Abstract
Hereditary eye diseases, particularly inherited retinal diseases (IRDs), are major causes of visual impairment and blindness. However, IRDs real-world impact in China remains limited. Our study aimed to investigate the socio-demographic characteristics, clinical burden, and perceived quality of life among individuals affected by inherited retinal diseases, with retinitis pigmentosa (RP) as the most common subtype. A cross-sectional national survey was conducted using both online and paper-based questionnaires distributed through hospitals and patient organizations. The questionnaire included sections on demographics, clinical history, genetic testing, symptoms, and the social and economic impact of the disease. A total of 1219 valid responses were collected. RP accounted for 49.08% of diagnoses. Nearly half of the patients (48.81%) reported onset before school age. Night blindness (59.15%) and visual field constriction (58.08%) were the most common symptoms. Cataracts were present in 18.21% of respondents. Psychosocial burden scores across seven domains (e.g., daily life, work, family) exceeded a mean of 6/10, indicating moderate-to-high stress levels. Additionally, 57.51% of households reported annual income below 100,000 RMB (~$14,000 USD), highlighting financial barriers to IRDs patient care and treatment. This survey reveals a substantial burden associated with hereditary eye diseases in China, impacting patients’ functional ability, mental well-being, and socioeconomic status. Our findings underscore the urgent need for public awareness, policy support, and affordable therapeutic options to address the needs of this underserved population.
Similar content being viewed by others
Introduction
Hereditary eye diseases (HEDs), especially inherited retinal dystrophies (IRDs), represent a significant and irreversible cause of visual impairment and blindness worldwide. IRDs are a genetically heterogeneous group of disorders characterized by the progressive degeneration of photoreceptors and other retinal cells, with an estimated prevalence of 1 in 3000 to 4000 individuals globally1. Among them, retinitis pigmentosa (RP) is the most common subtype and is often used as a representative condition in epidemiological studies due to its relatively high frequency, early onset, and chronic progression2,3.
Despite advances in molecular diagnostics and emerging therapeutic options such as gene therapy, most patients with hereditary eye diseases—particularly in low- and middle-income countries—face substantial challenges in accessing timely diagnosis, treatment, and psychosocial support4,5. In China, the epidemiology and real-world burden of IRDs remain poorly documented. National registries are lacking, and existing studies tend to focus on isolated clinical or genetic cohorts. As a result, public health planning and policy development for this population are severely hampered by the scarcity of population-level data.
To address this gap, we conducted a cross-sectional, nationwide survey among patients with hereditary retinal diseases in China, with a focus on RP as the most prevalent condition. The primary objectives were to1: describe the socio-demographic and clinical characteristics of affected individuals2; assess self-reported symptoms, comorbidities, and perceived disease progression3; evaluate the psychosocial and economic burden associated with hereditary eye disease4; explore patients’ reproductive intentions and treatment expectations.
By presenting one of the largest patient-reported datasets of its kind in China, this study aims to provide meaningful insights for researchers, clinicians, and policymakers. We hope that our findings can serve as a foundation for future research, guide service planning, and advocate for better access to care and support for individuals living with genetic eye diseases.
Methods
Questionnaire design
The data for this research originated from a structured questionnaire developed by a multidisciplinary expert panel comprising ophthalmologists, statisticians, and public health specialists. The questionnaire was available in both online and paper-based formats. Before official distribution, a pilot version was administered to 20 volunteers to assess clarity, readability, and content relevance. Feedback from the pilot resulted in minor revisions to the wording and layout.
The finalized questionnaire consisted of three domains1: Disease History and Symptoms2, Quality of Life and Social Burden, and3 Demographics. Question types included single-choice, multiple-choice, and open-ended questions. Most items were categorical and analyzed using descriptive statistics; open responses were coded thematically for further analysis. Content validity was confirmed through expert review, and respondents typically completed the survey within 10–15 min. The full English version of the questionnaire used in this study is available in Supplementary Material (Supplementary File 1), which was translated from the original Chinese version and reviewed by bilingual experts for accuracy.
Field research and data collection
We provided patients and their family members with both paper-based and QR code-based questionnaire options. Participants were recruited from outpatient clinics and patient organizations, with recruitment efforts also extended to community-based groups and professional networks. We employed a combination of convenience sampling and snowball sampling to access a broader range of individuals affected by the condition, as these methods are widely used in rare disease research. Inclusion criteria were1: a confirmed diagnosis of hereditary retinal diseases2; the ability to understand and answer the questionnaire3; willingness to participate in the study and provide informed consent. Exclusion criteria included1: inability to understand or answer the questionnaire consistently2; duplicated submissions3; presence of other retinal diseases such as diabetic retinopathy or macular degeneration.
The study protocol was approved by the Ethics Committee of Wuhan University Renmin Hospital Institutional Review Boards (No. WDRY 2023-K104), and all procedures were conducted by the Declaration of Helsinki. A total of 1219 valid survey responses were collected. The privacy of all participants was strictly protected throughout the process.
Data analysis
We performed descriptive statistical analyses using SPSS version 27. Categorical variables such as gender, education level, and household income were summarized using frequencies and percentages. Continuous variables, such as the socioeconomic impact score (ranging from 1 to 10), were analyzed using mean values and Mann–Whitney U tests, depending on distribution normality. No mortality data were collected or analyzed, and all results reflect cross-sectional self-reported findings at the time of the survey.
To assess the reliability of the socioeconomic impact scale, we calculated Cronbach’s alpha for internal consistency. All statistical tests were two-tailed, and p-values < 0.05 were considered statistically significant.
Data study and discussion
Upon completion of data analysis, we compared our findings with those of existing literature, particularly focusing on differences between our results and those of academic surveys. Literature referenced for comparison primarily includes research reports on the socioeconomic burdens of hereditary eye diseases in different countries or regions over the past two decades, studies on the etiology and complications of various types of hereditary eye diseases, and improvements in population distribution characteristics and treatment approaches for hereditary eye diseases both domestically and internationally in recent years.
Results
Demographic analysis
Of the 1219 respondents, 777 were male and 442 female (male: female ratio 1.76:1). Married individuals accounted for 64.40% of the sample. Educational attainment was distributed as follows: ≤ junior high school (25.18%), senior high/technical (17.06%), and college or higher (57.75%). According to ISCO-08 classification, occupations were distributed among white-collar workers (38.0%), manual laborers (13.2%), informal/flexible work (29.0%), and unemployed/non-working (19.8%). Approximately 57.51% of participants reported annual household income below 100,000 RMB. Detailed statistics are shown in Table 1.
Disease
We examined the age distribution at which patients began experiencing visual impairment (Fig. 1A).
Age at onset and complications of inherited retinal diseases (IRDs). (A) Distribution of self-reported age at onset among 1219 patients with IRDs in China. (B) Frequencies of major ocular complications reported in the same group, including cataract, macular edema (ME), macular tear (MT), and retinal detachment (RD).
We found that 48.81% of patients reported onset before school age, indicating that symptoms of hereditary retinal diseases often manifest in childhood. This finding is consistent with previous research1.
Distribution of relevant indicators
Disease types and genotypes
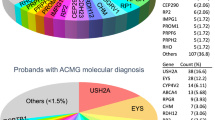
Among the 1219 respondents, 598 (49.08%) reported a diagnosis of retinitis pigmentosa (RP), while 329 (27.0%) had genetically confirmed mutations associated with hereditary retinal diseases. Approximately 3.42% had no genetic testing, 6.84% had genetic testing but did not receive a definitive diagnosis, indicating that over 10% of the population remained genetically undiagnosed (Fig. 2A).
Participants were selected from a predefined set of commonly reported genes(top 14 genes in China)in previous IRD studies6,7. The results showed that 35.87% of participants reported other genes not included in the list, 16.57% were classified as “gene not been tested,” referring to patients who had not undergone any genetic testing, and 10.81% were “genetic testing negative,” indicating that testing was performed but no pathogenic variants were identified (Fig. 2B).
Disease types and genotypes in the patient group. (A) Distribution of primary IRD diagnoses, with retinitis pigmentosa as the most common subtype. (B) Genetic testing results were categorized as (i) the top 14 commonly reported genes in China, (ii) other genes, (iii) “gene not been tested” (patients without any genetic testing), and (iv) “genetic testing negative” (patients tested but no pathogenic variants detected).
Complications and symptoms
We assessed complications after disease onset. Cataracts were the most common complication (18.21%), with macular edema (ME), macular tear (MT), and retinal detachment (RD) each under 10% (Fig. 1B).
Regarding symptoms, over half of respondents reported night blindness (59.15%) and visual field constriction (VF constriction) (58.08%). Central visual acuity reduction (CVA Loss) was reported by 48.97%, and 35.19% had refractive errors (RE). Other symptoms, including photopsia, metamorphopsia, floaters, nystagmus, eye pain, and color vision deficiency (CVD), were each reported by 10–20% of patients (Fig. 3).
Factors contributing to disease progression
Self-reported contributors to progression included excessive visual load (40.61%) and staying up late (23.46%). Notably, 16.57% reported symptom worsening after COVID-19 infection and 10.17% after vaccination, though no causal inference can be drawn from these cross-sectional data (Table 2).
In this study, “deterioration” was defined as self-perceived worsening of vision-related symptoms such as acuity loss or visual field narrowing. In subsequent discussions, we further analyze the factors contributing to disease progression.
Impact on social function, economic status, and family
Patients rated the impact of disease on daily life, occupation, social pressure, education, family responsibilities, economic stress, and overall negative impact on a 1–10 scale. Independent variance tests showed no significant effect of gender (p > 0.05) (Fig. 4A).
Subsequently, we conducted a reliability and validity analysis of the questionnaire. The Cronbach’s alpha coefficient based on standardized items was 0.942, the KMO coefficient was 0.923, and Bartlett’s spherical test significance was less than 0.05, indicating high reliability and validity of the questionnaire. Figure 4B presents mean ± SD scores factors; score > 6 indicating moderate-to-high perceived burden (Fig. 4B).
Impact of IRDs on patients’ daily lives. (A) Comparison of mean impact scores across major life domains between male and female patients, with no significance indicated by variance tests. (B) Radar chart summarizing the mean impact scores for each domain, illustrating the multidimensional burden of IRDs.
Impact on reproductive plans
On patients’ understanding of inheritance patterns (Fig. 5A). Over 40% reported “unknown”, while 33.10% reported autosomal recessive inheritance (AR), consistent with previous reports8.
Family pedigree analysis showed nearly 60% reported only themselves affected within three generations; 20% direct relatives affected; 7.10% collateral relatives affected; and 3.40% direct and collateral relatives both affected. About 10.80% were unclear about family history (Fig. 5B).
Overall, over 60% of respondents reported that their family plans were significantly influenced by the disease, with more than 30% of them abandoning or altering their plans for having children (Fig. 5C).
Effects of IRDs on reproductive planning. (A) Distribution of patients according to the known mode of inheritance (autosomal recessive, X-linked, autosomal dominant, digenic Inheritance, mitochondrial Inheritance, or unknown). (B) Family history of IRDs reported by participants. (C) Proportion of patients reporting that the disease has influenced their fertility intentions, including decisions to delay or forgo pregnancy.
Expectations
Nearly 40% of patients expressed strong optimism regarding the prospects of future effective treatments, while nearly 30% reported optimism. In contrast, only a small number of patients exhibited pessimistic attitudes (Fig. 6A).
Regarding the perspective on treatment waiting times, 35.30% of respondents indicated they would wait less than three years, 42.90% would wait between three and five years, and 21.80% would wait more than five years (Fig. 6B).
Discussion
In this study, we analyzed the demographic, clinical, and psychosocial profiles of patients with hereditary eye diseases.
Retinitis pigmentosa (RP) emerged as the most common diagnosis, consistent with previous studies on inherited retinal dystrophies1. Notably, nearly half of all respondents reported disease onset before school age, underscoring the early and lifelong impact of these conditions. Night blindness and visual field constriction were the most frequently reported symptoms, aligning with the known natural history of RP and similar disorders2. The psychosocial and economic burden associated with inherited retinal diseases is considerable. Patients reported moderate-to-high stress across domains, including daily life, work, family responsibilities, and financial concerns. Over 57% of respondents had an annual household income below 100,000 RMB, suggesting limited access to advanced interventions such as gene therapy. These findings are in line with prior research indicating reduced employment rates, higher dependency, and diminished quality of life among individuals with inherited visual impairments9. Although most patients were aware of their condition, a small subset remained unaware of their diagnosis for genotype, reflecting the diagnostic challenges or informational disparities associated with IRDs.
Analysis of disease-related indicators and quality of life in patients with hereditary eye diseases
Impact of cataracts and cataract surgery on patients
Among the 1,219 respondents, 222 (18.21%) reported cataracts as a comorbidity. When comparing the average value of RP patients with and without cataracts, those with cataracts reported significantly higher burden scores across six quality-of-life dimensions: daily life, occupation, social functioning, education, and family responsibilities (all p < 0.05). Additionally, in response to the question regarding the perceived overall impact of eye disease, cataract patients again reported higher distress levels (p = 0.002). (Table 3)
Cataract is an age-related disease, and the older the age, the heavier the disease burden of cataract visual disability. Studies have shown that the disease burden of cataract visual disability in people aged 65 years and older is more than seven times the average disease burden of the total population10. Based on the identification of this current situation, we make the prediction that the prevalence of cataracts in the patient population will further increase, and the burden of the disease will further increase with the aging process of the population.
Fifty patients had previous cataract surgery, and 8 individuals reported subjective worsening of their condition postoperatively. This observation aligns with previous studies suggesting that cataract surgery is generally safe and effective for RP patients11,12, improving visual acuity without accelerating retinal degeneration. These findings reinforce the value of timely surgical intervention in reducing disease burden and enhancing quality of life in this subgroup.
Impact of COVID-19 on patients
The COVID-19 pandemic has profoundly disrupted global healthcare systems, resulting in delayed medical visits, reduced follow-up, and psychological distress among patients with chronic diseases13. In our patient group, 16.57% of respondents perceived that the progression of their hereditary eye disease was related to the COVID-19 pandemic. This perception may stem from disruptions in regular ophthalmic care, reduced access to rehabilitation services, or decreased motivation to seek care due to lockdowns and infection risk. We used the Mann-Whitney U test to analyze the stress levels of COVID-19 patients and non-infected patients. The results showed that, except for educational stress, whose P value was significantly greater than 0.05, the P value of all other stress factors was less than 0.05. Therefore, we concluded that there were subjective differences in stress levels between COVID-19 patients and non-infected patients. (Table 4)
Although our survey did not include longitudinal ophthalmologic data, these self-reported impressions are consistent with the known challenges faced by visually impaired individuals during the pandemic. Previous studies have indicated that patients with chronic eye conditions experienced delayed treatments and worsening symptoms during COVID-19 lockdown periods, especially in low- and middle-income settings13. Moreover, stress and anxiety during the pandemic may exacerbate subjective visual complaints or amplify concern over disease deterioration14.
Taken together, these findings highlight the importance of maintaining continuity of care for patients with hereditary eye diseases, even during public health emergencies. Strategies such as teleophthalmology, remote counseling, and flexible scheduling may help mitigate the adverse impact of service interruptions and preserve visual and psychological stability in this vulnerable population.
Psychological burden and mental health implications
The psychological burden is exacerbated by economic constraints and limited treatment options. The mean economic pressure score was 6.60, indicating a moderate to high level of financial stress.
These barriers can worsen feelings of helplessness, frustration, and anxiety, especially in low-income families. The disease also exerts pressure on family dynamics and social relationships. The mean score for family-related stress was 8.15, second only to the overall negative life impact (8.28). Family members often serve as caregivers, which may strain finances and limit their own professional and social engagement. For younger patients, the risk of social exclusion and employment discrimination further heightens psychological distress and perceived isolation. These findings are consistent with existing literature, which reports high rates of depression, anxiety, and reduced social integration among individuals with visual impairment15. Addressing these psychological challenges requires a multidimensional approach that includes not only medical care but also emotional support, social inclusion initiatives, and financial assistance. Improving infrastructure, promoting disability awareness, and providing tailored employment counseling may help reduce mental health burden and enhance quality of life16.
Limitations
This study provides real-world insights into the socioeconomic impact of hereditary eye diseases in China; however, several limitations should be noted. Convenience sampling and snowball sampling methods may introduce selection bias, limiting the generalizability of the study results. The sample lacks geographic diversity and is not nationally representative, and the higher proportion of male respondents may be related to sampling methods as well as differences in participation and access to medical resources. Self-reported data may be subject to recall bias. The absence of longitudinal data prevents assessment of disease progression. Future studies would employ more rigorous sampling methods and undergo objective clinical validation.
Conclusion
This cross-sectional study of 1219 patients with hereditary eye diseases in China reveals a high burden of visual impairment and psychosocial distress, with early-onset retinitis pigmentosa as the most prevalent diagnosis. Many respondents reported severe symptoms and complications, delays in diagnosis, and limited access to genetic testing or advanced treatments.
These findings underscore the urgent need for greater public awareness, improved early diagnostic access, and more affordable treatment options to reduce disparities in care for this underserved population. Future efforts should also prioritize psychosocial support and genetic counseling to improve patient outcomes and equity in care delivery. These insights may also guide the development of targeted public health initiatives and inform health policy planning to expand access to early diagnosis, patient support, and emerging therapies for hereditary eye diseases in China.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Hartong, D. T., Berson, E. L. & Dryja, T. P. Retinitis pigmentosa. Lancet 368 (9549), 1795–1809 (2006).
Dias, M. F. et al. Molecular genetics and emerging therapies for retinitis pigmentosa: Basic research and clinical perspectives. Prog. Retin. Eye Res. 63, 107–131 (2018).
Berger, W., Kloeckener-Gruissem, B. & Neidhardt, J. The molecular basis of human retinal and vitreoretinal diseases. Prog. Retin. Eye Res. 29 (5), 335–375 (2010).
Paudel, N., Daly, A., Waters, F. & Stratieva, P. Genetic testing experiences of people living with inherited retinal degenerations: Results of a global survey. Ophthalmic Res. 67 (1), 201–210 (2024).
Song, M-S., Alluin, J. & Rossi, J. J. The effect of Dicer knockout on RNA interference using various Dicer substrate small interfering RNA (DsiRNA). Struct. Genes 13(3). (2022).
Ellingford, J. M. et al. Molecular findings from 537 individuals with inherited retinal disease. J. Med. Genet. 53 (11), 761–767 (2016).
Su, B. N., Shen, R. J., Liu, Z. L., Li, Y. & Jin, Z. B. Global spectrum of USH2A mutation in inherited retinal dystrophies: Prompt message for development of base editing therapy. Front. Aging Neurosci. 14, 948279 (2022).
Jin, B. et al. Genetic characteristics of suspected retinitis pigmentosa in a cohort of Chinese patients. Gene 853, 147087 (2023).
Pang, P. C. K., Lam, C. S. Y., Hess, R. F. & Thompson, B. Effect of dichoptic video game treatment on mild amblyopia–a pilot study. Acta Ophthalmol. 99 (3), e423–e432 (2021).
Zhu, M. Y. & Liu, J. Disease burden analysis of cataract visual disability in Chinese residents. Shandong Med. J. 55 (23), 85–87 (2015).
Asbell, P. A. et al. Age-related cataract. Lancet 365 (9459), 599–609 (2005).
Nguyen, X-T-A. et al. Outcome of cataract surgery in patients with retinitis pigmentosa. Am. J. Ophthalmol. 246, 1–9 (2023).
Bouhout, S. H., Jakubowska, M., Jaworski, W., Freeman, L. & Aubin, E. E. Impact of the COVID-19 pandemic on mental health among patients with chronic ocular conditions. Vision 7 (3), 1 (2023).
Syriga, M., Karampela, I., Dalamaga, M. & Karampelas, M. The effect of COVID-19 pandemic on the attendance and clinical outcomes of patients with ophthalmic disease: A mini-review. Metabol. Open 12, 100131 (2021).
Henes, S. T., Collier, D. N., Morrissey, S. L., Cummings, D. M. & Kolasa, K. M. Medical nutrition therapy for overweight youth in their medical home: The KIDPOWER experience. Patient Educ. Couns. 81 (1), 43–46 (2010).
Nordmann, J. P., Auzanneau, N., Ricard, S. & Berdeaux, G. Vision related quality of life and topical glaucoma treatment side effects. Health Qual. Life Outcomes 1, 75 (2003).
Acknowledgements
Not applicable.
Funding
National Natural Science Foundation of China (82471086).
Author information
Authors and Affiliations
Contributions
Yuqing Lin, Xiyang Dou and Lihong Li were the major contributors in reviewing the literature, writing the manuscript, and creating descriptive figures. Wenhui Zhou, Wenqing Zhang and Jason Zihan Wang were involved in the collection and collation of the data. Yin Shen and Lei Wang critically reviewed and revised the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained from all subjects and/or their legal guardians. And all methods were approved by Wuhan University Renmin Hospital Institutional Review Boards (No. WDRY 2023-K104).
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, Y., Dou, X., Li, L. et al. Burden and characteristics of inherited retinal diseases in China. Sci Rep 15, 32748 (2025). https://doi.org/10.1038/s41598-025-17714-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-17714-7