputation was implemented under the assumption of missing at random, even with minimal missingness (< 5% across all variables) observed in the dataset.
Machine learning
To identify the key variables affecting cardiorespiratory function in the during-pandemic group, the least absolute shrinkage and selection operator (LASSO), a logistic regression method for filtering variables, was initially adopted in this work to screen the candidate variables with the “glmnet” package of R21. Next, the random forest (RF), integrating multiple trees through the idea of ensemble learning to gain better accuracy, was employed to narrow down the candidate variables with the “randomForest” package as well. eXtreme Gradient Boosting (XGBoost) is an efficient, flexible, and lightweight algorithm that has been widely used in data mining, recommender systems, and other fields. In the present study, the XGBoost algorithm was implemented through the “xgboost” package to identify pivotal variables utilizing its built-in feature importance assessment capabilities.
To investigate factors associated with cardiopulmonary function status during the COVID-19 pandemic, 3,878 patients in the during-pandemic group were used to construct our models (Fig. 1). These data were randomly divided into a training set (70%) and a test set (30%). All models were trained on the training dataset and subsequently validated using the test set.
Statistical analysis
Continuous variables were reported as the mean ± standard deviation (SD) for normally distributed measurement data or median (P25-P75) for non-normally distributed measurement, and categorical variables were expressed as frequencies with percentages. For categorical variables, differences among the groups were evaluated by the Chi-square test followed by Bonferroni’s correction in multiple comparisons. For continuous variables, differences among the three groups were analyzed by one-way analysis of variance (ANOVA) with LSD or rank sum test with Kruskal-Wallis H test, followed by post-hoc analysis (Bonferroni’s correction). A 2-sided P value < 0.05 was considered significant for all tests. We conducted PSM to adjust the baseline characteristics of the groups. The following PSM settings were performed using the R package ‘MatchIt’ (v4.5.5) pairing and nearest neighbor methods, with a caliper of 0.05. Statistical analyses were performed using R 4.3.2.
Ethics
The study was approved by the Institutional Review Board (IRB) of General Hospital of Northern Theater Command with number: Y2024(190). As the data are anonymous, the informed consent stipulation was exempted. Due to the retrospective nature of the study, (General Hospital of Northern Theater Command of IRB) waived the need of obtaining informed consent. The research conformed to the principles of the Helsinki Declaration.
Results
Comparison of the baseline clinical characteristics
A total of 7,650 patients (2,252 pre-pandemic, 3,878 during-pandemic and 1,520 post-pandemic) who met inclusion criteria were enrolled in this study. The demographic and medical history characteristics of the entire cohort are shown in Table 1. Several baseline clinical characteristics among the three groups were significantly different (Supplementary Table 1).
Compared to the pre-pandemic and the post-pandemic patients, the during-pandemic patients were older. Moreover, patients during the pandemic exhibited a significantly higher percentage of abnormal PHQ-9 results compared to both the pre-pandemic and post-pandemic groups. In addition, compared to the other two groups, the proportion of patients with a history of stroke and myocardial infarction is lower in during-pandemic. Static pulmonary function indicators and laboratory test results also exhibit intergroup differences. However, some variables, such as SYNTAX score, target vessel, and history of hypertension and diabetes, were similar among the three groups.
PSM and CPET difference analysis
PSM was used to balance the baseline clinical characteristics among the three groups. The covariates used for propensity score generation, along with the standardized mean differences before and after matching, are presented in Supplementary Data 1.
Before PSM, a total of 7,650 patients were enrolled in the analysis, and 4,503 patients (1,503 pre-pandemic, 1,503 during-pandemic and 1,503 post-pandemic) were included in the analysis after PSM. The clinical data of the three groups after PSM are shown in supplementary Table 2.
The CPET results indicated that patients in the during-pandemic group demonstrated poorer cardiopulmonary exercise parameters compared to those in the pre-pandemic and post-pandemic groups. Patients demonstrated a declining trend in Peak VO2/kg during the pandemic.
Before PSM, as shown in Table 2, all CPET indexes in the pre-pandemic group were significant different from those in the during-pandemic group. After PSM (Table 3), Peak VO2/kg (15.07 ± 4.09 vs. 15.56 ± 3.74, p <.05), Peak METs (4.31 ± 1.17 vs. 4.44 ± 1.07, p <.05), Peak O2 pulse (9.27 ± 2.49 vs. 9.69 ± 2.31, p <.05), AT METs (3.37 ± 0.56 vs. 3.43 ± 0.46, p <.05) and AT O2 pulse (7.82 ± 1.96 vs. 8.11 ± 1.70, p <.05) of the during-pandemic group were lower than those of the pre-pandemic group. In addition, the proportion of patients with Weber C/D grade during the pandemic was slightly higher than that in the pre-pandemic group. However, the Peak VO2, AT VO2/kg and borg score were similar between the two groups.
Before PSM, compared with the post-pandemic group, there were differences in CPET indexes between the during-pandemic groups and the post-pandemic group (p <.05) except AT METs and Peak O2 pulse. After PSM (Table 3), Peak VO2 (1.12 ± 0.34 vs. 1.17 ± 0.35,p <.05), Peak VO2/kg (15.07 ± 4.09 vs. 15.69 ± 4.04,p <.05), AT VO2/kg (10.73 ± 2.33 vs. 11.25 ± 2.41, p <.05), AT O2 pulse (7.82 ± 1.96 vs. 8.01 ± 2.04, p <.05), Peak METs (4.31 ± 1.17 vs. 4.48 ± 1.15, p <.05) in the during-pandemic group were lower than those in the post-pandemic group, and Borg scores were higher than those in the post-pandemic group. However, AT METs, Peak O2 pulse, were similar between the two groups.
The during-pandemic patients exhibited mean VO₂/kg reductions of 0.49 mL/kg/min and 0.62 mL/kg/min compared to pre- and post-epidemic groups, respectively.
Screening of the key factors via machine learning
Due to the large number of research variables included in this study, the correlation between different variables, and the limited number of samples with positive outcome events, LASSO, RF and XGBoost were used to screen and reduce the dimension of variables except CPET, so as to select key variables related to Weber classification.
The predictive performance was evaluated through comprehensive metrics including recall, accuracy, precision, F1-score (Supplementary Table 3), confusion matrix analysis, Area Under the ROC Curve (AUC), and Receiver Operating Characteristic (ROC) curve examination (Fig. 2). All three models demonstrated robust performance across evaluation metrics. Model training parameters was provided in the Supplementary Table 4.
As shown in Fig. 3, we performed variables selection using the LASSO logistic regression model. The Fig. 3a showed the adjustment of parameters in the LASSO model using 10-fold cross validation to obtain a minimum standard. The binomial deviance was plotted versus log (λ). As shown in Fig. 3a, dotted vertical lines were drawn at the optimal values by using the minimum criteria (the left) and the 1 standard error of the minimum criteria (the right). Finally, we obtained 13 (Fig. 3b) as the most significant cardiopulmonary function-related variables. These variables are age, SYNTAX score, GAD-7, Hb, HbA1c, smoking, NT-pro BNP, BMI, FVC, FEV1, sex, ACS classification, prior PCI, respectively (Fig. 4a). The distribution of coefficients for each feature is shown in Supplementary Table 5.
Visualization of Variable Importance Screening and Ranking. (a) Variable importance plot of LASSO, and the top 13 variables were selected. (b) Variable importance plot of RF, and the top 15 variables were selected. (c) Variable importance plot of XGBoost, and the top 15 variables were selected. (d) The venn diagram displaying 11 common factors between LASSO, RF and XGBoost. Abbreviations: BMI, body mass index; FVC, forced vital capacity; NT-proBNP, N-terminal pro-brain natriuretic peptide; HbA1c, glycated hemoglobin; Hb, hemoglobin; GAD-7, Generalized Anxiety Disorder Questionnaire-7; ACS, acute coronary syndrome; hsCRP, Hypersensitive C-reactive protein; CK-MB, creatine kinase-MB, Glu, Fasting serum glucose; FEV1, forced expiratory volume in one second; PCI, percutaneous coronary intervention; VC, maximum vital capacity; TG, triglyceride.
As shown in Fig. 4b, the Random Forest model was used to select variables and derive variable importance. The important variables impacting cardiopulmonary function include (in decreasing importance): FVC, VCmax, FEV1, sex, BMI, SYNTAX score, age, NT-pro BNP, Hb, HbA1c, GAD-7, CK-MB, smoking, hsCRP, ACS classification.
XGBoost was additionally used to evaluate and filter candidate variables through Gini index gain criterion-based importance quantification, ultimately identifying the top 15 core variables demonstrating substantial significance for the target outcome. As shown in Fig. 4c, the variable importance hierarchy is visualized in descending order.
Through the combined selection process using LASSO, RF and XGBoost, a total of 11 variables common to the three models were identified for multivariate logistic regression analysis (Fig. 4d).
Multivariate logistic regression analysis of the key factors
We incorporated the key variables selected by the three models (Random Forest, LASSO, and XGBoost) and their intersecting variables into logistic regression respectively. The performance was evaluated using the C-index, with results showing comparable predictive accuracy across these models: RF (0.763), LASSO (0.766), XGBoost (0.764), and intersecting variables (0.763). Given the similar predictive performance and to balance model performance with parsimony, we ultimately selected the 11 intersection variables as the final predictors for inclusion in the logistic regression model. The multivariate logistic regression outcomes for the 11 variables are shown in Fig. 5 and Supplementary Fig. 1.
Multivariate Logistic Regression for Quantifying the Impact of Key Factors on Cardiopulmonary Function During the Pandemic. Abbreviations: OR, odds ratio; CI, confidence interval; BMI, body mass index; FVC, forced vital capacity; NT-proBNP, N-terminal pro-brain natriuretic peptide; HbA1c, glycated hemoglobin; Hb, hemoglobin; GAD-7, Generalized Anxiety Disorder Questionnaire-7; ACS, acute coronary syndrome; UA, Unstable Angina; STEMI, ST-segment elevation myocardial infarction; NSTEMI, Non-ST-segment elevation myocardial infarction.
During the pandemic, the males had a negative correlation of poor cardiopulmonary function than the females (OR = 0.37, 95% CI: 0.29–0.48). Smokers (OR = 1.38, 95%CI: 1.16–1.64) and those who had quit smoking (OR = 1.29, 95%CI: 1.04–1.60) face a higher risk compared to non-smokers. STEMI (OR = 2.72, 95%CI: 2.01–3.70) diagnoses were linked to a higher risk compared to UA. Patients with mild (OR = 1.21, 95%CI: 1.02–1.42), moderate (OR = 1.56, 95%CI:1.17–2.09) to severe (OR = 1.78, 95%CI: 1.06–3.06) GAD-7 levels also faced an increased risk versus those evaluated as normal. Considering potential reverse correlation, we conducted additional analyses modeling anxiety levels (GAD-7 score < 10 or > 10) as the dependent variable, with peak VO2/kg and Weber classification as independent variables. In the adjusted model (Supplementary Table 6), when compared with patients in Weber A, those in Weber C and Weber D were significantly associated with a higher risk of anxiety levels, and the adjusted OR (95% CI) were 1.54 (1.01–2.44) and 1.75 (1.01–3.09), respectively. Peak VO2/kg was negatively correlated with anxiety levels.
We additionally found that other positive correlation factors associated with suboptimal cardiopulmonary function for ACS patients after PCI were age (OR = 1.03, 95%CI: 1.02–1.04), HbA1c (OR = 1.25, 95%CI: 1.17–1.34), BMI (OR = 1.16, 95%CI:1.14–1.19), SYNTAX score (OR = 1.02, 95%CI: 1.01–1.03), NT-pro BNP (OR = 1.05, 95%CI:1.02–1.10). While, FVC (OR = 0.51, 95%CI: 0.45–0.58), Hb (OR = 0.98, 95%CI: 0.97-1.00) were negative correlation factors.
Discussion
The present study was the first to explore, within the context of implementing scientifically rigorous infectious disease management strategies11 the cardiopulmonary function disparities post-PCI between periods of COVID-19 pandemic and non-pandemic among patients with ACS. It evaluates the impact of the COVID-19 pandemic, as a significant public health event, on the postoperative cardiopulmonary function of ACS patients. Our findings indicate that during the pandemic, cardiopulmonary function declined compared to pre-pandemic levels, even in patients who had never been infected with the virus. Additionally, this research utilized machine learning algorithms to identify key factors influencing the Weber cardiopulmonary function classification during the pandemic. The present study offers a new perspective on understanding the effects of pandemics on cardiovascular treatment outcomes and highlights factors that need attention to improve patient prognoses in public health emergencies.
Cardiorespiratory Fitness (CRF) is a crucial indicator of health and prognosis, often serving as a vital sign of an individual’s overall well-being22. During the pandemic, participants showed notably lower values in Peak VO2/kg, Peak METs, Peak O2 Pulse, and AT O2 pulse compared to the pre-pandemic period, indicating a decline in cardiopulmonary endurance. This finding aligns with previous studies highlighting the potential negative effects of COVID-19 on cardiovascular health23. No universally accepted clinical threshold currently exists for peak oxygen uptake decline. Previous studies on exercise training in heart failure patients have often used a 6% decline as a reference. Heart failure patients have a lower baseline level of peak oxygen uptake, so the relative improvement ratio tends to be more significant with the same absolute increase. The HF-ACTION24 study showed that changes in peak VO2 of 0.6 mL/kg/min before and after rehabilitation were significantly associated with improved prognosis. Ugo Corrà et al. suggested that a 4% decline in peak VO2 in different subgroups could be considered indicative of deterioration25. In this study, the observed range of change in peak VO2 was 0.49–0.62 mL/kg/min (3–4%), consistent with previously reported ranges. Other studies have also demonstrated an association between changes in peak VO2 and cardiovascular risk. For example, Luc Vanhees et al. found that for every 1% increase in peak VO2 after CABG surgery, the risk of death decreased by 2%, indicating that even small changes in peak VO2 can influence cardiovascular risk26. The present study revealed that during the pandemic, patients’ peak VO2 declined by 3% and 4% compared to pre-pandemic and post-pandemic levels, respectively. This degree of change is sufficient to impact clinical outcomes in patients. What distinguishes this study, however, is that participants during the pandemic had not been infected with the SARS-CoV-2 virus. Our research suggests that, even without direct viral infection, declines in cardiopulmonary function occurred during the pandemic. This underscores that the impact of COVID-19 not limited to the objective outcome of viral infection, but also included psychological, cognitive, and behavioral changes—such as increased remote work, reduced outdoor activity27 and heightened psychosocial stress28—which can substantially affect recovery and treatment outcomes. Therefore, our study further emphasizes the importance of attending to the exercise rehabilitation processes of patients with ACS during the health crises.
By comparing clinical data of patients during the COVID-19 pandemic with data from before and after the pandemic, we found intriguing findings. Abnormal PHQ-9 scores rose significantly in during-pandemic patients, possibly due to increased stress and anxiety worsening mental health. Furthermore, this trend might may reflect concerns among patients and their families about the risk of contracting SARS-CoV-2 during medical visits, leading to a delay or reduction in their willingness to seek care29. A study published in JAMA Cardiology highlighted a negative correlation between the incidence of AMI and COVID-19 mortality, suggesting that changes in AMI incidence could be attributed to healthcare avoidance behaviors, a finding that aligns with our own perspective30. These results underscore the effects of the COVID-19 pandemic on patient cognition and behavior31.
Additionally, the present study showed that poor mental health was related to poor cardiopulmonary function and that lower exercise capacity (reflected by lower peak VO2 and higher Weber grade) was also associated with higher anxiety levels, highlighting the need to address mental health issues during the pandemic. Increased psychological stress, particularly anxiety, may stem from concerns about viral infection, social isolation, economic pressures, and fear of future uncertainty32. These psychological burdens may directly impact patients’ compliance with and motivation for rehabilitation activities, thereby hindering their cardiopulmonary recovery. The correlation between depressive states and cardiopulmonary function was less significant than that of anxiety, which may be related to the following reasons: patients with anxiety can self-regulate to adapt to the stress response brought by anxiety, which may be related to the fluctuation of stress hormone secretion, thereby affecting cardiopulmonary function. The physiological response of patients with depression may have reached a new equilibrium point, and the body’s response to stress has become numb or adapted, which may make the correlation with poor cardiopulmonary function less significant33,34. Therefore, future cardiac rehabilitation programs should integrate psychological health interventions to improve rehabilitation outcomes.
Although the global pandemic of the novel coronavirus has ended, the World Health Organization has issued an alert for “Disease X” - a hypothetical future potential pandemic pathogen35 highlighting the urgency of refining cardiovascular rehabilitation strategies in advance to meet such challenges. Especially for diseases requiring long-term rehabilitation, such as ACS patients after PCI surgery, ensuring the quality and continuity of cardiovascular disease long-term rehabilitation treatment during global health emergencies is crucial. This study provides a reference for this purpose.
The long-term impact of the pandemic requires sustained attention in future studies. Previous studies have found that people generally exhibit increased fatigue after the pandemic. The mechanism for fatigue requires investigation, with myostatin emerging as a key candidate pathway for future study. Myostatin, a regulatory factor secreted by muscle tissue, may play a key role in this process. Research by Mouisel et al. indicates that individuals lacking Myostatin exhibit greater muscle fatigue, decreased aerobic capacity, and increased anaerobic metabolism, specifically demonstrated by a decline in maximal oxygen uptake36,37. In a study of long-term care facility residents, Haritz found that non-frail individuals had higher serum Myostatin levels than frail individuals, and Myostatin levels were positively correlated with daily step counts and moderate physical activity38. However, during the pandemic, due to reduced outdoor activities, increased sedentary behavior, and prolonged bed rest, the frequency and intensity of exercise were significantly restricted, potentially leading to a decrease in Myostatin levels, thereby hindering its positive regulatory effect on muscles39. However, the role of Myostatin in muscle fatigue is still speculative. As a potential biomarker, Myostatin holds significant research value in assessing an individual’s aerobic capacity. In situations of long-term activity restriction, reducing Myostatin levels may serve as a potential method for alleviating skeletal muscle fatigue and promoting functional recovery.
Limitation
While the present study provides some information, it is not without limitations. The cross-sectional nature of the data limits our ability to establish causality. Meanwhile, the study’s findings may not be generalizable to all populations due to potential selection bias. Future research should focus on longitudinal studies to better understand the long-term effects of the pandemic on cardiopulmonary function and the effectiveness of various interventions. Given the inherent limitations of observational study designs in establishing causal inference, our clinical findings cannot definitively validate molecular pathways or exclude residual confounding, thereby requiring future experimental studies to determine the underlying mechanisms of these clinical observations.
Conclusions
The current study indicated (1) The current study identified adverse associations between the COVID-19 pandemic and cardiopulmonary function in patients with ACS following PCI, particularly linked to reduced peak oxygen uptake per kilogram. (2) Elder, female, higher BMI, higher SYNTAX score, increased NT-pro BNP, increased HbA1c, smoking, anxiety, and more severe ACS classification predicted worse CPET results.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in the electronic medical records system at the General Hospital of Northern Theater Command.
Abbreviations
- BMI:
-
body mass index
- FVC:
-
forced vital capacity
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- HbA1c:
-
glycated hemoglobin
- Hb:
-
hemoglobin
- GAD-7:
-
Generalized Anxiety Disorder Questionnaire-7
- ACS:
-
acute coronary syndrome
- hsCRP:
-
Hypersensitive C-reactive protein
- CK-MB:
-
creatine kinase-MB
- Glu:
-
Fasting serum glucose
- FEV1:
-
forced expiratory volume in one second
- PCI:
-
percutaneous coronary intervention
- VC:
-
maximum vital capacity
- TG:
-
triglyceride
References
Patel, U. et al. Early epidemiological indicators, outcomes, and interventions of COVID-19 pandemic: A systematic review. J. Glob Health. 10 (2), 020506 (2020).
Zuo, M. et al. Management strategies and outcomes of acute coronary syndrome (ACS) during Covid-19 pandemic. BMC Cardiovasc. Disord. 22 (1), 242 (2022).
Zeng, H. et al. A new coronavirus Estimation global score for predicting mortality during hospitalization in patients with COVID-19. Cardiol. Discov. 2 (2), 69–76 (2022).
Kaminsky, L. A. et al. Cardiorespiratory fitness and cardiovascular disease - The past, present, and future. Prog Cardiovasc. Dis. 62 (2), 86–93 (2019).
Glaab, T. & Taube, C. Practical guide to cardiopulmonary exercise testing in adults. Respir Res. 23 (1), 9 (2022).
Swank, A. M. et al. Modest increase in peak VO2 is related to better clinical outcomes in chronic heart failure patients: results from heart failure and a controlled trial to investigate outcomes of exercise training. Circ. Heart Fail. 5 (5), 579–585 (2012).
Harber, M. P. et al. Cardiorespiratory fitness as a vital sign of CVD risk in the COVID-19 era. Prog Cardiovasc. Dis. 76, 44–48 (2023).
Rajkomar, A., Dean, J. & Kohane, I. Machine learning in medicine. N Engl. J. Med. 380 (14), 1347–1358 (2019).
Haug, C. J. & Drazen, J. M. Artificial intelligence and machine learning in clinical medicine, 2023. N Engl. J. Med. 388 (13), 1201–1208 (2023).
Alahdab, F. et al. Development and validation of a machine learning model to predict myocardial blood flow and clinical outcomes from patients’ electrocardiograms. Cell. Rep. Med. 5 (10), 101746 (2024).
Cheng, Z. J. et al. Public health measures and the control of COVID-19 in China. Clin. Rev. Allergy Immunol. 64 (1), 1–16 (2023).
Fletcher, G. F. et al. Exercise standards for testing and training: a scientific statement from the American heart association. Circulation 128 (8), 873–934 (2013).
Clinical exercise testing. With reference to lung diseases: indications, standardization and interpretation strategies. ERS task force on standardization of clinical exercise testing. European respiratory society. Eur. Respir J. 10 (11), 2662–2689 (1997).
Guazzi, M. et al. EACPR/AHA scientific statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation 126 (18), 2261–2274 (2012).
Byrne, R. A. et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur. Heart J. 44 (38), 3720–3826 (2023).
Li, Y. & Han, Y. L. Interpretation of 2023 ESC guidelines for the management of acute coronary syndromes. Zhonghua Xin Xue Guan Bing Za Zhi. 51 (12), 1263–1267 (2023).
Weber, K. T., Kinasewitz, G. T., Janicki, J. S. & Fishman, A. P. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation 65 (6), 1213–1223 (1982).
Guazzi, M. et al. Revisiting and implementing the Weber and ventilatory functional classifications in heart failure by cardiopulmonary imaging phenotyping. J. Am. Heart Assoc. 10 (5), e018822 (2021).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166 (10), 1092–1097 (2006).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16 (9), 606–613 (2001).
Engebretsen, S. & Bohlin, J. Statistical predictions with Glmnet. Clin. Epigenetics. 11 (1), 123 (2019).
Ross, R. et al. Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign: A scientific statement from the American heart association. Circulation 134 (24), e653–e699 (2016).
Liu, F., Liu, F. & Wang, L. COVID-19 and cardiovascular diseases. J. Mol. Cell. Biol. 13 (3), 161–167 (2021).
Corrà, U., Mezzani, A., Bosimini, E. & Giannuzzi, P. Prognostic value of time-related changes of cardiopulmonary exercise testing indices in stable chronic heart failure: a pragmatic and operative scheme. Eur. J. Cardiovasc. Prev. Rehabil. 13 (2), 186–192 (2006).
O’Connor, C. M. et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301 (14), 1439–1450 (2009).
Vanhees, L., Fagard, R., Thijs, L. & Amery, A. Prognostic value of training-induced change in peak exercise capacity in patients with myocardial infarcts and patients with coronary bypass surgery. Am. J. Cardiol. 76 (14), 1014–1019 (1995).
Gao, W., Sanna, M., Chen, Y. H., Tsai, M. K. & Wen, C. P. Occupational sitting time, leisure physical activity, and All-Cause and cardiovascular disease mortality. JAMA Netw. Open. 7 (1), e2350680 (2024).
Qin, F. et al. Physical activity, screen time, and emotional Well-Being during the 2019 novel coronavirus outbreak in China. Int. J. Environ. Res. Public. Health. 17 (14), 5170 (2020).
Boyer, L. et al. The impact of hospital saturation on non-COVID-19 hospital mortality during the pandemic in france: a National population-based cohort study. BMC Public. Health. 24 (1), 1798 (2024).
Wilcock, A. D. et al. Factors underlying reduced hospitalizations for myocardial infarction during the COVID-19 pandemic. JAMA Cardiol. 9 (10), 914 (2024).
Gao, Y., Wang, Y., Chen, L., Xie, J. & Prieto-Alhambra, D. Hospitalization for COVID-19, other respiratory infections, and postacute Patient-Reported symptoms. JAMA Netw. Open. 7 (10), e2441615 (2024).
Luo, H. et al. Psychotropic drug prescribing before and during the COVID-19 pandemic among people with depressive and anxiety disorders: a multinational network study. Lancet Psychiatry. 11 (10), 807–817 (2024).
Ostrowska-Leśko, M. et al. Pathological changes and metabolic adaptation in the myocardium of rats in response to chronic variable mild stress. Int. J. Mol. Sci. 25 (11), 5899 (2024).
Elbau, I. G. et al. The brain’s hemodynamic response function rapidly changes under acute psychosocial stress in association with genetic and endocrine stress response markers. Proc. Natl. Acad. Sci. U S A. 115 (43), E10206–E10215 (2018).
Fei, Y., Huang, J. J. & Unveiling Disease, X. Strategies for tackling the new frontier of infectious diseases. Zoonoses 4, 980 (2024).
Mouisel, E. et al. Myostatin is a key mediator between energy metabolism and endurance capacity of skeletal muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 307 (4), R444–454 (2014).
Hjorth, M. et al. Myostatin in relation to physical activity and dysglycaemia and its effect on energy metabolism in human skeletal muscle cells. Acta Physiol. (Oxf). 217 (1), 45–60 (2016).
Arrieta, H. et al. Serum myostatin levels are higher in fitter, more active, and Non-Frail Long-Term nursing home residents and increase after a physical exercise intervention. Gerontology 65 (3), 229–239 (2019).
Caetano-Anollés, K., Mishra, S. & Rodriguez-Zas, S. L. Synergistic and antagonistic interplay between myostatin gene expression and physical activity levels on gene expression patterns in triceps brachii muscles of C57/BL6 mice. PLoS One. 10 (2), e0116828 (2015).
Funding
This research was funded by a grant from the LIAONING S&T Project [2022JH2/101500028].
Author information
Authors and Affiliations
Contributions
Yaling Han conceived the idea. Yaling Han and Quanyu Zhang designed the trial. Xingbo Mu performed the study and collected the data. Yi Zhang and Shengyi Wang checked the data. Xingbo Mu performed the data analysis. Yanchun Liang and Jian Zhang scrubbed data and maintained research data. Xingbo Mu and Sicheng Ning wrote the manuscript. Quanyu Zhang revised the paper. All authors reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mu, X., Ning, S., Zhang, Q. et al. Association between the COVID-19 pandemic and cardiopulmonary function in acute coronary syndrome patients without SARS-CoV-2 infection. Sci Rep 15, 30906 (2025). https://doi.org/10.1038/s41598-025-17016-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17016-y