Abstract
The prevalence of chronic diseases is influenced by multiple factors, making their management a complex social and multi-sectoral issue. China has implemented a multisectoral synergistic model for managing chronic diseases; however, enhancing its synergistic effectiveness remains necessary. This study aims to investigate the factors influencing multi-sectoral synergy in chronic disease management. We employed purposive sampling and multi-stage stratified sampling method to survey 160 personnel involved in chronic disease management across 10 departments of county-township-village three level in H District, Beijing. The SFIC (Starting Conditions, Facilitative Leadership, Institutional Design, and Collaborative Process) model served as the framework for the study, and structural equation modeling was conducted using AMOS 24.0 software to analyze the factors influencing the effectiveness of multisectoral collaboration in chronic disease management. The total effects of starting conditions, facilitative leadership, institutional design, and collaborative processes on the effectiveness of multi-sectoral collaboration in chronic disease management were 0.370, 0.638, 0.657, and 0.380, respectively. Among these factors, institutional design had the greatest impact on synergistic effectiveness (0.657). Additionally, the collaborative processes exhibited a mediating effect, contributing 0.525 to the total mediated effect. Starting conditions, facilitative leadership, institutional design, and collaborative processes all influence the effectiveness of multi-sectoral collaboration in chronic disease management, with the collaborative processes mediating these effects. Further efforts should focus on refining institutional design and facilitative leadership, while also considering the influence of the collaborative processes on synergistic effects.
Similar content being viewed by others
Introduction
Chronic non-communicable diseases (“chronic diseases”) have become a major public health problem threatening human health worldwide. According to the latest information from WHO, chronic diseases cause about 41 million deaths annually, accounting for 71% of the total number of deaths worldwide1. According to WHO estimates, if measures are untaken, the total number of deaths from chronic diseases will rise to 55 million by 20302. China has a grim picture of chronic disease, the prevalence of which has led to an increased disease and economic burden. Deaths due to chronic diseases have accounted for 88.5% of all deaths in the country in 2019, and the number of people with chronic diseases in China has exceeded 300 million, and the base of people with chronic diseases is still expanding3.
In order to respond effectively to chronic diseases, the statement “Health in All Policies (HiAP)” was presented at the Eighth International Conference on Health Promotion, which proposes that countries formulate cross-sectoral public health policies, emphasizing the impact of public policies on health systems and on the determinants of health and well-being4. Many countries have developed national policies for the management and prevention of chronic diseases in order to improve care for patients with chronic diseases or to prevent chronic diseases5. For example, in the United States, chronic disease prevention services are legally included in medical insurance6. The North Karelia Project in Finland has been effective in preventing and controlling chronic diseases by implementing community-based interventions based on multisectoral cooperation7. Singapore has instituted group interventions that include community action, multisectoral collaboration, and policy formulation8. In addition, cross-sectoral public policies in countries such as Australia, Switzerland, the United Kingdom and others are playing an active role9,10,11. Since the launch of the new healthcare reform in 2009, more attention has been paid to the prevention and control of chronic diseases in China, and chronic disease management was included as a basic public health service program in the 2010 policy12. The Medium- and Long-Term Plan for the Prevention and Control of Chronic Diseases in China (2017–2025) in 2017 proposed to improve the comprehensive chronic disease prevention and control mechanism that is government-led, sectoral collaboration, mobilization of the society, and participation of the whole population, which has facilitated the formation of a comprehensive prevention and control work environment for chronic diseases13.
As a common public health problem in China and around the world, the prevention and management of chronic diseases is a systematic project with cross-sectoral cooperation, which not only requires the collaboration of medical, preventive and insurance departments within the health system, but also the collaboration of other departments outside the health system14,15,16. Only through the formation of a multisectoral synergistic whole and effective synergistic mechanisms within and outside the health system in chronic disease management can we promote comprehensive chronic disease management.
It has become widely recognized that using intersectoral collaboration to address complex public health problems is an effective strategy. However, the effectiveness of multisectoral collaboration in chronic disease management is affected by many factors, such as common goals, political leadership, financial support, unclear responsibilities, and reward and punishment schemes17,18,19,20. However, relatively few empirical studies have explored how cross-sectoral collaboration can be fostered and sustained21. Although a multisectoral cooperation mechanism for chronic diseases has been established in China, the relationship between vertical and horizontal cooperation is not close enough, and the responsibilities and powers of each sector are not clear22,23. In addition, some non-health sectors are under-engaged24. Which elements of multisectoral collaboration in chronic disease management influence or facilitate multisectoral collaboration? For this problem, this study takes the SFIC synergistic governance model as the research framework, and constructs a framework for analyzing the factors influencing the multisectoral collaborative cooperation in chronic disease management through structural equation modeling, to explore how to promote and maintain cross-sectoral cooperation and tries to put forward some reference-value policy suggestions.
SFIC synergistic governance model
SFIC model is one of the classic synergistic governance models, which was proposed by American scholars Ansell and Gash in 200725. Ansell and Gash adopted the “successive approximation analysis method” to fully analyze the general rules and particularities of 137 cases of synergistic governance in different countries and fields, breaking the limitation that traditional synergistic governance theory only studies a certain field26. After continuous argumentation, the factors affecting the effectiveness of synergistic governance were finally proposed, and the SFIC model, an analytical model of synergistic governance theory, was summarized and constructed25. The letters S, F, I, and C in the SFIC model refer to the four core factors that influence the effectiveness of synergistic governance in the synergistic governance process: Starting Conditions, Facilitative Leadership, Institutional Design, and Collaborative Process. The effect of synergistic governance is the outcome of a combination of starting conditions, facilitative leadership, institutional design, and collaborative process27. Starting conditions refer to the factors affecting the cooperation of the various stakeholders, including resource/knowledge/power inequality, motivation/constraints on participation, and history of cooperation or conflict among the subjects. Facilitative leadership refers to the empowerment of the various subjects in the collaborative process, which can ensure that the process is effectively synergized and plays an important role in the effectiveness of synergistic optimization. Institutional design refers to formulating clear rules and systems for the synergistic process, so that each subject has a clear charter for participating in synergistic governance. The synergistic process is an internal dynamic cyclical process under the combined effect of three variables: starting conditions, catalytic leadership, and institutional design, and it is a process in which trust is built up through face-to-face dialogues and inputs are made into the collaborative process, a consensus is reached, and stage-by-stage results are achieved among the various subjects28. The analytical framework of the SFIC model is shown in Fig. 1.
The SFIC model has been more frequently applied to the collaborative analysis of public governance in different scenarios. Stephen B used the theoretical framework to analyze the Seattle light rail project, arguing that infrastructure development requires multi-sectoral collaboration to build collaborative coalitions across organizations and sectors to formulate and implement public policies29. Todor et al. argue that the creation of collaborative network organizations can provide a long-term effective collaborative basis for proper governance and management, showing significant benefits in terms of sharing knowledge, resources and risks30. In addition, the SFIC model has been effectively used in public services31 and blockchain governance32, but has not yet been found to be used in the health field. In China, the SFIC model has been applied to some extent in the health field. Liu Ying et al. 33 argued that the synergy of multiple subjects in the sports-medical integration model is insufficient, and many institutions are still in the state of “doing things in their own way”, so the SFIC model is used to analyze the reality of the dilemma of sports-medical integration in China. Yang Yusha et al. used SFIC as an analytical framework to comprehensively analyze the dilemma of synergistic cooperation among the various subjects of China’s medical association, and on this basis put forward the path of synergistic governance of the medical association34.
Materials and methods
Research scope
Chronic disease management involves internal synergy within the health system and internal and external synergy within the health system. In order to make the study more focused and feasible, the scope of collaborative chronic disease management was defined as internal collaboration within the “district-town-village” health system, and external collaboration within the “town-village” health system. The synergy within the health system is mainly the horizontal synergy of medicine, prevention and insurance, and the vertical synergy of “district-town-village” three-level medical institutions. The external synergy of the health system is mainly the synergy of government agencies at town and village levels and patriotic health campaign committees (Its main responsibilities are environmental governance, comprehensive health governance, assistance with key disease prevention and control and other public health work). The duties of each sector are shown in Table 1. The defined scope of this study is shown in Fig. 2.
Questionnaire design
We designed the questionnaire based on the four dimensions of the SFIC model and expert consultation. The questionnaire was divided into three parts: the first part was basic information about participants, the second part was the SFIC model scale for multisectoral collaborative management of chronic diseases, and the third part was the effect of synergy. The SFIC model scale for multisectoral collaborative management of chronic diseases has 19 items, with 4 items in the “Starting Conditions” dimension, 5 items in the “Facilitative Leadership” dimension, 5 items in the “Institutional Design” dimension, and 5 items in the “Collaborative Process” dimension. The synergistic effect has 4 items. All question item options in Part two and three were expressed on a five-point Likert scale, categorized into five levels from not agree at all to very agree, with scores of 1–5 assigned, which were used to quantify the survey respondents’ subjective feelings about multisectoral collaborative management of chronic diseases.
Data sources
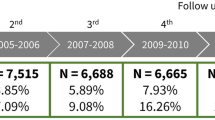
This study conducted a questionnaire survey in District H, Beijing. H District is one of the suburbs of Beijing, with mountainous areas accounting for 89% of the total area. At the end of 2021, there were 284 administrative villages and 36 communities, with a resident population of 441,000 in the district. Employing sampling method that included both purposive sampling and multi-stage stratified sampling. The questionnaire survey was conducted at the district level using the purposive sampling method, and 2–4 relevant personnel were respectively selected from the District Health Commission, District Community Health Center Management Center, District Center for Disease and Prevention and Control, District Medical Insurance Bureau, District Hospital and Patriotic Health Campaign Committee. A multi-stage stratified sampling method was used at the town and village levels. 6 towns were selected, and 1–2 relevant personnel from each town government and 8–10 medical personnel from each community health center were selected for the survey. In each town, 3 administrative villages were selected according to the geographical location and the level of economic development, and a total of 18 administrative villages were selected for questionnaire survey, and 1–2 persons from the village committee and 1 village doctor from the village health office were selected for survey in each village. 167 questionnaires were returned and 7 invalid questionnaires were excluded. Finally, a total of 160 valid questionnaires were included in the analysis with 95.81% validity rate. This study was conducted from September to October 2022.
Statistical analysis
First, we used frequency counts and percentages to characterize the basic characteristics of the respondents. Second, we calculated Pearson correlation coefficients to determine the associations among starting conditions, facilitative leadership, institutional design, and collaborative process. Finally, Structural Equation Modeling (SEM) was used to validate the path and integrated relationships among starting condition, facilitative leadership, institutional design, collaborative process, and synergistic effect. Maximum likelihood estimation was performed to estimate these parameters in SEM. Based on the N:q rule for SEM (sample size/parameter ≥ 5:1) and the academic experience that N = 100–150 is the minimum sample size for use of SEM35,36. In this study, the sample size of 160 and 19 parameters satisfy the requirements and the methodology is applicable. All statistical analyses were performed using SPSS 26.0 and AMOS 24.0. P < 0.05 was statistically significant.
Reliability and validity test
After designing the questionnaire, 18 respondents from the health sector and non-health sector were sought for pre-survey in August 2022 in District H to test the reliability and validity of the questionnaire. In this study, Cronbach’s alpha coefficient was used to measure the reliability of the SFIC model scale for multisectoral collaborative management of chronic diseases. The measurement results showed that the overall Cronbach’s alpha coefficient of the SFIC model scale was 0.855, and the Cronbach’s alpha coefficients of the four dimensions were all greater than 0.7. Thus, it indicated that the reliability of the scale was good. See Table 2.
The questionnaire designed in this study is based on the four core elements of SFIC, which was tested by KMO and Bartlett’s spherical test, and the results showed that the KMO = 0.934 (> 0.8) and χ2 = 3967.558(P < 0.001). This indicates that this scale is ready to be used for validated factor analysis. See Table 3.
Validity tests require the calculation of convergent and discriminant validity, and we used Amos to conduct a validated factor analysis and measure the relevant indicators. According to the validation criteria, the factor standardized loading coefficients for each item in the scale were greater than 0.7 and P < 0.05, indicating a strong correlation between the item and the dimension. When AVE > 0.5 and CR > 0.7, the scale has high convergent validity. As shown in Table 4, all the four dimensions had AVE > 0.5 and CR > 0.7, and the results indicated that the scale had good convergent validity. However, the factor standardized loading coefficient for item CH5 was less than 0.7, and item CH5 was deleted before proceeding to the next step in the analysis.
Discriminant validity needs to be discriminated by the correlation coefficient and AVE square root value. As shown in Table 5, the diagonal of the table is the AVE square root value and the rest of the values are the correlation coefficients, if the AVE square root value of a factor is greater than the absolute value of correlation coefficients between that factor and the other factors and all the factors present this result, the scale has a good discriminant validity. According to the discriminant criteria of discriminant validity, this scale has good discriminant validity among all four dimensions.
Based on the results of the above analysis, the scales of this study have good reliability and validity for further analysis.
Results
Based on the SFIC model and study hypotheses, an initial model of multisectoral synergistic management of chronic diseases was constructed. Starting condition, facilitative leadership, and institutional design were used as exogenous latent variables, collaborative process as a mediating variable, and synergistic effect of multisectoral management of chronic diseases as an endogenous latent variable. The initial model is shown in Fig. 3.
From the results of the fitness test of the initial model, the values of GFI, AGFI, RMSEA, NFI and TLI in the fitness index did not meet the evaluation criteria. In general, the fitness of the initial model is not high, so the model needs to be corrected according to the correction index. The model is theoretically supported by the SFIC synergistic governance theory, and the relationship among the potential variables is set according to the SFIC model, which has a certain theoretical basis. Thus only correction of the observed variables, latent variables, and error terms with respect to each other based on the MI values in the structural equation modeling is required. According to the correction coefficients of the model, six observed variables were deleted, seven correlations between error terms were added, and the model finally met the fitness criteria in all cases. As shown in Table 6.
The path coefficients between each latent variable were tested to be statistically significant. From the results of the impact effect analysis, the starting condition, facilitative leadership, and institutional design have a direct impact on the collaborative process, and a direct and indirect impact on the synergistic effect; the collaborative process has a direct impact on the synergistic effect. Institutional design had the greatest impact on synergistic effect (0.657), followed by facilitative leadership (0.638), and starting condition had the least impact (0.370). The collaborative process had the highest mediating effect value (0.281) between institutional design and synergistic effect, and the collaborative process had the lowest mediating effect value (0.091) between starting condition and synergistic effect, and the collaborative process had a total mediating effect value of 0.525, which accounted for 31.53% of the total effect of starting condition, facilitative leadership, institutional design and synergistic effect. As shown in Tables 7 and 8.
Discussion
Multisectoral collaboration is necessary to address the social determinants of health for chronic diseases, as the implementation of complex multilevel evidence-based health policies, environmental interventions, etc37. At present, the degree of standardization of chronic disease management in China has been greatly improved. The framework of chronic disease management with the participation of multiple departments has basically been formed, and the functions of different organizations involved in chronic disease management have been clarified in the relevant policies22,38. However, due to the influence of the long-standing misconception of “emphasizing treatment and neglecting prevention”, as well as the misperception formed over the years that disease prevention and control are primarily the responsibility of the health sector, the participation of other relevant sectors outside the health sector in chronic disease prevention and control has been insufficiently motivated, proactive and positive, and their responsibilities have been diluted39,40,41,42,43.
Drawing on the SFIC synergistic governance model, this study examines the influencing factors of multisectoral cooperation in chronic management and explores the elements that affect the participation of sectors in the prevention and control of chronic diseases. Measures are taken to address the main influencing factors, strengthen policy coordination and the linkage of multisectoral, and promote the formation of multisectoral synergistic governance for rural chronic disease prevention, control and management.
Our study identified that starting conditions, facilitative leadership, institutional design, and collaborative processes all significantly influenced synergistic effects. Specifically, institutional design exerted the most substantial impact on synergistic effects. Through relevant policies and systems, participation in chronic disease management has become mandatory across various sectors, with clarified responsibilities for each sector. For instance, in 2017, China’s State Council issued the Medium- and Long-Term Plan for the Prevention and Treatment of Chronic Diseases in China (2017–2025), marking the first issuance of such a plan by the State Council specifically targeting chronic disease prevention and treatment13. The policy sets specific targets, making its implementation a critical focus for oversight and supervision across all levels of government. This way is designed to facilitate the realization of various planning objectives and tasks. To address health inequities in Canada, the Government has developed 33 mandate letters focused on key determinants of health. These letters clarify the responsibilities of non-health sectors and outline measures targeting the conditions in which individuals are born, live, grow, work, and age. This approach seeks to explore and utilize initiatives beyond the health sector to enhance health equity44,45. In response to the rise in non-communicable diseases and obesity, Chile implemented stringent food labeling and advertising regulations in 2012 aimed at addressing the obesity epidemic46. Studies have demonstrated that the enforcement of these regulations has had a significant effect46,47.
Starting conditions refer to the initiation of collaborative management of chronic diseases. There is an urgent requirement for synergistic governance in chronic disease management; however, there is currently inadequate momentum towards achieving synergy48,49. In chronic disease management, underlying factors such as cognitive biases, power/resource mismatches, historical collaboration, and outcome expectations between non-health and health sectors are likely to influence the effectiveness of multisectoral synergistic collaboration. Operational and technical barriers between the non-health sector and the health sector, coupled with inadequate awareness of chronic diseases in the non-health sector, hinder the establishment of clear objectives and shared values for chronic disease management50,51. Within the healthcare sector, there exists a certain competitive relationship among medical institutions due to disparities in resources52,53. The investment of resources for chronic diseases by health sectors such as the Center for Disease Prevention and Control, health insurance departments, and hospitals also impacts the effectiveness of synergistic chronic disease management54,55,56.
Facilitative leadership is crucial for fostering trust, balancing relationships, and aligning interests among all stakeholders. However, differences in the strength of local government leadership and the capacity of various entities to fulfill their functions may lead to regional disparities in the effectiveness of chronic disease management. Health managers and leaders need the capability to respond to the changing landscape of chronic diseases57. Therefore, training is used to strengthen leaders’ understanding of chronic diseases and promote the enhancement of leadership capabilities58,59. Furthermore, leadership style, analytical thinking, and innovative thinking are key indicators of leadership competence, which are also essential for chronic disease management60,61.
Collaborative process is the central element of the SFIC model and is pivotal to the effectiveness of governing chronic diseases collaboratively. It includes face-to-face dialogue, trust-building, commitment to the process, consensus-building, and achieving phase outcomes. From 2000 to 2007, WHO formulated strategies, frameworks, and action plans targeting various risk factors of chronic diseases. Countries subsequently developed a series of evidence-based intervention strategies and measures addressing major risk factors, including tobacco control62,63, physical activity interventions64,65, diet66,67, and alcohol restriction68,69. In September 2011, the United Nations General Assembly convened the High-level Meeting on the Prevention and Control of Non-communicable Diseases in New York and adopted a political declaration70. The 8th International Conference on Health Promotion, organized by the WHO in 2013, adopted “Health in All Policies (HiAP)” as its theme. The Declaration of Helsinki issued by the Congress formally introduced HiAP and recognized that HiAP is integral to the achievement of the United Nations Millennium Development Goals and that individual countries should focus on HiAP when drafting their post-2015 development plans. In 2015, the United Nations launched the 2030 Agenda for Sustainable Development, which introduced Sustainable Development Goals and multiple quantifiable and measurable indicators. It encourages countries to develop national strategies based around HiAP to reduce premature mortality from chronic diseases71. Various countries have taken measures to control the development of chronic diseases in their countries in response to these indicators and HiAP, and have achieved certain results. This exemplifies a typical collaborative process72,73,74.
Policy suggestions
Based on the results and discussion, and in conjunction with the SFIC model, this study proposes a framework for the management of chronic diseases with multisectoral synergistic governance. It is shown in Fig. 4.
At the starting conditions level, establishing a robust public-interest value orientation is paramount to foster institutional trust. This requires systematic identification of comparative resource endowments and stakeholder interests across health and non-health sectors. Crucially, the complementary relationship between the professional expertise of health sectors and domain-specific resources of non-health sectors must be operationally defined. Health sectors should transition from functioning as regulatory authorities and dominant providers in chronic disease management toward becoming strategic facilitators and cross-sectoral coordinators. Concurrently, integrating key performance indicators—including disease prevalence rates and standardized management metrics—into non-health sector evaluation frameworks creates accountability mechanisms to incentivize resource commitment.
At the facilitative leadership level, establishing a Health for All Committee is essential to incorporate chronic disease management into government annual plans. This binding administrative approach exerts coordinative authority to: (ⅰ) resolve interdepartmental divergences, (ⅱ) mobilize full stakeholder participation in chronic disease management, and (ⅲ) forge synergistic collaboration. Certain departments must proactively cede authority, so as to form a synergistic governance system led by the government, with community health centers at the core and multi-sectoral participation.
At the institutional design level, establishing the comprehensive safeguard systems and regimes for chronic disease management: (ⅰ) Macro-level coordination of health and non-health sectors through governance structures featuring delineated responsibilities and seamless operational interfaces; (ⅱ) Meso-level implementation protocols defining stakeholder rights, obligations, and shared accountability mechanisms across sectors; (ⅲ) Micro-level service toolkits including evidence-based chronic disease manuals with integrated implementation/evaluation instruments for frontline providers.
At the collaborative processes level, establishing clear synergistic processes and information-sharing platforms. Strengthen horizontal and bottom-up synergies within the health system, and synergies between the health and non-health sectors. The information platform integrates information on demographics, disease composition, nutrition, environmental monitoring, sports and physical activity in the region, which facilitates the development of more scientific interventions through comprehensive information.
Strengths and limitations
First, this study introduces the classic synergistic governance model and applies it to the field of chronic disease management, which expands the scope of application of the SFIC model and provides a new theoretical perspective and analytical tool for multi-sectoral cooperation in chronic disease management. Second, this study enriches the research perspective of chronic disease management by focusing on both health and non-health sectors. Third, this study helps to attribute the problems of multisectoral cooperation in chronic disease management (starting conditions, facilitative leadership, institutional design, and collaborative process) and provides some reference values for strengthening intersectoral cooperation. Meanwhile, this study also has some limitations. First, this study used District H in Beijing as the study sample, which is not representative of the situation in Beijing or other areas, and the generalizability of the results needs to be further explored. Second, the selection of non-health sectors in this study was not comprehensive enough, and due to the influence of the COVID-19 pandemic, the access to data was limited, and some non-health sectors were not included in this study.
Conclusion
The utilization of the SFIC model in the multisectoral collaborative management of chronic diseases provides new research perspectives. In the multi-sectoral collaborative management of chronic diseases, starting conditions, facilitative leadership, institutional design, and collaborative processes collectively influence synergistic effects. Meanwhile, the collaborative processes itself acts as a mediator, with institutional design exerting the most significant impact on synergistic effects. Establishing and optimizing relevant systems can significantly influence the effectiveness of multisectoral collaborative management of chronic diseases. Empowering various stakeholder sectors to oversee chronic disease management processes, mobilize resource flows among sectors, and enhance awareness of chronic disease management in non-health sectors are crucial components.
Data availability
Data sets generated during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Noncommunicable diseases. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (2018).
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. https://www.who.int/publications/i/item/9789241506236 (2013).
The State Council Information Office. The State Council Information Office Held a Briefing on “China’s Population Nutrition and Chronic Disease Status Report (2020)”. https://www.gov.cn/xinwen/2020-12/24/content_5572983.htm. (2020).
Kickbusch, I. Health in all policies. BMJ 347, f4283 (2013).
Gassner, L., Zechmeister-Koss, I. & Reinsperger, I. National strategies for preventing and managing non-communicable diseases in selected countries. Front Public Health 10, 838051 (2022).
Bauer, U. E., Briss, P. A., Goodman, R. A. & Bowman, B. A. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 384, 45–52 (2014).
Puska, P., Laatikainen, T., Korpelainen, V. & Vartiainen, E. Contribution of the North Karelia project to international work in CVD and NCD prevention and health promotion. Glob. Heart 11, 243–246 (2016).
Cheah, J. Chronic disease management: A Singapore perspective. BMJ 323, 990–993 (2001).
Delany, T. et al. Health in all policies in South Australia: What has supported early implementation?. Health Promot. Int. 31, 888–898 (2016).
Peytremann-Bridevaux, I. & Burnand, B. Inventory and perspectives of chronic disease management programs in Switzerland: An exploratory survey. Int. J. Integr. Care 9, e93 (2009).
Willcox, S., Lewis, G. & Burgers, J. Strengthening primary care: Recent reforms and achievements in Australia, England, and the Netherlands. Issue Brief (Commonw Fund) 27, 1–19 (2011).
The Lancet Public Health, null. China’s health reform: 10 years on. Lancet Public Health 4, e431 (2019).
Kong, L.-Z. China’s medium-to-long term plan for the prevention and treatment of chronic diseases (2017–2025) under the healthy China initiative. Chronic Dis. Transl. Med. 3, 135–137 (2017).
De Jong, M., Tijhuis, Y., Koelen, M. & Wagemakers, A. Intersectoral collaboration in a Dutch community health promotion programme: Building a coalition and networks. Health Promot. Int. 38, daab207 (2023).
Adeleye, O. A. & Ofili, A. N. Strengthening intersectoral collaboration for primary health care in developing countries: Can the health sector play broader roles?. J. Environ. Public Health 2010, 272896 (2010).
Allen, P. et al. Perceived benefits and challenges of coordinated approaches to chronic disease prevention in state health departments. Prev. Chronic Dis. 11, E76 (2014).
Amri, M., Chatur, A. & O’Campo, P. An umbrella review of intersectoral and multisectoral approaches to health policy. Soc. Sci. Med. 315, 115469 (2022).
Tumusiime, P. et al. Building health system resilience in the context of primary health care revitalization for attainment of UHC: Proceedings from the Fifth Health Sector Directors’ Policy and Planning Meeting for the WHO African Region. BMC Proc. 14, 16 (2020).
Bennett, S., Glandon, D. & Rasanathan, K. Governing multisectoral action for health in low-income and middle-income countries: Unpacking the problem and rising to the challenge. BMJ Glob. Health 3, e000880 (2018).
Emerson, K. Collaborative governance of public health in low- and middle-income countries: Lessons from research in public administration. BMJ Glob. Health 3, e000381 (2018).
Hearld, L. R., Alexander, J. A., Wolf, L. J. & Shi, Y. The perceived importance of intersectoral collaboration by health care alliances. J. Commun. Psychol. 47, 856–868 (2019).
Hou, L., Chen, B., Ji, Y., Wang, B. & Wu, J. China CDC in Action—Hypertension prevention and control. China CDC Wkly 2, 783–786 (2020).
Wang, Z. et al. Changes in chronic disease management among community health centers (CHCs) in China: Has health reform improved CHC ability?. Int. J. Health Plann. Manage 32, 317–328 (2017).
Dai, B. Does China’s new cooperative medical scheme promote rural elders’ access to healthcare services in relation to chronic conditions?. Int Health 7, 32–41 (2015).
Ansell, C. & Gash, A. Collaborative governance in theory and practice. J. Public Admin. Res. Theory 18, 543–571 (2008).
Liu, W. & Yang, D. Research on the formation and optimization of the collaborative governance mechanism of Urban catastrophe risk: Based on SFlC model. Urban Dev. Stud. 29, 12–16 (2022).
Joaquín, H. Jr. The multisectoral trilemma of network management. J. Public Admin. Res. Theory 18, 1–31 (2008).
Yan, P., Xiao-ying, D., Ji-miao, W. & Song, D. Research on synergistic governance of cross-border economic cooperation zones in Yunnan Province based on the SFIC model. J. Yunnan Admin. Coll. 21, 125–130 (2019).
Comparative Perspectives on Seattle’s Light Rail Project. Stephen B, P. Theories of Governance. Policy Stud. J. 41, 583–608 (2013).
Tagarev, T., Davis, B. Á. & Cooke, M. Business, organisational and governance modalities of collaborative cybersecurity networks. Multimed. Tools Appl. 81, 9431–9443 (2022).
Bianchi, C., Nasi, G. & Rivenbark, W. C. Implementing collaborative governance: Models, experiences, and challenges. Public Manag. Rev. 23, 1581–1589 (2021).
Lumineau, F., Wang, W. & Schilke, O. Blockchain governance—A new way of organizing collaborations?. Organ. Sci. 32, 500–521 (2021).
Llu, Y. & Wang, Y. Promotion dilemma and strategy of physical-medicaintegration in China based on SFlc model. J. Shenyang Sport Univ. 40, 1–7 (2021).
Yang, Y. & Chen, Y. Research on collaborative path of medical alliance in China based on SFlc model. Health Econ. Res. 39, 52–55 (2022).
Jackson, D. L. Revisiting sample size and number of parameter estimates: Some support for the N: q hypothesis. Struct. Equ. Model. 10, 128–141 (2003).
Bentler, P. M. & Chou, C.-P. Practical lssues in structural modeling. Sociol. Methods Res. 16, 78–117 (1987).
Mazzucca, S. et al. Expanding implementation research to prevent chronic diseases in community settings. Annu. Rev. Public Health 42, 135–158 (2021).
Jiang, Y. et al. Gaps and directions in addressing non-communicable and chronic diseases in China: A policy analysis. Int. J. Environ. Res. Public Health 19, 9761 (2022).
Xiao, N., Long, Q., Tang, X. & Tang, S. A community-based approach to non-communicable chronic disease management within a context of advancing universal health coverage in China: Progress and challenges. BMC Public Health 14(Suppl 2), S2 (2014).
Lei, T., Yang, J., Hong, M. & Fu, D. Analysis of medical insurance payment to promote the prevention and control of chronic diseases-based on stakeholder theory. Health Econ. Res. 39, 38–41 (2022).
Jang, Y. et al. Research on the status of multi-sector cooperation innational chronic disease comprehensive control andprevention demonstration areas. Chin. J. Health Policy 12, 59–66 (2019).
Si, X., Zhai, Y., Zhu, X. & Ma, J. Multi-sectoral coordination and social participation forprevention and control of chronic disease in China fromCDC perspective. Chin. J. Prev. Control Chronic Dis. 27, 268–271 (2019).
Zhang, Y. & Qin, J. Challenges and strategies of non-communicable diseaseprevention and control from the perspective of Health inAll Policies: A survey in typical health cities in China. Chin. J. Health Policy 7, 65–69 (2014).
Lucyk, K. Intersectoral action on the social determinants of health and health equity in Canada: December 2019 federal government mandate letter review. Health Promot. Chronic. Dis. Prev. Can. 40, 314–323 (2020).
Smith, M. J. & Weinstock, D. Reducing health inequities through intersectoral action: Balancing equity in health with equity for other social goods. Int. J. Health Policy Manag. 8, 1–3 (2019).
Corvalán, C., Reyes, M., Garmendia, M. L. & Uauy, R. Structural responses to the obesity and non-communicable diseases epidemic: The Chilean Law of Food Labeling and Advertising. Obes. Rev. 14(Suppl 2), 79–87 (2013).
Caballero, S. et al. Eating contexts determine the efficacy of nutrient warning labels to promote healthy food choices. Front Nutr 9, 1026623 (2022).
Wolfenden, L. et al. A call to action: More collaborative implementation research is needed to prevent chronic disease. Aust. N. Z. J. Public Health 46, 549–553 (2022).
Duda-Sikuła, M. & Kurpas, D. Barriers and facilitators in the implementation of prevention strategies for chronic disease patients-best practice GuideLines and policies’ systematic review. J. Pers. Med. 13, 288 (2023).
Baugh Littlejohns, L. K. & Willis, C. D. Collaborative value creation framework: The potential for strengthening intersectoral partnerships in chronic disease prevention. Prog. Commun. Health Partnersh. 12, 463–472 (2018).
Najafi, M., Mosadeghrad, A. M. & Arab, M. Mechanisms of intersectoral collaboration in the health system: A scoping review. Iran J. Public Health 52, 2299–2312 (2023).
Xiao, Y., Qiu, Q.-M., Huang, Y.-X. & Zhu, S.-Y. Patients gather in large hospitals: The current situation of Chinese hospitals and the direction of medical reform. Postgrad. Med. J. 98, e43 (2022).
Liu, J. et al. Primary health institutions preference by hypertensive patients: Effect of distance, trust and quality of management in the rural Heilongjiang province of China. BMC Health Serv. Res. 19, 852 (2019).
Shen, M., He, W., Yeoh, E.-K. & Wu, Y. The association between an increased reimbursement cap for chronic disease coverage and healthcare utilization in China: An interrupted time series study. Health Policy Plan 35, 1029–1038 (2020).
Voetsch, K., Sequeira, S. & Chavez, A. H. A customizable model for chronic disease coordination: Lessons learned from the coordinated chronic disease program. Prev. Chronic Dis. 13, E43 (2016).
Francis, L., Dunt, D. & Cadilhac, D. A. How is the sustainability of chronic disease health programmes empirically measured in hospital and related healthcare services?-A scoping review. BMJ Open 6, e010944 (2016).
Figueroa, C. A., Harrison, R., Chauhan, A. & Meyer, L. Priorities and challenges for health leadership and workforce management globally: A rapid review. BMC Health Serv Res 19, 239 (2019).
Malakoane, B., Chikobvu, P., Heunis, J. C., Kigozi, N. G. & Kruger, W. H. Implementing an intervention to improve leadership/management of public healthcare services in the Free State Province, South Africa: Lessons learned. Afr. Health Sci. 23, 469–482 (2023).
Horváth, C. et al. How management and leadership training can impact a health system: Evaluation findings from a public health management training program in Cambodia. Front. Public Health 9, 784198 (2021).
Dorji, K., Tejativaddhana, P., Siripornpibul, T., Cruickshank, M. & Briggs, D. Leadership and management competencies required for Bhutanese primary health care managers in reforming the district health system. J Healthc Leadersh 11, 13–21 (2019).
Xirasagar, S., Samuels, M. E. & Curtin, T. F. Management training of physician executives, their leadership style, and care management performance: An empirical study. Am. J. Manag. Care 12, 101–108 (2006).
Sims, M. et al. Did smokefree legislation in England reduce exposure to secondhand smoke among nonsmoking adults? Cotinine analysis from the Health Survey for England. Environ. Health Perspect. 120, 425–430 (2012).
Haw, S. J. & Gruer, L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: National cross sectional survey. BMJ 335, 549 (2007).
Bull, F. & Dvorak, J. Tackling chronic disease through increased physical activity in the Arab World and the Middle East: challenge and opportunity. Br. J. Sports Med. 47, 600–602 (2013).
Conroy, M. B., Cook, N. R., Manson, J. E., Buring, J. E. & Lee, I.-M. Past physical activity, current physical activity, and risk of coronary heart disease. Med. Sci. Sports Exerc. 37, 1251–1256 (2005).
Levy, L. B. Dietary strategies, policy and cardiovascular disease risk reduction in England. Proc. Nutr. Soc. 72, 386–389 (2013).
Rodriguez-Fernandez, R. et al. Current salt reduction policies across gradients of inequality-adjusted human development in the WHO European region: minding the gaps. Public Health Nutr. 17, 1894–1904 (2014).
Gordon, R. & Anderson, P. Science and alcohol policy: a case study of the EU Strategy on Alcohol. Addiction 106(Suppl 1), 55–66 (2011).
Veryga, A. 2008-Lithuania’s year of sobriety: alcohol control becomes a priority of health policy. Addiction 104, 1259 (2009).
Lincoln, P. et al. Conflicts of interest and the UN high-level meeting on non-communicable diseases. Lancet 378, e6 (2011).
Manandhar, M., Hawkes, S., Buse, K., Nosrati, E. & Magar, V. Gender, health and the 2030 agenda for sustainable development. Bull World Health Organ 96, 644–653 (2018).
NCD Countdown 2030 collaborators. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 392, 1072–1088 (2018).
Jelaković, B. et al. Croatian action on salt and health (CRASH): On the road to success-less salt more health. Nutrients 16, 1518 (2024).
Rashid, S. et al. Availability and readiness of primary healthcare facilities for the management of non-communicable diseases in different districts of Punjab Pakistan. Front. Public Health 11, 1037946 (2023).
Acknowledgements
We thank all the participants, experts and researchers who participated in this study. We also thank the leaders of the Health Commission of H District, Beijing for their help and support for this study.
Funding
This study was supported by the Beijing Municipal Education Commission (grant number: SZ201910025008).
Author information
Authors and Affiliations
Contributions
Conceptualization: JL and JY. Methodology: JL and JY. Data collection and analysis: JL, NZ and GM. Drafted manuscript: JL and JY. Supervision: JY. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The studies involving human participants are reviewed and approved by the Ethics Committee of Capital Medical University (NO. Z2020SY117). The participants signed an informed consent form for their participation in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, J., Zhao, N., Gu, M. et al. Applying the SFIC synergistic governance model to analyze determinants of multisectoral collaborative chronic disease management in Beijing’s district H. Sci Rep 15, 33094 (2025). https://doi.org/10.1038/s41598-025-17690-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17690-y