Abstract
Low APGAR scores are the cause of 13.6% of new born morbidity and mortality. Even though much has been done, still the levels of birth asphyxia and neonatal mortality in Ethiopia are significantly high. This study aimed to assess determinants of low fifth-minute APGAR scores among singleton new born babies. An institution-based unmatched case-control study was conducted among 426 neonates. Cases and controls were selected by systematic random sampling. Bivariable and multivariable logistic regression analyses were employed. Association was assessed by adjusted odd ratio with 95% confidence. The study found that preterm birth (AOR: 4.29; 95% CI 1.91, 9.65), lack of antenatal care (AOR: 4.32; 95% CI 1.78, 10.47), instrumental delivery (AOR: 2.75; 95% CI 1.34, 5.66), meconium-stained amniotic fluid (AOR: 2.15; 95% CI 1.16, 3.98), anemia during labour (AOR: 2.99; 95% CI 1.27, 7.05), and maternal WBC ≥ 15,000/µL (AOR: 3.13; 95% CI 1.46, 6.67)were associated with low fifth-minute Apgar scores. Low fifth-minute Apgar scores are significantly associated with preterm delivery, lack of antenatal care, instrumental births, meconium-stained amniotic fluid, maternal anemia, and elevated maternal white-blood-cell counts. Strengthening antenatal services and improving obstetric practice can help reduce these risks.
Similar content being viewed by others
Introduction
APGAR score is a general and immediate assessment of newborn health used right after birth1. The APGAR score determines if a baby needs extra care or emergency help when given at birth and the fifth minute1,2. This recording method allows for consistent assessment of new-borns immediately after delivery3.
The fifth-minute APGAR score can evaluate how the baby responded to any prior resuscitation attempts. It includes five components: activity level (muscle tone), pulse rate, grimace reflexes, appearance (color), and respiration, each scored from 0 to 2, for a maximum total of ten points. Scores are recorded at the first and fifth minutes for all newborns, with 7–10 considered normal. If the score is below seven, assessments will continue every five minutes for up to 20 min1.
A low APGAR score can exacerbate severe cases of birth asphyxia, potentially leading to significant multiorgan impairment in new-borns. This may result in brain damage, lung dysfunction, cardiomyopathy, renal failure, hepatic issues, and necrotizing enter colitis4,5,6.
A low APGAR score at the fifth minute correlates with a rise in neonatal mortality7,8. In addition, a low APGAR score at the fifth minute correlates with future developmental and mental complications9.
The Apgar score is affected by many factors; including gestational age, maternal socio-demographic, maternal disease, injury, obstetric, and gynaecologic conditions10,11,12. The factors of the low fifth-minute APGAR score are different in a variety of areas in Ethiopia13,14, . Therefore, this study aimed to address the discrepancies in research concerning the factors contributing to low fifth-minute APGAR scores among singleton new-borns at public hospitals in the North Shoe Zone, Amhara Regional State, Ethiopia, in 2022.Consequently, the study focused on identifying the determinants of low fifth-minute APGAR scores.
Methods
Study design, period, and setting
An institution-based unmatched case-control study was employed in North Shoa Zone public hospitals from June 6 to July 14, 2022. This study was conducted in governmental hospitals in the North Shoa Zone, located within the Amhara regional state on the Ethiopian. Twelve hospitals, including two private and ten public (comprising seven primaries, two general, and one comprehensive specialised hospital), were included in the study.
Population
Study population
The study population for the cases included all singleton live new-borns delivered at public hospitals in the North Shoa Zone during the study period with a fifth-minute Apgar score below seven, regardless of the delivery method. The controls consisted of all singleton live new-borns delivered at the same hospitals during the study period with a normal fifth-minute Apgar score (≥ 7), also irrespective of the mode of delivery.
Eligibility criteria
Inclusion criteria for cases included all singleton live births delivered after viability (≥ 28 weeks of gestational age) with an APGAR score of less than seven in the fifth minute in the North Shoa Zone public hospitals during the study period. For controls, inclusion criteria comprised all singleton live births delivered after viability with an APGAR score of seven and above (≥ 7) during the same period. Exclusion criteria for both cases and controls included unknown gestational age and gross congenital anomalies incompatible with life, such as anencephaly, severe hydrocephalus, and Gastroschisis.
Sample size determination
We conducted sample size calculation for the unmatched case-control study using the formula for two population proportions, with a 1:2 ratio of cases to controls, a 95% confidence level, and 80% power. Utilizing the largest sample size reported in the literature, which accounted for the proportion of no antenatal care contacts among cases (8.2%) and controls (3.7%), yielded a sample size of 426 after incorporating a 5% non-response rate15. Thus, adjusting for the non-response rate, the final sample size was 426 (comprising 142 cases and 284 controls).
Sampling technique and procedure
Ten public hospitals in the North Shoa Zone were included in the study, with samples allocated proportionally based on the number of delivery services and units at each hospital, as per their annual reports. Mothers of infants with low fifth-minute APGAR scores (< 7) were invited to participate, while mothers of infants with normal APGAR scores (≥ 7) served as controls. Cases and controls were chosen using a systematic random sampling technique from the labour ward.
Data collection tool and quality control
Data collection was done by using structured, interviewer-administered questionnaires and checklists that were developed under literature and WHO guidelines [17–19]. Three Trained midwives conducted face-to-face interviews with mothers within 24 h post-delivery and reviewed relevant medical records. Prior to data collection, the questionnaire underwent rigorous review and translation to Amharic, followed by back-translation to verify language consistency. A pre-test was done on 5% of the population. One day training was given for data collectors and supervisors.
Study variables
Dependent variable: the low fifth-minute APGAR score.
Independent variables:
Socio-demographic factors.
Obstetric and gynaecologic factors.
Fetal and new-born-related variables.
Medical illness-related variables.
Operational definition
Low fifth-minute Apgar score: A new-born that delivered with an APGAR score of less than seven five minutes after delivery1.
Controls: When the new-borns has an APGAR score of ≥ 7 in the fifth minute after delivery.
Cases: New-borns with an APGAR score of less than seven based on the Apgar score checklist that was summed up by trained data collectors at the fifth minute after delivery1.
Data Processing and Analysis: The collected data were entered, cleaned and coded by Epi Data version 4.6. Analysis was conducted using STATA version 14.0. Multicollinearity tests ensured the reliability of findings, with all variance inflation factors being < 5. The model goodness of fit was assessed with the Hosmer-Lemeshow test. Variables with a p-value < 0.25 in Bivariable logistic regression were included in the multivariable logistic regression model. Statistical significance in the final model was set at a p-value < 0.05.
Results
Maternal socio-demographic characteristics
The study involved 426 women, comprising 142 cases and 284 controls, with a response rate of 100%. The mean age of participants was 28.2 years (SD: ±6.1). Most of both cases and controls were aged between 20 and 35 years. Regarding residence, more than half of cases (53.5%) and controls (48.6%) were rural residents. The majority of participants were married, and housewife was the primary occupation for a substantial proportion of both cases (40.8%) and controls (44.7%). In terms of educational level, a similar percentage of cases (31.0%) and controls (28.2%) had completed primary education.
Distribution of APGAR score at the fifth minute
At the fifth minute, 12 (8.45%) of the cases had an APGAR score of three, whereas 32 (11.27%) of the controls had a score of ten.
New-born characteristics of the study
More than half of the newborns in both the case group Were female 53.5% in the case group and 47.5% in the control group.
Preterm births were more prevalent among cases (23.9%) compared to controls (6.0%), and low birth weight was more common in cases (30.3%) than controls (13.0%) (Table 1).
Obstetrics and gynecologic characteristics of the study participants
The majority of mothers, comprising 122 (85.9%) of the cases and 273 (96.1%) of the controls, received at least one ANC service during their pregnancy for the current newborn. Additionally, over half of the women who received ANC services—67 (54.9%) of the cases and 155 (56.8%) of the controls attended these services more than three times (Fig. 1).
Among the participants, nearly half of the cases (69 or 48.6%) and 111 (39.1%) of the controls were Prmipara. Among the mothers in the study, 7 (4.9%) of the cases and 8 (2.8%) of the controls were diagnosed with antepartum haemorrhage during the current pregnancy. The study also found that pregnancy-induced hypertension was present in 25 (17.6%) of the cases and 31 (10.9%) of the controls. Meconium-stained amniotic fluid was observed in 35 (24.6%) of the cases and 39 (13.7%) of the controls. Additionally, over 20% of the cases (29 or 20.4%) and 34 (12.0%) of the controls reported a history of abortion or pregnancy loss before 28 weeks of gestation. Among these, 7 (24.1%) of the cases and 5 (14.7%) of the controls had a history of two or more abortions (Table 2).
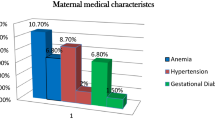
Medical illness history characteristics of the mothers
Among the total participants, 25 mothers in the case group (17.6%) and 12 mothers in the control group (4.2%) were diagnosed with anemia during the current labour, indicating a significant disparity in anemia prevalence between the cases and controls. Concerning chronic illness history, 11 cases (7.7%) and 14 controls (4.9%) were diagnosed with at least one maternal chronic illness, suggesting slightly higher prevalence among cases compared to controls. Additionally, a significant proportion of newborns, specifically 35 cases (24.6%) and 16 controls (5.6%), were born from mothers who developed maternal leukocytosis (white blood cells ≥ 15*10^3/µL), indicating a potentially higher risk associated with maternal leukocytosis in cases compared to controls.
Determinant factors associated with low fifth-minute APGAR score
The bivariable logistic regression analyses revealed that gestational age at birth, fetal presentation at birth, fetal birth weight, parity of the mother, antenatal visit for the current pregnancy, mode of delivery, the prolonged second stage of labor, meconium-stained liquor, augmentation with oxytocin, abortion history of the mother, anemia for the current labor, and presence of leukocytosis for the current labor were statistically significant with a LAS at fifth minute at p-value ≤ 0.25.
The results of the multiple model analysis showed that newborns with preterm (< 37 weeks of gestation) were 4.29 times more likely to develop a low Apgar score at fifth minutes than newborns delivered with ≥ 37 weeks of gestation (AOR: 4.29; 95% CI 1.91, 9.65). Mothers who had no antenatal care visit were 4.3 times more likely to have a low Apgar score infant at the fifth minute as compared to mothers who had antenatal care visit (AOR: 4.32; 95% CI 1.78, 10.47). The likelihood of developing a low Apgar score among neonates born with meconium-stained amniotic fluid was approximately two-fold higher than compared to those born without meconium-stained (AOR: 2.15; 95% CI 1.16, 3.98). Moreover, the fifth-minute low Apgar score was about 2.7 times higher among the mothers who gave birth through instrumental delivery than mothers who gave birth through spontaneous vaginal delivery (AOR: 2.75; 95% CI 1.34, 5.66).
The odds of new-borns having a low Apgar score were three times higher among those born to anemic mothers compared to non-anemic mothers (AOR: 2.99; 95% CI 1.27, 7.05). Additionally, the likelihood of a low Apgar score was significantly higher among women who developed leukocytosis (maternal WBC ≥ 15,000/µL) during labour. The data indicated that mothers with a white blood cell count of ≥ 15,000/µL during delivery were three times more likely to have a newborn with a low Apgar score compared to those with a white blood cell count of less than 15,000/µL (AOR: 3.13; 95% CI 1.46, 6.67) (Table 3).
Discussion
In this study being preterm (< 37weeks), no antenatal care visit, having instrumental delivery, meconium-stained liquor, anemia for the current labor, and presence of leukocytosis for the current labor were found to be significant determinants of low fifth minute APGAR score of the newborn. According to this study, premature newborns (< 37 weeks gestation) had a 4.2 times higher risk of having a low Apgar score at the fifth minute compared to newborns born at ≥ 37 weeks gestation. In preterm babies, an immature respiratory system could be the reason for this. Without surfactant, a premature baby’s lungs can’t expand and contract normally; this increases their risk for respiratory distress syndrome and may be hypoxic16. In contrast, this result was not supported by studies in Wolaita Sodo, Arba Minch, Hawassa, and Gonder13,17,18,19. The possible reason might be the previous studies were conducted in a single city hospital, but the current study was conducted in a wide study area that has more chance to get more findings. When the study area is wide, the probability of getting findings might be increased.
Newborns who delivered from mothers who had no antenatal care visit were 4.3 times more likely to have low Apgar score at the fifth minute as compared to newborns who delivered from mothers who had antenatal care visits. This was consistent with a study in Cameron and Hawassa17,20. This could be because antenatal care follow-up is used to create awareness about birth preparedness and readiness, and also it is the time for counselling for danger signs of pregnancy. Early identifying of danger signs and receiving appropriate maternal care are basic elements in maternal and neonatal health status. In addition, mothers who had no antenatal care visits will not be screened for danger signs and comorbidity problems21. However the result of this study was inconsistent with studies in Jima, Wolaita Sodo, and Debre Tabor University hospitals11,14,19, it might be because of the methodological difference, and the studies (Jima, Wolaita Sodo, and Debre Tabor) were conducted in higher-level hospitals only, but the current study included district hospitals that have more mothers those lacks ANC follow-up in a rural residence.
According to the recent study, newborns born with meconium-stained amniotic fluid had double the chance of having low Apgar scores compared to those without. This finding aligns with studies conducted in Australia, Maichew, Arba Minch, Debre Tabor, and Gonder14,18,19,22,23. This might bemeconium-stained amniotic fluid often indicates fetal distress, which can lead to compromised oxygen delivery and result in lower Apgar scores at birth.
A newborn that experiences meconium aspiration syndrome has an Apgar score of seven or less after about one to five minutes after birth24. However, the result is not supported by studies in Hawassa and Jima hospitals showed that meconium-stained liquor was not a significant factor for low Apgar score at fifth minutes11,17. This might be because of the number of health facilities included in the studies (Jima and Hawassa), The two studies were conducted in teaching hospitals, which might have more professional diversity for early detection and management.
In this study, new-borns delivered by mothers who had undergone instrumental delivery were 2.7 times more likely to have a low fifth-minute Apgar score compared to those delivered by mothers who had undergone spontaneous vaginal delivery. This finding was supported by studies conducted in Australia22 and Ghana25. This may be because a low Apgar score is a known complication of instrumental delivery. Neonatal complications such as fetal acidosis, cerebral trauma, hemorrhage, and brachial plexus injury can occur, especially in cases of shoulder dystocia, all of which can contribute to a low fifth-minute Apgar score and prolonged recovery26. In contrast, the studies in Brazil27, Gonder13, Debre Tabor14, and Jima11 did not support this finding, the possible reason might be the difference in study design, and study period. In addition, the sample size for the current study was comparatively larger than studies in Gonder, Debre Tabor, and Jima; when the sample size is larger the chance of including case finding might be increased.
In this study, neonates who had delivered from anemic mothers had nearly three times higher odds of having a low Apgar score than neonates who delivered from non-anemic mothers. The result was found to be consistent with studies done in Iraq28, Pakistan29, and Hawassa17. This similarity could be because maternal anemia leads to fetal hypoxia that affects the development (maturity) of placental blood vessels and in extra-uterine life immediately after birth the newborn may have difficulty breathing because of intrauterine hypoxia30.
Furthermore, this study revealed that; the likelihood of giving a low Apgar score newborn was significantly higher among women with white blood cell count ≥ 15,000/µL. It showed that newborns delivered from mothers with white blood cell count of ≥ 15,000/µL during delivery time were three-fold more likely to have a low Apgar score as compared to mothers of the neonate with white blood cell count of less than 15,000/µL. This finding also agreed with a study in Brazil27. The reason could be that infections during labour can be associated with devastating consequences for pregnant mothers and the fetus.
Conclusion
This study concluded that factors such as preterm birth, lack of antenatal care (ANC) follow-up, instrumental delivery, meconium-stained amniotic fluid, anemia, and leucocytosis were significantly associated with low APGAR scores at five minutes.
To reduce the incidence of low APGAR scores, it is essential to enhance ANC follow-up, minimize instrumental deliveries, prevent preterm labour, detect and manage meconium-stained amniotic fluid early, provide effective preconception health education on anemia during pregnancy, and improve the quality of obstetric care during labour and delivery.
Limitations of the study
The study was limited to single pregnancies, so the findings may not be applicable to multiple pregnancies. There is a possibility of recall bias in the data collection process. Additionally, the study did not account for certain potential risk factors for low APGAR scores, such as congenital anomalies and uterine rupture, as these conditions were not available for consideration at the time of the study.
Data availability
Availability of Data and Materials: The data utilized in this manuscript are available upon reasonable request by contacting one of the corresponding authors via email.
Abbreviations
- APGAR/Apgar:
-
Activity, pulse, grimace, appearance, and respiration
- APH:
-
Antepartum hemorrhage
- GDM:
-
Gestational diabetes melitus
- LAS:
-
Low Apgar score
- MSAF:
-
Meconium stained amniotic fluid
References
American academy of pediatrics committee on fetus and newborn. American college of obstetricians and gynecologists committee on obstetric practice. Apgar Score Pediatr. 136 (4), 819–822 (2015).
Kumaran, V. S. & Bray, Y. Palliative care for newborn infants–the current scene in new Zealand and the way forward. Sites: J. Social Anthropol. Cult. Stud. 7 (2), 113–129 (2010).
Wyckoff, M. H. et al. Part 13: neonatal resuscitation: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132 (18_suppl_2), S543–S60 (2015).
Bayih, W. A. et al. Prevalence and determinants of asphyxia neonatorum among live births at Debre Tabor general hospital, North central ethiopia: a cross-sectional study. Afr. Health Sci. 21 (1), 385–396 (2021).
Ellenberg, J. H. & Nelson, K. B. The association of cerebral palsy with birth asphyxia: a definitional quagmire. Dev. Med. Child. Neurol. 55 (3), 210–216 (2013).
Abdullah, A., Hort, K., Butu, Y. & Simpson, L. Risk factors associated with neonatal deaths: a matched case–control study in Indonesia. Global Health Action. 9 (1), 30445 (2016).
Moura, P. M. S. S. et al. Risk factors for perinatal death in two different levels of care: a case–control study. Reproductive Health. 11, 1–7 (2014).
Suokas, F. The effects of Apgar score defined asphyxia on adulthood cognition: A longitudinal study. (2017).
Yisma, E., Mol, B. W., Lynch, J. W., Mittinty, M. N. & Smithers, L. G. Associations between Apgar scores and children’s educational outcomes at eight years of age. Aust. N. Z. J. Obstet. Gynaecol. 61 (1), 35–41 (2021).
Fetus AAoPCo, K. L. et al. The apgar score. Pediatrics. 136(4), 819–822 (2015).
Getachew, B., Etefa, T., Asefa, A., Terefe, B. & Dereje, D. Determinants of low fifth minute Apgar score among newborn delivered in Jimma University medical center, Southwest Ethiopia. Int. J. Pediat. (2020).
Desalegn, M., Yohannes, T. & Tesfaye, L. Determinants of low Apgar score among newborns delivered by Cesarean section in Nigist Eleni Mohammed memorial specialized hospital, Southern Ethiopia. Sci. Rep. 14 (1), 12420 (2024).
Gudayu, T. W. Proportion and factors associated with low fifth minute Apgar score among Singleton newborn babies in Gondar university referral hospital; North West Ethiopia. Afr. Health Sci. 17 (1), 1–6 (2017).
Zewude, S. B., Ajebe, T. M., Gessesse, S. S. & Wassie, T. H. Proportion and predictive factors of low Apgar score at five minute among Singleton term neonates delivered in Debre Tabor specialized hospital, Northwest ethiopia: A cross-sectional study. Int. J. Afr. Nurs. Sci. 15, 100322 (2021).
Dassah, E. T., Odoi, A. T. & Opoku, B. K. Stillbirths and very low Apgar scores among vaginal births in a tertiary hospital in ghana: a retrospective cross-sectional analysis. BMC Pregnancy Childbirth. 14, 1–7 (2014).
Behrman, R. E. & Stith Butler, A. Institute of medicine committee on Understanding premature birth and assuring healthy outcomes board On Health Sciences Outcomes: Preterm Birth: Causes, Consequences, and Prevention. Preterm Birth: Causes, Consequences, and Prevention: National academies press Washington, DC; (2007).
Yeshaneh, A. et al. The determinants of 5th minute low Apgar score among newborns who delivered at public hospitals in Hawassa city, South Ethiopia. BMC Pediatr. 21 (1), 1–10 (2021).
Mersha, A., Shibiru, S. & Bante, A. Meconium-stained liquor and low birth weight increases the odds of low fifth-minute Apgar scores in public health facilities of Arba minch town, Southern ethiopia: a cross-sectional study. J. Pediatr. Neonatal Care. 10 (3), 86–90 (2020).
Ajibo, B. D. et al. Determinants of low fifth minute Apgar score among newborns delivered by Cesarean section at Wolaita Sodo university comprehensive specialized hospital, Southern ethiopia: an unmatched case control study. BMC Pregnancy Childbirth. 22 (1), 1–8 (2022).
Halle-Ekane, G. E. et al. Quality of antenatal care and outcome of pregnancy in a semi-urban area in Fako division, cameroon: a cross-sectional study. Women Health Open. J. 1 (2), 31–39 (2015).
Gross, K., Alba, S., Glass, T. R., Schellenberg, J. A. & Obrist, B. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy Childbirth. 12, 1–12 (2012).
Lai, S., Flatley, C. & Kumar, S. Perinatal risk factors for low and moderate five-minute Apgar scores at term. Eur. J. Obstet. Gynecol. Reproductive Biology. 210, 251–256 (2017).
Gebremedhin, M. M. et al. Determinants of low APGAR score in newborns delivered at Lemlem Karl general hospital, Northern ethiopia, 2018: a case control study. (2020).
Masood, M. et al. Association of Apgar score with meconium staining of amniotic fluid in labor. Cureus ;13(1). (2021).
Dassah, E. T., Odoi, A. T. & Opoku, B. K. Stillbirths and very low Apgar scores among vaginal births in a tertiary hospital in ghana: a retrospective cross-sectional analysis. BMC Pregnancy Childbirth. 14 (1), 1–7 (2014).
Shimalis, C. et al. Complications of instrumental vaginal deliveries and associated factors in hospitals of Western oromia, Ethiopia. SAGE Open. Med. 10, 20503121221113091 (2022).
Santos, N. C. P. et al. Factors associated with low Apgar in newborns in birth center. Revista Brasileira De Enfermagem. 72, 297–304 (2019).
Jasim, S. K., Al-Momen, H. & Al-Asadi, F. Maternal anemia prevalence and subsequent neonatal complications in Iraq. Open. Access. Macedonian J. Med. Sci. 8 (B), 71–75 (2020).
Shah, T. et al. Gestational anemia and its effects on neonatal outcome, in the population of hyderabad, sindh, Pakistan. Saudi J. Biol. Sci. 29 (1), 83–87 (2022).
Horowitz, K. M., Ingardia, C. J. & Borgida, A. F. Anemia in pregnancy. Clin. Lab. Med. 33 (2), 281–291 (2013).
Author information
Authors and Affiliations
Contributions
Conceptualization: BE and SH: Methodology: BE and LAM: Validation: BG, WZT, MT and WA: Formal Analysis: BE: Investigation: BE and LAM: Resources: BE, LAM, and BG: Writing-Original Draft Preparation: LAM; Writing-Review and Editing: BG, SH, and BE; Supervision: SH and BG. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was obtained from the institutional review boards of the Asrat Woldeyes Health Science Campus (protocol number IRB-014). Written informed consent was obtained from all study participants. This study was conducted in accordance with the principles outlined in the Declaration of Helsinki, and all methods were carried out following relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mengstie, L.A., Hailemeskel, S., Endewunet, B. et al. Determinants of low fifth minute Apgar scores among newborns at North Shoa Zone Public Hospitals in Ethiopia. Sci Rep 15, 34508 (2025). https://doi.org/10.1038/s41598-025-17677-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17677-9