Abstract
Superior capsule reconstruction (SCR) is established for irreparable massive rotator cuff tears (IMRCTs). Supraspinatus tendon reconstruction (STR), a novel technique restoring muscle anatomy, lacks comparative studies with SCR. To compare STR and SCR efficacy in shoulder function, ROM, and radiological outcomes for posterosuperior IMRCTs. This retrospective cohort study analyzed 59 patients (SCR: n = 16; STR: n = 43) treated between December 2019 and November 2023. Outcomes included isokinetic muscle strength, active ROM (forward flexion [FF], abduction [ABD], external rotation [ER], internal rotation [IR]), patient-reported scores (VAS, ASES, Constant, UCLA), and radiological measures (acromiohumeral distance [AHD], Sugaya score, Goutallier classification). Both groups demonstrated significant improvements in ROM, shoulder scores, and AHD postoperatively (P < 0.05). STR required shorter operative times (197.86 ± 32.88 vs. 291.25 ± 72.69 min, P < 0.01) and showed superior reductions in supraspinatus fat infiltration (Goutallier classification: P < 0.01) and greater gains in abduction (ΔABD: P = 0.021) and forward flexion strength (ΔFF: P < 0.01) compared to SCR. No differences were observed in VAS, ASES, or UCLA scores between groups (P > 0.05). Both techniques similarly improve shoulder function. STR demonstrates advantages in operative efficiency, muscle recovery, and mitigating fat infiltration, suggesting potential preference for posterosuperior IMRCTs.
Similar content being viewed by others
Introduction
Irreparable massive rotator cuff tears (IMRCTs) refer to conditions in which a massive rotator cuff tear cannot be surgically repaired, or the tendon-to-bone interface cannot be reconstructed with appropriate intensity1,2. Irreparable massive rotator cuff tears (IMRCTs) pose significant challenges in shoulder surgery, with posterosuperior tears being particularly debilitating3. Surgical options range from debridement to reverse arthroplasty4,5,6,7,8. but superior capsule reconstruction (SCR) has gained traction due to its biomechanical efficacy9,10,11, However, SCR does not address supraspinatus muscle dynamics, a gap targeted by the emerging supraspinatus tendon reconstruction (STR) technique (Fig. 1)12,13.
The superior stability of the glenohumeral joint is compromised in posterosuperior IMRCTs14. SCR strengthens passive stability by reconstructing the superior capsule, whereas STR restores dynamic stability by reconstructing the SSP tendon. Fascia lata autografts, with their low risk of allergic reactions and robust mechanical support, are commonly used in both techniques13,15 Biologically, SCR relies on graft-bone healing at the glenoid and rotator cuff footprint, while STR involves graft-muscle interface healing medially and graft-bone healing laterally16. Despite the distinct biomechanical and histological foundations of STR and SCR, no comparative studies have evaluated their clinical outcomes. This study compares STR and SCR in posterosuperior IMRCTs, hypothesizing that STR yields comparable or superior functional outcomes by restoring dynamic stability and muscle integrity.
Methods
Ethics and study design
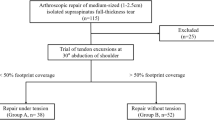
This study was conducted in accordance with the principles embodied in the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Southwest Hospital of Army Medical University, Chongqing, People’s Republic of China (approval no. KY2022126; approval date: October 11th, 2022) and the trial has been registered (No. ChiCTR2400094111). Written informed consent was obtained from all participants. This retrospective cohort study analyzed patients who underwent STR (n = 43) or SCR (n = 16) between December 2019 and November 2023. The data collected before surgery and 1 year postoperatively were analyzed. Improvements in shoulder function scores and active range of motion (ROM) were recorded. Changes in the acromiohumeral distance (AHD) were assessed via radiography, whereas repaired tendon retear and fat infiltration in the SSP muscle were evaluated using magnetic resonance imaging (MRI). Isokinetic muscle strength was used to evaluate SSP muscle strength in the STR group. The study design is illustrated in Fig. 2.
Patients
Shoulder joint peak torque was set as the primary outcome measure in this retrospective cohort study. The SCR group consisted of 16 patients with a mean degree of improvement of 0.81, with a standard deviation of 0.14. The STR group comprised 43 patients, with a mean degree of improvement of 0.97 and a standard deviation of 0.1. Based on our sample data, the power analysis calculated by PASS 2021 was 0.97894. The inclusion criteria included: (1) a torn rotator cuff tendon diagnosed as a posterosuperior MRCTs according to the California classification17; (2) a torn tendon that could not be repaired in the footprint area during arthroscopic surgery; (3) Hamada grade ≤ 3; (4) use of autologous fascia lata as the graft, and (5) follow-up of at least 1 year after surgery. The exclusion criteria were as follows: (1) combined with subscapularis tendon tear (Lafosse classification > grade 3); (2) severe medical diseases, including angiocardiopathy and endocrine diseases; (3) cervical diseases, cervical nerve palsy or axillary nerve palsy; (4) deltoid muscle dysfunction; and (5) a history of infection in the glenohumeral joint.
Surgical procedure
All surgeries were performed by the same surgeon (BHZ) at the same institution. Patients were placed under general anesthesia in the contralateral decubitus position. With cuff protection, the upper limb on the affected side was abducted to 30° and flexed at 20°. Conventional posterior, anterior, and anterolateral portals were selected. A 30° arthroscope (Smith & Nephew, Andover, MA, USA) was placed in the glenohumeral joint from the posterior portal and was then transferred to the subacromial space using the posterior approach to explore the degree of rotator cuff injury and the shape of the acromion. Subacromial debridement and decompression were performed through the lateral channels. The anterior, posterior, and medial rotator cuff stumps were completely released, and the tension for rotator cuff repair was evaluated using tissue-grasping forceps. If the rotator cuff stump could not be adequately restored with appropriate tension in the footprint area, STR or SCR was performed using autogenous fascia lata.
Harvesting the fascia graft
The width of the fascia lata was measured from the anterior to the posterior edge of the rotator cuff tendon lesion. For STR, the length of the fascia lata was determined by measuring the distance from the lateral edge of the greater tuberosity to the most medial spine of the scapula. For SCR, the length of the fascia lata was twice the length measured in the mediolateral direction from the superior edge of the glenoid to the lateral edge of the greater tuberosity. Starting approximately 2 cm proximal to the greater trochanter, a longitudinal incision was made along the lateral side of the femur to expose the fascia lata. Subsequently, the tensor fasciae lata was dissected and cut according to the previously measured length and width. For SCR surgery, the grafts were folded with a thickness ≥ 6 mm; while for STR surgery, the graft did not need to be folded, and was a natural thickness of 3–4 mm.
STR surgical procedure
The STR procedure followed established methods12. Two absorbable anchors (5.5 mm HEALIX ADVANCE) were placed medially on the rotator cuff footprint. Fascia lata grafts were attached with traction wires medially and laterally. A guide pin was inserted through the lateral portal, traversing the SSP muscle to the scapular spine’s medial edge. The fascia lata was tensioned medially and secured in a double-row configuration (VERSALOK for lateral row). An absorbable Lupine anchor fixed the medial graft under maximal tension. Residual infraspinatus tissue underwent posterior convergence before layered closure.
SCR surgical procedure
The SCR procedure followed established methods18. The fascia lata graft was fixed to the neck of the glenoid using two 5.5 mm diameter anchors at the 11 and 1 o’clock positions in the shoulder. Another two absorbable anchors were positioned along the medial line of the rotator cuff footprint. The suture from the anchors at the neck of the glenoid and the medial line of rotator cuff footprint was sewn in a mattress fashion to the medial and lateral of side of the fascial lata grafts, respectively. Then the graft was inserted directly through the anterolateral portal into the subacromial space. When the medial edge of the graft reached the superior glenoid, all sutures were tied. The lateral side of the fascia lata was attached to the rotator cuff footprint on the greater tuberosity using the compression double-row technique. The residual infraspinatus tissue was managed with posterior convergence in all patients after graft fixation. Subsequently, the incision was closed layer by layer to complete the operation.
Postoperative care and follow-up
Both STR and SCR group used the same rehabilitation protocols. Patients were recommended to use a 45° shoulder abduction brace for fixation for 6 weeks after surgery. Active exercises were allowed to strengthen the rotator cuff and scapular stabilizers 3 months after surgery. Shoulder function 1 year after surgery was collected and evaluated using the visual analog scale (VAS), American Shoulder and Elbow Surgeons (ASES), Constant, and University of California Los Angeles (UCLA) scores. Active shoulder ROM, including active forward flexion (FF), active abduction elevation (ABD), active external rotation (ER), and active internal rotation (IR), was also recorded19. The level of IR was graded using the cone of function, with levels ranging from C1 to S5 corresponding to grades 1 to 29, respectively. AHD and the Sugaya score were measured using computer-aided linear measurements (picture archiving and communication systems software, INFINITT; INFIN ITT Co) based on MRI images20,21. Fat infiltration of the SSP muscle was also evaluated using the modified grading system of Goutallier based on MRI images. In detail, an oblique sagittal MRI fat analysis and calculation technique was used (a 1.5-T magnetic resonance scanner, Magnetom Essenza; Siemens). All shoulder functions and radiological assessments were measured by two authors (J.W and BW.T.). When the results did not match, the average of the measurements was used.
Isokinetic muscle strength test
Patients were comfortably positioned in the seated position. A dynamometer was then securely attached to the patient’s arm on the side being tested to measure the isokinetic force. The patient’s elbow was flexed at approximately 90°, and their forearm was secured to the dynamometer with appropriate straps to ensure stability during the test. The isokinetic mode of the dynamometer was set at a predetermined speed of 60°/s to ensure standardized testing conditions. The patient was asked to perform maximal effort abduction movements. The dynamometer recorded the force generated by the patient during the abduction movement, providing quantitative data on muscle strength. Each patient performed three repetitions to obtain an average value.
Statistical analysis
All statistical analyses were performed using SPSS software (version 23.0; IBM Corp., Armonk, NY, USA). All statistics were collected, tabulated, and analyzed by an independent statistician. The normality of data distribution was verified using the Shapiro–Wilk test. The mean ± standard deviation represents data conforming to a normal distribution and the nonnormally distributed measurement data are represented by M (Q1, Q3). For data comparison, paired and independent t-tests were used for parametric quantitative variables, whereas the Wilcoxon signed-rank and Mann–Whitney tests were used for nonparametric quantitative variables. Qualitative variables were analyzed using the chi-squared test. Statistical significance was set at P < 0.05.
Results
Demographic parameters
The STR and SCR groups did not significantly differ with respect to sex, age, body mass index, Hamada grade, postoperative length of hospital stay (days), and preoperative AHD. However, the STR group had a shorter operation time than the SCR group (197.86 ± 32.88 min vs. 291.25 ± 72.69 min, P = 0.000) (Table 1).
All patients had good healing of incisions, and no patients experienced a ruptured rotator cuff during follow-up. One patient (SCR group) developed a muscle hernia in their thigh without significant pain or discomfort. Three patients (1 in SCR group and 2 in STR group) experienced numbness in the forearms postoperatively, but these symptoms resolved within 3–5 days after oral administration of mecobalamin.
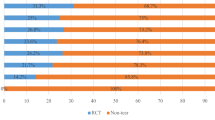
Active ROM parameters
Both the STR and SCR groups showed significant improvements in ROM 1 year postoperatively compared with baseline. In the STR group, FF improved from 106.86 ± 45.46 to 165 [150, 180], ABD from 125 [70, 160] to 165 [140, 180], ER from 40 [15, 45] to 60 [45, 60], and IR from 22 [19, 24] to 19 [19, 20]. In the SCR group, FF improved from 82.5 [52.5, 117.5] to 162.5 [146.25, 168.75], ABD from 84.38 ± 30.05 to 160 [151.25, 170], ER from 29.69 ± 11.61 to 52.5 [45, 60], and IR from 24 [22, 24] to 20 [18, 21.75]. However, the changes in postoperative ROM between the SCR and STR groups were equal (Table 2).
Evaluation of the shoulder function scores
Both the STR and SCR groups showed significant improvements in shoulder function scores 1 year postoperatively compared with baseline. In the STR group, VAS score improved from 5 [4, 6] to 2 [1, 2], ASES score from 51.4 ± 17.82 to 90 [88, 93], Constant shoulder score from 43 [30, 47] to 95 [90, 96], and UCLA shoulder score from 15 [13, 18] to 30 [32, 34]. In the SCR group, VAS score improved from 5 [4, 5.75] to 1.5 [1, 2], ASES score from 45.06 ± 11.12 to 91.5 [89.25, 93.5], Constant shoulder score from 37.88 ± 9.27 to 86.25 [91, 94.5], and UCLA shoulder score from 13.13 ± 2.63 to 31.5 [29, 32]. However, there was no differences in the magnitude of postoperative shoulder function changes between the SCR and STR groups (Table 3).
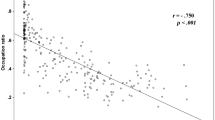
Radiological assessments
The AHD (SCR: 6.70 ± 1.61 to 8.41 ± 1.81; STR: 6.99 ± 2.19 to 8.72 ± 1.59) and Sugaya classification (SCR: 4 [4, 5] to 2 [1, 3]; STR: 4 [4, 5] to 2 [1, 2]) significantly increased 1 year postoperatively in both groups, compared with preoperative scans (P = 0.000). However, only the STR group showed improvement in Goutallier classification (2 [2, 3] to 2 [1, 2]), while there was no improvement in the SCR group postoperatively. There was no difference in magnitude of changes the AHD (1.71 ± 1.53 mm vs. 1.73 ± 2.04 mm, P = 0.973) or Sugaya classification (−3 [−3, −1.25] vs. −3 [−3, −2], P = 0.056) between the STR and SCR groups (Table 4; Fig. 3). However, the STR group achieved a higher improvement rate in Goutallier classification (−1 [−2, 0] vs. 0.25 ± 1.13) (Table 4).
Comparison of shoulder ABD and FF muscle strength
The results of the isokinetic muscle strength test indicated that both the STR and SCR groups achieved significant improvements after surgery, (P < 0.05). However, the STR group had greater ABD (P = 0.021) and FF (P = 0.00) muscle strength compared to the SCR group (Table 5).
Discussion
The present study demonstrated that STR achieved better clinical outcomes, reduced fat infiltration in the SSP muscle, and improved ABD and FF muscle strength at 1 year postoperatively compared to those of SCR.
Both STR and SCR resulted in significant improvements in shoulder function, including active ROM and shoulder function scores. However, no significant differences in the degree of improvements in shoulder function scores or AHD were observed between the two groups. Radiographic examination results showed that the superior transition of the humeral head was corrected in all patients in the STR and SCR groups. This might indicate that the improvement in outcomes depends on the restoration of mechanical stability. Additionally, the posterosuperior rotator cuff has a synergistic effect with the deltoid muscle during shoulder active abduction elevation and forward flexion. Although the muscle strength of both groups 1 year after surgery remained weaker compared to the healthy side, the improvement rate in the STR group was significantly higher than that in the SCR group. Mechanically, shoulder instability due to IMRCTs could be rebalanced by strengthening the dynamic stability mechanism via restoration of the SSP muscle dynamics in STR or strengthening the passive stability mechanism via reconstruction of the shoulder capsule in SCR9,12,22. Overall, both STR and SCR could mechanically achieve shoulder stability after surgery, although they are based on different stabilization tactics.
The muscle contraction force for the shoulder ROM depends on muscle quality. Fat infiltration in the SSP muscle is considered a predictor of poor postoperative shoulder function and an independent factor for contract strength3,23,24,25,26. The loss of mechanical stretching due to IMRCTs plays an initial role in fat infiltration in the SSP muscle. Therefore, fat infiltration induced by a rotator cuff tendon tear can almost be stopped after successful arthroscopic repair27. SSP muscle contraction strength tends to increase postoperatively and is characterized by type I tendon integrity28. In this study, STR restored the anatomy of the SSP muscle and reduced fat infiltration in the SSP muscle, whereas SCR did not. These two factors may increase the shoulder abduction muscle force. About cost-effectiveness analysis, the STR technique shows potential cost advantages, requiring fewer anchors and shorter OR time. The combined functional improvement and reduced revision rates suggest STR may offer better long-term cost-utility for healthcare systems. STR expands the indications for graft reconstruction, particularly in cases of posterosuperior IMRCTs with severe fatty infiltration in the supraspinatus muscle. In a word, STR offers the dual advantages of restoring supraspinatus muscle force and broader clinical applicability compared to SCR.
Fat infiltration induced by a rotator cuff tendon tear is also influenced by several factors such as tendon-derived stem cells and biological factors, in addition to mechanical force. Stem cells can differentiate into adipocytes and form fat infiltrates in the SSP muscle. Endogenous fibro-adipogenic progenitor cells are present within the rotator cuff and are likely to be sources of fat infiltration29. Rotator cuff-derived satellite cells can also be induced to differentiate into adipocytes instead of myogenic cells, increasing adipogenesis. However, the transplantation of autologous satellite cells from other muscles that are less prone to fat infiltration may also improve clinical outcomes30. In addition, fat infiltration was found to be associated with increased expression of inflammatory cytokines31,32,33,34 and mitochondrial dysfunction35, and fatty acid binding protein 4 inhibitors have been used to reverse the fat infiltration in the SSP muscle36. In this study, STR decreased postoperative fat infiltration in the SSP muscle, whereas no improvement was observed in the SCR group. Fascia lata autografts have been shown to revascularize 6 months postoperatively after good fascia lata-bone interface healing37. Therefore, fascial muscle interface healing might change the microenvironment of the SSP muscle and inhibit adipocyte differentiation. Overall, STR reversed the fat infiltration in the SSP muscle after restoration of mechanical stretching, while SCR delayed the deterioration of fat infiltration in the SSP muscle.
This study has several limitations. First, this was a retrospective cohort study, which may have introduced bias. Second, we did not collect preoperative isokinetic muscle strength data for the SCR group. However, we compared the operated side 1 year postoperatively with the healthy side in both the STR and SCR groups. Future randomized trials should validate these findings and the molecular mechanisms underlying the reduction in fat infiltration after STR.
Conclusion
STR is a viable alternative to SCR for posterosuperior IMRCTs, offering comparable functional outcomes with added benefits in muscle integrity and operative efficiency.
Data availability
The data are available from the corresponding author on reasonable request.
References
Oh, J. H., Park, M. S. & Rhee, S. M. Treatment strategy for irreparable rotator cuff tears. Clin. Orthop. Surg. 10 (2), 119–134. https://doi.org/10.4055/cios.2018.10.2.119 (2018).
Castricini, R., De Benedetto, M., Gervasi, E. & Castagna, A. Irreparable rotator cuff tears: a novel classification system. Musculoskelet. Surg. 98 (1), 49–53. https://doi.org/10.1007/s12306-014-0320-5 (2015).
Yamamoto, A. et al. Prevalence and risk factors of a rotator cuff tear in the general population. J. Shoulder Elb. Surg. 19 (1), 116–120. https://doi.org/10.1016/j.jse.2009.04.006 (2019).
Mirzaee, F., Aslani, M. A., Zafarani, Z. & Aslani, H. Treatment of massive irreparable rotator cuff tear with arthroscopic subacromial bursectomy, biceps tenotomy, and tuberoplasty. Arch. Bone Jt. Surg. 7 (3), 263–268 (2019).
Davies, A., Singh, P., Reilly, P., Sabharwal, S. & Malhas, A. Superior capsule reconstruction, partial cuff repair, graft interposition, arthroscopic debridement or balloon spacers for large and massive irreparable rotator cuff tears: a systematic review and meta-analysis. J. Orthop. Surg. Res. 17 (1), 552. https://doi.org/10.1186/s13018-022-03411-y (2022).
Thangarajah, T., Tsuchiya, S., Lukenchuk, J. & Lo, I. K. Arthroscopic revision rotator cuff repair of large and massive retears using an interpositional bridging dermal allograft. JSES Int. 6 (4), 643–648. https://doi.org/10.1016/j.jseint.2022.02.010 (2022).
Cartucho, A. Tendon transfers for massive rotator cuff tears. EFORT Open. Rev. 7 (6), 404–413. https://doi.org/10.1530/EOR-22-0023 (2022).
Preuss, F. R., Day, H. K., Peebles, A. M., Mologne, M. S. & Provencher, M. T. Reverse total shoulder arthroplasty for treatment of massive, irreparable rotator cuff tear. Arthrosc. Tech. 11 (6), e1133–e1139. https://doi.org/10.1016/j.eats.2022.02.022 (2022).
Mihata, T., McGarry, M. H., Pirolo, J. M., Kinoshita, M. & Lee, T. Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a Biomechanical cadaveric study. Am. J. Sports Med. 40 (10), 2248–2255. https://doi.org/10.1177/0363546512456195 (2012).
Burkhart, S. S. Superior capsule reconstruction. Instr Course Lect. 67, 433–438 (2018).
Mihata, T. et al. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears: comparison of clinical outcomes with and without subscapularis tear. Am. J. Sports Med. 48 (14), 3429–3438. https://doi.org/10.1177/0363546520965993 (2020).
Ma, L. et al. Supraspinatus tendon reconstruction using fascia Lata autograft for irreparable posterosuperior massive rotator cuff tears. Arthrosc. Tech. 12 (5), e629–e634. https://doi.org/10.1016/j.eats.2022.12.019 (2023).
Liao, Y., Zhou, Z., Wang, J., Li, H. & Zhou, B. Fascia Lata autografts achieve interface healing with the supraspinatus muscle histologically and mechanically in a rat supraspinatus tendon reconstruction model for massive irreparable rotator cuff tears. Arthroscopy 40 (11), 2655–2666. https://doi.org/10.1016/j.arthro.2024.02.048 (2024).
Adams, C. R., DeMartino, A. M., Rego, G., Denard, P. J. & Burkhart, S. S. The rotator cuff and the superior capsule. Why We Need both Arthrosc. 32 (12), 2628–2637. https://doi.org/10.1016/j.arthro.2016.08.011 (2016).
Wong, I., Burns, J. & Snyder, S. Arthroscopic graftjacket repair of rotator cuff tears. J. Shoulder Elb. Surg. 19 (2 Suppl), 104–109. https://doi.org/10.1016/j.jse.2009.12.017 (2010).
Liao, Y. et al. Supraspinatus tendon reconstruction versus the bridging technique in a rat model: histological, biomechanical, and functional outcomes. Am. J. Sports Med. 52 (10), 2628–2638. https://doi.org/10.1177/03635465241264805 (2024).
Pandey, V. & Jaap Willems, W. Rotator cuff tear: A detailed update. Asia Pac. J. Sports Med. Arthrosc. Rehabil Technol. 2, 1–14. https://doi.org/10.1016/j.asmart.2014.11.003 (2015).
Mihata, T. et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 29 (3), 459–470. https://doi.org/10.1016/j.arthro.2012.10.022 (2013).
Li, H. et al. Dynamic superior capsular reconstruction for irreparable massive rotator cuff tears: histologic analysis in a rat model and Short-term clinical evaluation. Am. J. Sports Med. 51 (5), 1255–1266. https://doi.org/10.1177/03635465231156619 (2023).
Li, H. et al. The short-term effectiveness of superior capsular reconstruction using autologous fascia Lata graft for irreparable massive rotator cuff tears (in Chinese). Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 35 (11), 1427–1433. https://doi.org/10.7507/1002-1892.202104003 (2021).
Sugaya, H., Maeda, K., Matsuki, K. & Moriishi, J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy 21 (11), 1307–1316. https://doi.org/10.1016/j.arthro.2005.08.011 (2005).
Liao, Y-T., Zhou, B-H. & Mihata, T. Superior capsule reconstruction: anatomy, biomechanics, indications, and graft treatment. Chin. Med. J. (Engl). 134 (23), 2847–2849. https://doi.org/10.1097/CM9.0000000000001849 (2021).
Goutallier, D., Postel, J-M., Gleyze, P., Leguilloux, P. & Driessche, S. V. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J. Shoulder Elb. Surg. 12 (6), 550–554. https://doi.org/10.1016/s1058-2746(03)00211-8 (2023).
Goutallier, D., Postel, J-M., Radier, C., Bernageau, J. & Zilber, S. Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J. Shoulder Elb. Surg. 18 (4), 521–528. https://doi.org/10.1016/j.jse.2008.11.006 (2009).
Hamano, N. et al. Does successful rotator cuff repair improve muscle atrophy and fatty infiltration of the rotator cuff? A retrospective magnetic resonance imaging study performed shortly after surgery as a reference. J. Shoulder Elb. Surg. 26, 967–974. https://doi.org/10.1016/j.jse.2016.10.016 (2017).
Yu, X-K. et al. The correlation between types of posterior upper rotator cuff tears and intramuscular fat infiltration based on magnetic resonance imaging: A retrospective observational study. Front. Bioeng. Biotechnol. 10, 859174. https://doi.org/10.3389/fbioe.2022.859174 (2022).
Wieser, K. et al. Changes of supraspinatus muscle volume and fat fraction after successful or failed arthroscopic rotator cuff repair. Am. J. Sports Med. 47 (13), 3080–3088. https://doi.org/10.1177/0363546519876289 (2019).
Yuri, T. et al. Influence of fat infiltration, tear size, and post-operative tendon integrity on muscle contractility of repaired supraspinatus muscle. Eur. J. Orthop. Surg. Traumatol. 32 (5), 837–843. https://doi.org/10.1007/s00590-021-03020-1 (2022).
Feeley, B. T. et al. Human rotator cuff tears have an endogenous, inducible stem cell source capable of improving muscle quality and function after rotator cuff repair. Am. J. Sports Med. 48 (11), 2660–2668. https://doi.org/10.1177/0363546520935855 (2020).
Schubert, M. F., Noah, A. C., Bedi, A., Gumucio, J. P. & Mendias, C. L. Reduced myogenic and increased adipogenic differentiation capacity of rotator cuff muscle stem cells. J. Bone Joint Surg. Am. 101 (3), 228–238. https://doi.org/10.2106/JBJS.18.00509 (2019).
Cipollaro, L., Sahemey, R., Oliva, F. & Maffulli, N. Immunohistochemical features of rotator cuff tendinopathy. Br. Med. Bull. 130 (1), 105–123. https://doi.org/10.1093/bmb/ldz016 (2019).
Yoon, J. P., Park, S-J., Kim, D-H. & Chung, S. W. Metformin increases the expression of Proinflammatory cytokines and inhibits supraspinatus fatty infiltration. J. Orthop. Surg. Res. 18 (1), 674. https://doi.org/10.1186/s13018-023-04163-z (2023).
Lee, Y-S., Kim, J-Y., Kim, K. I., Ki, S-Y. & Chung, S. W. Effect of fatty Acid-Binding protein 4 Inhibition on rotator cuff muscle quality: histological, biomechanical, and biomolecular analysis. Am. J. Sports Med. 47 (13), 3089–3099. https://doi.org/10.1177/0363546519873856 (2019).
Shirasawa, H. et al. Retinoic acid receptor agonists suppress muscle fatty infiltration in mice. Am. J. Sports Med. 49 (2), 332–339. https://doi.org/10.1177/0363546520984122 (2021).
Gumucio, J. P. et al. Reduced mitochondrial lipid oxidation leads to fat accumulation in myosteatosis. FASEB J. 33 (7), 7863–7881. https://doi.org/10.1096/fj.201802457RR (2019).
Lee, C. et al. Beige faps transplantation improves muscle quality and shoulder function after massive rotator cuff tears. J. Orthop. Res. 38 (5), 1159–1166. https://doi.org/10.1002/jor.24558 (2020).
Liao, Y-T. et al. Revascularization character of autologous fascia Lata graft following shoulder superior capsule reconstruction by enhanced magnetic resonance imaging. J. Orthop. Surg. Res. 17 (1), 485. https://doi.org/10.1186/s13018-022-03375-z (2022).
Acknowledgements
Chongqing Natural Science Fund (2023NSCQ‑MS‑X2660); Innovation Talents Support Program of PLA′s Ground Force, 2024IITZDB05.
Author information
Authors and Affiliations
Contributions
JW, ANY, FCY, and BWT finished the follow-up and collected the clinical dada. CKZ, GZ and ZYW joined the operation as an assistant. ZYW and CKZ drafted the initial manuscript. JW performed the Statistical analysis. BHZ designed the experiment, perform the surgery, analyzed the data, and reviewed manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Z., Zhang, C., Wang, J. et al. Comparative outcomes of supraspinatus tendon reconstruction and superior capsule reconstruction for massive irreparable posterosuperior rotator cuff tears. Sci Rep 15, 31322 (2025). https://doi.org/10.1038/s41598-025-17198-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17198-5