Abstract
Abnormalities in lipid metabolism play an important role in diabetic macular edema (DME), and the aim of this study was to investigate the correlation between ApoB/A1 levels and best corrected visual acuity (BCVA) and macular microstructural changes in DME patients after anti-VEGF treatment. Through a retrospective cohort analysis of 61 patients (61 eyes) with non-proliferative diabetic retinopathy combined with macular edema treated with 3 + PRN anti-VEGF regimen and followed up for three months, grouped by median ApoB/A1, the differences between the efficacy indexes of the two groups were compared. The results showed that the macular edema regression rate was significantly higher in the high ApoB/A1 ratio group than in the low ratio group at one month after treatment(P < 0.05), and at three months after treatment, the high ApoB/A1 ratio group was better than the low ratio group in BCVA improvement (58.1% vs. 26.7%), inner retinal layer restoration (38.7% vs. 10.0%), and hyperreflective foci (HF) reduction (41.9% vs. 6.7%). aspects were better than those in the low ratio group (P < 0.05). The results of ordered logistic regression analysis showed that the ApoB/A1 ratio was significantly correlated with the change in macular edema at one month after treatment and the change in the number of HF at three months after treatment. Conclusions showed that the ApoB/A1 ratio was significantly correlated with short-term improvement of BCVA and macular microstructure after anti-VEGF treatment in DME patients, and it is expected to be used as an objective biomarker for assessing the efficacy of anti-VEGF treatment in DME patients.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is a major microvascular complication of diabetes mellitus, involving about 30%-40% of diabetic patients1with diabetic macular edema (DME) as a serious complication threatening vision2. Due to its pathophysiologic mechanism, although anti-VEGF treatment is the first-line option3there are problems such as large individual differences in efficacy, high treatment cost and continuous deterioration of vision in some patients. Recent studies have found that abnormalities in lipid metabolism are closely related to the progression of DME4Increased blood viscosity, plasma lipoprotein leakage, and blood stasis caused by hyperlipidemia induce ischemic and hypoxic damage to retinal tissues, which accelerates macular vascular leakage. However, studies such as the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR)5and Diabetes Control and Complications Trial (DCCT)6have found significant heterogeneity in the association of conventional lipoprotein indices with DR and DME, and these indices are susceptible to biological fluctuations due to dietary factors. In contrast, apolipoprotein, as the core structural protein of lipoprotein particles, has a closer molecular association with the pathologic process of DME. Among them, apolipoproteinB (ApoB) is involved in the transport of almost all types of atherogenic lipoproteins such as very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and low-density lipoprotein (LDL), whereas apolipoproteinA1 (ApoA1) focuses on the transport of the anti-atherogenic lipoprotein high-density lipoprotein (HDL) and promotes cholesterol metabolism7,8. Clinical evidence suggests that an elevated ApoB/A1 ratio is significantly and positively correlated with the risk and severity of DME, and the mechanism may involve a dynamic balance between the antiangiogenic properties of ApoA1 and the retinal vasculotoxicity mediated by ApoB9,10suggesting that this ratio may be a biomarker superior to traditional indicators. However, its role in the assessment of anti-VEGF efficacy has not been clarified. In this study, we innovatively integrated ApoB/A1 levels and optical coherence tomography angiography (OCTA) imaging features, and systematically analyzed their multidimensional associations with best corrected visual acuity (BCVA) and OCTA biomarkers in DME patients after anti-VEGF treatment, aiming to construct a precise diagnostic and treatment system of DME, and to provide a new basis for efficacy monitoring and prognostic judgment.
Method
This retrospective cohort study included 61 patients (61 eyes) with nonproliferative diabetic retinopathy with macular edema from 61 patients who were first seen at the Affiliated Eye Hospital of Nanchang University from November 2023 to November 2024 and received the 3 + PRN anti-VEGF regimen. Patients with a history of intraocular surgery within the last 6 months, comorbidities with other fundus pathologies causing macular edema, refractive interstitial clouding that interfered with fundus observation, lipid-lowering therapy, and poor glycemic control of type 2 diabetes mellitus with a HbA1c > 10.0% were excluded. Patients who had not received any form of intravitreal injection or laser treatment in the past, with a central subfield thickness (CST) ≥ 250 μm, or with a CST < 250 μm but with significant visual decline > 0.1 LogMAR or microstructural damage such as leakage or interlayer separation in the macular area as shown by OCTA, were included in this study. All patients enrolled in this study underwent BCVA assessment, OCTA, intraocular pressure measurements, slit-lamp and dilated fundus examinations, and lipid-related markers. The study followed the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Eye Hospital of Nanchang University (YLP20250054). All patients signed an informed consent form.
Biochemical measurements
Fasting (≥ 8 h) blood samples were collected three days before admission for analysis of HbA1C, total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), ApoA1, and ApoB.
BCVA assessment
BCVA was measured using the international standard logarithmic visual acuity scale and recorded after conversion to logMAR units.
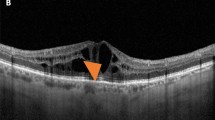
Imaging examinations
A ZEISS Cirrus-HD5000 Optical Coherence Tomograph was used to perform OCTA examination of the patient, capture B-scan images of the horizontal direction of OCTA through the macular central fovea, and record and analyze the following indexes in the retinal area of 6-mm width around the macular central fovea: (1) Central subfield thickness (CST), defined as the vertical length from the inner limiting membrane of the macular central fovea to the upper edge of the RPE reflex. (2) Hyperreflective foci (HF) was defined as focal echogenic lesions distributed within the retinal neuroepithelium with a diameter between 20 and 40 μm and a reflected signal intensity not lower than that of the retinal pigment epithelium11with the number graded according to the criteria of the study by Wen12: a small number of ≤ 10, a moderate number of 11–20, and a large number of > 20. (3) Disorganization of retinal inner layer (DRIL) was defined as disorganization of the hierarchical structure between ganglion cells-inner plexiform layer or inner plexiform layer-outer plexiform layer, and the boundaries were not recognizable13. (4) IO/OS segment, complete continuity of the IO/OS segment is defined as a continuous high reflectance line at the observation level, weakened defined as a irregular reflectance, and interrupted defined as the disappearance of the line reflectance14. All examinations were performed by the same senior ophthalmic technician, and image analysis was performed independently by the same two senior physicians, who were unaware of the effects of anti-VEGF treatment, to ensure standardization of data collection and consistency in interpretation of results.
Evaluation of efficacy after anti-VEGF therapy
Referring to the classification criteria in previous studies, the patients’ BCVA improvement was classified into three categories: decrease in BCVA (ΔBCVA≤-0.1LogMAR), stability in BCVA (-0.1LogMAR < ΔBCVA < 0.1LogMAR), and improvement in BCVA (ΔBCVA ≥ 0.1LogMAR)15. The patients’ macular edema was classified into four categories: persistent edema (CST > 250 μm both before and after treatment), regressed edema (CST > 250 μm before treatment, CST ≤ 250 μm after treatment), incident edema (CST ≤ 250 μm before treatment, CST > 250 μm after treatment), and no edema (CST ≤ 250 μm both before and after treatment)16. Similarly, the structural condition of the retinal inner layer was classified into four categories: persistent DRIL, regressed DRIL, incident DRIL, and no DRIL17,18. The number of HF was categorized into three levels (a small number ≤ 10, a moderate number 11–20, and a large number > 20), and the change in the number of HF was categorized into decreasing, stabilizing, and increasing according to the level at which they were placed before and after anti-VEGF treatment. According to the changes of IO/OS segment, it can be divided into three categories: deterioration, stability and improvement.
Statistical analysis
IBM SPSS 27.0 software was used to statistically analyze the data related to the two groups of patients. The median overall ApoB/A1 ratio of the included subjects was calculated to categorize the patients into two subgroups: high and low. For continuous data, normality was assessed using the Kolmogorov-Smirnov Test and Levene’s test for chi-square. Information that conformed to normal distribution was expressed as mean ± SD, otherwise as median and interquartile range. Two independent samples t-test or Mann-Whitney test was used for statistical analysis between two groups for continuous variables. Categorical variables were expressed as numbers and percentages, and the chi-square test or Fisher exact test was used for statistical analysis between two groups. Ordered logistic regression was used to analyze the risk factors influencing the outcome of anti-VEGF treatment in patients. P < 0.05 was considered statistically significant.
Results
Comparison of baseline characteristics and differences in patients with DME
The study involved 61 patients with DME in 61 eyes, who were categorized into 31 patients with 31 eyes in the high ratio group and 30 patients with 30 eyes in the low ratio group according to the median overall ApoB/A1 ratio. Table 1 shows that both groups had similar general body and ocular conditions at baseline, and the differences shown in lipid parameters can be considered as an effect of the grouping criteria.
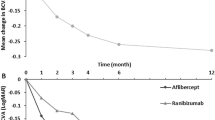
Comparison of changes in BCVA after anti-VEGF treatment compared with pretherapy changes between the two groups
There was no significant difference in the improvement of BCVA between the two groups at one month after anti-VEGF treatment but at three months after treatment, the proportion of patients with improved visual acuity was significantly higher in the group with a high ApoB/A1 ratio than in the group with a low ratio (58.1% vs. 26.7%), and the proportion of patients with stabilized visual acuity was even higher in the group with a low ratio (46.7% vs. 19.4%), which is a statistically significant difference (χ2 = 7.098, P = 0.029)(Table 2).
Comparison of changes in macular edema after anti-VEGF treatment compared with pretherapy changes between the two groups
There was a significant difference in the improvement of macular edema between the two groups after one month of anti-VEGF treatment (P < 0.05). The proportion of patients with high ApoB/A1 ratio who had macular edema regression was significantly higher than that with low ApoB/A1 ratio (35.5% vs. 6.7%), and the proportion of patients with persistent edema was lower (41.9% vs. 70.0%). There was no statistically significant difference between the two groups at three months after treatment (χ2 = 5.566, P = 0.062).(Table 3).
Comparison of changes in retinal inner layer after anti-VEGF treatment compared with pretherapy changes between the two groups
At one month after anti-VEGF treatment, there was no significant difference in the improvement of inner retinal layer between the two groups, and at three months after treatment, the proportion of regressed DRIL was significantly higher in the high ApoB/A1 ratio group than in the low ratio group (38.7% vs. 10.0%), and the proportion of persistent DRIL was higher in the low ratio group (70.0% vs. 45.2%), which was a statistically significant difference (χ2 = 8.104, P = 0.030)(Table 4).
Comparison of the change in the number of HF after anti-VEGF treatment compared with pretherapy changes in the two groups
At one month after anti-VEGF treatment, there was no significant difference in the changes in the number of HF between the two groups, and at three months after treatment, the proportion of HF decreased significantly in the high ApoB/A1 ratio than in the low ratio group (41.9% vs. 6.7%), and the difference was statistically significant (χ2 = 10.230, P = 0.006)(Table 5).
Comparison of the change in continuity of IS/OS segment after anti-VEGF treatment compared with pretherapy changes in the two groups
There was no significant difference in IS/OS segment changes at different time points after anti-VEGF treatment between the two groups (P < 0.05).(Table 6).
Ordered logistic regression analysis of changes in macular edema at one month after treatment
In the logistic regression modeling, the ApoB/A1 ratio was found to be significantly associated with the severity of macular edema at one month after treatment (OR = 28.247, 95% CI: 2.376-335.814, P = 0.008). This suggests a global effect of the ApoB/A1 ratio in predicting a shift toward better clinical outcomes. However, in comparisons of specific thresholds (e.g. persistent edema vs. incident edema and incident edema vs. regressed edema), the correlation did not reach statistical significance (P > 0.05), which may be due to the limited power of the subgroup analysis. Other factors did not correlate (P > 0.05) with the severity of macular edema outcomes at one month after treatment.(Table 7).
Ordered logistic regression analysis of changes in BCVA at three months after treatment
In the logistic regression model, the ApoB/A1 ratio was found to be non-significantly associated with the change in BCVA at three months after treatment (OR = 1.593, 95% CI: 0.435–5.837, P = 0.482). Other factors such as age, gender and LDL-C level were not significantly associated with changes in BCVA after three months of treatment. (P > 0.05)(Table 8).
Ordered logistic regression analysis of changes in the number of HF at three months after treatment
In the logistic regression model, the ApoB/A1 ratio was found to be significantly correlated with the change in the number of HF at three months after treatment (OR = 28.247, 95% CI: 2.376-335.814, P = 0.008). In particular, for each unit increase in the ApoB/A1 ratio, the probability of the number of HF changing from stable to decreased increased 51.026-fold and the correlation was statistically significant (P > 0.05). There was no correlation (P > 0.05) between age, gender, and LDL-C level and the change of HF number at three months after treatment.(Table 9).
P < 0.05 was statistically significant.
Ordered logistic regression analysis of changes in DRIL at three months after treatment
In the logistic regression model, no significant correlation was found between the ApoB/A1 ratio, age, gender, and LDL-C level and the changes in the inner retinal structure at three months after treatment (P > 0.05).(Table 10).
Discussion
In this study, we found that ApoB/A1 ratio was associated with the response to anti-VEGF efficacy in DME patients by grouping DME patients with different ApoB/A1 ratio levels (high and low level groups) and comparing the changes in relevant indexes before and after anti-VEGF treatment. We followed up the two groups for three months and found that at one month after treatment, there was no significant difference in the improvement of BCVA, retinal inner layer, the number of HF and IS/OS segment between the two groups, while the improvement of macular edema showed a significant difference. Patients with low levels of ApoB/A1 were more inclined to have persistent macular edema and patients with high levels were more inclined to have regression of macular edema. At three months after treatment, the two groups showed significant differences in BCVA, inner retinal layer, and the number of HF. Patients with high levels of ApoB/A1 were more likely to show improvement, such as an increase in BCVA, restoration of retinal inner layer, and a decrease in the number of HF, while patients with low levels were more likely to show persistence or progression of the disease. The ordered logistic regression analysis showed that the ApoB/A1 ratio was significantly and independently associated with the changes of macular edema one month after treatment and HF three months after treatment. This suggests that abnormal lipid metabolism may play an important role in the pathophysiologic process of DME and influence the efficacy of anti-VEGF therapy.
Notably, the present study observed a positive correlation between the ApoB/A1 ratio and the response to anti-VEGF therapy, which is not the same as the results of previous studies, and this finding has led us to put forward a new thought on the traditional lipid pathology theory. Normally, in the lipid metabolism system, ApoA1, as a major component of HDL, not only promotes cholesterol metabolism, but also has an anti-angiogenic effect, which may delay the progression of DR by inhibiting pathologic neovascularization, whereas ApoB, as a major component of LDL, may exacerbate the pathologic progression of DR and DME by activating the oxidative stress response and the release of pro-inflammatory factors that aggravate the dysfunction of the blood-retinal barrier and DME pathology9,19. Previous studies have confirmed that ApoA1 is one of the novel independent risk markers for DR9and Soedarman20 et al. found that the risk of DME was significantly reduced for every 10 mg/dL increase in ApoA1 levels. In contrast, an increase in the ApoB/A1 ratio was associated with an elevated risk of DME, suggesting that alterations in the balance between these apolipoproteins may play a key role in the development of the disease. High levels of the ApoB/A1 ratio, which may reflect an increased risk of dyslipidemia and vascular disease, showed a positive effect in this study, with an increase in the ratio correlating with a better therapeutic outcome, an apparent contradiction that may involve the heterogeneity of lipid function in retinal diseases.
Recent studies21,22 on the differential pathologic effects of HDL in age-related macular degeneration (AMD) and coronary artery disease (CAD) have found that HDL, which promotes reverse cholesterol transport, improves endothelial function, and reduces the risk of CAD23is positively associated with the development of AMD24,25. The occurrence of this phenomenon seems to suggest that the clinical value of lipoprotein metabolic markers needs to be reassessed in relation to disease-specific mechanisms. In AMD, elevated HDL may be converted into dysfunctional pro-oxidant and pro-inflammatory particles that impede cholesterol efflux and promote aberrant accumulation of oxidative metabolites in Bruch’s membrane, which ultimately drives the progression of AMD26,27. Meanwhile, studies have shown that LDL reduces lipid deposition in the Bruch membrane by down-regulating the expression of retinal pigment epithelial (RPE) cell surface receptors and exerts a preventive effect on AMD28. Genomic studies have further confirmed that key genetic variants in lipid metabolism influence AMD risk by regulating HDL/LDL balance29,30.
Based on the specific pathogenesis of HDL in AMD, we hypothesized that it may be involved in the developmental process of DME through similar pathways. As a major component of HDL, there is a significant correlation between the biological activity of ApoA1 and the functional status of HDL. The retina, as a special neural tissue continuously exposed to light radiation, is highly susceptible to photo-oxidation31and in the state of high glucose, the dysfunction of high levels of HDL is accompanied by a decrease in the activity of ApoA1, which leads to an impairment of oxidized lipid scavenging, thus exacerbating the endothelial damage of the retinal vasculature. Meanwhile, it has been pointed out that high levels of HDL dysfunction are associated with elevated serum levels of CRP and overactivation of the complement system, which may laterally suggest that lipoproteins may influence anti-VEGF efficacy indirectly by affecting the inflammatory pathway32. In addition, studies have shown that ApoA1 overexpression in the retina of diabetic patients is an early pathological feature33and the aqueous humor apolipoprotein profile is significantly altered and ApoA1 is significantly elevated during the progression of DR34suggesting that the decrease in the ApoB/A1 ratio may originate from the body’s compensatory response to oxidative damage, i.e., by up-regulating the synthesis of ApoA1 in order to enhance the ability of lipid clearance, but this compensatory mechanism may fail to be effective in improving clinical outcomes due to local microenvironmental disturbances.
In conclusion, the present study innovatively explored the value of ApoB/A1 ratio in the assessment of the efficacy of anti-VEGF therapy in patients with DME, and the significant elevation of ApoB/A1 ratio may have a profound positive effect on the visual prognosis of patients with DME through the sophisticated regulation of the balance of the intricate network of lipids-inflammation-oxidative stress, which is expected to serve as a novel biomarker for predicting the efficacy of anti-VEGF therapy in patients with DME. However, there are some limitations in our study: 1. The small sample size and short follow-up time of this study are not yet sufficient to assess the long-term effect of ApoB/A1 ratio on the efficacy of anti-VEGF therapy in patients with DME.2. The condition of patients with NPDR was not classified (such as mild, moderate, and severe NPDR) through FFA. Subgroup analyses of grading and subtyping of DME have not yet been performed in the present study.3. Although a statistically significant positive correlation was found between the ApoB/A1 ratio and short-term BCVA and macular microstructural changes after anti-VEGF treatment in DME patients, there is a lack of molecular-level mechanistic studies, which need to be further explored in the future through cellular, animal, and pharmacological intervention experiments.
Conclusions
The results of this study showed that the ApoB/A1 ratio was correlated with the short-term improvement of BCVA and some macular microstructure after anti-VEGF treatment in DME patients. Elevated levels of the ratio were accompanied by improvement of BCVA, regression of macular edema, restoration of inner retinal layer, and reduction in the number of HF, but had no significant effect on the changes in the IO/OS segment. ApoB/A1 is expected to be used as a biomarker to evaluate the efficacy of anti-VEGF therapy in DME patients, but its validity still requires validation through extensive clinical trial data.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due but are available from the corresponding author on reasonable request.
References
Tan, T. E. & Wong, T. Y. Diabetic retinopathy: looking forward to 2030. Front. Endocrinol. (Lausanne). 13, 1077669 (2022).
Omori, K. et al. Inhibition of stromal cell-derived factor-1α/CXCR4 signaling restores the blood-retina barrier in pericyte-deficient mouse retinas. JCI Insight 3 (2018).
Karst, S. G. et al. Association of changes in macular perfusion with Ranibizumab treatment for diabetic macular edema: a subanalysis of the restore (extension) study. JAMA Ophthalmol. 136, 315–321 (2018).
Zhang, X. et al. Dysregulated serum lipid metabolism promotes the occurrence and development of diabetic retinopathy associated with upregulated Circulating levels of VEGF-A, VEGF-D, and PlGF. Front. Med. (Lausanne). 8, 779413 (2021).
Klein, B. E., Moss, S. E., Klein, R. & Surawicz, T. S. The Wisconsin epidemiologic study of diabetic retinopathy. XIII. Relationship of serum cholesterol to retinopathy and hard exudate. Ophthalmology 98, 1261–1265 (1991).
Miljanovic, B., Glynn, R. J., Nathan, D. M., Manson, J. E. & Schaumberg, D. A. A prospective study of serum lipids and risk of diabetic macular edema in type 1 diabetes. Diabetes 53, 2883–2892 (2004).
Cho, K. H. Structural and functional changes of reconstituted high-Density lipoprotein (HDL) by incorporation of α-synuclein: A potent antioxidant and Anti-Glycation activity of α-synuclein and apoA-I in HDL at high molar ratio of α-synuclein. Molecules 26 (2021).
Ma, X. et al. Adjustment of the GRACE risk score by monocyte to High-Density lipoprotein ratio improves prediction of adverse cardiovascular outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Front. Cardiovasc. Med. 8, 755806 (2021).
Kalaivani, V. & Jaleel, A. Apolipoprotein(a), an enigmatic anti-angiogenic glycoprotein in human plasma: A curse or cure? Pharmacol. Res. 158, 104858 (2020).
Mao, R. et al. AIBP limits angiogenesis through γ-secretase-mediated upregulation of Notch signaling. Circ. Res. 120, 1727–1739 (2017).
Lee, H., Lee, J., Chung, H. & Kim, H. C. Baseline spectral domain optical coherence tomographic hyperreflective foci as a predictor of visual outcome and recurrence for central serous chorioretinopathy. Retina 36, 1372–1380 (2016).
Wen, D. Correlation between OCT biomarkers and non-response to anti-VEGF therapy in patients with diabetic macular edema ( (2023).
Sun, J. K. et al. Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema. JAMA Ophthalmol. 132, 1309–1316 (2014).
Das, R., Spence, G., Hogg, R. E., Stevenson, M. & Chakravarthy, U. Disorganization of inner retina and outer retinal morphology in diabetic macular edema. JAMA Ophthalmol. 136, 202–208 (2018).
Amoaku, W. M. et al. Defining response to anti-VEGF therapies in neovascular AMD. Eye (Lond). 29, 721–731 (2015).
Zhou, J. et al. Two-week central macular thickness reduction rate > 37% predicts the long-term efficacy of anti-vascular endothelial growth factor treatment for macular edema secondary to retinal vein occlusion. Front. Med. (Lausanne). 9, 851238 (2022).
Radwan, S. H. et al. Association of disorganization of retinal inner layers with vision after resolution of center-involved diabetic macular edema. JAMA Ophthalmol. 133, 820–825 (2015).
Moreno-Martínez, A. et al. ESASO classification relevance in the diagnosis and evolution in diabetic macular edema patients after dexamethasone implant treatment. Graefes Arch. Clin. Exp. Ophthalmol. 262, 2813–2821 (2024).
Crosby-Nwaobi, R. et al. Cross talk between lipid metabolism and inflammatory markers in patients with diabetic retinopathy. J. Diabetes Res. 191382 2015 (2015).
Soedarman, S. et al. Serum Apolipoprotein A1 and B are associated with 6-month persistent and incident diabetic macular oedema in type 2 diabetes. BMJ Open. Ophthalmol 8 (2023).
Wang, Z., Xu, L., Sun, L., Jiang, X. & Wang, J. The role of computed tomography angiography in assessing the correlation between properties of coronary atherosclerotic plaque and blood lipids. Technol. Health Care. 32, 2265–2275 (2024).
Hogg, R. E. et al. Cardiovascular disease and hypertension are strong risk factors for choroidal neovascularization. Ophthalmology 115, 1046–1052e1042 (2008).
Wang, M. et al. Inflammatory markers modify the risk of recurrent coronary events associated with Apolipoprotein A-I in postinfarction patients. J. Clin. Lipidol. 11, 215–223 (2017).
Burgess, S. & Davey Smith, G. Mendelian randomization implicates high-density lipoprotein cholesterol-associated mechanisms in etiology of age-related macular degeneration. Ophthalmology 124, 1165–1174 (2017).
Cheung, C. M. G. et al. Plasma lipoprotein subfraction concentrations are associated with lipid metabolism and age-related macular degeneration. J. Lipid Res. 58, 1785–1796 (2017).
Eren, E., Yilmaz, N. & Aydin, O. High density lipoprotein and it’s dysfunction. Open. Biochem. J. 6, 78–93 (2012).
Pikuleva, I. A. & Curcio, C. A. Cholesterol in the retina: the best is yet to come. Prog Retin Eye Res. 41, 64–89 (2014).
Wang, Y. et al. The association between the lipids levels in blood and risk of age-related macular degeneration. Nutrients 8 (2016).
Cheng, C. Y. et al. Corrigendum: new loci and coding variants confer risk for age-related macular degeneration in East Asians. Nat. Commun. 6, 6817 (2015).
Chen, W. et al. Genetic variants near TIMP3 and high-density lipoprotein-associated loci influence susceptibility to age-related macular degeneration. Proc. Natl. Acad. Sci. U S A. 107, 7401–7406 (2010).
Girotti, A. W. & Kriska, T. Role of lipid hydroperoxides in photo-oxidative stress signaling. Antioxid. Redox Signal. 6, 301–310 (2004).
Grassmann, F. et al. Genetic Pleiotropy between age-related macular degeneration and 16 complex diseases and traits. Genome Med. 9, 29 (2017).
Simó, R., García-Ramírez, M., Higuera, M. & Hernández, C. Apolipoprotein A1 is overexpressed in the retina of diabetic patients. Am. J. Ophthalmol. 147, 319–325e311 (2009).
Saucedo, L., Pfister, I. B., Schild, C., Zandi, S. & Garweg, J. G. Aqueous humor apolipoprotein concentration and severity of diabetic retinopathy in type 2 diabetes. Mediators Inflamm 2406322 (2022). (2022).
Funding
Training Program for Academic and Technical Leaders of Major Disciplines - Young Talents of Jiangxi Province (No. 20232BCJ23044); Natural Science Foundation of Jiangxi Province (No. 20224BAB206050); Science and Technology Key Program of Education Department of Jiangxi Province (No. GJJ2200125); Science and Technology Program Project of Jiangxi Provincial Administration of Traditional Chinese Medicine (No. 2024B0623).
Author information
Authors and Affiliations
Contributions
Weiyi Zhang: Collection and statistical analysis of data, paper writing; Yuling Zou: Paper guidance and revision, financial support.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, W., Zou, Yl. Elevated ApoB/A1 ratio predicts enhanced short-term efficacy of anti-VEGF therapy in diabetic macular edema. Sci Rep 15, 33009 (2025). https://doi.org/10.1038/s41598-025-18317-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-18317-y