Abstract
Childhood obesity is a major global health concern and is associated with increased risks of cardiovascular and metabolic diseases. School-based exercise interventions that combine high-intensity interval training with other exercise modalities may be effective, but the optimal approach for obese children remains unclear. This single-blind randomized controlled trial included thirty obese children (body mass index [BMI] ≥ 95th percentile for age and sex, mean age 10.1 ± 0.7 years, 15 boys and 15 girls). Participants were randomly assigned to one of three groups: concurrent training with sprint interval and aerobic exercise (CT1, n = 10, 5 boys, 5 girls), concurrent training with sprint interval and strength exercise (CT2, n = 10, 5 boys, 5 girls), or a non-exercise control group (CON, n = 10, 5 boys, 5 girls). Both intervention groups completed two sessions per week for eight weeks, each consisting of 10 min of sprint interval training followed by either 10 min of aerobic exercise (CT1) or 10 min of strength training (CT2). Body composition and cardiorespiratory fitness (CRF) were measured at baseline and post-intervention. Both CT1 and CT2 groups showed significant reductions in BMI and fat mass, and significant improvements in maximal oxygen uptake (VO2max) compared to the control group (all p < 0.05). The increase in VO2max was greater in the CT2 group than in the CT1 group (6.1 vs. 3.1 mL/kg/min, p < 0.01). Visceral adipose tissue was significantly reduced in CT1, while waist circumference was significantly reduced in CT2. No significant differences were found between the intervention groups for these outcomes. No adverse events were reported. Eight weeks of school-based sprint interval concurrent training, combined with either aerobic or strength exercise, effectively improved body composition and cardiorespiratory fitness in obese children. These results support the inclusion of such exercise protocols in school programs for the prevention and management of childhood obesity.
Similar content being viewed by others
Introduction
Childhood obesity remains one of the most urgent global public health challenges, with its prevalence doubling since 1990 and obesity alone tripling. By 2021, over 170 million children and adolescents were classified as obese, and this number is projected to rise significantly by 20501. Childhood obesity is associated with a significantly higher risk of cardiovascular diseases (CVD), including metabolic syndrome, hypertension, and type II diabetes, as well as adverse effects on mental health and cognitive development2. Given that obese children are more likely to remain obese into adulthood, effective intervention strategies are of paramount importance3,4. However, the specific comparative effects of SIT-based concurrent training protocols combining aerobic versus resistance training modalities in obese children remain unclear.
Physical activity is a key component in managing childhood obesity5. Traditionally, aerobic training (AT) has been the primary exercise prescription for reducing body fat6,7. While effective in reducing body weight, conventional obesity interventions often result in skeletal muscle loss, which not only diminishes the overall efficacy of weight reduction but also complicates long-term weight maintenance8. Consequently, the integration of resistance training into obesity intervention protocols has been recognized as a critical component9. Concurrent training (CT), which synergistically combines aerobic and resistance exercises, has gained widespread acceptance in athletic and fitness domains due to its demonstrated efficacy in enhancing physical performance and promoting holistic health benefits10,11. Emerging evidence indicates that CT interventions in pediatric obesity populations can significantly elevate daily physical activity (PA) levels, enhance cardiorespiratory fitness (CRF) parameters, augment muscular strength, optimize body composition, and improve bone health metrics, particularly among obese children12,13. In recent years, there has been growing scientific interest in high-intensity interval training (HIIT) as a time-efficient and potentially more engaging alternative to traditional exercise modalities14. Sprint interval training (SIT), a specific mode of HIIT, has been proven to have better effects in pediatric populations with overweight and obesity conditions, yielding substantial health benefits while simultaneously enhancing exercise enjoyment and improving program adherence rates15. However, exclusive reliance on SIT protocols presents inherent limitations, particularly in educational settings where the implementation of structured, diversified physical activity programs is essential for comprehensive physical education16. Within this context, the strategic integration of SIT into concurrent training paradigms emerges as a promising intervention approach17. However, to date, there is a notable lack of randomized controlled trials directly comparing the effects of different SIT-based concurrent training protocols—specifically, combinations of SIT with aerobic exercise (SIT + AT) versus SIT with resistance exercise (SIT + RT)—on body composition and cardiorespiratory fitness among obese children. Most existing evidence is either limited to adult populations or evaluates SIT or CT in isolation, rather than in a synergistic, school-based context. Given the distinct physiological adaptations elicited by aerobic and resistance training, systematically comparing these two concurrent protocols in a pediatric population is both scientifically novel and practically significant. Therefore, this study aimed to address this critical research gap by evaluating and comparing the efficacy of 8 weeks of SIT-based concurrent training protocols, combined with either aerobic or resistance exercise, on body composition and cardiorespiratory fitness in obese children.
We hypothesized that both protocols would improve body composition and cardiorespiratory fitness in obese children, with the aerobic-based protocol potentially being more effective in reducing fat mass.
Subjects and methods
Study design
This study employed a single-blind, randomized controlled trial (RCT) with a parallel-group design. Participants were randomly assigned to one of three groups: Concurrent Training Group 1 (CT1), Concurrent Training Group 2 (CT2), and the Control Group (CON). One week before the intervention, trained instructors guided participants through a familiarization session to ensure they were accustomed to the exercise protocols and testing procedures. Assessments were conducted twice, at baseline (pre-test) and post-intervention (post-test), with each testing session completed on the same day. Body composition was measured first, followed by cardiorespiratory fitness (CRF) evaluation, adhering to a standardized sequence. The post-test was conducted three days after the intervention to ensure accurate data collection. Body composition assessments were carried out in the laboratory, while CRF measurements took place in the school setting.
Participants
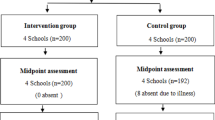
After screening 56 children for eligibility, 42 were randomized and allocated into three groups (see Fig. 1). During the course of the study, 12 participants dropped out or were lost to follow-up (4 from each group) due to personal reasons, injury, or lack of time. Thus, a total of 30 obese children (CT1, n = 10; CT2, n = 10; CON, n = 10; each group: 5 boys and 5 girls) completed the 8-week intervention and were included in the final analysis. Allocation concealment was maintained throughout the randomization and intervention process.
A total of 30 children (mean age: 10.1 ± 0.7 years; mean body mass index [BMI]: 24.3 ± 0.9 kg/m2; 15 boys and 15 girls) who were classified as obese according to the criteria of Cole et al.18 were enrolled in this randomized controlled trial. Participants were recruited from the Experimental School in Shenzhen, China, through convenience sampling based on school-based recruitment and local pediatrician consultations. The inclusion criteria were as follows: (1) age between 9 and 13 years; (2) Tanner stage 1 to 3 (pubertal stage assessed by a trained pediatrician according to the Tanner classification); (3) BMI ≥ 95th percentile for gender and age; (4) no regular physical exercise or training outside of school physical education classes in the past six months; (5) no contraindications to physical activity; and (6) self-reported physical activity < 2 hours per week as assessed by the International Physical Activity Questionnaire (IPAQ). Exclusion criteria included: (1) underlying or genetic diseases; (2) fractures or musculoskeletal injuries within the past six months; (3) contraindications to exercise; and (4) refusal to complete the exercise program at designated times and locations.
The trial was registered at the Chinese Clinical Trial Registry (ChiCTR2100048737, registered on 15/07/2021).
This study was approved by the Medical Ethics Committee of the Faculty of Medicine at Shenzhen University (Approval No: PN-202400005). All methods were performed in accordance with the relevant guidelines and regulations. Prior to the study, the guardians and class teachers were informed of the experimental design, training plan, and their respective rights and obligations. Informed consent was obtained from all the participants and their legal guardian(s).
In the present study, a simple randomization procedure was implemented using SPSS software (v25.0; SPSS Inc., Chicago, IL, USA) to generate random allocation sequences. To ensure allocation concealment, the investigator responsible for generating the randomization schedule was not involved in participant recruitment or enrollment procedures (Fig. 1). The randomization scheme was documented in triplicate, with copies securely maintained by the principal investigator, school administration, and independent statistician, respectively. Both participants and outcome assessors were blinded to group allocation throughout the study period. Intervention protocols were administered separately for each experimental group to prevent cross-contamination. An independent researcher, blinded to group assignments, conducted all statistical analyses to maintain the integrity of the data interpretation process. After allocation, both participants and the data analysts were blinded. During the intervention, each exercise intervention group underwent their respective training sessions. An independent researcher was responsible for statistical analysis of the data, ensuring that they were unaware of the specific allocation of interventions.
Anthropometry, blood pressure and body composition measures
The subjects’ height (cm) was measured using a stadiometer (Kaiyuan Electronics HW-600, Zhengzhou, China), while body weight (kg), BMI (kg/m2), body fat mass (kg), body fat percentage (%), lean body mass (kg), and visceral fat area (cm2) were measured using the InBody770 device (Biospace, Seoul, Korea). Body composition measurements were conducted by a professional research team, with the requirement that subjects fast for at least 10 h prior to testing. During the testing, participants were instructed to remove their shoes, wear lightweight, form-fitting clothing, and remove any metallic items. Waist circumference (WC; in cm) was measured with a non-elastic tape measure at the end of a normal exhalation, between the lower rib margin and the iliac crest.
Blood pressure was measured using an Omron electronic blood pressure monitor (HEM-1020, Osaka, Japan). Measurements were taken after the subjects had been seated quietly for 10 min. Two consecutive measurements were recorded, and the lower of the two values was used and reported to one decimal place in mmHg.
Cardiorespiratory fitness and maximal aerobic speed
All participants completed the 20-meter shuttle run test (20-mSRT), and their VO2max and maximal aerobic speed (MAS) were estimated using the corresponding formula19,20. The 20-mSRT is a well-established and widely recognized test for assessing maximal aerobic capacity in young individuals21 and is familiar to youth. Heart rate was monitored in real-time using a heart rate sensor (Polar team OH1, Finland).
The specific procedure for the 20-mSRT is as follows: after an adequate warm-up, participants performed shuttle runs between two lines 20 m apart, following the rhythm of the music, with progressively increasing speed. The test was terminated and the performance recorded when one of the following conditions was met: (1) failure to reach the end line twice consecutively; (2) reaching the predicted maximal heart rate (220—age); or (3) voluntary withdrawal by the subject. The running speed at the end of the test was considered the maximal aerobic speed (MAS). VO2max was then calculated using the following formula:
where gender is coded as 1 for males and 0 for females, and the number of laps represents the total number of 20-meter shuttles completed.
Training interventions
The intervention group participated in exercise sessions twice a week, each lasting 20 min, while the control (CON) group did not engage in any additional physical activity beyond the regular school physical education and activity curriculum. The CT1 and CT2 groups began each session with a 10-minute Sprint Interval.
Training (SIT) session, consisting of six repetitions of 30-second sprints performed at maximum effort, followed by 30-second rest periods and 60 s of rest between sets. After completing the sprints, participants rested until their heart rate decreased to below 100 beats per minute. Subsequently, they engaged in a 10-minute workout: the CT1 group performed stair climbing, while the CT2 group engaged in a core strength training session. The intensity of both the stair-climbing and core strength exercises was maintained at 60–70% of the participants’ maximum heart rate (HRmax). Training data for the two training groups are detailed in Table 1.
Stair climbing was performed at an intensity of 60–70% of maximal heart rate (HRmax), with participants completing approximately 15–20 steps per minute. The core strength training for the CT2 group included a series of exercises designed to target the abdominal and lower body muscles, such as planks, leg raises, bicycle crunches, seated scissor kicks, sit-ups, Russian twists, cross-knee touches, glute bridges, and alternating ankle touches. These exercises were performed with appropriate sets and durations, ensuring the intensity was maintained at the desired HRmax range throughout the session (Fig. 2).
Statistical analysis
A total of 30 obese children (15 boys, 15 girls) with simple obesity were recruited from an elementary school in Shenzhen. A sample size calculation (G*Power 3.1.9.2, Franz-Faul, Universität Kiel, Germany, α = 0.1, power = 0.5, and effect size of 0.6) revealed a minimum of 27 participants would be required in our study.
All statistical analyses were performed using the SPSS Statistical Software (v25.0; SPSS Inc., Chicago, IL, USA). Descriptive statistics (mean ± standard deviation) were calculated for all variables. The normality of the data distribution was assessed using the Shapiro-Wilk test, and homogeneity of variances was evaluated with Levene’s test.
A 2 × 3 mixed-design repeated measures analysis of variance (ANOVA) was conducted to examine the effects of time (pre- vs. post-intervention) and group (CT1, CT2, CON) on body composition and cardiorespiratory fitness indicators. If a significant interaction between group and time was found, Bonferroni post-hoc tests were applied for pairwise comparisons. Effect sizes were calculated using partial eta squared (η2). Analysis of covariance (ANCOVA) was used to adjust for the potential influence of age and baseline values on significant differences within and between groups. The statistical significance level was set at p < 0.05 for all analyses.
Results
A 2 × 3 mixed-design repeated measures analysis of variance (ANOVA) was conducted to examine the effects of time (pre- vs. post-intervention) and group (CT1, CT2, CON) on body composition and cardiorespiratory fitness indicators. The overall MANOVA results indicated a significant main effect of Time (Wilks’ Lambda = 0.391, F = 5.032, p < 0.001) and a significant interaction effect of Group × Time (Wilks’ Lambda = 0.369, F = 2.088, p = 0.006), suggesting that the intervention had differential effects on the measured outcomes across time points. The main effect of Group was also statistically significant (Wilks’ Lambda = 0.202, F = 3.961, p < 0.001), indicating differences among groups regardless of time. All differences and data are presented in Figs. 3 and 4, and Table 2.
Percentage changes in anthropometric and cardiometabolic indicators in the three groups after the intervention. Values are presented as mean ± SD. Percentage change was calculated as (post − pre)/pre×100%. Statistical significance was determined by analysis of variance (ANOVA), with between-group differences indicated as follows: CT1 vs. CT2, *P < 0.05 and **P < 0.01; CT1 vs. CON, #P < 0.05 and ##P < 0.01; CT2 vs. CON, †P < 0.05 and ††P < 0.01. CT1: sprint interval training plus aerobic training group; CT2: sprint interval training plus strength training group; CON: control group. BM, body mass; BMI, body mass index; WC, waist circumference; %BF, body fat percentage; FM, fat mass; VAT, visceral adipose tissue; LBM, lean body mass; VO2max, maximal oxygen uptake; SBP, systolic blood pressure; DBP, diastolic blood pressure; HRR, heart rate recovery.
Box plots of anthropometric and cardiorespiratory fitness measures at baseline and post-intervention for the intervention (CT1, CT2) and control (CON) groups. (a) Body mass index (BMI, kg/m2); (b) Waist circumference (WC, cm); (c) body fat percentage (%BF); (d) Maximal oxygen uptake (VO2max, mL/kg/min). Data are presented as median with interquartile range. Significant differences within each group (baseline vs. post-intervention) are indicated by *P < 0.05 and **P < 0.01 (blue symbols). Significant differences between the intervention and control groups are indicated by #P < 0.05 and ##P < 0.01 (purple symbols). “ns” denotes no significant difference.
At baseline, there were no significant differences among groups in any of the outcome variables (p > 0.05), confirming homogeneity across groups before the intervention. After the intervention, significant within-group improvements were observed in height, weight, BMI, fat mass, lean mass, and VO2max in the experimental groups compared to baseline values (all p < 0.05).
Post-hoc analyses with Bonferroni correction further revealed that the CT1 group exhibited greater improvements in body composition metrics (BMI, fat mass reduction, lean mass increase) and VO2max compared to the CT2 and CON groups (all p < 0.01). The CT2 group also demonstrated improvements compared to the CON group, but the effect sizes were smaller than those observed in the CT1 group.
Effect size (ES) calculations indicated that the changes in VO2max were large (ES > 0.8) in the CT1 group, moderate (0.5 ≤ ES < 0.8) in the CT2 group, and trivial (ES < 0.2) in the CON group. Similarly, reductions in fat mass were of a large magnitude in the CT1 group and moderate in the CT2 group, while the CON group showed minimal changes.
In summary, CT1 led to the most pronounced improvements in both cardiovascular fitness and body composition, followed by CT2, while the CON group exhibited no significant changes. The significant Group × Time interaction suggests that training modality plays a crucial role in determining the extent of physiological.
adaptations.
Discussion
The primary aim of this study was to examine the effects of two sprint interval training (SIT)-based concurrent training (CT) protocols on body composition and cardiorespiratory fitness (CRF) in obese children. Our findings demonstrated that both SIT-based CT groups achieved reductions in body weight, BMI, BF%, waist circumference, and improved VO2max in obese children.
Body composition
Fat is a significant indicator of body composition that affects obese children’s health. Consistent with previous findings by Cao et al.22 was that positive effects of FM and %BF reduction after a 12-week school-based SIT program in obese children. Another study by Bouamra et al.23 demonstrated that 9-week CT intervention which combined SIT and RT promoted significantly greater gains compared to single HIIT or single RT on body composition, especially in FM, %BF and BMI. Although the SIT protocol of this study was similar to our study, the differences in RT content may be the main reason for the different results (such as elastic band RT, core RT, and stair climbing training). The results of two other long-term CT intervention studies (9 months and 12 months) also support the findings of this study24,25. Therefore, the present study indicates that SIT-based CT improves body composition in obese children, and it appears that a longer intervention period may lead to greater improvements.
Excessive visceral adipose tissue (VAT) in obese children is closely associated with cardiovascular system impairment, cognitive dysfunction, and metabolic diseases26,27. Meta-analysis indicating that CT resulted in greater reductions in VAT in youths when compared to aerobic exercise alone9. However, mechanistic studies specifically in children remain limited, though emerging evidence suggests that some key pathways observed in adults may also be relevant in pediatric populations.
Recent studies in children and adolescents have shown that high-intensity interval and concurrent training can activate the AMPK pathway, enhancing fatty acid oxidation and glucose uptake, which leads to VAT reduction9,28. For example, García-Hermoso et al. found that multi-modal exercise training improved adipokine profiles and insulin sensitivity in obese children, suggesting activation of energy metabolism pathways similar to those reported in adults. Furthermore, resistance training in pediatric populations has been associated with increased secretion of growth hormone and testosterone, both of which facilitate lipolysis and muscle synthesis, thereby contributing to the reduction of visceral fat13,29. Notably, the hormonal response to resistance exercise may be more pronounced in children and early adolescents due to pubertal development stages.
In addition, aerobic training can enhance mitochondrial biogenesis and improve cellular oxidative capacity in children12,30, thus promoting the utilization of fatty acids as an energy source and further decreasing VAT. Importantly, regular exercise in obese children has also been shown to reduce pro-inflammatory cytokines such as TNF-α and IL-613,31, alleviating chronic low-grade inflammation that is closely linked with increased VAT.
Taken together, these pediatric studies support the hypothesis that high-intensity and concurrent exercise interventions reduce VAT in obese children through integrated metabolic, hormonal, and anti-inflammatory mechanisms, which may differ in magnitude and kinetics from those in adults.
Cardiorespiratory fitness
Improving CRF during childhood is an important health goal, as low CRF strongly predicts future cardiovascular and metabolic disease risks32. Obese children typically have lower CRF levels compared to their normal-weight peers33. Studies indicate that increasing CRF reduces the risk of cardiovascular disease and premature mortality34. Both SIT-based CT training significantly improved CRF in obese children, with both groups showing increased maximal oxygen uptake (VO2max). These results consistent with a recent study by Astorino, which reported the significant CRF improvements following school-based CT interventions for overweight/obese students, differences in measurement methods and settings may affect comparability; our study used a field-based 20m shuttle run test to estimate VO2max, whereas Astorino et al. used a laboratory-based cycle ergometer test with direct gas analysis23. In practical scenarios, our study demonstrated that SIT-based CT significantly enhances obese children’ VO2max. Our research extends this knowledge, confirming that the SIT combined with aerobic or resistance training, similarly improves CRF in school settings. The strong VO2max improvements in the CT2 group indicate resistance training does not hinder cardiovascular improvements but rather enhances both muscular and aerobic fitness simultaneously. By the end of the program, children in both intervention groups performed better in the 20-meter shuttle endurance test, indicating enhanced exercise tolerance. Enhanced CRF through school-based exercise aligns with findings from other school CT studies reporting improved endurance performance in obese youth23,35,36. Overall, our results and increasing literature suggest that high-intensity interval training effectively improves cardiovascular health in youth, particularly with sufficient duration.
In summary, current study results support the use of school-based sprint interval concurrent training as an effective, practical approach to improve health indicators in obese children. Expanding such programs in schools can significantly contribute to preventing and managing childhood obesity, ultimately reducing chronic disease risk and promoting healthier adulthood trajectories.
This study has several limitations. First, dietary intake and habitual physical activity were not objectively monitored during the intervention. Although participants were instructed to maintain their usual eating patterns and daily activity levels, with weekly verbal reminders provided to reinforce compliance, uncontrolled variations in these factors may have influenced the outcomes, as both diet and physical activity are known to affect training adaptations. Future studies should incorporate validated dietary assessment tools (e.g., 24-hour recalls, food diaries) and objective activity monitoring (e.g., accelerometry) to better isolate the effects of the training protocols. Second, the relatively small sample size (n = 30) may limit the generalizability of the findings. Third, the intervention period was relatively short (8 weeks), which may not have been sufficient to capture long-term effects. In addition, sleep patterns were not strictly controlled, which could also have affected the results. Future research with larger sample sizes, longer intervention durations, and rigorous control of dietary intake, habitual physical activity, and sleep patterns is warranted to confirm and extend the present findings.
Conclusions
SIT-based concurrent training is an effective exercise prescription for improving body composition and enhancing cardiorespiratory fitness in obese elementary school students. In this study, both concurrent training protocols significantly improved body composition and cardiorespiratory fitness compared to the control group. Notably, the protocol combining sprint interval training with aerobic exercise (CT1) resulted in greater reductions in body mass index (BMI), fat mass, and greater improvements in VO2max compared to the protocol combining sprint interval training with strength training (CT2). However, these differences should be interpreted cautiously due to the limited sample size and short intervention duration, and further studies are needed to confirm these findings. Based on these results, it is suggested that schools consider implementing this type of exercise program as part of obesity prevention and control strategies.
Data availability
The datasets generated and/or analyzed during the current study are available as supplementary material and have been submitted along with this manuscript.
References
Kerr, J. A. et al. Global, regional, and National prevalence of child and adolescent overweight and obesity, 1990–2021, with forecasts to 2050: A forecasting study for the global burden of disease study 2021. Lancet S0140673625003976 https://doi.org/10.1016/S0140-6736(25)00397-6 (2025).
Chung, S. T., Krenek, A. & Magge, S. N. Childhood obesity and cardiovascular disease risk. Curr. Atheroscler Rep. 25, 405–415. https://doi.org/10.1007/s11883-023-01111-4 (2023).
Weihrauch-Blüher, S. & Wiegand, S. Risk factors and implications of childhood obesity. Curr. Obes. Rep. 7, 254–259. https://doi.org/10.1007/s13679-018-0320-0 (2018).
Reilly, J., Kelly, J. & Long-Term Impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int. J. Obes. 2005. 35, 891–898. https://doi.org/10.1038/ijo.2010.222 (2010).
Martin, A. et al. March Physical Activity, Diet and Other Behavioural Interventions for Improving Cognition and School Achievement in Children and Adolescents with Obesity or Overweight - Martin, A – 2018 | Cochrane Library Available online: https://www.cochranelibrary.com/cdsr/doi/ (2025). https://doi.org/10.1002/14651858.CD009728.pub3/full (accessed on 7).
Cao, M., Quan, M. & Zhuang, J. Effect of High-Intensity interval training versus Moderate-Intensity continuous training on cardiorespiratory fitness in children and adolescents: A Meta-Analysis. Int. J. Environ. Res. Public. Health. 16, 1533. https://doi.org/10.3390/ijerph16091533 (2019).
Donnelly, J. E. et al. American college of sports medicine American college of sports medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc. 41, 459–471. https://doi.org/10.1249/MSS.0b013e3181949333 (2009).
Bellicha, A. et al. Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: an overview of 12 systematic reviews and 149 studies. Obes. Rev. 22, e13256. https://doi.org/10.1111/obr.13256 (2021).
García-Hermoso, A., Ramírez-Vélez, R., Ramírez-Campillo, R., Peterson, M. D. & Martínez-Vizcaíno, V. Concurrent aerobic plus resistance exercise versus aerobic exercise alone to improve health outcomes in paediatric obesity: A systematic review and Meta-Analysis. Br. J. Sports Med. 52, 161–166. https://doi.org/10.1136/bjsports-2016-096605 (2018).
Nader, G. A. Concurrent Strength and Endurance Training: From Molecules to Man. Med. Sci. Sports Exerc.38, 1965. https://doi.org/10.1249/01.mss.0000233795.39282.33 (2006).
Wilson, J. M. et al. Concurrent training: A Meta-Analysis examining interference of aerobic and resistance exercises. J. Strength. Cond Res. 26, 2293. https://doi.org/10.1519/JSC.0b013e31823a3e2d (2012).
Monteiro, P. A. et al. Concurrent and aerobic exercise training promote similar benefits in body composition and metabolic profiles in obese adolescents. Lipids Health Dis. 14 https://doi.org/10.1186/s12944-015-0152-9 (2015).
Antunes, B., de Monteiro, M. M., Silveira, P. A., Cayres, L. S. & da Silva, S. U. Effect of concurrent training on risk factors and hepatic steatosis in obese adolescents. Rev. Paul Pediatr. 31, 371–376. https://doi.org/10.1590/S0103-05822013000300015 (2013).
Cao, M., Tang, Y., Li, S. & Zou, Y. Effects of High-Intensity interval training and Moderate-Intensity continuous training on cardiometabolic risk factors in overweight and obesity children and adolescents: A Meta-Analysis of randomized controlled trials. Int. J. Environ. Res. Public. Health. 18, 11905. https://doi.org/10.3390/ijerph182211905 (2021).
Daniel Boullosa, B., Dragutinovic, J. F., Feuerbacher, S., Benítez-Flores, E. F. & Coyle March, Moritz Schumann Effects of Short Sprint Interval Training on Aerobic and Anaerobic Indices: A Systematic Review and Meta-analysis - Boullosa – 2022 - Scandinavian Journal of Medicine & Science in Sports - Wiley Online Library Available online: (2025). https://onlinelibrary.wiley.com/doi/10.1111/sms.14133 (accessed on 7).
Mura, G., Vellante, M., Nardi, A. E., Machado, S. & Carta, M. G. Effects of School-Based physical activity interventions on cognition and academic achievement: A systematic review. CNS Neurol. Disord Drug Targets. 14, 1194–1208. https://doi.org/10.2174/1871527315666151111121536 (2015).
Laird, R. H. et al. Evaluation of performance improvements after either resistance training or sprint Interval-Based concurrent training. J. Strength. Cond Res. 30, 3057–3065. https://doi.org/10.1519/JSC.0000000000001412 (2016).
Cole, T. J., Bellizzi, M. C., Flegal, K. M. & Dietz, W. H. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320, 1240–1243. https://doi.org/10.1136/bmj.320.7244.1240 (2000).
Buchan, D. S., Ollis, S., Thomas, N. E. & Baker, J. S. The influence of a high intensity physical activity intervention on a selection of health related outcomes: an ecological approach. BMC Public. Health. 10, 8. https://doi.org/10.1186/1471-2458-10-8 (2010).
Léger, L. A., Mercier, D., Gadoury, C. & Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 6, 93–101. https://doi.org/10.1080/02640418808729800 (1988).
Boreham, C. A., Paliczka, V. J. & Nichols, A. K. A comparison of the PWC170 and 20-MST tests of aerobic fitness in adolescent schoolchildren. J. Sports Med. Phys. Fit. 30, 19–23 (1990).
Cao, M., Tang, Y. & Zou, Y. Integrating High-Intensity interval training into a school setting improve body composition, cardiorespiratory fitness and physical activity in children with obesity: A randomized controlled trial. J. Clin. Med. 11, 5436. https://doi.org/10.3390/jcm11185436 (2022).
Bouamra, M. et al. Concurrent training promotes greater gains on body composition and components of physical fitness than Single-Mode training (Endurance or Resistance) in youth with obesity. Front. Physiol. 13 https://doi.org/10.3389/fphys.2022.869063 (2022).
Carnier, J., Mello, M. T. & de Aerobic training (AT) is more effective than aerobic plus resistance training (AT + RT) to improve anorexigenic/orexigenic factors in obese adolescents. Appetite 69, 168–173. https://doi.org/10.1016/j.appet.2013.05.018 (2013).
Garcia-Vicencio, S. et al. Combined Endurance and Strength or Only Endurance Training? Effects of Training Mode on Neuromuscular Characteristics and Functional Abilities in Obese Adolescent Girls Enrolled in a Weight-Reduction Program. In Cell Biology and Translational Medicine, Volume 21; Turksen, K., Ed., Advances in Experimental Medicine and Biology; Springer Nature Switzerland: Cham, ; Vol. 1450, pp. 143–159 ISBN 978-3-031-56831-2. (2023).
Tchernof, A. & Després, J. P. Pathophysiology of human visceral obesity: an update. Physiol. Rev. 93, 359–404. https://doi.org/10.1152/physrev.00033.2011 (2013).
Raine, L. B. et al. Visceral adipose tissue, and cognitive function in childhood. J. Pediatr. 187, 134–140e3. https://doi.org/10.1016/j.jpeds.2017.05.023 (2017).
Richter, E. A. & Ruderman, N. B. AMPK and the biochemistry of exercise: implications for human health and disease. Biochem. J. 418, 261–275. https://doi.org/10.1042/BJ20082055 (2009).
Kraemer, W. J., Ratamess, N. A., Hymer, W. C., Nindl, B. C. & Fragala, M. S. Growth Hormone(s), testosterone, Insulin-Like growth factors, and cortisol: roles and integration for cellular development and growth with exercise. Front. Endocrinol. 11 https://doi.org/10.3389/fendo.2020.00033 (2020).
Bishop, D. J., Lee, M. J. C. & Picard, M. Exercise as mitochondrial medicine: how does the exercise prescription affect mitochondrial adaptations to training?? Annu. Rev. Physiol. https://doi.org/10.1146/annurev-physiol-022724-104836 (2024).
Beavers, K. M., Brinkley, T. E. & Nicklas, B. J. Effect of exercise training on chronic inflammation. Clin. Chim. Acta Int. J. Clin. Chem. 411, 785–793. https://doi.org/10.1016/j.cca.2010.02.069 (2010).
Lang, J. J. et al. Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of Meta-Analyses representing over 20.9 million observations from 199 unique cohort studies. Br. J. Sports Med. 58, 556–566. https://doi.org/10.1136/bjsports-2023-107849 (2024).
Tsiros, M. D. et al. Adiposity is related to decrements in cardiorespiratory fitness in obese and Normal-Weight children. Pediatr. Obes. 11, 144–150. https://doi.org/10.1111/ijpo.12037 (2016).
Wildgust, H. J., Hodgson, R. & Beary, M. The paradox of premature mortality in schizophrenia: new research questions. J. Psychopharmacol. Oxf. Engl. 24, 9–15. https://doi.org/10.1177/1359786810382149 (2010).
Gäbler, M., Prieske, O., Hortobágyi, T. & Granacher, U. The effects of concurrent strength and endurance training on physical fitness and athletic performance in youth: A systematic review and Meta-Analysis. Front. Physiol. 9 https://doi.org/10.3389/fphys.2018.01057 (2018).
Garcia-Vicencio, S. et al. Combined Endurance and Strength or Only Endurance Training? Effects of Training Mode on Neuromuscular Characteristics and Functional Abilities in Obese Adolescent Girls Enrolled in a Weight-Reduction Program. In Cell Biology and Translational Medicine, Volume 21: Stem Cell in Lineage, Secretome Regulation and Cancer; Turksen, K., Ed., Springer Nature Switzerland: Cham, pp. 143–159 ISBN 978-3-031-56832-9. (2024).
Acknowledgements
This work was supported by the 2024 Annual Educational Research Planning Project: “Construction and Empirical Research on Obesity Prevention Models for Primary and Secondary School Students in China from the Perspective of Home-School-Society Collaboration” (Project No. 202416307635B).
Author information
Authors and Affiliations
Contributions
Yuhang Gao wrote the main manuscript text, prepared all figures, and handled the submission. Minhua Wu and Jun Chen were responsible for data collection and analysis. Zhenyu Feng contributed to the literature review and formatting. Xiao-dong Wang provided supervision and writing guidance. Meng Cao supervised the entire study and reviewed the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gao, Y., Wu, M., Chen, J. et al. Effects of school-based concurrent training on body composition and cardiorespiratory fitness in obese children in a randomized controlled trial. Sci Rep 15, 33300 (2025). https://doi.org/10.1038/s41598-025-19041-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19041-3