Abstract
Childhood obesity and poor dietary habits represent significant public health challenges globally. Schools provide a crucial environment for interventions promoting physical activity and healthy eating behaviors due to their extensive reach and influential role in child development. This overview aims to synthesize evidence on the effectiveness of school-based interventions promoting physical activity and healthy eating behaviors among school-aged children, examining the role of behavior change techniques (BCTs) and behavioral determinants influencing their success. This study is an overview of systematic reviews and follows the Cochrane Handbook for Systematic Reviews of Interventions as well as the PRIOR (Preferred Reporting Items for Overviews of Reviews) statement. A literature searches until September 30, 2024, was performed in four electronic databases for this Overview: Cochrane database of systematic reviews, MEDLINE via PubMed, Epistemonikos, and PsycINFO. No language restrictions were imposed. Data were included and extracted from all systematic reviews evaluating interventions implemented in school settings targeting physical activity, healthy eating, or both, in children aged 6–11 years. Two reviewers independently screened the identified articles and extracted data related to the study characteristics, intervention components, behavioral outcomes (e.g., moderate-to-vigorous physical activity, dietary quality), cognitive outcomes (e.g., self-efficacy, knowledge, attitudes), and biological outcomes (e.g., BMI, waist circumference), classifying BCTs using standardized classifications whenever available. The AMSTAR-2 tool was used to evaluate the methodological quality of the included studies. Six systematic reviews, encompassing over 230,000 participants, were included. Multicomponent interventions combining physical activity, dietary education, cognitive strategies, and environmental modifications demonstrated consistent positive outcomes. Effective BCTs frequently identified included goal setting, self-monitoring, restructuring the physical environment, and providing feedback on behavior, especially via digital platforms. While significant improvements were consistently noted in behavioral outcomes such as increased physical activity and improved dietary habits, evidence regarding cognitive and biological outcomes like BMI reduction was moderate yet favorable. Methodological quality varied, with most reviews rated critically low, except for one high-quality Cochrane review. School-based interventions integrating multiple BCTs, particularly goal setting, self-monitoring, feedback, and environmental restructuring, are effective in promoting physical activity and healthy eating among school-aged children. Future interventions should emphasize long-term sustainability, technological integration, and address existing methodological limitations to enhance effectiveness and generalizability.
Systematic review registration Registered in PROSPERO CRD42024587296 on September 16, 2024.
Similar content being viewed by others
Introduction
Childhood obesity and unhealthy dietary habits have emerged as critical global public health issues, requiring action across multiple levels of influence as emphasized by the socio-ecological model1,2. According to the World Health Organization (WHO), the prevalence of childhood overweight and obesity has significantly increased over the past few decades, with an estimated 39 million children under the age of five classified as overweight or obese in 20223. This rise is associated with numerous health problems, including increased risk of cardiovascular disease, type 2 diabetes, and psychological disorders later in life4,5. Moreover, inadequate physical activity and poor nutrition during childhood can hinder cognitive development and academic performance6,7,8.
Promoting physical activity and healthy eating from an early age is essential for establishing lifelong healthy habits. Schools provide a unique and influential setting to address these behaviors within a socio-ecological framework, as they encompass individual, interpersonal, organizational, and community influences9. Physical activity plays a vital role in maintaining a healthy weight, strengthening bones and muscles, and improving mental health10. Similarly, a balanced diet—rich in fruits, vegetables, and whole grains, and low in ultra-processed foods—supports optimal growth and reduces the risk of developing chronic diseases11. Schools are key environments for implementing multi-component interventions that integrate educational, behavioral, and structural strategies, and the socio-ecological model provides a robust framework for understanding how multi-level influences interact to shape the effectiveness of school-based interventions12.
Previous multi-component school-based reviews have examined the effects of such interventions on physical activity, dietary habits, and obesity prevention. For example, Busch et al.13 reviewed school-based programs addressing multiple adolescent health behaviors; Amini et al.14 synthesized reviews on childhood obesity prevention; Love et al.15 explored the effectiveness and equity of physical activity interventions; and Pfldderer et al.16 compared rural versus urban/suburban contexts. These reviews highlight promising strategies but also reveal variability in effectiveness and a lack of integration between behavioral science frameworks and intervention design. This overview addresses this gap by explicitly linking behavioral determinants to theoretical frameworks, such as the theoretical domains framework (TDF) and the COM-B model, and by identifying effective Behavior Change Techniques (BCTs).
Behavioral determinants—such as motivation, social support, self-efficacy, and environmental factors—play a central role in shaping physical activity and dietary behaviors. These determinants can be systematically mapped to the domains of the TDF (e.g., Social Influences, Beliefs about Capabilities, Environmental Context and Resources)17 and to the components of the COM-B model (Capability, Opportunity, Motivation)18, which in turn guide the selection of relevant BCTs19, such as goal setting, social support, and self-monitoring. This structured linkage provides a practical, evidence-based approach for designing interventions that foster lasting behavior change20.
In the field of nutrition, the theory of planned behavior (TPB)21,22,23—which examines how attitudes, subjective norms, and perceived behavioral control predict intentions and behaviors—is frequently used to inform intervention strategies. The TPB and related theories, such as the theory of reasoned action, are incorporated into the integrative model of behavioral prediction, which aligns with several TDF domains, including social influences and beliefs about capabilities17. Similarly, self-determination theory24—which emphasizes the importance of intrinsic motivation—maps onto TDF domains such as reinforcement and motivation. Social support from peers and teachers, another key determinant, is also represented within the TDF Social Influences domain and is operationalized through specific BCTs, such as modeling or facilitating social comparison18,25.
Another key component to consider is the structural conditions within the school environment that support healthier behaviors—such as the built environment, regulatory measures, and the availability of affordable healthy food26. When evaluating regulatory measures and their effectiveness, it is useful to distinguish, as traditionally noted by public administration scholars, between “the carrot, the stick, and the sermon”27.
Despite acknowledging the importance of school-based interventions, the effectiveness of these programs varies widely. This may be due to differences in design, implementation, contextual factors, and the extent to which behavioral determinants, theory-based frameworks, and supportive structural changes are integrated28,29. This article adopts a behavioral science approach17,18,30,31, applying the COM-B model, the TDF, and BCT taxonomy to synthesize evidence from school-based interventions promoting physical activity and healthy eating.
This overview of systematic reviews aims to synthesize evidence on the effectiveness of school-based interventions for promoting physical activity and healthy eating in schoolchildren. Additionally, it explores the role of behavioral determinants in influencing the success of these interventions. By addressing identified gaps in previous reviews and integrating behavioral science frameworks, this review provides valuable insights for policymakers, educators, and public health professionals in the implementation of strategies aimed at reducing the prevalence of childhood obesity and promoting healthier lifestyles in the school environment32.
Methods
Study design
This study is an overview of systematic reviews and adheres to the Cochrane Handbook for Systematic Reviews of Interventions33 and the PRIOR (Preferred Reporting Items for Overviews of Reviews) statement34. The PRIOR checklist is reported in Supplementary Material Appendix 1; and sex and gender equity in research (SAGER) guidance35, in Supplementary Material Appendix 2.
Protocol and registration
The protocol for this overview was prospectively registered in PROSPERO (CRD42024587296) on September 16, 2024 (Supplementary Material Appendix 3). In writing and reporting this overview, we followed the Cochrane Handbook for Systematic Reviews of Interventions and the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines36. The complete protocol can be downloaded from this link in PROSPERO37.
Patient and public involvement
Patients and the public were not involved in the design or conduct of this study. Therefore, no ethical approval was required for this overview.
Eligibility criteria
The eligibility criteria were reported in detail in our protocol (Supplementary Material Appendix 3). The inclusion criteria for this overview were based on the population, intervention, comparison, outcome, and study type (PICOS) framework (Table 1). No restrictions on language or publication status were applied during study selection, ensuring the inclusion of all potentially relevant evidence regardless of the original language of publication.
We included reviews reporting outcomes related to physical activity, healthy eating behaviors, and anthropometric measures (BMI, BMI z-scores, nutritional status categories, waist circumference). Anthropometric measures were eligible whether they were synthesized at the review level (via meta-analysis or narrative synthesis) or reported within individual interventions included in the review, even when no aggregate synthesis was performed for these measures. This approach ensured the inclusion of relevant evidence on body composition and weight-related outcomes across a range of review designs and reporting formats.
All systematic reviews (SRs) were included, operationally defined as any secondary research that included only primary clinical studies, with an explicit search strategy in at least two databases33,39.
Information sources
This overview employed a comprehensive search strategy across MEDLINE (via PubMed), the Cochrane Database of Systematic Reviews (CDSR), Epistemonikos, and PsycINFO. To ensure completeness, reference lists of included reviews were screened, and supplementary searches were conducted, including manual reference checks, citation searching (n = 293), and additional records from websites (n = 4) and organizations (n = 1). All sources were critically evaluated, with search details documented for transparency, and search strategies are available in Supplementary Material Appendix 4.
Search strategy
The electronic search strategy (Supplementary Material Appendices 5 and 6) was conducted from database inception to September 30, 2024, with no restrictions. Additional searches included manual bibliography screening and outreach to authors and experts to identify further eligible studies. Eligibility criteria are detailed in Table 1.
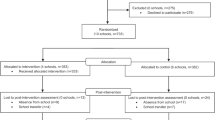
Study selection process
After de-duplication using Rayyan™ software40 and pilot testing, two independent reviewers (GD and AB) screened titles and abstracts, followed by full texts, in a blinded manner within Rayyan™. Prior to formal screening, the team conducted a calibration exercise on a random sample of 50 records to harmonize the application of eligibility criteria and establish consensus-based decision rules. Throughout the screening process, a senior reviewer (GF) performed periodic quality checks to ensure adherence to the protocol. Rayyan™ was used to manage the screening workflow, including importing references, automatic de-duplication, applying inclusion/exclusion labels, maintaining an audit trail of decisions, and flagging conflicts for resolution. Disagreements were resolved through discussion and, when necessary, adjudicated by the third reviewer (GF). Reasons for full-text exclusions were recorded in Rayyan™ and are reported in Supplementary Material Appendix 7.
At the title and abstract screening stage, 428 records were excluded because they did not meet one or more eligibility criteria (e.g., wrong population age group, not a school-based setting, non-prevention focus, or not a systematic review). In accordance with Cochrane guidance33, detailed reasons are reported only for the 39 full-text articles that were assessed but excluded; these are listed in Supplementary Material Appendix 7.
The inter-rater reliability was assessed using Cohen’s kappa coefficient41. Two independent reviewers evaluated the full texts (see Supplementary Material Appendix 8).
Data collection process
We developed a data extraction tool in Microsoft Excel to collect various study data recommended by Cochrane42,43. The data extracted from the included systematic reviews were tested and calibrated within the team (Supplementary Material Appendix 9). For this purpose, one author initially created the spreadsheet and extracted data from a single systematic review. Subsequently, two authors (GD and AB) independently extracted data from three systematic reviews, and all authors provided feedback on whether the data elements were complete and the extracted data unambiguous.
During this calibration phase, inter-rater agreement between GD and AB was 92% across 135 extracted items, with discrepancies (n = 11) mainly related to the categorization of BCTs and intervention outcomes. These discrepancies were resolved through discussion, with one case requiring adjudication by a senior reviewer (GF).
Once consensus was reached, one author created a data extraction manual for the spreadsheet, which is available in Supplementary Material Appendix 10.
Data items
Data items included systematic review characteristics; PICOS criteria; and variables related to digital behavior change intervention (Table 2).
Quality appraisal of the included systematic reviews
We performed critical appraisals of systematic reviews using AMSTAR-244, as outlined in our protocol (Supplementary Material Appendix 3). AMSTAR-2 consists of 16 items that evaluate the thoroughness of various elements within the systematic reviews, such as the preparation process, literature search, study selection, data extraction, and analysis, as well as potential biases (e.g., risk of bias, publication bias, or funding sources). Based on the type and number of weaknesses identified (i.e., unmet items), the reviews were assigned a confidence rating: high, moderate, low, or critically low.
Two authors independently (GD and AB) assessed all systematic reviews using an Excel spreadsheet (version 10; Microsoft Inc.), reaching consensus through discussion (Supplementary Material Appendix 11).
Overlap in primary studies included in reviews
To ensure the accuracy of primary study outcome data and prevent double counting, we first evaluated whether the included systematic reviews shared overlapping primary studies. This assessment was conducted by creating a citation matrix and calculating the overall corrected covered area (CCA) using the GROOVE (Graphical Representation of Overlap for Overviews) tool45. The GROOVE tool provides a method for interpreting the extent of overlap, where a CCA of 0–5% indicates a slight overlap, 6–10% a moderate overlap, 11–15% a high overlap, and greater than 15% a very high overlap in primary studies cited in multiple systematic reviews.
Data synthesis methods
The findings of the included systematic reviews were synthesized narratively and organized into summary tables describing their characteristics, methodological quality, and key outcomes. Data were extracted using a standardized template (Supplementary Material Appendix 9) and structured around core categories: type of intervention and mode of delivery; who provided the intervention and how; where, when, and how much; review period; number and design of included studies; population and sample size; outcomes of interest; intervention effectiveness; effectiveness of BCTs or components; and most frequently used BCTs.
Whenever possible, interventions were coded using the Behavior Change Technique Taxonomy version 1 (BCTTv1) and the theoretical domains framework (TDF)17,46. The extraction of BCTs was primarily based on those explicitly reported by the original review authors. In cases where BCTs were not identified in the included reviews, a trained researcher with expertise in BCT coding independently coded the intervention descriptions using the BCT Taxonomy v1 framework19,47. This approach allowed for consistent identification and classification of behavior change mechanisms across studies. Where coding was not feasible due to insufficient detail, the original descriptions provided by the authors were retained.
Outcomes were grouped into three primary domains: (1) behavioral outcomes, including physical activity levels, sedentary time, dietary habits (e.g., fruit/vegetable intake, water consumption), and adherence to healthy routines (e.g., active commuting); (2) cognitive outcomes, such as knowledge, self-efficacy, and attitudes toward healthy behaviors; and (3) biological outcomes, such as BMI or zBMI, waist circumference, nutritional status, and physical fitness.
To assess the effectiveness of BCTs, we developed a matrix mapping the presence and strength of each BCT across outcome types and reviews. A five-level coding system was applied: “▾” for strong evidence of a negative effect, “O” for mixed or null evidence, “O−” and “O+” for limited evidence of a negative or positive effect, respectively, and “▴” for strong evidence of a positive effect. This classification, adapted from Michie et al. approach of Michie et al.46,48, allowed us to compare intervention components across heterogeneous reviews and outcomes.
AMSTAR-2 was used to assess methodological quality, and meta-analysis or GRADE results were recorded when available. Sex and gender were analyzed using the SAGER Guidelines35, to determine whether sex-disaggregated data were reported and whether interventions considered gender-related differences in outcomes or implementation. These guidelines helped ensure a rigorous and equitable analysis of how interventions may differentially impact boys and girls (Supplementary Materials Appendix 12).
Finally, where possible, cross-review comparisons were made to identify converging patterns in effective components (e.g., use of self-monitoring, goal setting, or environmental restructuring) and to examine consistency of effects across settings, populations, and delivery modes.
Results
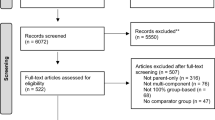
From a total of 483 identified records, 45 full-text articles were assessed for eligibility. Of these, 39 were excluded, leading to the inclusion of 6 systematic reviews in this overview49,50,51,52,53,54 (Fig. 1). The inter-rater reliability for full-text screening was robust (Kappa = 0.89). Additional studies were identified through supplementary methods, including website searches, and citation searching, ensuring a comprehensive review (Supplementary Material Appendix 4).
Characteristics of systematic reviews
A total of six systematic reviews published between 2018 and 2024 were included. The number of primary studies per review ranged from 13 to 172, covering 230.915 participants combined. The included studies were published between 2004 and 2023 and were conducted mostly in high-income countries such as the United States, United Kingdom, Australia, Canada, and several European nations, based on the World Bank classifications55 (Supplementary Material Appendix 13).
All reviews included randomized controlled trials (RCTs), with five also incorporating non-randomized or observational studies. One review54 included only RCTs. All six reviews included children under 11 years of age, although some also included adolescents. The interventions were implemented primarily in school or school-related settings (e.g., after-school programs, active school transport initiatives). All data are reported, and the detailed characteristics of the individual systematic reviews are presented in Supplementary Material Appendices 13 and 14. The synthesis of study characteristics across all six systematic reviews is shown in Table 3. Additionally, to provide a quick reference, Table 4 presents a condensed summary of each included review, focusing on the author, population, intervention, number of studies, study designs, and main findings.
Characteristics of the interventions
Scope and focus of interventions
The characteristics of interventions reviewed consistently underscore schools as critical environments for promoting physical activity and healthy eating behaviors among children. Four reviews specifically addressed physical activity promotion50,51,53,54, while five reviews targeted combined interventions incorporating both physical activity and healthy eating49,51,52,53,54 as detailed in Table 3. Comprehensive interventions addressing both behaviors generally showed greater effectiveness compared to interventions targeting single domains alone.
Structural and environmental modifications
Structural and environmental changes emerged as integral to effective intervention strategies. Five reviews emphasized specific environmental modifications, such as upgrading playground facilities, improving walking and cycling infrastructure, cafeteria enhancements, and the introduction of school gardens49,51,52,53,54. These structural approaches were consistently linked to positive behavioral outcomes and were usually implemented as part of broader multi-component interventions. They contributed to increased availability of, and access to, spaces for physical activity and healthy food options.
Duration and frequency of activities
Duration and frequency of intervention activities were identified as critical determinants of effectiveness. While intervention periods varied significantly from 6 weeks to 2 years, interventions exceeding 6 months with extended follow-up periods of at least 12 months generally demonstrated greater success in establishing sustained healthy behaviors49,52,54. Effective interventions also employed regular engagement strategies, with activities occurring daily or weekly.
Use of theory
Explicit theoretical grounding was noted in three reviews, which referenced the use of Social Cognitive Theory and Self-Determination Theory49,52,54. Only one study reported the use of specific BCTs, such as goal setting, self-monitoring, and feedback49.
The inclusion of technological components was relatively limited but demonstrated moderate effectiveness. Specifically, two reviews evaluating wearable activity trackers and mobile feedback systems highlighted their potential utility in increasing children’s physical activity levels50,54.
Technological components
In summary, interventions combining physical activity and healthy eating, supported by structural modifications, sustained durations, and regular participant engagement, consistently yielded significant positive outcomes. These findings, explicitly detailed in Table 5, emphasize the necessity for comprehensive, theoretically-informed, and strategically integrated interventions within educational settings (Table 5 and Supplementary Material Appendices 13 and 14).
Effectiveness of interventions
Effectiveness according to behavior change techniques (BCTs)
The most frequently reported BCTs identified in the included systematic reviews were goal setting (BCT 1.1), self-monitoring of behavior (BCT 2.3), and restructuring the physical environment (BCT 12.1). These techniques demonstrated robust evidence regarding their effectiveness in improving both physical activity levels and healthy eating behaviors. For instance, Klein et al.52 highlighted that interventions combining physical activity and nutritional components significantly improved body mass index (BMI), waist circumference, and body fat percentage. In this context, BCTs such as goal setting and self-monitoring were explicitly identified as effective components supporting adherence to healthy behaviors among school-aged children (see Tables 5 and 6).
The use of feedback on behavior (BCT 2.2) showed moderate yet consistent effects, particularly when provided through digital devices such as wearable trackers or mobile apps. Casado-Robles et al.50, through their systematic review and meta-analysis, found that wearable device-based interventions significantly increased daily physical activity (mean increase of 1692 steps/day; p < 0.001; d = 0.220 for moderate-to-vigorous physical activity), along with modest reductions in sedentary time (d = 0.172; p = 0.011). These effects appeared particularly beneficial among less active adolescents and female participants, who typically exhibit lower baseline activity levels (see Tables 5 and 6).
Regarding the technique information about health consequences (BCT 5.1), findings were mixed. However, this BCT was notably effective for sustaining long-term behavior change. Allcott-Watson et al.49 specifically identified this technique as promising, especially for maintaining healthy dietary behaviors beyond the intervention period. Complementary techniques such as problem-solving (BCT 1.2) and action planning (BCT 1.4) were also reported to be effective in promoting medium- and long-term dietary behavior changes, notably improving the consumption of fruits and vegetables (see Tables 5 and 6).
Behavioral outcomes
All six systematic reviews reported improvements in physical activity and dietary behaviors. There were consistent increases in moderate-to-vigorous physical activity (MVPA), daily step counts, and reductions in sedentary time. Dai51 reported that culturally tailored interventions involving family participation significantly improved MVPA among children from disadvantaged settings. Spiga et al.54 demonstrated small yet statistically significant BMI z-score reductions (− 0.05; 95% CI − 0.09 to − 0.02; p < 0.05), emphasizing the combined effectiveness of dietary and physical activity interventions compared to diet-only approaches (see Tables 5 and 6).
Adherence to healthy behaviors, such as increased water consumption and healthier snack choices, was notably higher in interventions explicitly using the aforementioned BCTs (e.g., Klein et al.52; Larouche et al.53; see Table 5).
Cognitive outcomes
Four systematic reviews50,51,52,54 reported improvements in self-efficacy, frequently associated with educational and motivational components, such as goal-setting, counseling sessions, and personalized feedback. Three reviews51,52,54 documented significant increases in knowledge about healthy eating and positive shifts in attitudes toward physical activity. However, these outcomes were often assessed through self-report measures, somewhat limiting the certainty of these results (see Tables 5 and 6).
Biological outcomes
All systematic reviews reported biological measures such as BMI, zBMI, waist circumference, and physical fitness levels. The strongest evidence was provided by Spiga et al.54, which reported moderate-certainty evidence for BMI reductions at medium-term follow-up, clinically relevant for childhood obesity prevention (mean difference zBMI: − 0.05; 95% CI − 0.09 to − 0.02; p < 0.05; see Tables 5 and 6).
Additional clinical biomarkers such as blood glucose or cholesterol levels were rarely reported. Klein et al.52 was one of the few reviews mentioning these biomarkers, although not systematically analyzed (see Table 5).
Sex and gender equity in research (SAGER) application
The application of the sex and gender equity in research (SAGER) guidelines revealed that most of the reviewed studies included sex- or gender-disaggregated data, although in some cases, this information was limited. In general, significant differences between boys and girls were observed, with boys typically exhibiting higher levels of physical activity, while girls demonstrated greater adherence to dietary interventions. One study, Dai51, specifically reported that girls had lower baseline physical activity levels but showed greater improvements post-intervention. Nevertheless, the absence of explicit gender-specific analyses in some studies restricts the depth of conclusions related to equity (Supplementary Material Appendices 15 and 16).
Quality appraisal of the included systematic reviews
Overall, confidence in the results of the systematic reviews was high in 17% (1/6) of the reviews, moderate in 0%, low in 0%, and critically low in 83% (5/6). The most frequent methodological weaknesses identified were lack of a complete list of excluded studies (5/6 reviews, 83%49,50,51,52,53), no reporting of funding sources for primary studies (5/6 reviews, 83%; same five as above), and absence of a registered or published review protocol (2/6 reviews, 33%51,52).
By contrast, the Cochrane review by Spiga et al.54 was rated as high quality, fulfilling all AMSTAR-2 critical domains (see Table 7; For full details, see Supplementary Material Appendix 17).
Overlap in primary studies included in reviews
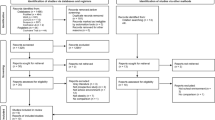
The overlap assessment revealed that most primary studies were cited only once across the systematic reviews. Overall, there was a minimal overlap in the 293 primary studies included in the 6 systematic reviews, with a Corrected Covered Area (CCA) of 0.82. Comparisons between pairs of systematic reviews indicated that 93% (14 out of 15) had a low overlap (< 5%), 6% (1 out of 15) had a moderate overlap (5% to < 10%), and none of the comparisons showed high (10% to < 15%) or very high (≥ 15%) overlap. These findings are illustrated in Fig. 2 and detailed in Supplementary Material Appendices 18 and 19.
Discussion
Principal results
This overview of systematic reviews synthesized evidence from six comprehensive reviews evaluating the effectiveness of school-based interventions aimed at promoting physical activity and healthy eating. The findings confirm that BCTs—such as goal setting (1.1), self-monitoring of behavior (2.3), and restructuring the physical environment (12.1), including spaces for healthier food consumption—consistently show strong evidence of effectiveness in improving PA levels and dietary behaviors in school settings. Framed within the COM-B model18, these BCTs influence behavior by enhancing capability (e.g., self-monitoring increases self-awareness and goal-directed behavior), opportunity (e.g., environmental restructuring provides supportive contexts for behavior), and motivation (e.g., goal setting promotes clear intentions and intrinsic motivation).
Additionally, techniques such as feedback on behavior (2.2) and information about health consequences (5.1) exhibited moderate effectiveness, particularly through digital platforms, likely due to their capacity to deliver timely, personalized feedback that enhances reflective motivation. Importantly, social support techniques, including unspecified (3.1), practical (3.2), emotional (3.3) support, social reward (10.4), and social incentives (10.5), were identified as essential in facilitating healthy behaviors in school settings. The involvement of parents, teachers, teaching assistants, and the broader social environment within schools provides critical emotional encouragement, practical assistance, and reinforcement, significantly bolstering children’s adherence and engagement in physical activity and healthy eating interventions. Biological outcomes, notably BMI reductions, showed modest but clinically relevant improvements, reinforcing the utility of comprehensive, multicomponent interventions.
Comparison with prior work
Our findings align with previous overviews and systematic reviews suggesting that multicomponent school-based interventions integrating physical, dietary, cognitive, and environmental elements are more effective than single-domain interventions. Consistent with the existing literature, goal setting and self-monitoring were repeatedly identified as effective BCTs in promoting sustained behavioral change. Additionally, similar to earlier studies, we found that feedback mechanisms, particularly those utilizing digital tools, significantly enhance intervention effectiveness. Moreover, our results regarding modest but significant BMI reductions align with previous evidence, underscoring the importance of sustained, integrated interventions for childhood obesity prevention.
Importantly, recent evidence from Imad et al.56 provides a complementary perspective. Their umbrella review mapped components of obesity prevention interventions and highlighted that not all multicomponent strategies yield favorable BMI outcomes. For instance, diet-only interventions in primary school settings and some broad school-based programs were frequently classified as likely ineffective for BMI/zBMI. In contrast, curriculum modifications in physical education and policies targeting the school food environment were identified as the most consistently effective components. Our overview complements these findings by expanding the focus beyond anthropometric indicators to include behavioral and cognitive outcomes, and by systematically coding intervention content using BCTTv1 and the TDF. This approach clarifies how effective components—such as goal setting, self-monitoring, and social support—operate within school contexts, providing insights into mechanisms of change that can inform the design of future interventions.
Taken together, these findings not only reinforce the theoretical and methodological evidence base but also have direct implications for public health practice.
Public health implications
Beyond theoretical and methodological advances, these findings have direct public health relevance. Schools represent one of the most equitable and scalable platforms for influencing children’s health trajectories, reaching diverse populations during critical developmental stages. Embedding evidence-based strategies—such as goal setting, self-monitoring, and supportive school food and physical activity environments—into school health policies and curricula can strengthen long-term obesity prevention efforts, help reduce inequities, and ensure a sustainable impact at the population level.
Sex and gender equity in research (SAGER)
A notable strength of this synthesis is the explicit incorporation of sex and gender equity in research (SAGER) guidelines, which facilitated the identification of important gender-specific differences in intervention effectiveness. The majority of reviewed studies included sex- or gender-disaggregated data, though with some limitations in detail. Notably, boys generally exhibited higher baseline levels of physical activity, while girls demonstrated greater adherence and improvement in dietary interventions. For instance, Dai51 reported that girls, despite lower initial physical activity levels, showed substantial improvements following interventions, emphasizing the critical need for tailored strategies addressing gender-specific behaviors and barriers. Nonetheless, the absence of detailed gender-specific analyses in some reviews limits the depth of conclusions related to equity, underscoring a vital area for future research.
Evidence gaps
Despite the comprehensive nature of the included reviews, several important evidence gaps were identified. First, few reviews systematically assessed or explicitly reported long-term adherence to healthy behaviors beyond the immediate post-intervention period. Additionally, most reviews focused on studies conducted in high-income countries, which may limit the generalizability of findings to low- and middle-income settings, where different behavioral determinants could influence the effectiveness of interventions.
There was also limited evidence regarding the effectiveness of BCTs that target emotional and motivational components, such as reducing negative emotions (BCT 11.2) or using self-incentives (BCT 10.7). This highlights a need for further research into strategies that address these dimensions of behavior.
Another notable limitation across studies was the selection of outcome indicators. For instance, using changes in zBMI scores to evaluate interventions targeting both healthy eating and physical activity may fail to capture meaningful behavioral improvements. In some cases, positive changes in dietary habits or physical activity levels may occur without being reflected in anthropometric indicators, suggesting the need for broader and more sensitive outcome measures.
Finally, conducting a meta-meta-analysis or meta-regression was not feasible due to substantial methodological and statistical heterogeneity across the included reviews (e.g., population age ranges, intervention types, outcome measures, and analytic strategies). Furthermore, the critically low methodological quality of most included reviews (per AMSTAR-2) limited the appropriateness of higher-level quantitative pooling. Instead, this overview synthesized the evidence qualitatively and systematically mapped intervention strategies and BCTs, providing actionable insights that complement prior meta-analytic evidence.
Strengths and limitations
This overview benefits from rigorous methodology, including adherence to PRISMA guidelines, comprehensive searches across multiple databases, and systematic methodological quality assessments using AMSTAR-2. Furthermore, applying the BCTTv1 allowed systematic identification and comparison of effective components. However, limitations include potential bias due to the critical low methodological quality ratings of most included systematic reviews. Additionally, significant heterogeneity in intervention duration, delivery modes, and measurement methods across primary studies limits precise comparative analyses.
A notable strength of this overview is the minimal overlap of primary studies across the included systematic reviews. Specifically, the corrected covered area (CCA) was very low (0.82%), indicating a highly efficient and complementary coverage of the literature. This minimal overlap ensures that the synthesized evidence provides a comprehensive representation of existing interventions, thus enhancing confidence in the robustness and breadth of our conclusions.
Conclusions
This overview highlights that multicomponent, school-based interventions are effective in improving physical activity, dietary behaviors, and related biological outcomes in children. Key BCTs—such as goal setting, self-monitoring, environmental restructuring, and the use of digital feedback mechanisms—consistently yield positive results.
For successful implementation, educational institutions should invest in teacher training programs focused on BCTs, enhance school infrastructure to support active environments, increase the availability of healthy food options, and incorporate digital tools for behavior monitoring and feedback. Additionally, it is essential to examine the environmental conditions that support physical activity and healthy eating. These include the availability of infrastructure and equipment, access to affordable healthy food options, the presence of healthy foods in school cafeterias, internal school policies that limit access to unhealthy foods, and broader regulatory measures in surrounding areas that promote healthy environments. This calls for an intervention approach grounded in a socio-ecological model.
Addressing the identified evidence gaps—particularly those related to the long-term sustainability of behavior change and the limited use of BCTs targeting emotional and motivational aspects—is critical. Future research should prioritize methodological rigor, incorporate explicit theoretical frameworks, apply gender-sensitive approaches, and promote equity in intervention design. Above all, it should assess the structural conditions that enable the adoption and maintenance of healthy behaviors.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AMSTAR-2:
-
A MeaSurement Tool to Assess systematic Reviews 2
- BCT:
-
Behavior change technique
- BCTTv1:
-
Behavior change technique taxonomy version 1
- BMI:
-
Body mass index
- CDSR:
-
Cochrane database of systematic reviews
- CCA:
-
Corrected covered area
- GRADE:
-
Grading of recommendations, assessment, development, and evaluation
- MVPA:
-
Moderate-to-vigorous physical activity
- OSF:
-
Open science framework
- PICOs:
-
Population, intervention, comparison, outcome, study type
- RCT:
-
Randomized controlled trial
- SAGER:
-
Sex and gender equity in research
- SR:
-
Systematic review
- TDF:
-
Theoretical domains framework
References
Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design (Harvard University Press, 1979). Available: https://www.hup.harvard.edu/books/9780674224575.
McLeroy, K. R., Bibeau, D., Steckler, A. & Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 15, 351–377. https://doi.org/10.1177/109019818801500401 (1988).
World Health Organization. Obesity and Overweight. [cited 4 Sep 2024]. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Sahoo, K. et al. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 4, 187–192. https://doi.org/10.4103/2249-4863.154628 (2015).
Barton, M. Childhood obesity: A life-long health risk. Acta Pharmacol. Sin. 33, 189–193. https://doi.org/10.1038/aps.2011.204 (2012).
Asigbee, F. M., Whitney, S. D. & Peterson, C. E. The link between nutrition and physical activity in increasing academic achievement. J. Sch. Health 88, 407–415. https://doi.org/10.1111/josh.12625 (2018).
Martin, A., Booth, J. N., Laird, Y., Sproule, J., Reilly, J. J. & Saunders, D. H. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Library (2018). [cited 16 Sep 2024]. Available: https://doi.org/10.1002/14651858.CD009728.pub3/full.
Donnelly, J. E. et al. Physical activity, fitness, cognitive function, and academic achievement in children: A systematic review. Med. Sci. Sports Exerc. 48, 1197–1222. https://doi.org/10.1249/MSS.0000000000000901 (2016).
Story, M., Kaphingst, K. M., Robinson-O’Brien, R. & Glanz, K. Creating healthy food and eating environments: Policy and environmental approaches. Annu. Rev. Public Health 29, 253–272. https://doi.org/10.1146/annurev.publhealth.29.020907.090926 (2008).
Janssen, I. & LeBlanc, A. G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 7, 40. https://doi.org/10.1186/1479-5868-7-40 (2010).
World Health Organization. Healthy Diet. [cited 4 Sep 2024]. Available: https://www.who.int/news-room/fact-sheets/detail/healthy-diet.
Watson, A., Timperio, A., Brown, H., Best, K. & Hesketh, K. D. Effect of classroom-based physical activity interventions on academic and physical activity outcomes: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 14, 114. https://doi.org/10.1186/s12966-017-0569-9 (2017).
Busch, V., de Leeuw, J. R. J., de Harder, A. & Schrijvers, A. J. P. Changing multiple adolescent health behaviors through school-based interventions: A review of the literature. J. Sch. Health 83, 514–523. https://doi.org/10.1111/josh.12060 (2013).
Amini, M., Djazayery, A., Majdzadeh, R., Taghdisi, M.-H. & Jazayeri, S. Effect of school-based interventions to control childhood obesity: A review of reviews. Int. J. Prev. Med. 6, 68. https://doi.org/10.4103/2008-7802.162059 (2015).
Love, R., Adams, J. & van Sluijs, E. M. F. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes. Rev. 20, 859–870. https://doi.org/10.1111/obr.12823 (2019).
Pfledderer, C. D. et al. School-based physical activity interventions in rural and urban/suburban communities: A systematic review and meta-analysis. Obes. Rev. 22, e13265. https://doi.org/10.1111/obr.13265 (2021).
Cane, J., O’Connor, D. & Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 7, 37. https://doi.org/10.1186/1748-5908-7-37 (2012).
Michie, S., van Stralen, M. M. & West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 6, 42. https://doi.org/10.1186/1748-5908-6-42 (2011).
Michie, S. et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 46, 81–95. https://doi.org/10.1007/s12160-013-9486-6 (2013).
Trethewey, S. P., Reynolds, E. K. & Trethewey, C. S. Behavioural determinants of health: Individual versus societal responsibility. Br. J. Gen. Pract. 71, 301–302. https://doi.org/10.3399/bjgp21X716237 (2021).
Sajjad, M., Bhatti, A., Hill, B. & Al-Omari, B. Using the theory of planned behavior to predict factors influencing fast-food consumption among college students. BMC Public Health 23, 987. https://doi.org/10.1186/s12889-023-15923-1 (2023).
Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 50, 179–211. https://doi.org/10.1016/0749-5978(91)90020-T (1991).
Taghdisi, M. H., Babazadeh, T., Moradi, F. & Shariat, F. Effect of educational intervention on the fruit and vegetables consumption among the students: Applying theory of planned behavior. J. Res. Health Sci. 16, 195–199 (2016).
Ryan, R. M. & Deci, E. L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 55, 68–78. https://doi.org/10.1037/0003-066x.55.1.68 (2000).
Van der Horst, K. et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ. Res. 22, 203–226. https://doi.org/10.1093/her/cyl069 (2007).
Jaime, P. C. & Lock, K. Do school based food and nutrition policies improve diet and reduce obesity?. Prev. Med. 48, 45–53. https://doi.org/10.1016/j.ypmed.2008.10.018 (2009).
Tummers, L. Public policy and behavior change. Public Adm. Rev. 79, 925–930. https://doi.org/10.1111/puar.13109 (2019).
Jayasinghe, S. & Hills, A. P. Strategies to improve physical activity and nutrition behaviours in children and adolescents: A review. Nutrients 15, 3370. https://doi.org/10.3390/nu15153370 (2023).
Langford, R., Bonell, C. P., Jones, H. E., Pouliou, T., Murphy, S. M., Waters, E., et al. The WHO health promoting school framework for improving the health and well‐being of students and their academic achievement—Langford, R. Cochrane Library (2014). [cited 4 Sep 2024]. Available: https://doi.org/10.1002/14651858.CD008958.pub2/full.
Duarte, G. et al. Introduction to behavioral science and its practical applications in public health. Medwave 25, e3017. https://doi.org/10.5867/medwave.2025.01.3017 (2025).
Armayones Ruiz, M. et al. Barriers and facilitators for safe sex behaviors in students from universidad de Santiago de Chile (USACH) through the COM-B model. BMC Public Health 23, 677. https://doi.org/10.1186/s12889-023-15489-y (2023).
Katz, D. L., O’Connell, M., Njike, V. Y., Yeh, M.-C. & Nawaz, H. Strategies for the prevention and control of obesity in the school setting: Systematic review and meta-analysis. Int. J. Obes. (Lond.) 32, 1780–1789. https://doi.org/10.1038/ijo.2008.158 (2008).
Pollock, M., Fernandes, R. M., Becker, L. A., Pieper, D., Hartling, L. & Chapter, V. Overviews of reviews. In: Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane (eds Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J. & Welch, V. A.) (2022). www.training.cochrane.org/handbook. [Internet]. [cited 4 Dec 2022]. Available: https://training.cochrane.org/handbook/current/chapter-v.
Gates, M. et al. Reporting guideline for overviews of reviews of healthcare interventions: Development of the PRIOR statement. BMJ 378, e070849. https://doi.org/10.1136/bmj-2022-070849 (2022).
Heidari, S., Babor, T. F., De Castro, P., Tort, S. & Curno, M. Sex and gender equity in research: Rationale for the SAGER guidelines and recommended use. Res. Integr. Peer Rev. 1, 2. https://doi.org/10.1186/s41073-016-0007-6 (2016).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339, 2535. https://doi.org/10.1136/bmj.b2535 (2009).
Duarte, G., de Oliveira Barbosa, A., Ferrari, G., Araneda-Flores, J., Arancibia, D., Pinheiro-Fernandes, A. et al. Promoting physical activity and healthy eating in school settings: Protocol for an overview of systematic reviews and the impact of behavioral determinants in children aged 11 and under. PROSPERO (2024). CRD42024587296. [cited 26 Nov 2024]. Available: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024587296.
Food and Agriculture Organization of the United Nations. FAO School Food and Nutrition Framework. [cited 4 Sep 2024]. Available: https://openknowledge.fao.org/items/679d1e4a-a5e0-4eba-9758-e76dd7cf376b.
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. J. Cochrane handbook for systematic reviews of interventions. In: Version 6.3 (Updated February 2022). Cochrane (2022). [Internet]. [cited 24 Nov 2022]. Available: https://handbook-5-1.cochrane.org/.
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 5, 210. https://doi.org/10.1186/s13643-016-0384-4 (2016).
Viera, A. J. & Garrett, J. M. Understanding interobserver agreement: The kappa statistic. Fam. Med. 37, 360–363 (2005).
Cochrane Consumers and Communication La Trobe University, Ryan, R., Synnot, A. M. P. & Hill, S. Data Extraction Template (2018) [cited 25 May 2024]. https://doi.org/10.26181/5b57cfd711743
Ryan, R. & Hill, S. Supporting implementation of cochrane methods in complex communication reviews: Resources developed and lessons learned for editorial practice and policy. Health Res. Policy Syst. 17, 32. https://doi.org/10.1186/s12961-019-0435-0 (2019).
Shea, B. J. et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358, j4008. https://doi.org/10.1136/bmj.j4008 (2017).
Bracchiglione, J. et al. Graphical representation of overlap for OVErviews: GROOVE tool. Res. Synth. Methods 13, 381–388. https://doi.org/10.1002/jrsm.1557 (2022).
Michie, S., West, R., Sheals, K. & Godinho, C. A. Evaluating the effectiveness of behavior change techniques in health-related behavior: A scoping review of methods used. Transl. Behav. Med. 8, 212–224. https://doi.org/10.1093/tbm/ibx019 (2018).
Castro, O. et al. Translating the behaviour change technique taxonomy version 1 into Spanish: Methodology and validation. Wellcome Open Res. 9, 298. https://doi.org/10.12688/wellcomeopenres.21388.1 (2024).
Mair, J. L. et al. Effective behavior change techniques in digital health interventions for the prevention or management of noncommunicable diseases: An umbrella review. Ann. Behav. Med. 57, 817–835. https://doi.org/10.1093/abm/kaad041 (2023).
Allcott-Watson, H., Chater, A., Troop, N. & Howlett, N. A systematic review of interventions targeting physical activity and/or healthy eating behaviours in adolescents: Practice and training. Health Psychol. Rev. 18, 117–140. https://doi.org/10.1080/17437199.2023.2173631 (2024).
Casado-Robles, C., Viciana, J., Guijarro-Romero, S. & Mayorga-Vega, D. Effects of consumer-wearable activity tracker-based programs on objectively measured daily physical activity and sedentary behavior among school-aged children: A systematic review and meta-analysis. Sports Med. Open 8, 18. https://doi.org/10.1186/s40798-021-00407-6 (2022).
Dai, C.-L. School health program: Impacting physical activity behaviors among disadvantaged students. J. Sch. Health 89, 468–475. https://doi.org/10.1111/josh.12758 (2019).
Klein, D. H. et al. Impact of school-based interventions on pediatric obesity: A systematic review. Cureus 15, e43153. https://doi.org/10.7759/cureus.43153 (2023).
Larouche, R., Mammen, G., Rowe, D. A. & Faulkner, G. Effectiveness of active school transport interventions: A systematic review and update. BMC Public Health 18, 206. https://doi.org/10.1186/s12889-017-5005-1 (2018).
Spiga, F. et al. Interventions to prevent obesity in children aged 5 to 11 years old. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD015328.pub2 (2024).
World Bank Country and Lending Groups. World Bank Data Help Desk. [cited 30 May 2024]. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
Imad, N. et al. Identifying effective obesity prevention intervention components: An umbrella review mapping systematic review evidence. Obes. Rev. 26, e13878. https://doi.org/10.1111/obr.13878 (2025).
Acknowledgements
We acknowledge to officials and managers of the Gabriela Mistral Local Education Service (SLEP-GM), Santiago, Chile.
Funding
This study is funded by the Agencia Nacional de Investigación y Desarrollo (ANID) Chile through the Proyecto FONDEF 2023, grant agreement no. FONDEFIT23I0031. The funders had no role in the study design; collection, analysis, and interpretation of the data; writing of the report; or decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by GD, AP, TP and AB. Methodology: GD, AB, and GF. The literature search strategy was developed by GD, AP and AB. Articles were located, identified, and evaluated by GD and AB. Data were extracted and checked by these same authors. The initial dimension and criteria list was composed and discussed by all the authors. Supervision: AP, JA and TP. Writing—original draft: The manuscript was drafted and edited by GD, AB y GF. with close revision and feedback from AP and TP as well as review and feedback from all other coauthors. Validation: TP and AP. Writing—review and editing: GD, AB, GF, AP, DA, JA and TP.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Anselmi, G.D., de Oliveira Barbosa, A.A., Ferrari, G. et al. Overview of systematic reviews on behavioral determinants of physical activity and healthy eating in schoolchildren. Sci Rep 15, 35379 (2025). https://doi.org/10.1038/s41598-025-19332-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-19332-9