Abstract
Women of childbearing age (WCBA) are a high-risk group for musculoskeletal (MSK) disorders and face significant challenges. A comprehensive analysis is needed to understand the impacts and develop suitable strategies. Detailed data on MSK disorders in WCBA over the past 32 years, including rheumatoid arthritis (RA), osteoarthritis (OA), low back pain (LBP), neck pain (NP), gout, and other musculoskeletal disorders (OMSKDs), were collected from the Global Burden of Disease database (GBD2021). The burden of these diseases and trends were assessed using prevalence, disability-adjusted life years (DALYs), the Socio-Demographic Index (SDI), and estimated annual percentage changes , with forecasts made up to 2050.From 1990 to 2021, among WCBA, the number of patients with MSK disorders increased from 245,428,271 to 401,422,090. The rate of increase in prevalence was the greatest in middle SDI regions, while high SDI regions bear the highest age-standardized DALYs rate. The conditions with the most significant increase in Age-Standardized Prevalence Rate are ranked as OA, gout, OMSKDs, RA, and NP, while LBP remained relatively unchanged. The ARIMA model forecasts that the number of cases will further rise, and it is estimated that approximately 500 million WCBA will be affected by MSK diseases by 2050. The contributions of obesity and renal dysfunction to the burden of MSK disorders will further increase.WCBA face a significant burden from MSK disorders, and this burden is forecast to increase further. There is an urgent need to invest more in medical resources to manage MSK conditions in WCBA. Focus on the significant increase in specific MSK disorders and controlling modifiable risk factors is crucial.
Similar content being viewed by others
Introduction
Musculoskeletal (MSK) disorders are highly prevalent and one of the most common health concerns for working-age individuals seeking healthcare services1,2. Common MSK disorders include rheumatoid arthritis (RA), osteoarthritis (OA), low back pain (LBP), neck pain (NP), and gout. These conditions impose a significant global burden, contributing 21.3% of total years lived with disability (YLDs), second only to mental and behavioral disorders3,4,5,6. Chronic musculoskeletal pain (MSP), a core clinical manifestation of MSK disorders, not only limits physical activity but also leads to functional decline, depression, and social isolation7. Severe MSP can further impair mobility and hand dexterity, resulting in premature retirement and a decline in quality of life8. Notably, the burden of MSK disorders is significantly higher in women than in men, with this gender disparity being especially pronounced in Women of childbearing age (WCBA)9.
WCBA face unique challenges due to the interaction between MSK disorders and pregnancy. Studies have shown that MSK disorders are associated with an increased risk of severe pregnancy complications, and pregnancy itself may be a trigger or exacerbate existing MSK conditions10,11,12.. More than 50% of pregnant women experience pregnancy-related lower back pain, with many reporting pain severe enough to interfere with daily activities, disrupt sleep, and lead to high absenteeism13,14,15. Furthermore, MSK disorders can be linked to adverse pregnancy outcomes16.. Women with RA may experience disease flare-ups during pregnancy, leading to complications such as preeclampsia, fetal growth restriction, and preterm birth. Disease activity should be controlled before pregnancy to minimize these risks17.
Furthermore, WCBA often find themselves at a crucial stage in their career development while simultaneously taking on caregiving responsibilities for both children and elderly family members. Chronic MSP-induced functional decline may force these women to exit the workforce prematurely, exacerbating the socio-economic burden18,19. As the global population ages, the burden of MSK disorders continues to rise. It is crucial to recognize that reproductive age is a critical period for the accumulation of health risk factors in women. Without effective prevention and intervention during this stage, the burden of MSK diseases may dramatically increase in old age20,21.
To comprehensively cover all the MSK disorder categories defined by GBD and systematically assess the overall burden of these diseases in WCBA, we have included six MSK disorders. This article presents the comprehensive analysis of the overall burden of MSK disorders in WCBA, including RA, OA, LBP, NP, gout, and other MSK disorders. This study systematically evaluates the epidemiological features of MSK disorders in WCBA, identifies common modifiable risk factors, and provides scientific evidence for policymakers to optimize healthcare resource allocation and set priorities for disease prevention.
Materials and methods
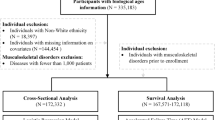
Date sources
Since 1990, the global GBD database has collected and integrated epidemiological data from 21 GBD regions and 204 countries and territories, encompassing the global burden of 371 diseases and injuries. All necessary data were downloaded from the Global Health Data Exchange (GHDx) query tool (https://vizhub.healthdata.org/gbd-results/). Our analysis focuses on the prevalence and disability-adjusted life years (DALYs) of MSK disorders in WCBA 15–49 years, including gout, LBP, NP, OA, other MSK disorders, and RA and associated risk factors. The data were categorized by age, sex, geographical region, country, and SDI from 1990 to 2021.Additionally, we identified the following MSK disorders-related risk factors based on the GBD 2021 database: gout is linked to high body-mass index and kidney dysfunction; LBP is associated with occupational ergonomic factors, high body-mass index, and smoking; OA is associated with high body-mass index; and RA is associated with smoking22.
Definition
The SDI is a composite measure used to assess the socio-economic development level of countries and regions. SDI values range from 0 (lowest development level) to 1 (highest development level). The 204 countries and territories are divided into five SDI categories: low, low-middle, middle, high-middle, and high.
In the GBD2021 database, MSK disorders are defined as a broad group of conditions that lead to both disability and, in some cases, death. These disorders include RA, OA, LBP, NP, gout, and a diverse category of other musculoskeletal conditions.
RA is a systemic autoimmune disorder that causes pain, swelling, and deformation of the joints and may be accompanied by systemic symptoms. OA is the most common form of arthritis, involving chronic inflammation, breakdown, and structural alterations of whole joints. LBP is defined as pain in the area on the posterior aspect of the body from the lower margin of the twelfth ribs to the lower gluteal folds (with or without pain referred into one or both lower limbs) that lasts for at least one day. NP is defined as neck pain (with or without pain referred into the upper limb[s]) that lasts for at least one day. The “neck” includes the area from the occiput to the first thoracic vertebra. Gout is a rheumatic disease that is characterised by deposition of monosodium urate (MSU) crystals in the synovial fluid of joints and in other tissues, causing inflammation. OMSKDs is a heterogeneous rest category comprising a wide range of disorders of muscles, bones, and ligaments that are not included in the five GBD defined musculoskeletal diseases (rheumatoid arthritis [RA], osteoarthritis [OA], low back and neck pain, and gout) Prevalence data for these conditions come from population-based health surveys and insurance claims, covering a range of conditions including systemic lupus erythematosus, infectious arthropathies, inflammatory polyarthropathies, joint disorders, systemic connective tissue disorders, deforming dorsopathies, spondylopathies, muscle disorders, synovium and tendon disorders, soft tissue disorders, bone density and structure disorders, osteomyelitis, other osteopathies, chondropathies, and other musculoskeletal and connective tissue disorders23.
Statistical analysis and data visualization
To comprehensively understand the burden of MSK disorders in WCBA (15–49 years), descriptive analyses were conducted at the global, regional, and national levels. The analysis accounted for variability by reporting 95% uncertainty intervals (UIs) or 95% confidence intervals (CIs). Statistical analysis was performed using R software (version 3.4.2), and visualizations were created using ggplot2 to describe regional and temporal trends.
EAPC measures the average annual percentage change of Age-Standardized Rate(ASR) over time, used to assess the trends of MSK disorders in this population24 The EAPC was calculated using the following formulas:
Predictive analysis
The ARIMA model is a widely used time series analysis technique that combines autoregression (AR), integration (I), and moving average (MA) components to identify trends and cyclical patterns in data, enabling the forecast of future changes based on past observations25 This model was employed to forecast future trends in the prevalence and DALYs of MSK disorders among WCBA over the next 29 years. Differencing was applied to convert the non-stationary data into stationary data, with validation using autocorrelation (ACF) and partial autocorrelation (PACF) functions. The optimal ARIMA model was selected using the auto.arima() function, based on the Akaike Information Criterion (AIC).
Results
MSK disorders in WCBA: global trends
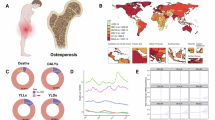
The number of WCBA with MSK disorders increased from 245,428,271 (95% UI: 222,990,429–271,339,478) in 1990 to 401,422,090 (95% UI: 366,668,084–438,622,816) in 2021, reflecting an increase of approximately 63.56%. DALYs increased from 26,623,213 (95% UI: 19,236,070–34,913,124) in 1990 to 42,404,916 (95% UI: 30,756,210–55,691,457) in 2021, a rise of about 59.27%. In 2021, the Age-Standardized Prevalence Rate (ASPR) was 18,351.67 (95% UI: 16,673.9–20,289.16). From 1990 to 2021, this rate showed an upward trend, with an Estimated Annual Percent Change (EAPC) of 0.41 (95% CI 0.38–0.43).
Among specific diseases, the most significant increase observed from 1990 to 2021 was in OA, with an EAPC of 1.39 (95% CI 1.26–1.51), followed by gout, with an EAPC of 0.98 (95% CI 0.94–1.01), OMSKDs, with an EAPC of 0.94 (95% CI 0.91–0.97), RA, with an EAPC of 0.89 (95% CI 0.87–0.92), and NP, with an EAPC of 0.22 (95% CI 0.13–0.30). There was no significant change in LBP, with an EAPC of − 0.08 (95% CI − 0.13 to − 0.03), as the 95% CI includes 0. (Table 1; Fig. 1).
MSK disorders in WCBA: age patterns
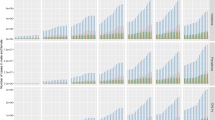
From 1990 to 2021, the ASPR for females aged 15–49 increased across all age subgroups. The most significant increases were observed in the 25–29 years age group (EAPC = 0.15; 95% CI 0.12 to 0.19), the 35–39 years age group (EAPC = 0.15; 95% CI 0.09 to 0.20), and the 45–49 years age group (EAPC = 0.15; 95% CI 0.12 to 0.17), with each demonstrating similar rates of increase.
The smallest increase was observed in the 15–19 years age group, with an EAPC of 0.06 (95% CI 0.03 to 0.08). For example, in the 25–29 years age group, the ASPR was 15,467.12 (95% UI 12,624.09 to 18,609.33) in 1990, and by 2021, it had increased to 16,002.28 (95% UI 13,116.75 to 19,071.98) (Table 1; Figs. 2A, B and 3A, B).
Global burden of MSK disorders in WCBA by age, and SDI region from 1990 to 2021 (number of cases) . (A) Trends in DALYs cases and prevalence cases by age; (B) Number of DALYs cases and prevalence cases by age in 2021; (C) Trends in DALYs cases and prevalence cases by SDI region; (D) Number of DALYs cases and prevalence cases by SDI region in 2021.
Burden of MSK disorders in WCBA by SDI
In 2021, the Middle SDI region had the highest number of WCBA(125,836,401, 95% UI 114,744,896–137,868,255). In all SDI regions, an increase in the ASPR and DALYs of MSK disorders in WCBA was observed. From 1990 to 2021, The Middle SDI region saw the largest increase in ASPR (EAPC = 0.73, 95% CI 0.7–0.75), rising from 16,528.26 (95% CI 14,987.31–18,295.28) to 20,346.5 (95% UI 18,553.12–22,291.94). In contrast, the Low SDI region saw the smallest increase(EAPC = 0.08, 95% CI 0.03–0.13), with the ASPR rising from 15,754.89 (95% CI 14,292.63–17,529.47) to 16,009.3 (95% UI 14,514.97–17,730.98).
From the perspective of ASDR, similar results to ASPR were observed. From 1990 to 2021, the Middle SDI region had the largest increase(EAPC = 0.63, 95% CI 0.6–0.65), and the ASDR rose from 1790.46 (95% CI 1293.17–2343.97) to 2135.31 (95% UI 1547.55–2807.69). In contrast, the Low SDI region saw the smallest increase(EAPC = 0.07, 95% CI 0.02–0.12), and the ASDR increased from 1681.78 (95% CI 1210.69–2202.4) to 1704.06 (95% UI 1225.35–2241.85) (Table 1; Figs. 2C, D and 3C, D).
Correlation analysis
Based on the correlation analysis between the Social Development Index (SDI) and the burden of MSK disorders across 21 global geographical regions from 1990 to 2021, our findings reveal significant heterogeneity in the impact of socioeconomic levels on disease patterns. The age-standardized disability-adjusted life years (ASDR) of diseases such as RA, OA, gout, and overall MSK disorders show a positive correlation with SDI. However, the ASDR of LBP exhibits a non-linear fluctuation, increasing with SDI until it peaks around 0.8 and then declines. For NP, the burden remains relatively stable, with the highest ASDR observed at an SDI of approximately 0.6. OMSKDs follow a “rise-decline-sharp increase” pattern of fluctuating growth (Fig. 4).
MSK disorders in WCBA: national trends
From 1990 to 2021, the United Arab Emirates saw the largest increase in the ASPR of MSK disorders among WCBA, rising from 19,321.64 (95% UI 17,237.26 to 21,607.41) to 27,448.14 (95% UI 24,651.86 to 30,845.59), with an EAPC of 1.1 (95% CI 0.93 to 1.28). It is worth noting that in 2021, the United States of America had the highest ASPR of MSK disorders, with 31,052.34 (95% UI 29,612.35 to 32,506.1).
India (8,258,973, 95% UI 5,958,290 to 10,996,164) had the highest number of DALYs, followed by China (5,666,910, 95% UI 4,088,129 to 7,501,814) and the United States of America (2,515,549, 95% UI 1,840,820 to 3,291,285). The highest ASPR were observed in Japan (3368.47, 95% UI 2415.45 to 4492.24), Chile (3367.2, 95% UI 4553.48 to 8477.80), and the United States of America (3322.43, 95% UI 2431.28 to 4346.99).
Overall, the ASPR of MSK disorders has significantly increased in economically developed countries such as the United Arab Emirates and the United States. Meanwhile, populous countries like India and China bear a tremendous burden of MSK disorders among WCBA (Table S1; Fig. 5).
MSK disorders in WCBA: regional level
In 2021, the global burden of MSK disorders among WCBA showed significant regional variation. The highest number of cases was observed in South Asia (107,679,173, 95% UI 97,890,798 to 118,997,958), followed by East Asia (58,985,879, 95% UI 53,786,991 to 65,170,978) and North Africa and the Middle East (36,788,065, 95% UI 33,255,671 to 40,856,970).
In terms of disease severity, High-income North America had the highest ASDR (3312.94, 95% UI 2423.07 to 4332.69), followed by Southern Latin America (3292.37, 95% UI 2378.29 to 4352.42) and High-income Asia Pacific (3234.27, 95% UI 2321.32 to 4297.44). The lowest DALY rates were observed in Eastern Sub-Saharan Africa (1440.85, 95% UI 1024.83 to 1907.81), Oceania (1558.21, 95% UI 1110.68 to 2071.46), and Central Sub-Saharan Africa (1558.76, 95% UI 1118.18 to 2041.79). Notably, ASPR and DALY rates were generally higher in high-income regions compared to low- and middle-income regions. For instance, High-income North America’s ASPR reached 30,950.54 (95% UI 29,403.8 to 32,396.61), approximately 2.3 times higher than Eastern Sub-Saharan Africa (13,601.8, 95% UI 12,193.17 to 15,202.79).
From 1990 to 2021, the ASPR and ASDR for MSK diseases among WCBA increased across all regions, but the rate of increase varied. The largest increase in ASPR was observed in East Asia (EAPC = 0.86, 95% CI 0.8 to 0.92), followed by Southeast Asia (0.63, 95% CI 0.61 to 0.66) and North Africa and the Middle East (0.61, 95% CI 0.57 to 0.65), while the slowest increase was seen in Central Sub-Saharan Africa (EAPC = 0.11, 95% CI 0.06 to 0.16) and Eastern Sub-Saharan Africa (EAPC = 0.11, 95% CI 0.06 to 0.16). The upward trend in ASDR mirrored this, with East Asia (EAPC = 0.64, 95% CI 0.59 to 0.70), North Africa and the Middle East (EAPC = 0.58, 95% CI 0.54 to 0.62), and Southeast Asia (EAPC = 0.55, 95% CI 0.53 to 0.58) showing the largest increases (Table 1; Fig. 6).
Risk factors of MSK disorders in WCBA
The study revealed a significant increasing trend in the age-standardized disability-adjusted life years (ASDR) for diseases related to high body mass index, with the highest annual percentage change (EAPC) observed for OA at 2.45 (95% CI 2.3–2.59), followed by gout (2.14; 95% CI 2.09–2.18) and LBP (1.82; 95% CI 1.79–1.86). The ASDR for gout associated with kidney dysfunction also showed a gradual increase of 0.47 (95% CI 0.43–0.52). In contrast, the ASDR for LBP caused by occupational ergonomic factors and smoking showed a decreasing trend, with EAPC of − 0.34 (95% CI − 0.37 to − 0.31) and − 1.39 (95% CI − 1.45 to − 1.33), respectively. The ASDR for RA caused by smoking also showed a decreasing trend, with an EAPC of − 1.02 (95% CI − 1.13 to − 0.9). This trend highlights that metabolic risks have become the core driver of MSK disease burden among WCBA, while the control of traditional modifiable risk factors, such as occupational exposure and smoking, is showing early signs of improvement (Table S2; Fig. 7).
Forecast of MSK disorders in WCBA from 2022 to 2050
Overall forecast
By 2050, the global number of women with MSK disorders is expected to exceed 505 million, showing a significant increase of approximately 105.87% compared to the 2021 baseline (around 245 million). Notably, the ASPR for MSK disorders among WCBA will continue to rise, with projections indicating that it will reach 22,692.84 per 100,000 people by 2050, representing a 9.74% increase from 2021.
Disease subtype analysis reveals that all six MSK diseases covered in the GBD study are expected to show an increase in cases. Among these, the prevalence of OA will see the most significant rise, with a projected increase of 45.53% compared to 2021, becoming the primary driver of overall disease prevalence. In terms of ASPR, OA, OMSKDs, RA, and LBP are expected to see significant increases, while the ASPR for gout and NP is forecast to remain relatively stable.
Specifically, OA will see the largest increase in ASPR, with a 25.62% rise, reaching 3062.39 people by 2050. OMSKDs will see the second-highest increase in ASPR, projected to rise by 23.78% to 9840.11 by 2050. Over the next three decades, the MSK disease landscape may undergo structural changes, with degenerative joint diseases potentially becoming a major challenge for public health systems.(Table S3, S4; Fig. 8).
Risk factor-related forecast
The ASDR for gout (kidney dysfunction/high BMI) and RA (smoking-related) is projected to remain stable. In contrast, the ASDR for smoking-related LBP is expected to decrease by 43.4%, while the ASDR for LBP due to occupational ergonomic factors is anticipated to decrease by 9.83%. Notably, metabolic risk factors are emerging as the primary drivers of increase: the ASDR for LBP associated with high BMI is expected to rise by 47.78%, from 113.35 in 2021 to 167.51 in 2050, marking the highest growth rate among all risk-disease combinations. Furthermore, the ASDR for OA associated with high BMI is projected to rise by 42.18%, from 19.00 in 2021 to 27.01 in 2050, underscoring the cumulative impact of obesity-related chronic conditions on the MSK disease burden. These findings suggest that systematic interventions targeting high BMI will be crucial in reducing the MSK disease burden over the next three decades. (Table S5; Fig. 9).
Discussion
This study, based on the Global Burden of Disease (GBD) database, provides a systematic analysis of the disease burden evolution of six MSK disorders (RA, OA, LBP, NP, gout, and OMSKDs) among WCBA from 1990 to 2021, providing a basis for developing targeted intervention strategies.
In 2021, approximately 400 million WCBA globally were affected by MSK disorders, with a ASPR of 20,597.84. From 1990 to 2021, only LBP showed a stable burden, while RA, OA, NP, gout, and OMSKDs saw significant increases. Predictive models suggest that if current trends continue, by 2050, over 500 million WCBA will be affected globally, indicating that MSK disorders will place increasing pressure on healthcare resources, posing a severe challenge to healthcare systems and requiring special focus on this high-risk group.
Geographically, South Asia and East Asia bear the heaviest MSK disorders burden among WCBA, mainly due to large populations and lifestyle/socio-cultural factors. High-income North America, especially the United States, has the highest ASPR. Correlation analysis shows a positive association between the Socio-Demographic Index (SDI) and Age-Standardized Disability Rate (ASDR), which could be related to the higher prevalence of chronic, difficult-to-treat MSK disorders (such as metabolic OA and gout) in high-SDI countries, often associated with longer disease durations. However, this association does not imply causation, and further research is needed to explore the underlying factors. We hypothesize that Modern lifestyle factors, such as increased sedentary behavior, higher consumption of ultra-processed foods, and the obesity epidemic, may further exacerbate the disease burden26,27,28. Additionally, occupational pressures on WCBA in high-income countries (e.g., high-intensity work) may contribute to higher disease prevalence29.
Notably, the Middle SDI regions have observed the most significant increase in MSK disease burden among WCBA. We believe there are several hypotheses worth attention and further confirmation: Middle SDI regions often face issues of unequal healthcare resource distribution (especially in rural and remote areas)30. At the same time, rapid industrialization and urbanization have increased occupational exposure risks (e.g., prolonged standing, repetitive physical labor)31,32 and environmental hazards (e.g., air pollution)33. From a social psychology perspective, a significant portion of WCBA in these regions often have to balance multiple roles within both family and society34. The complex social relationships, childcare responsibilities, and household labor lead to physical and mental fatigue, which may exacerbate MSK disorders through neuroendocrine mechanisms35,36,37. Research shows that the lack of household assistance is an important risk factor for recurrent LBP13 Further research is necessary to better understand these contributing factors and their interplay, ultimately helping to inform more effective public health strategies and interventions.
The burden of MSK disorders in WCBA varies across different age groups. The ASPR in the 15–19 age group increased the slowest between 1990 and 2021, indicating a relatively low burden of MSK disorders in this group. However, the ASPR in the subgroups within the 25–49 age range increased significantly faster, with a similar upward trend across different subgroups. This phenomenon may be closely related to physiological changes, lifestyle, and occupational factors37,38 For these age groups, clinical screening targeted at musculoskeletal diseases prevalent in their age range is important. Early and timely intervention through clinical screening, along with addressing occupational factors related to musculoskeletal health and improving the work environment, may help mitigate the long-term impact of these conditions on quality of life.
Biologically, women typically have smaller skeletal structures and lower muscle density, making their bones and joints more prone to degenerative changes. The association between women and certain rheumatic symptoms and diseases, such as MSP and OA, has been well established, with clear gender differences in the incidence and prevalence of these diseases39. Additionally, the cyclical hormonal fluctuations during the female menstrual cycle offer another explanation for the observed differences in MSK injuries. In a typical 28–35 day cycle, estrogen and progesterone levels fluctuate, leading to women being frequently exposed to dynamic changes in sex hormone concentrations. Given that sex hormone receptors are widely distributed across tissues in the body, including skeletal muscles and connective tissues, hormonal changes can directly affect the activity within these tissues40,41. Estrogen has a profound impact on bone strength and structure by promoting osteoblast activity42. A study of 9,811 community residents (average age 65) found an association between decreased sex hormone concentrations and increased chronic pain risk after adjusting for age and BMI43. Notably, women are more likely to suffer from chronic pain, and the severity and frequency of MSP are closely associated with negative emotions44,45.
Regarding reproductive health, WCBA face unique challenges related to MSK diseases, such as rheumatoid arthritis (RA), which can impair fertility. Compared to the general population, pregnancy outcomes in RA patients are often unsatisfactory, particularly in those with high disease activity46. Research indicates that women with RA are at a higher risk of developing gestational diabetes, likely due to the use of corticosteroids to manage disease activity during pregnancy. This can lead to reduced peripheral insulin sensitivity, increased hepatic glucose production, and suppressed pancreatic insulin secretion, contributing to the development of diabetes in RA patients47. Women with RA planning to conceive should prioritize disease activity control, and it is essential to strengthen communication between patients, obstetricians, and rheumatologists to develop individualized treatment plans for women with high disease activity preparing for pregnancy48. Furthermore, pregnancy itself may exacerbate MSK conditions. A prospective study of 325 pregnant women in the Middle East found that nearly two-thirds experienced LBP, pelvic pain, or both during their pregnancy49.
Our research shows that from 1990 to 2021, the contribution of high BMI to gout, back pain, and OA in WCBA has significantly increased. Obesity has become a global issue, with 23% of women in this age group now obese50. Global studies indicate that, across most age groups and countries, women are generally less active than men, and this gap widens with age51, further contributing to the higher prevalence of MSK disorders in women. Obesity is a stronger risk factor for female OA than for males, as it increases the load on weight-bearing joints and is associated with systemic inflammation, which may exacerbate OA52. Obesity may also cause irregular menstruation, endometrial disease, and infertility, and obese women have a higher risk of complications during pregnancy, such as hypertension, gestational diabetes, preterm birth, and cesarean sections53. As a modifiable risk factor, promoting scientific weight management is crucial. Additionally, gout related to renal dysfunction is on the rise, highlighting the need to prioritize kidney protection in clinical management. Estrogen and progesterone have protective effects on renal blood flow, glomerular filtration rate, and ion and water reabsorption, while testosterone tends to impair these functions54. Therefore, clinical practice and basic research should incorporate gender-specific considerations. Notably, the contribution of occupational ergonomics and smoking to MSK disorders has decreased, likely due to increased awareness of the harmful effects of tobacco and improvements in the work environment.
In the coming decades, the number of people worldwide suffering from MSK disorders is expected to increase significantly. Countries with large territories and populations will face greater challenges in combating MSK disorders, as developing and strengthening the implementation of control programs is more complex and costly. The burden of OA, gout, and OMSKDs among WCBA has shown a significant increase, requiring special attention. Given the rapid changes in population structure and disease burden in developing countries, it is necessary to adopt a proactive approach to alleviate this future burden. There is an urgent need for research to evaluate the most effective and affordable strategies for preventing and managing the MSK disease burden. We propose the following targeted interventions: First, control modifiable risk factors, especially obesity. We suggest launching public health campaigns and conducting early screenings to raise awareness of MSK disorder risk factors, especially the importance of controlling body mass index (BMI). Secondly, optimizing the allocation of medical resources for WCBA, emphasizing clinical screening for different age groups, and focusing on the development of primary healthcare capabilities are essential to ensure patients receive professional medical guidance. MSK disorders also significantly increase the demand for rehabilitation55. To meet rehabilitation needs, countries worldwide should allocate sufficient funds for rehabilitation services. Rehabilitation can effectively relieve pain, enhance muscle strength in MSK disorder patients, thereby improving physical activity and quality of life56. Third, increase investment in basic research on MSK disorders to explore new therapies for MSK health and focus on the development of personalized treatment plans. Fourth, pay attention to the MSK health of pregnant women. Issues such as childbirth, family planning, disease activity control, and birth outcomes should be included in preconception counseling, with special emphasis on maintaining strict disease control at every critical stage57. Fifth, establish stricter workplace safety standards for WCBA to reduce the negative impact of occupational ergonomic factors on them. Additionally, further high-quality epidemiological investigations are necessary OMSKDs encompass various MSK conditions that are not individually classified. Further collection of specific information on OMSKDs is both necessary and valuable.
Although the GBD study is comprehensive, it has several limitations that could impact the accuracy of its results. Data from various organizations and regions can differ in quality and completeness, particularly in areas with limited medical infrastructure. Misdiagnosis, missed diagnoses, and documentation loss due to inadequate medical performance in underdeveloped countries may have led to an underreporting of diseases in GBD. Additionally, certain significant MSK disorders, such as systemic lupus erythematosus and spondyloarthritis, are categorized under OMSKDs based on ICD-10 mapping. GBD uses advanced models like DisMod-MR 2.1 and spatiotemporal Gaussian process regression to estimate disease burden, but these models have inherent uncertainties and cannot fully address potential data challenges. Improving data collection and disease management in underdeveloped regions in the future will enhance the accuracy of the research.
Conclusion
The results show that from 1990 to 2021, the burden of OA, gout, and OMSKDs in WCBA has increased significantly. Projections suggest that the burden of MSK disorders in WCBA will continue to rise, with approximately 500 million WCBA expected to be affected by MSK disorders by 2050. Notably, obesity and kidney dysfunction are expected to contribute more to the disease burden and require special attention. Although progress has been made in diagnosis and treatment, reducing the global burden of MSK disorders in WCBA remains a challenge for researchers and clinicians. WCBA face unique challenges posed by MSK disorders. We recommend further high-quality epidemiological research, strengthening the allocation of primary healthcare resources, focusing on MSK disorders screening for WCBA, and actively supporting potential therapies and emerging technologies to improve healthcare outcomes.
Data availability
The data sets generated and/or analyzed during the current study are available in the GBD repository.
Abbreviations
- GBD:
-
Global Burden of Disease
- WCBA:
-
Women of childbearing age
- SDI:
-
Socio-Demographic Index
- EAPC:
-
Estimated annual percentage changes
- ASR:
-
Age-standardized rate
- ASDR:
-
Age-Standardized Disability-adjusted life years rate
- ASPR:
-
Age-Standardized Prevalence Rate
- CI:
-
Confidence interval
- UI:
-
Uncertainty intervals
- MSK:
-
Musculoskeletal
- MSP:
-
Musculoskeletal pain
- LBP:
-
Low back pain
- NP:
-
Neck pain
- RA:
-
Rheumatoid arthritis
- OA:
-
Osteoarthritis
- OMSKDs:
-
Other musculoskeletal disorders
- BMI:
-
Body mass index
- ARIMA:
-
Autoregressive integrated moving average
References
Main, C. J. & Williams, A. C. Musculoskeletal pain. BMJ (Clin. Res. ed). 325(7363), 534–537 (2002).
Burton, K. & Kendall, N. Musculoskeletal disorders. BMJ (Clin. Res. ed). 348, g1076 (2014).
Murray, C. J. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859), 2197–2223 (2012).
Hoy, D. G. et al. The global burden of musculoskeletal conditions for 2010: An overview of methods. Ann. Rheum. Dis. 73(6), 982–989 (2014).
Sànchez-Riera, L. et al. The global burden attributable to low bone mineral density. Ann. Rheum. Dis. 73(9), 1635–1645 (2014).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859), 2163–2196 (2012).
Dieppe, P. Chronic musculoskeletal pain. BMJ (Clin. Res. ed). 346, f3146 (2013).
Niederstrasser, N. G., Wainwright, E. & Stevens, M. J. Musculoskeletal pain affects the age of retirement and the risk of work cessation among older people. PLoS ONE 19(3), e0297155 (2024).
Cao, F. et al. Global, regional and national temporal trends in prevalence for musculoskeletal disorders in women of childbearing age, 1990–2019: An age-period-cohort analysis based on the Global Burden of Disease Study 2019. Ann. Rheum. Dis. 83(1), 121–132 (2024).
Salari, N. et al. The global prevalence of low back pain in pregnancy: A comprehensive systematic review and meta-analysis. BMC Pregnancy Childbirth 23(1), 830 (2023).
Hardcastle, S. A. Pregnancy and lactation associated osteoporosis. Calcif. Tissue Int. 110(5), 531–545 (2022).
Vleeming, A., Albert, H. B., Ostgaard, H. C., Sturesson, B. & Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 17(6), 794–819 (2008).
Sencan, S., Ozcan-Eksi, E. E., Cuce, I., Guzel, S. & Erdem, B. Pregnancy-related low back pain in women in Turkey: Prevalence and risk factors. Ann. Phys. Rehabil. Med. 61(1), 33–37 (2018).
Liddle, S. D. & Pennick, V. Interventions for preventing and treating low-back and pelvic pain during pregnancy. Cochrane Database Syst. Rev. 9, Cd001139 (2015).
Kalus, S. M., Kornman, L. H. & Quinlivan, J. A. Managing back pain in pregnancy using a support garment: A randomised trial. BJOG Int. J. Obstet. Gynaecol. 115(1), 68–75 (2008).
Helmick, C. G. et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthr. Rheum. 58(1), 15–25 (2008).
Castro-Gutierrez, A., Young, K. & Bermas, B. L. Pregnancy and management in women with rheumatoid arthritis, systemic lupus erythematosus, and obstetric antiphospholipid syndrome. Rheum. Dis. Clin. North Am. 48(2), 523–535 (2022).
Caruso, C. C. 2015 Reducing risks to women linked to shift work, long work hours, and related workplace sleep and fatigue issues. J. Women’s Health 24(10), 789–794 (2002).
Denmark, F., Novick, K. & Pinto, A. Women, work, and family: Mental health issues. Ann. N. Y. Acad. Sci. 789, 101–117 (1996).
Kemp, B. R. et al. Do early-life social, behavioral, and health exposures increase later-life arthritis incidence?. Res. Aging 44(7–8), 479–493 (2022).
Global age-sex-specific fertility. Mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1160–1203 (2020).
Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440) 2162–203 (2024).
Global, regional, and national burden of other musculoskeletal disorders, 1990–2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021 Lancet Rheumatol. 5(11) e670-e82 (2023)
Cen, J. et al. Global, regional, and national burden and trends of migraine among women of childbearing age from 1990 to 2021: Insights from the Global Burden of Disease Study 2021. J. Headache Pain 25(1), 96 (2024).
Foreman, K. J. et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet 392(10159), 2052–2090 (2018).
Wadden, T. A., Brownell, K. D. & Foster, G. D. Obesity: Responding to the global epidemic. J. Consult. Clin. Psychol. 70(3), 510–525 (2002).
Baker, P. & Friel, S. Food systems transformations, ultra-processed food markets and the nutrition transition in Asia. Glob. Health 12(1), 80 (2016).
Boutari, C. & Mantzoros, C. S. A 2022 update on the epidemiology of obesity and a call to action: As its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metab. Clin. Exp. 133, 155217 (2022).
Prince, S. A. et al. Intrapersonal, social and physical environmental determinants of moderate-to-vigorous physical activity in working-age women: A systematic review protocol. Syst. Rev. 3, 132 (2014).
Yu, Q. et al. Trend and equity of general practitioners’ allocation in China based on the data from 2012–2017. Hum. Resour. Health 19(1), 20 (2021).
Mousavi, S. J. et al. Low back pain in Iran: A growing need to adapt and implement evidence-based practice in developing countries. Spine 36(10), E638–E646 (2011).
Nagasu, M. et al. Prevalence and risk factors for low back pain among professional cooks working in school lunch services. BMC Public Health 7, 171 (2007).
Bade, K. J., Mueller, K. T. & Sparks, J. A. Air pollution and rheumatoid arthritis risk and progression: Implications for the mucosal origins hypothesis and climate change for RA pathogenesis. Curr. Rheumatol. Rep. 26(10), 343–353 (2024).
Damaske, S. & Frech, A. Women’s work pathways across the life course. Demography 53(2), 365–391 (2016).
Yip, Y. B., Ho, S. C. & Chan, S. G. Socio-psychological stressors as risk factors for low back pain in Chinese middle-aged women. J. Adv. Nurs. 36(3), 409–416 (2001).
Virgara, R., Maher, C. & Van Kessel, G. The comorbidity of low back pelvic pain and risk of depression and anxiety in pregnancy in primiparous women. BMC Pregnancy Childbirth 18(1), 288 (2018).
Strazdins, L. & Bammer, G. Women, work and musculoskeletal health. Soc. Sci. Med. (1982) 58(6), 997–1005 (2004).
Li, X., Sundquist, J. & Sundquist, K. Socioeconomic and occupational risk factors for rheumatoid arthritis: A nationwide study based on hospitalizations in Sweden. J. Rheumatol. 35(6), 986–991 (2008).
Long, H. et al. Prevalence trends of site-specific osteoarthritis from 1990 to 2019: Findings from the Global Burden of Disease Study 2019. Arthritis Rheumatol. 74(7), 1172–1183 (2022).
Hewett, T. E., Zazulak, B. T. & Myer, G. D. Effects of the menstrual cycle on anterior cruciate ligament injury risk: A systematic review. Am. J. Sports Med. 35(4), 659–668 (2007).
Hamlet, W. P., Liu, S. H., Panossian, V. & Finerman, G. A. Primary immunolocalization of androgen target cells in the human anterior cruciate ligament. J. orthop. Res. Off. Publ. Orthop. Res. Soc. 15(5), 657–663 (1997).
Cawthon, P. M. Gender differences in osteoporosis and fractures. Clin. Orthop. Relat. Res. 469(7), 1900–1905 (2011).
de Kruijf, M. et al. Lower sex hormone levels are associated with more chronic musculoskeletal pain in community-dwelling elderly women. Pain 157(7), 1425–1431 (2016).
Pang, H. et al. Low back pain and osteoarthritis pain: A perspective of estrogen. Bone res. 11(1), 42 (2023).
Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the Global Burden of Disease 2019 Study. BMJ (Clin. res, ed) 376 e068208 (2022).
de Jong, P. H. & Dolhain, R. J. Fertility, pregnancy, and lactation in rheumatoid arthritis. Rheum. Dis. Clin. North Am. 43(2), 227–237 (2017).
Imatoh, T. et al. Development of a novel algorithm for detecting glucocorticoid-induced diabetes mellitus using a medical information database. J. Clin. Pharm. Ther. 42(2), 215–220 (2017).
Kocarnik, J. M. et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 8(3), 420–444 (2022).
Blümel, J. E. et al. Menopause could be involved in the pathogenesis of muscle and joint aches in mid-aged women. Maturitas 75(1), 94–100 (2013).
Broughton, D. E. & Moley, K. H. Obesity and female infertility: Potential mediators of obesity’s impact. Fertil. Steril. 107(4), 840–847 (2017).
Smolen, J. S., Aletaha, D. & McInnes, I. B. Rheumatoid arthritis. Lancet 388(10055), 2023–2038 (2016).
Nicolella, D. P. et al. Mechanical contributors to sex differences in idiopathic knee osteoarthritis. Biol. Sex Differ. 3(1), 28 (2012).
Knight, M., Kurinczuk, J. J., Spark, P. & Brocklehurst, P. Extreme obesity in pregnancy in the United Kingdom. Obstet. Gynecol. 115(5), 989–997 (2010).
Harvey, B. J. & Alvarez de la Rosa, D. Sex differences in kidney health and disease. Nephron 149(2), 77–103 (2025).
Cieza, A. et al. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10267), 2006–2017 (2021).
Chen, N., Fong, D. Y. T. & Wong, J. Y. H. Secular trends in musculoskeletal rehabilitation needs in 191 countries and territories from 1990 to 2019. JAMA Netw. Open 5(1), e2144198 (2022).
Littlejohn, E. A. Pregnancy and rheumatoid arthritis. Best Pract. Res. Clin. Obstet. Gynaecol. 64, 52–58 (2020).
Acknowledgements
We sincerely thank the collaborators of the Global Burden of Disease Study 2021 for their outstanding work.
Funding
This research was funded by the National Natural Science Foundation of China (No.82272568); the Sanming Project of Medicine in Shenzhen (No.SZSM202211019).
Author information
Authors and Affiliations
Contributions
The conception and design: XTZ, LKD and JBL; analysis and interpretation of the data: LKD,HCD,LL,JZL,WBX; the drafting of the paper: HCD and SL; revising it critically for intellectual content: LKD,XTZ and ZCT; and the final approval of the version to be published: all authors; and that all authors agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Given that the study is based on de-identified and publicly accessible epidemiological datasets, the Institutional Review Board at the University of Washington has approved the waiver of informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Du, H., Li, S., Tian, Z. et al. Global burden of six musculoskeletal disorders in women of childbearing age from 1990 to 2021. Sci Rep 15, 35423 (2025). https://doi.org/10.1038/s41598-025-19382-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-19382-z