Abstract
exploring the therapeutic efficacy of a 3D-printed multiple microporous titanium metatarsal and polyethylene sesamoid prosthesis based on finite element analysis. A patient with defect in the first metatarsal was enrolled. A digital model of the first metatarsal and medial cuneus prosthesis was designed from the contralateral images and the relevant anatomical parameters measured in the preoperative period (Model A). Model B was obtained by finite element analysis and iterative optimization of Model A. Model A and Model B designed with a microporous, an insertion structure for bone ingrowth and fusion, and a polyethylene sesamoid for limb weight-bearing. The object A and object B, made from titanium, were generated by 3D printing. The polyethylene sesamoid was manufactured by computerized numerical control technology. The prosthesis consist of object B and polyethylene sesamoid was implanted into the patient. The clinical parameters were evaluated. The maximum displacements of Model A and Model B were 0.031 mm and 0.019 mm. the deviation of the stress results was controlled within 5% between Model A and Model B. The object A with 63% weighed object B. There is significant difference for pressure in M1 and M5 area between bilateral foot. The AOFAS score was 48 before surgery and 88 after 15 months of surgery. The VAS score of before surgery, after 15 months of surgery and after 27 months of surgery was 7, 2 and 1, respectively. The lightweight and microporous design based on finite element analysis for metatarsal prosthesis, and manufactured by titanium and polyethylene can Reconstruct the arch.
Similar content being viewed by others
Introduction
The first metatarsal bone plays an important role in the function of the normal foot. In the normal gait, approximately 15% of the load passes through the first ray, and 30–50% of the toe load of all five toes is transmitted through the hallux1,2. Even in elderly individuals, the combined load on the first metatarsophalangeal joint averages 35% of body weight3. Therefore, the absence of the first metatarsal bone often causes severe dysfunction4,5.
For large metatarsal defects, iliac bone grafts, fibula grafts, metal grafts6,7,8 and other methods are currently available. However, complication rates ranging from 10 to 49% are reported for iliac bone and fibula grafts9,10,11. The complications include infection, prolonged pain, malunion and delayed union12,13,14. Although metal grafts have better stability, they cause bone loss and even implant detachment due to their unique stress-shielding effect15,16.
Titanium and its alloys, as a type of metal grafts, are widely used in medical because of their excellent biocompatibility, good corrosion resistance and high strength. 3D printing via additive manufacturing can intelligently optimize the bearing structure of the implant. In addition, the design of the porous structure can promote the growth of bone cells17. The porous titanium scaffolds were manufactured by 3D printing technology and implanted into experimental sheep with metatarsal bone defects; the results proved that the porous titanium scaffold is a good substitute for autogenous bone and is suitable for the treatment of large segmental bone defects18. Researchers have used 3D printing technology to create personalized porous polyethylene jaw implants and achieved good results without complications such as infection or implant displacement. Polyethylene has become an important material for jaw filling19. To our knowledge, there is currently no research on implant surgery for 3D-printed microporous titanium structure metatarsal bone or on the clinical application of the 3D-printed polymer polyethylene sesamoid.
In this study, based on the CT data of patients’ feet, we constructed individualized metatarsal bone and medial cuneus prosthesis models with a lightweight design. After the mechanical properties were verified by finite element analysis (FEA), the 3D-printed first metatarsal and medial cuneus prosthesis was implanted, and good clinical effects were achieved.
Materials and methods
Clinical data
The participant was provided informed consent during the study and this study is approved by Ethics Committee of Zigong Fourth People’s Hospital. All methods in this research were performed in accordance with the relevant guidelines and regulations.
A male,58-year-old and 158-cm-tall, was diagnosed with traumatic bone defects in the first metatarsal and medial cuneus. Debridement, bone cement implantation and filling, and anterior and external thigh free flap grafting were performed in an orderly fashion at our hospital (Fig. 1). Difficulty walking after bone cement filling and request for reoperation. The symmetry, range of motion, nerve response, and blood vessels of the bilateral foot and ankle joints were examined; X-rays were performed to preliminarily confirm the bone defect; and computed tomography (CT) was subsequently performed. The images were obtained via Digital Imaging and Communications in Medicine (DICOM) for 3D reconstruction (Sweep voltage at 135 kV, cross-sectional thickness at 0.5 mm and resolution of 512*512 pixels). The CT images of the bilateral feet were imported into Mimics 22.0 (Materialise, Leuven, Belgium). The case time line as follow (Table 1).
A 58-year-old man was diagnosed with a large segmental defect in the left first metatarsal bone and medial cuneus after trauma. (A) X-ray image of the immediate trauma. (B) X-ray image of the bone cement implantation after 1 month. (C) X-ray image of the bone cement implantation after 3 months. (D) Appearance of the anterolateral femoral free flap grafts postoperatively.
Preparation of first metatarsal and medial cuneus prosthesis
Lightweight design of prosthesis
The metatarsal bone prosthesis model was generated by mirroring the healthy portion of the patient, and screw holes and prosthesis stems were designed (defined as Model A) (Fig. 2A,B). Model A had a volume of 23,991 mm3. The volume of the bone cement filling of the patient’s affected side was measured to be 14,148 mm3 before the second surgery. Prior optimization preprocessing was carried out on Model A using Geomagic Wrap 2021 (3DS Systems, USA) and SolidWorks 2017 (Dassault Systemes). A static finite element model of the normal foot was established in ANSYS Workbench 19.1 (ANSYS, Inc., PA, USA) (Fig. 3A). The foot and Model A are defined as isotropic materials with the same elastic modulus and Poisson’s ratio parameters20,21. To enhance the accuracy of the finite element model, second-order tetrahedral (Tetra10) elements were used for meshing. The mesh size for the bones was controlled at 2–3 mm, while the mesh size for Model A, screws, Model A-bone contact, and screw-bone contact was controlled at 1–1.5 mm. After multiple iterations, the average skewness of the prosthesis finite element model was reduced to 0.39. The bone-bone, screw-bone, prosthesis-bone, and prosthesis-screw contact interfaces were set as bonded interfaces. The angle between the first metatarsal bone and the horizon in the standing position was 30°. This angle increases to 70° during gait, and the internal stress in the first metatarsal bone reaches its maximum22,23. One of the FEA projects set Model A at an angle of 30° between the first metatarsal and the horizontal plane. A vertical force of 500 N was applied to the surface of the astragalus at this point, with fixation points at the bottom of the calcaneal tuberosity, the sesamoid prosthesis and the fifth metatarsal head. The other project of the FEA was configured with Model A at an angle of 70° between the first metatarsal and the horizontal plane. A force of 500 N was applied along the direction of prosthesis A on the surface of the astragalus, with fixation points at the sesamoid prosthesis and the fifth metatarsal head. (Fig. 3B,C).
Configuration of the Statics FEA for the prosthesis model. (A) Finite element mesh division of prosthesis model A. (B) Application of a 500 N force perpendicular to the horizontal plane on the upper surface of the Astragalus (Prosthesis A forms a 30° angle with the horizontal plane), with fixation points at the calcaneal tuberosity, sesamoid prosthesis and fifth metatarsal head. (C) Application of a 500 N force along the direction of prosthesis A on the upper surface of the astragalus (prosthesis A forms a 70° angle with the horizontal plane), with fixation points at the sesamoid prosthesis and the fifth metatarsal head.
Topology optimization was performed separately for the two finite element analysis results of Model A to achieve lightweight design of the prosthetic structure. The contact interface between the prosthesis and bone, screw holes, and prosthesis stems were set as the exclusion region. The remaining parts of the prosthesis were designated as the design region. The optimization type was set to ‘topology optimization - level set based’ with a convergence tolerance of 0.01 and maximum iteration limit of 200 cycles. The optimization goal was set to retain a volume of 14,148 mm3, which corresponds to approximately 60% of the original volume. The results of topological optimization for Model A in two directions were exported as two STL files using Ansys software. These models are then subjected to Boolean union operations in 3-Matic (Materialise, Leuven, Belgium). The resulting synthetic model was smoothly corrected and denoted Model B (Fig. 2C,D), with a volume of approximately 15,165 mm3. Model B was subsequently analyzed with Ansys software using the same settings as Model A to evaluate prosthesis stress and displacement.
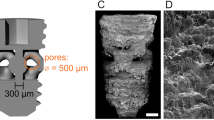
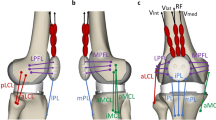
The prosthesis included two parts, a titanium metatarsal bone and a polyethylene sesamoid prosthesis (both are medical grade implantable materials), connected through a locking structure. The surface of the titanium metatarsal bone was designed with micropores (pore size of 600 μm/strut thickness of 150 μm/porosity of 70%, surface roughness of 20 μm)24. The metatarsal bone had prosthesis stems at both ends for attachment to the navicular bone of the foot and the first phalanx. Additionally, five holes 3.5 mm in diameter were designed for locking screws to enhance the initial stability of the prosthesis. A total of 18 small holes were designed on the surface of the titanium metatarsal bone to connect it to the ligaments (Fig. 2E,F).
Manufacture of prosthesis
The metatarsal Prostheses (Model A and B) were imported into an electron beam molten metal rapid prototyping system (ARCAM, Sweden, 2003), and the printed material was Ti6Al4V powder with an average diameter of 45–105 μm. The maximum scanning speed of the electron beam was 8000 ms− 1 and the accuracy of printing was ± 0.2 mm. The metatarsal prosthesis was cleaned in a powder recovery system and washed in acetone, ethanol, and distilled water with an ultrasonic machine for 30 min each. The sesamoid was manufactured by computerized numerical control (CNC), and the material was polyethylene. The surface of the prosthesis was polished to make it smooth (Fig. 4). Our entire production and utilization process strictly adheres to the Regulation on the Supervision and Administration of Medical Devices, with the Provisions for the Supervision and Administration of Custom-Made Medical Devices and the Guiding Principles for the Review of Additive Manufacturing Medical Device Registration serving as our operational guidelines.
Internal fixation surgery
The titanium metatarsal bone and polyethylene sesamoid prosthesis were sterilized. The patient assumed a supine position, and his ankle and foot area were sterilized following the administration of general anesthesia. A 15 cm long skin incision was subsequently created along the edge of the anterolateral femoral flap (Fig. 5A). The deep structures were exposed after incising the subcutaneous fat. The bone cement filling was removed (Fig. 5B), and the wound was rinsed repeatedly. With the assistance of the 3D-printed guide (Fig. 5C), the whole prosthesis was implanted with polyethylene sesamoid prosthesis (Fig. 5D) and reinforced with screws with an operation time of 90 min and bleeding of 100 ml, and the implant was confirmed to be stable (Fig. 5E,F).
Surgical procedure (A) The skin and soft tissue were incised to fully expose the surgical area. (B) Removal of bone cement filling. (C) Drilling cavities assisted by the 3D-printed navigation template to facilitate the implantation of the prosthesis stem. (D) Implantation of the proximal prosthesis stem. (E) Locking screw fixation and ligament reconstruction. (F) Appearance of the affected limb 1 week after surgery.
Evaluation parameters
The von Mises stress can represent the stress distribution of internal fixation, and its maximum value represents the position where internal fixation is most prone to failure and fracture. Displacement represents the largest variable of the model under the loaded condition, and the larger the displacement, the greater the risk of model fracture.
Postoperative X-rays and CT images can be registered with the prosthesis, which can objectively indicate whether the position of the prosthesis is good. The functional efficacy of the first metatarsal and medial cuneus prosthesis of patient was scored using the AOFAS score. The patients’ pain was evaluated using the VAS.
The patient’s height and weight were measured. A foot pressure assessment system (Med-Track, China; 53 mm × 44.7 mm × 2 mm; resolution of 4 sensors/cm2; data acquisition frequency, 200–500 Hz; pressure range, 0–200 N/cm2) was connected to the computer. The patient’s center of gravity and arch index were measured under the static evaluation system of the foot pressure assessment system (Fig. 6A). The foot was divided into 11 areas during the dynamic assessment system measurements (Fig. 6B). Under standing position, since the main stress areas of the planta were distributed in the first metatarsal head, fifth metatarsal head and heel areas25, the M1-M5 areas and the HM and HL areas were selected as the evaluation indices of plantar pressure distribution in this study. The pressure in the metatarsal M1-M5 areas and the heel HM and HL areas were measured during gait, which reflects the distribution of the patient’s plantar weight after implantation of the prosthesis.
Planting pressure test and functional assessment 15 months after surgery. (A) The patient remained standing to complete a static plantar stress test. (B) The bilateral plantar fascia was divided into 11 areas. (C) The static plantar stress distribution in the 11 areas. (D) Full dorsal extension of the ankle joint. (E) Full plantar flexion of the ankle joint.
Results
FEA for prosthesis
After FEA and iterative optimization, the A and B volumes were 23,991 mm3 and 15,165 mm3, respectively, and the volume of model B was approximately 63% of that of model A, which was close to 60% of the initial setting (Table 2). The finite element Model B contains 55,000 elements and 100,000 nodes. The average solving time of Model B was approximately 1 h, and both the displacement and stress converge successfully. The maximum displacements of Model A and Model B were 0.031 mm and 0.019 mm, respectively, with the displacement deviation controlled within 1%. The average stress values of the sesamoid prosthesis support for Model A and Model B were 2.86 MPa and 2.31 MPa at 30° and 5.16 MPa and 4.02 MPa at 70°, respectively, indicating that the average stress values of Model B were lower than those of Model A at different angles and that the deviation of the stress results was controlled within 5%. In this study, we designed the middle part of the Model B to be 68.66 mm in length, and the total length of the first metatarsal bone and medial cuneiform bone on the healthy side was 68.95 mm, with a proximal prosthesis stem of 20.02 mm and a distal prosthesis stem of 12.38 mm. The printed prostheses of the object A and object B weighed 87.9 g and 62.2 g, respectively.
Clinical performance
Following the second surgery, serial X-rays and CT scans were obtained during the follow-up period, with subsequent 3D reconstruction performed. Postoperative patient clinical performance was assessed after 15 months of follow-up; The patient exhibited good wound healing at 2 weeks after surgery, could keep standing and could perform basic foot activities (Fig. 6D,E). The patient could walk with the assistance of crutches 1 month after surgery and could walk independently 2 months after surgery. Postoperative X-ray and CT (Fig. 7) showed that the prosthesis was stably placed and that there was no loosening at 15 months after surgery. The patients had an AOFAS score of 48 before surgery and an AOFAS score of 88 fifteen months after surgery; additionally, The VAS score of before surgery, after 15 months of surgery and after 27 months of surgery was 7, 2 and 1, respectively.
Radiographic images of the affected limb at different postoperative stages. (A) X-ray image immediately after surgery. (B) X-ray image 3 months after surgery. (C) X-ray image 15 months after surgery. (D,E). Three-dimensional reconstruction of the affected limb 15 months after surgery. (F) Immediately postoperative CT image suggesting good prosthetic insertion. (G) CT 15 months postsurgery, suggesting no loosening of the prosthesis.
Plantar pressure test
According to the static plantar pressure test, the arch index of the left foot and right foot were 18.36% and 19.28%, respectively, with a difference of 5% between the bilateral arch index. The patient had a barycenter shift of 1.39 ± 0.16° (Fig. 6C). The gait plantar pressure test showed that pressure distribution in the M1 area on the affected side was significantly higher than that in the M1 area on the healthy side (210.19 Kpa VS 60.63 Kpa, P < 0.01), and the pressure distribution in the M5 area on the affected side was significantly less than that in the M5 area on the healthy side (112.87 Kpa VS 187.84 Kpa, P < 0.01); and there was no significant difference for pressure distribution in the other areas (Table 3).
Discussion
Weight reduction based on FEA
Exploring a lightweight prosthesis is an intractable problem for orthopedics doctors since lightweight prostheses are more beneficial for patient mobility and surgical placement26,27. Although the implant design and biological materials have improved, the rejection rate reaches 30–50% in orthopedic prostheses, which is mainly due to the heavy weight of prostheses and the low comfort of prostheses28. Finite element analysis (FEA) for the construction of complex constitutive body models based on CT data has become a very valuable tool for clinical bone research29,30. Based on CT data, scholars constructed a reasonable talus model after weight reduction, obtained the stress distribution of the model under the maximum load in all directions through FEA to verify its safety, and obtained a scaffold for talar prostheses with both weight reduction and mechanical stability31. The researchers designed a hip prosthesis with a weight reduction of 15–17% via direct metal laser sintering (DMLS, a 3D print technology). The FEA and fatigue test results showed that the prosthesis had good performance32. In this study, the stress distribution and deformation of the prosthesis were obtained through FEA under two extreme loading conditions of gait, and the weight was reduced. The weight of the prosthesis was reduced from 87.9 to 62.2 g. FEA was subsequently performed on the prosthesis after weight reduction to ensure that it could theoretically meet the clinical mechanical requirements. Additive manufacturing technology provides support in terms of weight reduction and strength improvement33. We manufactured the abovementioned object B by DMLS and successfully placed it in the missing toe bone of the patient. The placement went smoothly, and the procedure took only 94 min. The Model B had a length of 68.66 mm, which is close to the length of the healthy metatarsal bone (68.95 mm); the Model B had a volume of 15,165 mm3, which is close to the volume of initial bone cement filling (14,148 mm3). Under static plantar pressure testing 15 months after surgery, there was only a 5% difference between the affected and healthy arch index of the patients.
Microporous devices for prosthesis surfaces
The foot is important for assisting in load bearing, balance, shock absorption and flexibility in the ground topography of the human body. As one of the main structures of the foot, the first metatarsal bone plays a vital role in maintaining the structural stability of the foot34,35. The design based on reverse engineering and the manufacture of prostheses by 3D printing can fully meet individual appearance requirements and stability requirements, especially because the mechanical properties of lattice structures show significant advantages28, which are recommended methods for manufacturing orthopedic prostheses36. In this study, a prosthesis stem, locking screw structures and holes for tendon attachment were designed at both ends of the metatarsal prosthesis. Immediate postoperative X-ray showed that the prosthesis was completely fitted with the surrounding bone tissue, joints and ligaments, confirming the initial stability of the foot. An ideal prosthesis should have a precisely controlled and fully interconnected multiple microporous structure to achieve complete regeneration and bone fusion of massive bone and ultimately achieve long-term stability of the overall structure37. In this study, the surface of a metatarsal prosthesis was treated with multiple micropores and manufactured with DMLS to ensure the precise presentation of the multiple microporous structure. The X-ray images showed no displacement or loosening 15 months after surgery, the AOFAS score increased by 21 points, the VAS score decreased by 3 points compared with the preoperative score, and the walking distance, range of motion and pain sensation of the affected side improved, which indicated that the long-term stability of the prosthesis improved the prosthesis and quality of life.
Superiority of polyethylene for sesamoid manufacture
Accurate reconstruction of the sesamoid bone is very important for preventing bunions and maintaining inter-plantar Angle38. During long-term progression, the sesamoid bone is considered to the site of ossification of tendons or ligaments39. Since the first metatarsal bone bears considerable pressure when walking, joint fusion easily causes serious pain and mobility disorders40,41. Since metal prostheses usually result in skin necrosis, soft and durable materials are recommended. As an ideal Cenozoic material, polyethylene can help tissue integrate, has the advantages of good stability and anti-infectivity, strong toughness and stiffness, cannot be absorbed or metabolized, is often used as the first choice of prosthesis material used in surgical operations such as sternum and facial bone remodeling, and has good clinical effects42,43. In this study, polyethylene was used as the material for the sesamoid prosthesis, and combined with the advantages of personalized design, the polyethylene sesamoid prosthesis was successfully implanted into the patient. According to the plantar gait pressure test 15 months after surgery, the pressure distribution in the M1 area on the affected side (around the prosthesis of the sesamoid) was significantly greater than that in the M1 area on the healthy side (210.19 Kpa vs. 60.63 Kpa, P < 0.01), and that in the M5 area was the opposite (112.87 Kpa vs. 187.84 Kpa, P < 0.01). These findings indicate that the stress on the affected foot is transferred to the polyethylene sesamoid prosthesis area during gait, which may be related to the local force dispersion by the polythene sesamoid prosthesis and provide excellent comfort for the plantar foot under pressure.
Conclusion
Through reverse engineering and a lightweight design based on FEA, we used DMLS technology to create personalized titanium metatarsal prostheses, which have been successfully applied in the clinic with their short operation time and limited bleeding. The initial structural stability and long-term structural stability were established, and the patient’s foot function was basically restored.
Data availability
Data is provided within the manuscript.
References
Jakob, H. A. C. & Zollinger, H. Biomechanics of the forfoot in view of osteotomies in this area. Med. Orth Tech. 113, 262–266 (1993).
Cavanagh, P. R., Rodgers, M. M. & Iiboshi, A. Pressure distribution under symptom free feet during barefoot standing. Foot Ankle. 7, 262–276 (1987).
Wyss, U. P., McBride, I., Murphy, L., Cooke, T. D. & Olney, S. J. Joint reaction forces at the first MTP joint in a normal elderly population. J. Biomech. 23 (10), 977–984 (1990).
Becker, A. First metatarsal malunion. Foot Ankle Clin. 14 (1), 77–90 (2009).
Bayod López, J., Becerro de Bengoa Vallejo, R., Losa Iglesias, M. E. & Doblaré, M. Mechanical stress redistribution in the first metatarsal bone after autologous bone harvesting. J. Am. Podiatr. Med. Assoc. 107 (6), 497–510 (2017).
Coriaty, N. et al. Titanium scaffolding: An innovative modality for salvage of failed first ray procedures. J. Foot Ankle Surg. 57 (3), 593–599 (2018).
Winters, B. S., Czachor, B. & Raikin, S. M. Metatarsophalangeal fusion techniques with first metatarsal bone loss/defects. Foot Ankle Clin. 20 (3), 479–491 (2015).
Jogani, A. D., Garje, V., George, P. K., Rathod, T. & Bhaladhare, S. M. Reconstruction of first metatarsal bone loss following osteomyelitis by a modified masquelet technique: A case report. J. Orthop. Case Rep. 10 (9), 118–120 (2020).
Raikin, S. M. & Brislin, K. Local bone graft harvested from the distal tibia or calcaneus for surgery of the foot and ankle. Foot Ankle Int. 26 (6), 449–453 (2005).
Schulhofer, S. D. & Oloff, L. M. Iliac crest donor site morbidity in foot and ankle surgery. J. Foot Ankle Surg. 36 (2), 155–161 (1997).
Bia, A., Guerra-Pinto, F., Pereira, B. S., Corte-Real, N. & Oliva, X. M. Percutaneous osteotomies in hallux valgus: A systematic review. J. Foot Ankle Surg. 57 (1), 123–130 (2018).
Wippermann, B. W., Schratt, H. E., Steeg, S. & Tscherne, H. [Complications of spongiosa harvesting of the Ilial crest. A retrospective analysis of 1,191 cases]. Chirurg 68 (12), 1286–1291 (1997).
Mankovecky, M. R., Prissel, M. A. & Roukis, T. S. Incidence of nonunion of first metatarsal-phalangeal joint arthrodesis with autogenous Iliac crest bone graft after failed Keller-Brandes arthroplasty: A systematic review. J. Foot Ankle Surg. 52 (1), 53–55 (2013).
Usuelli, F. G., Tamini, J., Maccario, C., Grassi, M. & Tan, E. W. Bone-block arthrodesis procedure in failures of first metatarsophalangeal joint replacement. Foot Ankle Surg. 23 (3), 163–167 (2017).
Niinomi, M. & Nakai, M. Titanium-based biomaterials for preventing stress shielding between implant devices and bone. Int. J. Biomater. 2011, 836587 (2011).
Díaz Fernández, R. Tratamiento Del hallux valgus moderado y Severo mediante doble osteotomía percutánea Del primer Metatarsiano [Treatment of moderate and severe hallux valgus by performing percutaneous double osteotomy of the first metatarsal bone]. Rev. Esp. Cir. Ortop. Traumatol. 59 (1), 52–58 (2015).
Coşkun, Z., Çelik, T. & Kişioğlu, Y. Metatarsal bone model production using 3D printing and comparison of material properties with results obtained from CT-based modeling and real bone. Proc. Inst. Mech. Eng. H. 237 (4), 481–488 (2023).
Wieding, J., Lindner, T., Bergschmidt, P. & Bader, R. Biomechanical stability of novel mechanically adapted open-porous titanium scaffolds in metatarsal bone defects of sheep. Biomaterials 46, 35–47 (2015).
Chang, P. C. Computer-assisted planning and 3D printing-assisted modeling for chin augmentation. Aesthet. Surg. J. 38 (1), 1–10 (2017).
Wang, Y., Li, Z., Wong, D. W., Cheng, C. K. & Zhang, M. Finite element analysis of Biomechanical effects of total ankle arthroplasty on the foot. J. Orthop. Translat. 12, 55–65 (2017).
Miyoshi, S., Takahashi, T., Ohtani, M., Yamamoto, H. & Kameyama, K. Analysis of the shape of the tibial tray in total knee arthroplasty using a three dimension finite element model. Clin. Biomech. (Bristol Avon). 17 (7), 521–525 (2002).
Whyss, U. P. Joint reaction forces at the first MTP joint in a normal elderly population. J. Biomech. 23 (10), 977–984 (1990).
Kristen, K. H. et al. The first metatarsal bone under loading conditions: A finite element analysis. Foot Ankle Clin. 10 (1), 1–14 (2005).
Zhang, Y. et al. The contribution of pore size and porosity of 3D printed porous titanium scaffolds to osteogenesis. Biomater. Adv. 133 (112651), 1–11 (2022).
Seaman, T. J. & Ball, T. A. Pes cavus. In: StatPearls. (StatPearls Publishing, 2023).
Staiger, M. P., Pietak, A. M., Huadmai, J. & Dias, G. Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 27 (9), 1728–1734 (2006).
Ren, Y., Zhao, H., Yang, K. & Zhang, Y. Biomechanical compatibility of high strength nickel free stainless steel bone plate under lightweight design. Mater. Sci. Eng. C Mater. Biol. Appl. 101, 415–422 (2019).
Poddar, P., Olles, M. & Cormier, D. Mechanical response of carbon composite octet truss structures produced via axial lattice extrusion. Polym. (Basel). 14 (17), 3553 (2022). Published 2022 Aug 29.
ahr, D. H. & Reisinger, A. G. A review on recent advances in the constitutive modeling of bone tissue. Curr. Osteoporos. Rep. 18 (6), 696–704 (2020).
Pahr, D. H. & Zysset, P. K. Finite element-based mechanical assessment of bone quality on the basis of in vivo images. Curr. Osteoporos. Rep. 14 (6), 374–385 (2016).
Kang, Y., Kim, S., Kim, J., Lee, J. W. & Park, J. C. Evaluating the validity of lightweight Talar replacement designs: Rational models and topologically optimized models. Biomater. Res. 26 (1), 10 (2022). Published 2022 Mar 14.
Delikanli, Y. E. & Kayacan, M. C. Design, manufacture, and fatigue analysis of lightweight hip implants. J. Appl. Biomater. Funct. Mater. 17 (2), 2280800019836830 (2019).
Liu, C. et al. Design and fabrication of extremely lightweight truss-structured metal mirrors. Mater. (Basel). 15 (13), 4562 (2022).
Gupta, R., Grove, K., Wei, A., Lee, J. & Akkouch, A. Ankle and foot arthroplasty and prosthesis: A review on the current and upcoming state of designs and manufacturing. Micromachines (Basel). 14 (11), 2081 (2023). Published 2023 Nov 10.
Zumofen, L. et al. Properties of additive-manufactured open porous titanium structures for patient-specific load-bearing implants. Front. Mech. Eng. 7, 830126 (2022).
Burn, M. B., Ta, A. & Gogola, G. R. Three-dimensional printing of prosthetic hands for children. J. Hand Surg. Am. 41 (5), e103–e109 (2016).
Li, Y. et al. Additively manufactured biodegradable porous magnesium. Acta Biomater. 67, 378–392 (2018).
Huang, E. H., Charlton, T. P., Ajayi, S. & Thordarson, D. B. Effect of various hallux valgus reconstruction on sesamoid location: A radiographic study. Foot Ankle Int. 34 (1), 99–103 (2013).
van der Naald, M., van der Naald, N., van der Velde, D. & Schuurman, A. H. Fracture of the sesamoid bone of the thumb: A case report and review of the literature. JBJS Case Connect. 9 (1), e10 (2019).
Womack, J. W. & Ishikawa, S. N. First metatarsophalangeal arthrodesis. Foot Ankle Clin. 14 (1), 43–50 (2009).
Schuh, R. & Trnka, H. J. First metatarsophalangeal arthrodesis for severe bone loss. Foot Ankle Clin. 16 (1), 13–20 (2011).
Bidois, L. M., Porter, C. & Singh, H. P. Attachment issues: A case report of a promising sternal implantation with 3D-printed polyethylene. Plast. Reconstr. Surg. Glob Open. 9 (12), e3985 (2021).
Hernando, J. et al. Reconstruction of liposarcoma resection defect with a made-to-measure polyethylene prosthesis using three-dimensional digital technology. J. Craniofac. Surg. 29 (1), e16–e17 (2018).
Funding
The experimental equipment and site are provided by Sichuan Medical Association Orthopaedics (ShangAnTong) Special Scientific Research Project (Grant No. 2024SAT07), Sichuan University-Zigong City Science and Technology Cooperation Project (Grant No. 2024CDZG-24), Zigong Key Science and Technology Plan (Collaborative Innovation Project of Zigong Academy of Big Data for Medical Science and Artificial Intelligence) (Grant No. 2024-YGY-01-03), Research Special Project of Chengdu Medical College Education Development Foundation (Grant No. 25LHZG-11) and Health Commission of Sichuan Province Medical Science and Technology Program (Grant No. 24CGZH03). There is no conflict of interest among all authors. All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
BW.Q and DW.S contributed the paper writing,C.W. and JY. D. contributed the construction, data analyze and paper revision. HG. H. and XG.W. contributed the clinical operation assistance. L.X. and H.L. completed the postoperative follow-up data collection. TC.Y. contributed the communication with patients.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, C., Shen, D., Qin, B. et al. Clinical application research on the titanium metal metatarsal prosthesis designed through FEA and manufactured by 3D printing. Sci Rep 15, 35491 (2025). https://doi.org/10.1038/s41598-025-19302-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-19302-1