Abstract
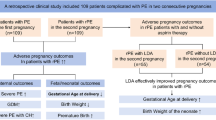
Knowing the predictors of pregnancy outcomes in patients with recurrent spontaneous abortion (RSA) is extremely critical. Accordingly, we aimed to determine the effects of the difference between mean gestational sac diameter and crown-rump length (mGSD-CRL) on the pregnancy outcomes in patients with RSA at 6–10 gestational weeks, as well as to explore its significance in predicting the pregnancy outcomes of patients with RSA. This retrospective cohort study included 256 pregnant women at 6–10 weeks of gestation and with RSA who had visited our hospital from January 2020 to March 2023. The patients were allocated to three groups based on the mGSD-CRL difference: Group A: mGSD-CRL ≤ 10 mm, Group B: 10 mm < mGSD-CRL ≤ 15 mm, and Group C: mGSD-CRL > 15 mm. The pregnancy failure rate in Group A was 22%, which was higher than those that in Group B (5.5%) and Group C (9.4%), with statistically significant differences (P < 0.05). Binary logistic regression analysis revealed that the mGSD (odd ratio [OR] = 1.14, 95% confidence interval [CI] = 1.06–1.23, P = 0.001), the CRL (OR = 1.16, 95% CI = 1.05–1.28, P = 0.004), and mGSD-CRL (OR = 1.12, 95% CI = 1.01–1.24, P = 0.026) were independent risk factors affecting the pregnancy outcome of patients with RSA. However, the uterine artery peak systolic value to end-diastolic value (UtA-S/D), D-dimer (DD), adenosine diphosphate (ADP), and arachidonic acid (AA) were not related (P > 0.05). The area under the receiver operator characteristic (ROC) curve of mGSD-CRL at 6–10 weeks of pregnancy was 0.566, with a cutoff value of 9.50 mm. The sensitivity and specificity were 90% and 36%, respectively. Compared with their prediction value, the combined prediction of mGSD-CRL, mGSD, and CRL exhibited a higher value (AUC = 0.718) in predicting pregnancy outcomes. A weak negative correlation was detected between ADP and mGSD-CRL difference (r = − 0.165, P = 0.025). In patients with RSA, mGSD-CRL acts as an independent risk factor affecting pregnancy outcomes, thereby effectively predicting the early pregnancy outcomes of patients with RSA. Thus, a low mGSD-CRL difference signifies the heightened probability of miscarriage, thereby urgently requiring clinicians to pay timely attention.
Trial registration: The study is registered at ClinincalTrails.gov (Trial registration number: NCT06081556, October 13, 2023).
Similar content being viewed by others
What does this study add to the clinical work?
This study examines whether that mGSD-CRL acts as an independent risk factor affecting pregnancy outcomes in patients with RSA, considering that it can effectively predict the early pregnancy outcomes of patients with RSA.
Introduction
Recurrent spontaneous abortion (RSA) is the occurrence of two or more consecutive miscarriages with the same partner before 28 weeks of gestation, including biochemical pregnancies1. The incidence of RSA in women of childbearing age is 1–5%2. The etiology of RSA is diverse and involves various genetic factors, abnormal reproductive tract anatomy, endocrine disorders, thrombophilia, immune dysfunction, infection factors, and systemic diseases in pregnant women3. RSA is difficult to treat, and the recurrence rate of miscarriage in patients with RSA is as high as 40%4, which can lead to considerable physical and psychological distress in the patients. Therefore, predicting the outcome of subsequent pregnancies in patients with RSA is important. Previous studies have suggested that human chorionic gonadotropin, estradiol, and early pregnancy ultrasound indicators, including fetal heart rate, crown-rump length (CRL), and mean gestational sac diameter (mGSD), have value implications in predicting the occurrence of miscarriage5,6. However, a recent study reported that in women undergoing in vitro fertilization, a smaller mGSD-CRL difference is associated with a higher rate of spontaneous abortion7. Therefore, the mGSD-CRL difference can also serve as another predictive indicator for the pregnancy outcome in patients with RSA. Additionally, in recent years, thrombophilia-induced RSA has garnered increasing research attention as it is an important cause of early and late miscarriages8. Therefore, in this retrospective cohort study, we determined the effects of the mGSD-CRL difference and thrombophilia on pregnancy outcomes in patients with RSA at 6–10 weeks of gestation. We aimed to explore its value for predicting the pregnancy outcomes of patients with RSA.
Materials and methods
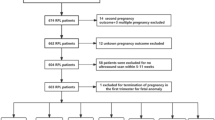
Study design and patient selection
In total, 256 pregnant women with RSA who visited the First Affiliated Hospital of Xiamen University from January 2020 to March 2023 were included in the study. The inclusion criteria were as follows: (1) patients diagnosed with RSA based on medical history, (2) those who intend to continue the pregnancy, (3) singleton pregnancy, (4) gestational age is between 6 and 10 weeks, and (5) the conception for the current pregnancy was natural. The exclusion criteria were as follows: (1) individuals with multiple pregnancies or ectopic pregnancies, (2) conception through assisted reproductive techniques, and (3) chromosomal abnormalities in pregnant women or their partners. In addition, patients with RSA included in the study often exhibit comorbidities such as thrombophilia, antiphospholipid syndrome, and connective tissue diseases, considering that they usually undergo several treatments before pregnancy, including anticoagulation (e.g., low-molecular-weight heparin), antiplatelet (e.g., low-dose aspirin), and immunosuppressive therapies.
Grouping
The patients were divided into three groups based on the mGSD-CRL difference: Group A: mGSD-CRL ≤ 10 mm, Group B: 10 mm < mGSD-CRL ≤ 15 mm, and Group C: mGSD-CRL > 15 mm. The mGSD was calculated as the average of the anteroposterior, transverse, and longitudinal diameters of the gestational sac.
Outcome measures
(1) General information: Clinical data, including age, number of previous adverse pregnancies, gestational age, mGSD, CRL, mGSD-CRL, D-dimer (DD), adenosine diphosphate (ADP), arachidonic acid (AA), and the ratio of uterine artery peak systolic value to end-diastolic value (UtA-S/D), were collected. (2) The pregnancy outcome at 14 weeks was considered successful if a visible embryo and cardiac activity were confirmed via ultrasound, whereas it was considered a failure if abortion or no cardiac activity was confirmed in the gestational sac by ultrasound.
Statistical analysis
SPSS 26.0 software was used for statistical analysis. Continuous data are presented as the mean ± standard deviation (\({\bar{\text{x}}}\) ± SD). One-way analysis of variance was used to perform multiple group comparisons, whereas independent sample t-tests were used for comparisons between groups. Categorical data are presented as numbers (%), and chi-square tests were used for group comparisons. Binary logistic regression analysis was used for independent risk factor analysis. Bivariate Spearman’s correlation coefficient was used for correlation analysis. Receiver operating characteristic (ROC) curves were used to determine the diagnostic potential of mGSD, CRL, and the mGSD-CRL difference, and their combinations in predicting the pregnancy outcome. The seven main fixed-effect predictor sets were as follows: (1) mGSD alone; (2) CRL alone; (3) mGSD-CRL difference alone; (4) log (mGSD, CRL, and mGSD-CRL differences); (5) log(mGSD, CRL); (6) log(mGSD, mGSD-CRL difference); (7) log(CRL, mGSD-CRL difference). In addition, we calculated the Youden index (Youden index = sensitivity + specificity-1) to determine the optimal cut-off value, where the point at which this value is maximized was determined as the optimal cut-off value. An AUC value of >0.5 indicated that the diagnostic technique was meaningful. In addition, when comparing the performance of two or more diagnostic tests, the ROC curve with the largest AUC was considered to have a better diagnostic performance. P < 0.05 was considered to indicate statistically significant.
All methods were performed in accordance with the relevant guidelines and regulations.
Results
Comparison of general information
Groups A, B, and C included 41, 109, and 106 individuals, respectively. The average ages of the three groups were 32.44 ± 4.94, 31.77 ± 3.62, and 31.65 ± 4.17 years, respectively. The average gravidity (number of previous adverse pregnancies) of the three groups was 2.44 ± 0.90, 2.5 ± 0.74, and 2.49 ± 0.85, respectively. The average gestational weeks of the three groups were 7.85 ± 1, 7.46 ± 0.90, and 7.46 ± 0.91, respectively. No statistically significant differences were detected in terms of age and gravidity among the three groups (P > 0.05). Moreover, no statistically significant differences were detected in UtA-S/D, ADP, AA, and DD among the three groups (P > 0.05). However, statistically significant differences were detected in the gestational age, mGSD, and CRL among the three groups (P < 0.05) (Table 1).
Comparison of pregnancy outcomes among the three groups
Pregnancy failure rate: The pregnancy failure rate of the three groups was 22%, 5.5%, and 9.4%, respectively; Group A exhibited the highest failure rate compared to Group B and Group C, and the difference was statistically significant (P < 0.05). No statistically significant difference was found in the pregnancy failure rate between Group B and Group C (P>0.05) (Table 2).
Prediction of risk factors for pregnancy outcomes
Through binary logistic regression analysis, we determined that UtA-S/D, ADP, AA, and DD were not associated with the pregnancy outcomes in patients with RSA (P > 0.05). However, mGSD (odd ratio [OR] = 1.14, 95% confidence interval [CI] = 1.06–1.23, P = 0.001), CRL (OR = 1.16, 95% CI = 1.05–1.28, P = 0.004), and mGSD-CRL (OR = 1.12, 95% CI = 1.01–1.24, P = 0.026) were identified as independent risk factors affecting pregnancy outcomes. The larger the mGSD, the longer the CRL, the greater the mGSD-CRL, and the higher the success rate of pregnancy in patients with RSA (Table 3).
Predictive value of mGSD, CRL, and mGSD-CRL for pregnancy outcomes in patients with RSA
The AUC for mGSD was 0.713, and the 95% CI was 0.61 and 0.82, with a cutoff value of 22.84 mm. The sensitivity was 64.9%, and the specificity was 72%. The AUC for CRL was 0.684, and the 95% CI was 0.59 and 0.78, with a cutoff value of 8.55 mm. The sensitivity was 58.4%, and the specificity was 76%. The AUC for mGSD-CRL was 0.566, 95% CI was 0.42 and 0.71, with a cutoff value of 9.50 mm. The sensitivity was 90%, and the specificity was 36%. Combined AUCs were generated through the logistic regression model method. The AUCs for the combinations were all 0.718, and the 95% CI were all 0.62 and 0.82. The sensitivity was 64.1%, and the specificity was 72% (Table 4; Fig. 1).
The difference means mGSD-CRL.
Correlation analysis of AA, ADP, DD, and UtA-S/D with the mGSD-CRL difference
The results of the bivariate Spearman’s correlation coefficient test indicated a weak negative correlation between ADP and the mGSD-CRL difference (r = − 0.165, p = 0.025). However, AA, DD, and UtA-S/D were not associated with the mGSD-CRL difference (P > 0.05) (Table 5).
Discussion
Currently, treating patients with RSA is challenging, and another pregnancy failure can seriously affect the physical and psychological health of the patients9. Therefore, predicting pregnancy outcomes in early pregnancy on the basis of certain indicators can help physicians intervene early and treat actively to improve pregnancy outcomes in patients with RSA.
In 1991, Bryann Bromley et al. studied 16 pregnant women and showed that when the mGSD-CRL difference was ≤ 5 mm at 5.5–9 weeks of gestation, the probability of early pregnancy loss was as high as 94%10. In 2009, Altay et al. showed that the mGSD-CRL difference at the 10th week could predict the risk of spontaneous abortion; the cutoff value of the mGSD-CRL difference was set at 10 mm, with a sensitivity of 67% and specificity of 89%11. Thus, these studies indicate that determining the mGSD-CRL difference in early pregnancy can help predict pregnancy outcomes.
In the present study, patients with RSA were assigned to three groups on the basis of the mGSD-CRL difference at 6–10 weeks of gestation, and the effects of different mGSD-CRL values and thrombosis-related indicators on pregnancy outcomes were studied. The results showed that when mGSD-CRL was ≤ 10 mm, the pregnancy failure rate was 22%, which was higher than that for the other two groups (5.5% for the mGSD-CRL difference at 10–15 mm and 9.4% for the mGSD-CRL difference > 15 mm), and the difference was statistically significant (P < 0.05). When the mGSD-CRL difference was 10–15 mm or ≥ 15 mm, no significant difference was observed in the pregnancy failure rate (P > 0.05). The present results are consistent with those reported by Altay11 and Kapfhamer JD7. Moreover, the binary logistic regression analysis showed that mGSD, CRL, and mGSD-CRL were independent risk factors affecting the pregnancy outcomes, and the larger the mGSD, the longer the CRL, and the greater the mGSD-CRL difference, the higher the success rate of pregnancy for patients with RSA.
Thrombophilia is a pathological condition that predisposes individuals to blood clot formation and is caused by various genetic or acquired factors. Furthermore, it can interfere with the exchange of substances between the mother and the fetus, leading to poor placental perfusion, uterine ischemia, hypoxia, and even miscarriage12. A study has shown that approximately two-thirds of unexplained recurrent miscarriages are caused by thrombophilia13. In a previous study, multiple indicators such as activated partial thromboplastin time, prothrombin time, DD, ADP, AA, and PDP have been used to predict thrombophilia14. Additionally, a recent study indicated an association between RSA and increased uterine artery resistance15. Increased uterine artery resistance can affect endometrial receptivity, leading to failed embryo implantation. Furthermore, it can affect the placental blood flow, causing local oxidative stress, microthrombi formation, gradual cell apoptosis, and ultimately resulting in pregnancy failure16. However, in contrast to the previous studies, the present study showed that UtA-S/D, ADP, AA, and DD were not associated with pregnancy outcomes in patients with RSA. The discrepancy may be attributed to the fact that the patients in the present study received anticoagulant and/or antiplatelet therapy before pregnancy. Thus, further research is warranted to validate the present results.
The present ROC curve analysis showed that the AUC for the mGSD-CRL at 6–10 weeks of pregnancy was 0.566, 95% CI was 0.42–0.71, and the cutoff value was 9.50 mm, with a sensitivity of 90% and specificity of 36%. Altay et al.11 set the cutoff value at 10 mm, with a sensitivity of 67% and specificity of 89%. Nazari A CJ et al.17 set the cutoff value at 10.1 mm, with a sensitivity of 56.4% and specificity of 82.1%. The cutoff values of these three studies were similar. Moreover, we calculated the AUC for the mGSD, CRL, and mGSD-CRL combination. The results revealed that, when compared with mGSD and CRL, mGSD-CRL was not significantly advantageous in predicting pregnancy outcomes (the AUC for mGSD was 0.713, and the AUC for CRL was 0.684), whereas mGSD was more advantageous in predicting the pregnancy outcomes compared to CRL (the AUC for mGSD was 0.713, and the AUC for CRL was 0.684). However, the AUC for the combination of these three indicators was 0.718, suggesting that combined testing was more beneficial in predicting pregnancy outcomes. This result is consistent with those reported by Kapfhamer et al.7. Moreover, when compared to the other two, mGSD-CRL showed a higher sensitivity but a lower specificity. Clinically, the core value of mGSD-CRL lies in the strong exclusion ability of its negative outcome, which can be applied as a preliminary screening tool to identify high-risk groups that require further diagnosis, especially for patients with recurrent miscarriage. However, we should also be cautious of its high false-positive rate. It is therefore necessary to confirm whether further treatment is required by combining clinical and other more specific tests, such as the increase in the HCG level at the early stage of pregnancy and the CRL and mGDS values of the corresponding gestational week. However, whether these results are related to the small sample size remains to be verified.
The cause of small gestational sacs remains unclear. The correlation analysis revealed a weak negative correlation between mGSD-CRL and ADP (r = − 0.165, P = 0.025), whereas AA, DD, and UtA-S/D were not related to mGSD-CRL, suggesting that increased ADP levels might result in small gestational sacs. In the early stage, the embryo relies on an adequate supply of maternal blood to obtain nutrients and oxygen. Insufficient blood flow directly inhibits the expansion of the gestational sac and embryo differentiation. ADP is an indicator of thrombophilia, and thrombophilia can lead to poor placental perfusion, because of which possibly exhibits correlation with the small mGSD-CRL difference. A retrospective study in 2017 on pregnancies after in vitro fertilization and embryo transfer indicated that abnormal ultrasound indicators in early pregnancy, such as early symmetrical growth restriction, empty sacs, small embryos, yolk sacs without embryos, and small gestational sacs, were related to chromosomal abnormalities18. The present study included 41 pregnant women with GSD-CRL ≤ 10 mm, and among them, nine women experienced embryonic demise before the 14th week of pregnancy. Among these nine women, seven women (77.78%) experienced embryonic demise because of chromosomal abnormalities. Therefore, a chromosomal abnormality is speculated as one of the causes of small gestational sacs. However, owing to the small sample size in the present study, no definitive conclusion could be drawn, warranting further research to verify this finding.
To the best of our knowledge, we are the first to examine the difference in mGSD-CRL in patients with RSA, investigate the relationship between mGSD-CRL and early pregnancy outcomes in these patients, and suggest the cutoff value of mGSD-CRL. Thus, the present study is a crucial reference for future studies. Moreover, the present study revealed that UtA-S/D, ADP, AA, and DD were not associated with the pregnancy outcomes in patients with RSA. Nevertheless, the study has several limitations. First, the study has a small sample size of only 256 women, of which only 41 showed an mGSD-CRL difference ≤ 10 mm. Second, because patients with RSA often exhibit comorbidities such as thrombophilia, antiphospholipid syndrome, and connective tissue diseases, they usually undergo several treatments before pregnancy, including anticoagulation, antiplatelet, and immunosuppressive therapies. The effect of these therapies on the study results, if any, remains unknown. Thus, future studies should explore this aspect thoroughly.
Conclusion
In conclusion, the present study suggests that mGSD-CRL is an independent risk factor affecting pregnancy outcomes in patients with RSA and can effectively predict early pregnancy outcomes. However, UtA-S/D, ADP, AA, and DD are not associated with pregnancy outcomes in these patients. The cutoff value for predicting pregnancy outcomes in patients with RSA showing an mGSD-CRL difference at 6–10 weeks of gestation is 9.5 mm, with a sensitivity of 90% and specificity of 36%. Thus, the lower the mGSD-CRL value, the higher the probability of miscarriage, necessitating that clinicians pay timely attention.
Data availability
The data and materials relevant to this study can be made available upon a reasonable request to the corresponding author.
References
Association OaGSotCM, group Rmdatecw. Expert consensus on the diagnosis and treatment of recurrent spontaneous abortion (2022). Chin. J. Obstet. Gynecol. 57 (9), 653–667 (2022).
Gao, L. et al. Characteristics of immune cell changes before and after immunotherapy and their clinical significance in patients with unexplained recurrent spontaneous abortion. Genet. Mol. Res. 13, 1169–1178 (2014).
The Reproductive Immunology Professional Committee of the Chinese Society of Human Body Health Science and Technology Promotion Association. Expert consensus on the etiological examination of recurrent miscarriage. Chin. J. Family Plann. Obstet. 14 (22), 3–9 (2022).
Royal College of Obstetricians and Gynecologists. The investigation and treatment of couples with recurrent first - trimester and second trimester miscarriage. RCOG Green-top Guideline. 17, 1–18 (2011).
Puget, C. et al. Serial hCG and progesterone levels to predict early pregnancy outcomes in pregnancies of uncertain viability: A prospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 220, 100–105 (2018).
Papaioannou, G. I. et al. Ultrasonographic prediction of early miscarriage. Hum. Reprod. 26 (7), 1685–1692 (2011).
Kapfhamer, J. D. et al. Difference between mean gestational sac diameter and crown -rump length as a marker of first -trimester pregnancy loss after in vitro fertilization. Fertil. Steril. 109 (1), 130–136 (2018).
Olivera et al. A retrospective assessment of thrombophilia in pregnant women with first and second trimester pregnancy loss. Int. J. Environ. Res. Public Health 19(24), 16500 (2022).
Cuenca, D.. Pregnancy loss: Consequences for mental health. Front. Glob Womens Health 3, 1032212.
Bromley, B. H. B., Laboda, L. A. & Benacerraf, B. R. Small sac size in the first trimester: A predictor of poor fetal outcome. Radiology 1991, 375–377 (1991).
Altay, M. M., Yaz, H. & Haberal, A. The assessment of the gestational sac diameter, crown-rump length, progesterone and fetal heart rate measurements at the 10th gestational week to predict the spontaneous abortion risk. J. Obstet. Gynaecol. Res. 35 (2), 287–292 .
Xu, L. & Cheng, W. The impact of thrombosis on fertility. Chin. J. Fam Plan. Gynecot. 13, 3–7 (2021).
Vora, S., Shetty, S. & Ghosh, K. Thrombophilic dimension of recurrent fetal loss in Indian patients. Blood Coagul Fibrinolysis: Int. J. Haemost Thromb. 19, 581–584 (2008).
Elmahashi, M. O. et al. Low dose aspirin and low-molecular-weight heparin in the treatment of pregnant Libyan women with recurrent miscarriage. BMC Res. Notes. 7, 23 (2014).
Lian, X. et al. Analysis of the guidance and predictive value of uterine artery flow parameters in patients with recurrent spontaneous abortion. J. Obstet. Gynaecol. Res. 49 (3), 803–811 (2023).
Elmahashi, M. O., Elbareg, A. M., Essadi, F. M., Ashur, B. M. & Adam, I. Low dose aspirin and low-molecular-weight heparin in the treatment of pregnant Libyan women with recurrent miscarriage. BMC Res. Notes. 7, 23 (2014).
Nazari, A. C. J., Epstein, R. H. & Dietterich, C. er al. Relationship of small-for-dates sac size to crown-rump length and spontaneous abortion in patients with a known date of ovulation. Obstet Gynecol 78, 369–373. (1991).
Li, X. et al. Correlation analysis between ultrasound findings and abnormal karyotypes in the embryos from early pregnancy loss after in vitro fertilization-embryo transfer. J. Assist. Reprod. Genet. 34 (1), 43 (2017).
Acknowledgements
The authors thank their study participants, who kindly donated their samples and time. The authors thank Medjaden Inc. for the scientific editing of this manuscript.
Funding
This manuscript was supported by the National Natural Science Foundation of China (Grant No.: 81601284).
Author information
Authors and Affiliations
Contributions
Ling Yan: conception and design of the study, sample collection, interpretation of data, and writing of the manuscript; Yiming Su: conception and design of the study, critical revision, final approval of the manuscript; Zhenhua Liao: sample collection, data analysis, and interpretation of data; Hongqin Chen: sample collection, data analysis, and data interpretation. Jing Ran: conception and design of the study, critical revision, final approval of the manuscript, and funding.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study has been approved by the Medical Ethics Committee of the First Affiliated Hospital of Xiamen University (No. 2023 − 114). Written informed consent was obtained from all participants of the study.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yan, L., Su, Y., Liao, Z. et al. Difference between mean gestational sac diameter and crown rump length predicts pregnancy outcome in patients with recurrent spontaneous abortion. Sci Rep 15, 33010 (2025). https://doi.org/10.1038/s41598-025-18390-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-18390-3