Abstract
Urgent-start peritoneal dialysis (USPD) has been identified as the efficient approach to initiate renal replacement treatment in end-stage renal disease patients. Cardiovascular mortality of urgent dialysis is an important issue. The present work focused on assessing risk factors related to cardiovascular death in USPD patients. We carried out the present multicenter retrospective cohort study in Northeast China, included adults initiating USPD between 2013 and 2019. Follow-up was conducted in every patient till the occurrence events below: technical failure, death, loss-to-follow-up, and renal transplantation. There were altogether 1549 cases enrolled into this work. Among them, 123 encountered cardiovascular death. Upon multivariate regression, predictors of cardiovascular death included advanced age (HR 1.045, 95% CI [1.031, 1.060]; p < 0.001), higher eGFR (HR 1.084, 95% CI [1.052, 1.117]; p = 0.001), combined with DM (HR 1.471, 95% CI [1.026, 2.110]; p = 0.036), and advanced HF stage (class III versus class 0-I, HR 5.262; 95% CI [3.281, 8.437]; p < 0.001; class IV versus class 0-I, HR 6.409; 95% CI [4.145, 9.912]; p < 0.001). In addition, the predictors of cardiovascular death in diabetic USPD patients included advanced age (HR 1.052, 95% CI [1.027, 1.078]; p < 0.001) and advanced HF stages (class III versus class 0-I, HR 7.843; 95% CI [4.249, 14.476]; p < 0.001; class IV versus class 0-I, HR 5.285; 95% CI [2.880, 9.698]; p < 0.001). Moreover, the predictors of cardiovascular death in elderly USPD patients were advanced age (HR 1.045, 95% CI [1.016, 1.075]; p < 0.001) and advanced HF stages (class III versus class 0-I, HR 3.407; 95% CI [1.911, 6.073]; p < 0.001; class IV versus class 0-I, HR 5.039; 95% CI [2.982, 8.516]; p < 0.001). Risk factors related to cardiovascular death included advanced age, higher eGFR, combined with diabetes, and advanced heart failure stages among USPD patients.
Similar content being viewed by others
Introduction
End-stage renal disease (ESRD) shows a growing incidence globally1,2 which increases the health care burden worldwide3,4. Dialysis is the most frequently adopted type of kidney replacement treatment (78%) compared with kidney transplantation5. Urgent-start hemodialysis requires vascular access via central venous catheter (CVC), which is associated with a high risk of bloodstream infection, an increased medical cost and a higher risk of mortality6. A portion of CVC patients suffer from complications like uncapped ports, perforation, accidental removal, and disconnection from the extracorporeal circuit, leading to fatal vascular access hemorrhage and contributing to deaths among patients receiving hemodialysis7. Urgent-start peritoneal dialysis (USPD) is to initiate peritoneal dialysis (PD) in 2 weeks8 and it has been demonstrated with high safety and practicability for uremia patients who are referred late to dialysis9,10.
Great efforts have been made to combat cardiovascular disease (CVD) worldwide. Notably, chronic kidney disease (CKD) usually occurs accompanied by CVD11. Overall, most CKD patients are associated with a higher risk of CVD death than progression to kidney failure12. The CVD-induced mortality in ESRD patients increases by 20 folds relative to the general population13,14. Similarly, cardiovascular death represents the most common factor inducing mortality among PD patients15. Therefore, investigating the prognostic factors for cardiovascular death and discovering potential treatment targets are of great clinical significance for PD patients, especially for those with USPD who are in emergency. However, data regarding cardiovascular death in USPD patients are scarce. To our knowledge, risk factors related to cardiovascular death in USPD patients are not identified for the time being. Consequently, we conducted the present work for assessing cardiovascular death and examining the probable risk factors among USPD cases.
Materials and methods
Objects of study
We carried out the present multicenter retrospective cohort study in five centers from Northeast China, including the Second Hospital of Jilin University, the second part of The First Hospital of Jilin University, Jilin Central Hospital, Xing’an League People’s Hospital, and Jilin FAW General Hospital. We enrolled adults initiating PD between January 1st, 2013 and 31st, December 2019, and excluded those who had insufficient records, or initiated PD after 2 weeks following catheter insertion. The enrolled patients were followed up till the occurrence of one or more events below: technical failure, death, loss-to-follow-up, and renal transplantation. This study was conducted following relevant ethical requirements. This retrospective study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Second Hospital of Jilin University (No. 2020031). The requirement for informed consent was waived by the Ethics Committee of the Second Hospital of Jilin University due to the retrospective nature of the study and the use of anonymized data.
Data extraction
PD therapy was performed with integrated Y-sets and Double-cuff Tenckhoff straight catheters. Educated and experienced physicians and nurses were responsible for conducting PD training. Following insertion, dialysis solution (500 mL) was added to irrigate the catheter for four times. The commercial glucose-based PD solutions (Huaren Pharmaceutical Ltd. China or Baxter Healthcare Guangzhou Ltd. China) were utilized in each patient. The glucose contents in dialysis prescriptions were 1.5%, 2.5% and 4.25%, and exchange frequency and volume were determined according to patient requirements. Each patient underwent low-volume PD exchanges in the supine position, and the initial exchange volumes were about 0.65–1.5 L, which were directly supervised by a PD nurse in the automated peritoneal dialysis (APD) and continuous ambulatory peritoneal dialysis (CAPD) pattern. We determined the fill volume based on patient weight, and later gradually increased it to 2 L per cycle in 2 weeks. CAPD patients received 3–4 exchanges every day, whereas APD patients received 6–9 cycles every day. PD initiation was conducted using the decremental method in patients experiencing primarily fluid retention, which was initiated with the 4.25% glucose dialysate solution down to the 1.5% glucose solution. Meanwhile, for patients developing the primarily uremic syndrome, the maximum prescription PD method with 1.5% glucose solution was proposed. Upon the completion of 2 weeks USPD treatment, patients were discharged from hospital and continued the standard home-based CAPD or APD. CAPD patients received an exchange volume of 2 L in each cycle for 3–5 cycles every day; whereas APD patients received an exchange volume of 2 L in each cycle for 3–5 cycles at night and 0–2 manual exchanges during daytime. Additionally, treatment protocols were adjusted according to patients’ clinical manifestations in follow-up. Baseline data within one week prior to PD catheter implantation included demographic data [age, sex, protopathy (with glomerulonephritis group being a control for analysis), with diabetes mellitus (DM), with hypertension, heart failure (HF) stage16,17 (those without functional limitations (class 0), with occasional effort dyspnoea (class I), with HF symptoms on ordinary exertion (class II), on less-than-ordinary exertion (class III), or at rest (class IV), antibiotic application before admission], and biochemical data (serum white cell count, hemoglobin, serum albumin, serum urea nitrogen, serum creatinine, estimated glomerular filtration rate (eGFR) (by CKD-EPI creatinine equation), serum sodium, serum potassium, serum calcium, serum phosphorus, and blood glucose). Standard laboratory technologies were employed for biochemical measurements.
Definition of study outcomes
Cardiovascular death was our primary endpoint, which referred to death with a definite cardiovascular cause or death not definitely induced by a noncardiovascular cause18. Censoring events encompassed technical failure, loss-to-follow-up, and renal transplantation. Technical failure referred to the permanent PD cessation and transfer to hemodialysis.
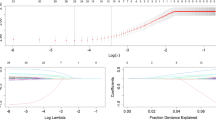
Statistical analysis
Normally-distributed parametric continuous data were indicated by mean ± standard deviation (SD) and analyzed with Student’s t-test. Whereas non-normally-distributed continuous data were indicated by median (Q1-Q3), and examined with Wilcoxon’s rank-sum test. Categorical data were indicated by frequency (percentage) and analyzed by chi-square (χ2) test. In follow-up, cumulative hazard of cardiovascular death was assessed by plotting Kaplan-Meier survival curves. Risk factors related to USPD outcomes were analyzed by Cox proportional hazard analysis. Given the collinearity between serum creatinine and eGFR, only eGFR (and not serum creatinine) was included in the multivariable regression models. Covariates in the Cox model satisfying P < 0.05 upon univariate analysis were used for multiple Cox regression. We carried out the forward elimination process for identifying factors independently predicting cardiovascular death. Data were indicated by hazard ratio (HR) as well as 95% confidence interval (CI). SPSS (version 24.0, IBM, New York, USA) and survival package in R (version 4.3.3) were adopted for statistical analysis. P < 0.05 (two-sided) stood for statistical significance. GraphPad Prism (version 8.0) was employed for plot drawing.
Results
Baseline features of 1549 USPD patients
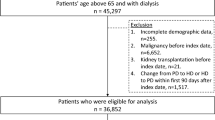
A total of 1549 cases initiating USPD between 2013 and 2019 were enrolled into the present work. There were 56.6% of male participants. Meanwhile, the median age of initiating USPD treatment was 55. The elderly accounted for 38.5% of all patients, and 36.7% of them had diabetic mellitus (DM). Table 1 displays baseline patient features.
Mortality and cause of deaths
Of these 1549 patients, cardiovascular death occurred in 123 patients, accounting for 41.4% of the total deaths, and the cardiovascular death risk was highest within the initial 6 months (30.1%). Figure 1a and b display the cumulative survival curves of cardiovascular death in USPD and that stratified by DM. Cardiovascular death was significantly different between DM and non-DM in USPD patients. Cumulative survival curve of cardiovascular death in USPD stratified by age is displayed in Fig. 1c. Clearly, cardiovascular death was significantly different in elderly compared with non-elderly among USPD patients.
Cumulative survival curves for the cardiovascular death in the overall USPD patients and stratified by diabetes and age. (a) Cumulative survival curves for the cardiovascular death in the overall USPD patients; (b) Cumulative survival curves for the cardiovascular death in the overall USPD patients stratified by diabetes; (c) Cumulative survival curves for the cardiovascular death in the overall USPD patients stratified by age.
Risk factors related to cardiovascular death among overall USPD patients
Univariate Cox regression identified advanced age, combined with DM, higher blood glucose, higher eGFR, lower BUN, lower potassium, lower albumin and advanced HF stages as predicting factors for cardiovascular death. According to multivariate regression, advanced age (HR 1.045, 95%CI [1.031, 1.060]; p < 0.001), higher eGFR (HR 1.084, 95%CI [1.052, 1.117]; p = 0.001), combined with DM (HR 1.471, 95%CI [1.026, 2.110]; p = 0.036), and advanced HF stage (class III versus class 0-I, HR 5.262; 95% CI [3.281, 8.437]; p < 0.001; class IV versus class 0-I, HR 6.409; 95%CI [4.145, 9.912]; p < 0.001) were related to cardiovascular death (Fig. 2).
Risk factors related to cardiovascular death among diabetic USPD patients
There were altogether 568 diabetics among USPD patients. Univariate Cox regression demonstrated advanced age and advanced HF stages as predicting factors for cardiovascular death. While in the multivariate regression, advanced age (HR 1.052, 95%CI [1.027, 1.078]; p < 0.001) and advanced HF stages (class III versus class 0-I, HR 7.843; 95%CI [4.249, 14.476]; p < 0.001; class IV versus class 0-I, HR 5.285; 95%CI [2.880, 9.698]; p < 0.001) (Fig. 3a) were risk factors related to cardiovascular death.
Risk factors related to cardiovascular death in non-diabetic USPD patients
Univariate Cox regression suggested lower serum albumin, higher blood glucose, higher phosphorus, higher eGFR, BUN, advanced age and advanced HF stages as predicting factors for cardiovascular death. While multivariate regression identified that advanced age (HR 1.042, 95%CI [1.024, 1.061]; p < 0.001), higher eGFR (HR 1.091, 95%CI [1.056, 1.126]; p < 0.001), higher blood glucose (HR 1.203, 95%CI [1.051, 1.337]; p = 0.007) and advanced HF stage (class III versus class 0-I, HR 2.898; 95%CI [1.351, 6.216]; p = 0.006; class IV versus class 0-I, HR 8.316; 95%CI [4.467, 15.480]; p < 0.001) (Fig. 3b) as risk factors related to cardiovascular death.
Risk factors for cardiovascular death among elderly USPD patients
There were altogether 596 elderly USPD patients (≥ 60 years). Univariate Cox regression identified advanced age, higher blood glucose and advanced HF stages as predicting factors for cardiovascular death. While multivariate regression suggested advanced age (HR 1.045, 95%CI [1.016, 1.075]; p < 0.001) and advanced HF stages (class III versus class 0-I, HR 3.407; 95%CI [1.911, 6.073]; p < 0.001; class IV versus class 0-I, HR 5.039; 95%CI [2.982, 8.516]; p < 0.001) were risk factors associated with cardiovascular death (Fig. 4a).
Risk factors related to cardiovascular death among non-elderly USPD patients
Univariate Cox regression demonstrated lower serum albumin, higher blood glucose, lower phosphorus, higher eGFR, BUN, DM and advanced HF stages as predicting factors for cardiovascular death. Whereas multivariate regression suggested higher eGFR (HR 1.091, 95%CI [1.060, 1.124]; p < 0.001), DM (HR 2.081, 95%CI [1.112, 3.894]; p = 0.022) and advanced HF stages (class III versus class 0-I, HR 9.960; 95%CI [4.377, 22.667]; p < 0.001; class IV versus class 0-I, HR 11.097; 95%CI [5.087, 24.206]; p < 0.001) were risk factors for cardiovascular death (Fig. 4b).
Discussion
In our study, we found that cardiovascular death represented a leading factor inducing mortality among USPD patients. Risk factors related to cardiovascular death were advanced age, higher eGFR, combined with DM, and advanced HF stages. After stratification by age and DM, advanced HF stage was a powerful risk factor related to cardiovascular death. Besides, there were different risk factors for cardiovascular death in DM and non-DM or in elderly and non-elderly USPD patients.
Cardiovascular death was the major factor inducing mortality, which occupied 41.4% of total deaths in USPD patients in our study, consistent with the current relevant research. CVDs can greatly threaten human health, which show unexceptionally high morbidity and mortality rates and account for a major factor inducing mortality among ESRD patients19,20. Similar to hemodialysis, nearly 50% of PD deaths are caused by cardiovascular events, and more and more efforts are made to identify modality-specific factors that promote such events21. A study finds that age, blood pressure, body mass index, fasting glucose, serum lipids, sodium, phosphorus, albumin, and total protein are strong predicting factors for cardiovascular death of PD22. Typically, the triglyceride-glucose index contributes to predicting 1-year major adverse cardiovascular events among ESRD patients with concurrent coronary artery disease23. Moreover, IL-6 is the most creditable factor predicting CVD and death among ESRD patients24. USPD is an important option for CKD patients who require urgent kidney replacement, since it is convenient for home-based therapy25. Risk factors in USPD are not entirely consistent with those in the ESRD and routine PD populations, which may be because such patients may delay treatment and experience more serious complications. Health professionals should offer appropriate care and instructions to patients who are making the decision to receive dialysis treatment26. Better education on PD and better control of body weight, blood pressure, fasting glucose, serum lipids, sodium, phosphorus, albumin, and IL-6 may help reduce cardiovascular events in USPD treatment.
HF represents the complicated syndrome resulting from damage to the cardiac structure or function, which is usually the end stage of different CVDs. HF still shows a high prevalence, leads to a high mortality rate, and brings a substantial disease burden worldwide27. Due to the decrease in kidney function, the HF prevalence increases, about 44% of dialysis patients develop HF, while 50% of them experience decrease ejection fraction28. Patients undergoing long-term dialysis are inclined to develop HF and are associated with high mortality and morbidity rates29,30. HF patients on dialysis are linked with dismal prognostic outcome, and the 5-year survival rate is reported to be 12.5%31. According to FIGARO-DKD analysis results, finerenone decreased the newly-onset HF and improved additional HF outcomes among type 2 diabetes and CKD patients32. However, the use of finerenone in ESRD is prohibitive. The mechanism of HF is multiple. Notably, the dysregulated cell death enhances the CVDs pathogenesis, which can be a promising clinical treatment target. ROS generation has been suggested to be tightly associated with cell death, which can promote CVDs genesis and progression19. The impaired mitochondrial bioenergetics is related to HF33. Interventions targeting the mitochondrial bioenergetics and ROS may be meaningful for ESRD patients with HF.
DM represents a rapid-growing disorder globally, and type 2 diabetes mellitus accounts for a major factor inducing kidney failure worldwide34. DM may usually occur with CVDs. Atherosclerosis and progressive immune inflammation are mostly asymptomatic and silent in diabetic patients35. Devastating CVDs and diabetic kidney disease lead to an increased mortality rates, and an overall decreased quality of life in individuals with DM36. PD has been identified as the efficient renal replacement treatment in diabetic patients37. Meanwhile, PD is suitable for patients with concurrent CVDs, since PD patients with and without CVDs share similar laboratory and clinical targets, hospitalizations, peritonitis rates, and technical survivals38. However, coronary artery calcification progresses rapidly among dialysis patients, which leads to a higher risk of death39. The relation of DM with poor cardiovascular prognosis among PD patients involves many factors. Firstly, the poor glycemic control may be incrementally related to the increased mortality among diabetic PD patients40. Secondly, patients with DM exhibit inferior nutritional status, which is associated with all-cause hospitalizations41. Thirdly, insulin resistance is correlated with microvascular and macrovascular consequences, and PD can result in the increased glucose levels, which serves as the continuous insulin-secretagogue stimulus and probably exacerbate insulin resistance among PD patients with DM42. Consequently, it is desirable to lower glucose level in PD solutions and investigate novel hypoglycemic strategies with pharmacological effects without direct insulin injection. For patients with kidney disease and type 2 diabetes, canagliflozin is found to induce a decreased risk of cardiovascular events and kidney failure at the median of 6.2-year follow-up. However, effective drugs for treating diabetic ESRD are lacking34. At present, no evidence has supported using therapeutic agents like mineralocorticoid receptor antagonist or sodium-glucose cotransporter 2 inhibitor for DM in ESRD43. More clinical trials of drugs for improving the prognosis of diabetic ESRD patients are urgently needed.
Advanced age was associated with cardiovascular death among USPD patients in the present work. CVD accounts for the major cause inducing disability and mortality worldwide among the elderly44,45,46. The same is true for PD patients. Typically, cardiovascular events are the most frequently seen cause of death among elderly PD patients47. Ischemic heart disease is especially a risk factor related to the long-time prognosis in elderly PD patients48. Platelet dysregulation shows an apparently increasing trend with age, which facilitates to make CVD a major factor inducing mortality among the elderly49. Moreover, accidental falls can be quite frequent among PD patients, which may be usually unrecognized. Falls are related to a higher risk of mortality in elderly PD50. The care of elderly patients with PD is particularly important. Of course, the use of cardiovascular medications among elderly patients with PD would be of great importance too. The existing statin therapy is beneficial for primarily preventing adverse results, all-cause death or stroke among Koreans with the age of ≥ 75 years51. In a study, adult patients receiving maintenance hemodialysis, statin therapy, preferably plus ezetimibe, were related to the reduced all-cause mortality risk52. Statin therapy is related to the markedly decreased total cholesterol, low-density lipoprotein cholesterol, and C-reactive protein levels, but the possible benefits of statin for CVD risk among PD patients are not definitely concluded yet53. More high-quality studies should be conducted for assessing the possible benefits of statin therapy for elderly USPD patients.
The increased eGFR level initiating dialysis was related to cardiovascular death in our study. Similar findings were found in another study showing that initiating PD early was related to the increased cardiovascular death risk in elderly patients54. It is reasonable to speculate that patients starting dialysis at the high eGFR level may be associated with a greater risk of comorbidities. Moreover, a study showed that the higher eGFR level was related to low fluctuation of hemoglobin and led to unfavorable cardiovascular outcome55which further explained our findings. Baseline eGFR levels vary widely in different PD clinical studies, which may play a role in the heterogeneity of study population. In conclusion, early dialysis has adverse effects on the prognosis of the USPD population.
The present work has the main strengths below. As far as we know, the present work is the first to determine potential risk factors related to cardiovascular death among USPD patients. Nonetheless, there are certain limitations. Firstly, this retrospective study inevitably led to some bias. Secondly, our study did not examine the relation of time-varying values with mortality. Thirdly, our study relied on the NYHA functional class for the assessment of heart failure severity, which, while clinically relevant, is subjective and may be prone to misclassification. Moreover, objective measures of cardiac function, such as left ventricular ejection fraction (LVEF) and other echocardiographic indices, were not available in our dataset. Given the well-established prognostic value of LVEF, particularly in the dialysis populations, the absence of such data is a significant limitation to be noted. Future studies incorporating comprehensive echocardiographic assessments will provide further insights into the relationship between cardiac function and cardiovascular outcomes in this patient population. Consequently, more large prospective researches regarding the cardiovascular prognostic outcome in USPD patients should be conducted.
Conclusion
To sum up, risk factors for cardiovascular death include advanced age, high eGFR, combined with DM, and advanced HF stages among USPD patients.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
McCullough, K. P., Morgenstern, H., Saran, R., Herman, W. H. & Robinson, B. M. Projecting ESRD incidence and prevalence in the united States through 2030. J. Am. Soc. Nephrology: JASN. 30, 127–135. https://doi.org/10.1681/asn.2018050531 (2019).
Johansen, K. L. et al. Epidemiology of Kidney Disease in the United States. Am. J. kidney diseases: official J. Natl. Kidney Foundation 81, A8–a11 https://doi.org/10.1053/j.ajkd.2022.12.001 (2023).
Thurlow, J. S. et al. Global epidemiology of End-Stage kidney disease and disparities in kidney replacement therapy. Am. J. Nephrol. 52, 98–107. https://doi.org/10.1159/000514550 (2021).
Tang, S. C. W. et al. Dialysis care and Dialysis funding in Asia. Am. J. Kidney Diseases: Official J. Natl. Kidney Foundation. 75, 772–781. https://doi.org/10.1053/j.ajkd.2019.08.005 (2020).
Lok, C. E., Huber, T. S., Orchanian-Cheff, A. & Rajan, D. K. Arteriovenous access for hemodialysis: A review. Jama 331, 1307–1317. https://doi.org/10.1001/jama.2024.0535 (2024).
Agarwal, A. K. & Roy-Chaudhury, P. Taurolidine/Heparin lock solution and Catheter-Related bloodstream infection in hemodialysis: A randomized, Double-Blind, Active-Control, phase 3 study. 18, 1446–1455 https://doi.org/10.2215/cjn.0000000000000278 (2023).
Keiko, I., Michael, J. & Hemodialysis Emergencies, C. G., Core Curriculum American journal of kidney diseases: the official journal of the National Kidney Foundation 77, https://doi.org/10.1053/j.ajkd.2020.11.024 (2021).
Xieyi, G., Xiaohong, T., Xiaofang, W. & Zi, L. Urgent-start peritoneal Dialysis in chronic kidney disease patients: A systematic review and meta-analysis compared with planned peritoneal Dialysis and with urgent-start Hemodialysis. 41, 179–193 https://doi.org/10.1177/0896860820918710 (2021).
Xu, D., Liu, T. & Dong, J. Urgent-Start peritoneal Dialysis complications: prevalence and risk factors. Am. J. Kidney Diseases: Official J. Natl. Kidney Foundation. 70, 102–110. https://doi.org/10.1053/j.ajkd.2016.12.021 (2017).
Hu, X. et al. Break-in period ≤ 24 hours as an option for Urgent-start peritoneal Dialysis in patients with diabetes. Front. Endocrinol. 13, 936573. https://doi.org/10.3389/fendo.2022.936573 (2022).
Imaizumi, T. et al. Excess risk of cardiovascular events in patients in the united States vs. Japan with chronic kidney disease is mediated mainly by left ventricular structure and function. Kidney Int. 103, 949–961. https://doi.org/10.1016/j.kint.2023.01.008 (2023).
KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 105, S117–s314 https://doi.org/10.1016/j.kint.2023.10.018 (2024).
Cozzolino, M. et al. Cardiovascular disease in dialysis patients. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 33, iii28-iii34 https://doi.org/10.1093/ndt/gfy174 (2018).
Lai, A. C. et al. A personalized approach to chronic kidney disease and cardiovascular disease: JACC review topic of the week. J. Am. Coll. Cardiol. 77, 1470–1479. https://doi.org/10.1016/j.jacc.2021.01.028 (2021).
Krediet, R. T. & Balafa, O. Cardiovascular risk in the peritoneal Dialysis patient. Nat. Rev. Nephrol. 6, 451–460. https://doi.org/10.1038/nrneph.2010.68 (2010).
Hunt, S. A. et al. ACC/AHA. Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation 112, e154-235 https://doi.org/10.1161/circulationaha.105.167586 (2005).
Postorino, M., Marino, C., Tripepi, G. & Zoccali, C. Prognostic value of the new York heart association classification in end-stage renal disease. Nephrol. Dialysis Transplantation: Official Publication Eur. Dialysis Transpl. Association - Eur. Ren. Assoc. 22, 1377–1382. https://doi.org/10.1093/ndt/gfl813 (2007).
Bonaca, M. P. et al. American college of cardiology/american heart association/european society of cardiology/world heart federation universal definition of myocardial infarction classification system and the risk of cardiovascular death: observations from the TRITON-TIMI 38 trial (Trial to assess improvement in therapeutic outcomes by optimizing platelet Inhibition with Prasugrel-Thrombolysis in myocardial infarction 38). Circulation 125, 577–583. https://doi.org/10.1161/circulationaha.111.041160 (2012).
Xu, T., Ding, W., Ji, X., Ao, X. & Liu, Y. Oxidative Stress in Cell Death and Cardiovascular Diseases. 9030563 https://doi.org/10.1155/2019/9030563 (2019).
Jankowski, J., Floege, J., Fliser, D., Böhm, M. & Marx, N. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation 143, 1157–1172. https://doi.org/10.1161/circulationaha.120.050686 (2021).
Mehrotra, R., Devuyst, O., Davies, S. J. & Johnson, D. W. The current state of peritoneal Dialysis. J. Am. Soc. Nephrology: JASN. 27, 3238–3252. https://doi.org/10.1681/asn.2016010112 (2016).
Yu, D. et al. Development and validation of risk prediction models for cardiovascular mortality in Chinese people initialising peritoneal dialysis: a cohort study. Sci. Rep. 8, 1966. https://doi.org/10.1038/s41598-018-20160-3 (2018).
Xie, E. et al. The triglyceride-glucose index predicts 1-year major adverse cardiovascular events in end-stage renal disease patients with coronary artery disease. Cardiovasc. Diabetol. 22, 292. https://doi.org/10.1186/s12933-023-02028-7 (2023).
Honda, H. et al. Serum albumin, C-reactive protein, Interleukin 6, and fetuin a as predictors of malnutrition, cardiovascular disease, and mortality in patients with ESRD. Am. J. Kidney Diseases: Official J. Natl. Kidney Foundation. 47, 139–148. https://doi.org/10.1053/j.ajkd.2005.09.014 (2006).
Alves, C. A. et al. Urgent-Start peritoneal dialysis: Brazilian experience. Blood Purif. 52, 556–563. https://doi.org/10.1159/000529133 (2023).
Lin, M. L. & Chu, K. H. The experience of urgent Dialysis patients with end-stage renal disease: A qualitative study. 17, e0261941 https://doi.org/10.1371/journal.pone.0261941 (2022).
Jia, Y. et al. Effect of air pollution on heart failure: systematic review and Meta-Analysis. Environ. Health Perspect. 131, 76001. https://doi.org/10.1289/ehp11506 (2023).
House, A. A. et al. Heart failure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int. 95, 1304–1317. https://doi.org/10.1016/j.kint.2019.02.022 (2019).
Banerjee, D., Rosano, G. & Herzog, C. A. Management of heart failure patient with CKD. Clin. J. Am. Soc. Nephrology: CJASN. 16, 1131–1139. https://doi.org/10.2215/cjn.14180920 (2021).
Zoccali, C. et al. Cardiovascular complications in chronic kidney disease: a review from the European renal and cardiovascular medicine working group of the European renal association. 119, 2017–2032 https://doi.org/10.1093/cvr/cvad083 (2023).
Banerjee, D., Ma, J. Z., Collins, A. J. & Herzog, C. A. Long-term survival of incident Hemodialysis patients who are hospitalized for congestive heart failure, pulmonary edema, or fluid overload. Clin. J. Am. Soc. Nephrology: CJASN. 2, 1186–1190. https://doi.org/10.2215/cjn.01110307 (2007).
Filippatos, G. & Anker, S. D. Finerenone reduces risk of incident heart failure in patients with chronic kidney disease and type 2 diabetes: analyses from the FIGARO-DKD trial. 145, 437–447 https://doi.org/10.1161/circulationaha.121.057983 (2022).
Zhuang, L., Jia, K. & Chen, C. DYRK1B-STAT3 drives cardiac hypertrophy and heart failure by impairing mitochondrial bioenergetics. 145, 829–846 https://doi.org/10.1161/circulationaha.121.055727 (2022).
Perkovic, V. et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 380, 2295–2306. https://doi.org/10.1056/NEJMoa1811744 (2019).
Esper, R. J. & Nordaby, R. A. Cardiovascular events, diabetes and guidelines: the virtue of simplicity. Cardiovasc. Diabetol. 18, 42. https://doi.org/10.1186/s12933-019-0844-y (2019).
Cole, J. B. & Florez, J. C. Genetics of diabetes mellitus and diabetes complications. Nat. Rev. Nephrol. 16, 377–390. https://doi.org/10.1038/s41581-020-0278-5 (2020).
Gorsane, I. et al. Peritoneal Dialysis in diabetes patients. Tunis. Med. 97, 1017–1020 (2019).
Querido, S. et al. Peritoneal dialysis is a reasonable option in patients with cardiovascular disease Clinical nephrology 87, 111–116 https://doi.org/10.5414/cn108957 (2017).
Haitao, Z. et al. Progression of vascular calcification and clinical outcomes in patients receiving maintenance Dialysis. JAMA Netw. Open 6 https://doi.org/10.1001/jamanetworkopen.2023.10909 (2023).
Duong, U. et al. Glycemic control and survival in peritoneal Dialysis patients with diabetes mellitus. Clin. J. Am. Soc. Nephrology: CJASN 6, 1041–1048. https://doi.org/10.2215/cjn.08921010 (2011).
Grzywacz, A. & Lubas, A. Inferior nutritional status significantly differentiates Dialysis patients with type 1 and type 2 diabetes. 15 https://doi.org/10.3390/nu15071549 (2023).
Lambie, M. et al. Insulin resistance in cardiovascular disease, uremia, and peritoneal Dialysis. Trends Endocrinol. Metab. 32, 721–730. https://doi.org/10.1016/j.tem.2021.06.001 (2021).
Tsapas, A. & Avgerinos, I. Comparative effectiveness of Glucose-Lowering drugs for type 2 diabetes: A systematic review and network Meta-analysis. 173, 278–286 https://doi.org/10.7326/m20-0864 (2020).
Liberale, L. et al. Inflammation, aging, and cardiovascular disease: JACC review topic of the week. J. Am. Coll. Cardiol. 79, 837–847. https://doi.org/10.1016/j.jacc.2021.12.017 (2022).
Evans, M. A., Sano, S. & Walsh, K. Cardiovascular disease, aging, and clonal hematopoiesis. Annu. Rev. Pathol. 15, 419–438. https://doi.org/10.1146/annurev-pathmechdis-012419-032544 (2020).
Wu, Q. & Zhao, Y. Trend, regional variation and socioeconomic inequality in cardiovascular disease among the elderly population in china: evidence from a nationwide longitudinal study during 2011–2018. 8 https://doi.org/10.1136/bmjgh-2023-013311 (2023).
Gao, L. et al. Outcomes of elderly peritoneal Dialysis patients: 65–74 years old versus ≥ 75 years old. Ren. Fail. 45, 2264977. https://doi.org/10.1080/0886022x.2023.2264977 (2023).
Ma, X. Y. et al. Characteristics and prognostic outcome factors between young and elderly peritoneal Dialysis patients: a prospective cohort study. Annals Palliat. Med. 11, 2952–2960. https://doi.org/10.21037/apm-22-1008 (2022).
Poscablo, D. M. et al. An age-progressive platelet differentiation path from hematopoietic stem cells causes exacerbated thrombosis. Cell 187, 3090–3107e3021. https://doi.org/10.1016/j.cell.2024.04.018 (2024).
Farragher, J. et al. Accidental falls and risk of mortality among older adults on chronic peritoneal Dialysis. Clin. J. Am. Soc. Nephrology: CJASN. 9, 1248–1253. https://doi.org/10.2215/cjn.11001013 (2014).
Jun, J. E. et al. Statins for primary prevention in adults aged 75 years and older: A nationwide population-based case-control study. Atherosclerosis 283, 28–34. https://doi.org/10.1016/j.atherosclerosis.2019.01.030 (2019).
Jung, J., Bae, G. H., Kang, M., Kim, S. W. & Lee, D. H. Statins and All-Cause mortality in patients undergoing Hemodialysis. J. Am. Heart Assoc. 9, e014840. https://doi.org/10.1161/jaha.119.014840 (2020).
Lee, D. Y. et al. Improvement of clinical outcomes in patients undergoing peritoneal Dialysis using hydroxymethylglutaryl-CoA reductase inhibitors: A systematic review and meta-analysis. J. Chin. Med. Association: JCMA. 86, 155–165. https://doi.org/10.1097/jcma.0000000000000840 (2023).
Peng, Y. et al. Early initiation of PD therapy in elderly patients is associated with increased risk of death. 14 1649-1656 https://doi.org/10.1093/ckj/sfaa214 (2021).
Liu, D. et al. High hemoglobin fluctuation was a protective factor for cardiovascular-related death in peritoneal Dialysis (PD) patients: A retrospective analysis of 232 patients with PD. J. Clin. Lab. Anal. 36, e24548. https://doi.org/10.1002/jcla.24548 (2022).
Acknowledgements
We are grateful to all staff of the five peritoneal dialysis centers, whose assistance in data collection and follow-up made this paper possible.
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly to the manuscript. Ling-Fei Meng analyzed the data and wrote the manuscript; Li-Ming Yang, Xue-Yan Zhu, Zhan-Shan Sun, and Xiao-Xuan Zhang provided the data and confirm the accuracy of data; and Wen-Peng Cui designed the study and reviewed the manuscript. All the authors have approved and agreed to this study and manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics declarations
The requirement for informed consent was waived by the Ethics Committee of the Second Hospital of Jilin University due to the retrospective nature of the study and the use of anonymized data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Meng, L., Yang, L., Zhu, X. et al. Risk factors for cardiovascular death in urgent-start peritoneal dialysis patients: a multicenter retrospective cohort study. Sci Rep 15, 33527 (2025). https://doi.org/10.1038/s41598-025-18015-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18015-9