Abstract
Understanding root canal morphology is essential for successful endodontic treatment. This study aimed to investigate morphological variations in root and canal systems of anterior and premolar teeth across different age groups and genders in a Saudi Arabian subpopulation using a novel classification system. A total of 3573 maxillary and mandibular anterior and premolar teeth in 209 patients were examined using cone-beam computed tomography (CBCT) in a Saudi subpopulation. The number of roots was identified, and root canal configurations were classified according to Ahmed et al. coding system (Int Endod J 50(8):761–770, 2017). Demographic data including gender (male and female) and age (divided into 6 groups—10–20, > 20–30, > 30–40, > 40–50, > 50–60, > 60–70) were recorded. The Chi-square test was used for statistical analysis, and the significance level was set at 0.05 (P = 0.05). Results showed that maxillary and mandibular central incisors, lateral incisors, and canines predominantly exhibited the 1TN1 configuration. Maxillary first premolars had a higher prevalence of double-rooted variants with code 2TN B1 P1. Maxillary second premolars more frequently displayed the 1TN1–2−1 configuration. No significant gender and age differences were observed in maxillary anterior and premolar teeth (p > 0.05). A number of supplemental configurations such as 2TNB1–2P1, 3TN MB1 DB1 P1, and 3TN 1(MB1 DB1) P1 were noted in maxillary premolars. For mandibular anteriors, results showed no significant difference by gender, but for age, mandibular incisors showed more prevalence of complex canal configurations up to 40 years. However, the difference with other age groups (> 40–70 years) was not statistically significant (p < 0.05). For mandibular premolars, the code 1TN1 was observed in more than 90% of the teeth with no significant differences in gender and age groups (p > 0.05). Several supplemental configurations such as 1TN1–2−3, 1TN1–2−3−2, 2TN B1/L1, and 2TN 1B1/L1) were noted in mandibular first premolars. This study identified a wide range of root and canal anatomical variations in anterior and premolar teeth within a Saudi subpopulation. The findings revealed that while age influenced the complexity of root canal systems in mandibular incisors, no significant association between gender and canal complexity was observed. The Ahmed et al. classification system offered a detailed analysis of these complex variations, providing a clear understanding of the root canal morphology in this population.
Similar content being viewed by others
Introduction
Understanding the intricate morphology of the root canal systems is vital for the success of endodontic treatment1,2. The root canal anatomy is complex, and can provide a protected environment for microbial flora, posing a challenge for clinicians aiming to thoroughly clean, shape, and fill the root canals3. Effective endodontic treatment relies on the clinician’s knowledge of these anatomical variations. Failure to adequately navigate the complex root canal system can lead to treatment failures and persistent infections4,5. The factors influencing root canal morphology include age, gender, and ethnicity, necessitating studies focused on specific populations to improve clinical practice and treatment outcomes6.
Root canal morphology varies significantly among different populations7,8,9. In general, maxillary and mandibular anterior teeth are characterized by single roots that often contain one or two canals10,11. However, deviations from this norm are not uncommon and can be influenced by genetic, developmental, and environmental factors12,13. For example, Iqbal et al.14 demonstrated significant anatomical variations in the mandibular anterior teeth among Saudi individuals, highlighting the importance of region-specific data. Similarly, variability has been observed in the root and canal anatomy of maxillary premolars, where the number of roots and types of canal configurations can differ markedly based on geographic and demographic factors15,16,17,18,19,20. Moreover, in mandibular premolars, although they are typically single-rooted, studies have reported complex configurations, particularly in the first premolars, which can complicate clinical procedures21,22,23.
Historically, the classification of root canal systems has been guided by the Vertucci classification system, which, while comprehensive, has limitations in describing the full spectrum of anatomical variations, particularly in maxillary premolars and anterior teeth9,24,25. The Ahmed et al.24 classification system offers several advantages over Vertucci system, particularly in its clinical relevance and applicability. Unlike the Vertucci system, which primarily focuses on root canal configuration patterns, the Ahmed et al. system provides a more comprehensive framework by incorporating multiple variables such as tooth number, root and canal configurations. This approach allows for a detailed assessment of complex anatomical variations, which are often encountered in clinical practice24. By offering greater precision and adaptability, the Ahmed et al. classification system enhances the accuracy of diagnosis, treatment planning, and outcomes in endodontics, making it a valuable tool for addressing the challenges posed by diverse and intricate root canal morphologies.
The advent of cone beam computed tomography (CBCT) has revolutionized the field of endodontics by providing high-resolution, three-dimensional images that allow for detailed visualization of root and canal anatomy26. CBCT enables clinicians to assess the number of roots and the complexity of canal systems more accurately than traditional two-dimensional radiography27. Furthermore, this imaging modality offers multiplanar views, including sagittal, coronal, and axial sections, which are crucial for identifying variations in canal morphology and planning effective treatments28. Additionally, the lower radiation exposure of CBCT compared to conventional CT scans makes it a safer option for patients while providing the detailed anatomical insights necessary for high-quality care29.
Root canal morphology varies significantly across populations due to genetic, ethnic, and environmental factors, which underscores the need for population-specific investigations. The Saudi population, with its unique genetic and demographic characteristics, provides an opportunity to uncover regional variations that may not be apparent in studies conducted on other populations. Such data are particularly relevant for endodontic practices, where accurate knowledge of root and canal anatomy is critical for successful treatment outcomes. However, despite the clear advantages of using CBCT for evaluating dental anatomy, there is limited data on the root and canal morphology specific to the Saudi population, particularly using the comprehensive Ahmed et al. classification system24. This study aimed to fill this gap by employing CBCT to investigate the morphological variations in root and canal morphology of permanent anterior and premolar teeth in a Saudi subpopulation.
Materials and methods
Ethical approval and study samples
This study was conducted according to the guidelines of the Declaration of Helsinki and the current study obtained independent approval from the Institutional Review Board of Prince Sattam bin Abdulaziz University, Al-Kharj, with the reference number PSAU2020024. The CBCT images were sourced from the College of Dentistry, Prince Sattam Bin Abdulaziz University, Al Kharj, Saudi Arabia. These images were initially captured for various purposes unrelated to this study, such as for assessing traumatic injuries and conducting surgical procedures. The informed consent was obtained from all subjects and/or their legal guardian(s).
Sample size calculation
The sample size calculation was performed using the Raosoft sample size calculator, considering a population of 373,177 from Alkharj city30, with a standard error of 6% and a confidence level of 90%. The initial calculated sample size was 182. After incorporating a 20% dropout rate, the final calculated sample size was determined to be 209. The chosen method ensured sufficient representation to identify meaningful differences in root canal morphology within the Saudi Arabian subpopulation.
Inclusion and exclusion criteria of CBCT images
In this study, CBCT images were included based on the following criteria: only permanent maxillary and mandibular anterior and premolar teeth with fully developed roots were included. Teeth were required to be either sound or exhibit small carious lesions or restorations that did not compromise root structure. CBCT images with artefacts, teeth with resorption defects, fractures, or a history of root canal treatment were excluded. The rationale for these criteria was to ensure a clear and accurate evaluation of root and canal morphology without confounding factors that might obscure anatomical structures. This approach aimed to include teeth representative of the general Saudi subpopulation while minimizing potential variability caused by pathological or treatment-induced changes. Furthermore, the age range of participants was unrestricted to capture a diverse demographic representative of the Saudi population. However, the potential limitations in representativeness due to the sample’s distribution across age and gender groups were acknowledged, as this could influence the generalizability of findings.
CBCT specifications
CBCT data were acquired using a KODAK Carestream 9300–3D machine which provides high-resolution imaging essential for detailed analysis of dental structures. The standardized field of view (FOV) of 15 × 15 cm3 provided comprehensive imaging of both the maxillary and mandibular arches while maintaining high-resolution detail for anterior and premolar teeth. This FOV size allowed to adequately capture the anatomical structures of interest, ensuring precise assessment of root and canal morphology. The voxel size of 160 μm ensured high-resolution imaging suitable for detailed analysis of root and canal morphology. A tube voltage of 82 kVp and tube current of 6 mA ensured adequate image contrast and clarity. The exposure time of 3 seconds provided a balance between image quality and patient safety by limiting radiation exposure. Analysis of the CBCT images was performed using 3S 3D imaging software (V3, Carestream Health Inc, USA) version 5.1. Image processing tools were utilized to adjust contrast and brightness for optimal visualization.
Methods for interpretation
Root and canal morphology of the maxillary and mandibular anterior and premolar teeth were classified according to Ahmed et al.24 coding system. The images were evaluated in three planes (coronal, sagittal, and axial) by two observers. Disagreements in interpretation were resolved through discussion until a consensus was reached.
Subgroup analysis
The CBCT images were categorized based on gender (male, female) and age groups (10–20, > 20–30, > 30–40, > 40–50, > 50–60, > 60). Additionally, the images were stratified by tooth type, including maxillary central and lateral incisors, maxillary canines, maxillary first and second premolars, mandibular central and lateral incisors, mandibular canines, and mandibular first and second premolars.
Assessment parameters
The anatomy of teeth was assessed based on parameters as follows:
-
A single-rooted tooth The tooth had a clear single root (a bifid root apex tip was considered as single-rooted).
-
A double-rooted tooth The tooth had bifurcated roots (regardless of partial or complete root separation).
-
A three-rooted tooth The tooth had three roots (regardless of partial or complete separation). Fusion of roots along the entire root length or partial fusion with shared canals was also considered in classification, following the criteria established by Ahmed and Dummer31.
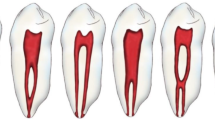
Examples for root canal configuration codes are shown below as follows:
Single-rooted configurations
-
1.
1TN1 (Refers to a single-rooted tooth with one canal configuration).
-
2.
1TN1–2-1 (A single-rooted tooth with one canal initially (1), bifurcating into two canals (2), and merging into one canal (1) before exiting at a single foramen).
-
3.
1TN1–2 (A single-rooted tooth with one canal initially (1), that bifurcates into two independent canals (2) and exits as two separate foramina).
-
4.
1TN1–2-3 (A single-rooted tooth with one canal initially (1), bifurcating into two canals (2), and terminating in three canals with three separate foramina (3)).
-
5.
1TN1–2-3−2 (A single-rooted tooth with one canal initially (1), bifurcating into two canals (2), terminating in three canals (3), and exiting through two foramina (2)).
Double-rooted configurations
-
1.
2TN B1 P1 (A double-rooted tooth where the buccal (B) and palatal (P) roots each contain one canal configuration).
-
2.
2TN B1 L1 (A double-rooted tooth with a buccal (B) root and lingual (L) root, each having one canal configuration).
-
3.
2TN B1–2 P1 (A double-rooted tooth where the buccal (B) root starts with one canal (1), bifurcates into two canals (2), and the palatal (P) root remains with one canal (1)).
-
4.
2TN 1B1 L1 (A double-rooted tooth where the buccal (B) root has one canal (1), and the lingual (L) root also has one canal (1) with a common canal coronally to both roots).
-
5.
2TN 1M1 D1–2-1 (A double-rooted tooth where the mesial (M) root has one canal (1), and the distal (D) root begins with one canal (1), bifurcates into two canals (2), and terminates as one canal (1, with a common canal coronally to both roots).
-
6.
2TN M1 D1 (A double-rooted tooth where the mesial (M) and distal (D) roots each one canal configuration).
Multi-rooted configurations
-
1.
3TN MB1 DB1 P1 (A three-rooted tooth with mesiobuccal (MB), distobuccal (DB), and palatal (P) roots, each having one canal configuration).
-
2.
3TN 1(MB1 DB1) P1 (A three-rooted tooth with the mesiobuccal (MB) and distobuccal (DB) roots having a common canal coronally (superscript before the root name) and each root has one canal, and the palatal (P) root having one canal (1)).
Calibration
To ensure consistent and accurate interpretation of CBCT images, observers underwent a detailed training and calibration protocol. This process was conducted in collaboration with an expert endodontist who provided guidance and validated the training outcomes. The training involved a structured session using a pilot sample of 50 CBCT images, which were specifically chosen to represent a range of root and canal morphologies, including variations in root number, and canal configuration (e.g., single, multiple, or complex canals). Observers were trained to analyse CBCT images systematically in three planes—axial, sagittal, and coronal—using specific criteria based on the Ahmed et al. classification system. During this phase, image contrast, brightness, and magnification tools were employed to ensure optimal visualization. Observers documented their findings independently, focusing on key variables such as root number and canal configuration, presence of fusion, and any deviations from typical anatomical patterns.
Disagreements in interpretation were resolved through a consensus protocol, which involved a detailed review of the images by both observers and the expert endodontist. This discussion was guided by predefined criteria for root and canal morphology, ensuring that decisions were consistent with the classification system used. To quantify interobserver reliability, the Intraclass Correlation Coefficient (ICC) was calculated based on the findings of the 50 pilot images. The ICC value of 0.85 indicated excellent agreement between observers, reflecting the reliability of their assessments. This robust calibration process ensured uniformity in image interpretation, enhancing the reproducibility and validity of the study’s findings.
Statistical analysis
Statistical analysis was performed using SPSS version 24 (IBM SPSS Statistics, Armonk, NY, USA). Descriptive statistics, including frequency and standard percentage, were calculated. A chi-square test was employed for data analysis, with a significance level set at 0.05 (p = 0.05).
Results
A total of 3573 maxillary and mandibular anterior and premolar teeth in 209 patients were examined using CBCT in a Saudi subpopulation of the Alkharj area, with a mean age group of 25–30 years. The number of roots was identified, and root canal configurations were classified according to Ahmed et al. classification systems.
Table 1 provides descriptive statistics for the study sample. The age distribution ranged from 10 to 70 years, with the majority falling between 30 and 40 years (43.8%). Male participants comprised 66.7% of the sample, while females accounted for 33.3%. The most prevalent root canal configuration across all tooth types was 1TN1, observed in 80.80% of the total sample.
Maxillary anterior teeth
Table 2 presents the distribution of root and canal anatomy in males and females in maxillary anterior teeth. The most common root canal configuration observed in both males and females across all tooth types was 1TN1. There were no significant differences in root canal configurations between males and females for any of the maxillary anterior tooth types (p > 0.05). Table 3 shows the distribution of root and canal morphology in maxillary anterior teeth based on age groups showing that the 1TN1 configuration is predominantly observed across all age groups for maxillary central incisors, lateral incisors, and canines. For maxillary central incisors, the 1TN1 configuration was present in 100% of teeth across all age groups with no other configurations noted. Maxillary lateral incisors exhibited the 1TN1 configuration in 100% of teeth for most age groups and 88.88% in the 40–50 age group, where one instance of the code 2TN B1 P1 configuration was noted. Maxillary canines showed the 1TN1 configuration in nearly all age groups, with minimal occurrences of the 1TN1–2−1 and 1TN1–2 configurations (p = 0.620). Overall, the 1TN1 configuration is highly prevalent across age groups with minor and statistically non-significant variations (Fig. 1).
Maxillary premolars
Table 4 presents the distribution of root and canal morphology in maxillary premolars by gender. Both males and females showed a predominant occurrence of the 2TN B1 P1 configuration in maxillary first premolars (80% and 78%, respectively) and the 1TN1 configuration in maxillary second premolars (12.56% and 11.53%, respectively). Additional configurations such as 1TN1–2−1, and 1TN1–2 were observed across both genders, along with other configurations such as 2TN B1–2 P1, 3TN MB1 DB1 P1, and 3TN 1(MB1 DB1) P1 (Figs. 2 and 3). While variations in root canal configurations were observed between males and females, they were not statistically significant for maxillary premolars (p > 0.05). Table 5 illustrates the root and canal morphology in different age groups in maxillary premolars. The 2TN B1 P1 (79.30%) and 1TN1 (47.19%) configurations predominated across all age groups, with varying proportions in maxillary first and second premolars, respectively. Additionally, supplemental configurations such as 1TN1–2−1, 1TN1–2, 2TNB1–2P1, 3TN MB1 DB1 P1, and 3TN 1(MB1 DB1) P1 were noted (Fig. 4). However, no significant differences were noted in the distribution of root canal configurations among different age groups for maxillary premolars (p > 0.05).
Root canal anatomy of three-rooted maxillary premolars and double-rooted maxillary premolars. (a,b) Three-rooted maxillary premolars with a common canal coronal to the MB and DB root canals. The bifurcation is in the middle third. (c) There is no common canal since the bifurcation is in the coronal third. (d) Double-rooted maxillary second premolar and a canal configuration 1–2 in the buccal root.
Mandibular anteriors
Table 6 shows the distribution of root and canal morphology in mandibular anterior teeth by gender. The 1TN1 configuration was predominant in both males and females for mandibular central incisors (75.68% males, 75.0% females) and lateral incisors (76.35% males, 83.20% females). The 1TN1–2−1 configuration was also noted, which is more common in the age groups up to > 30–40 years compared to > 40–70 years, however, there was no significant differences in central incisors and lateral incisors between genders (p < 0.05). In mandibular canines, the 1TN1 configuration was highly prevalent (96.53% males, 96.94% females) with minimal occurrences of other configurations and significant gender differences (p = 0.035*). Additionally, supplemental configurations in maxillary central and lateral incisors such as 1TN1–2−1 and 1TN1–2 were noted, and 2TN B1 L1 and 2TN 1B1 L1 were observed in mandibular canines (Figs. 5 and 6).
CBCT images showing double rooted mandibular canines without (a, b) and with (c,d) a common canal. The common canal is identified in teeth with canal bifurcations in double-rooted canines located in the middle and apical thirds of the root. Double-rooted canines with coronal canal bifurcations (located in the coronal third of the root) do not have a common canal.
Table 7 depicts the distribution of root and canal morphology in mandibular anterior teeth across different age groups. No significant differences were observed in the distribution of root canal configurations among age groups for mandibular central and lateral incisors (> 0.05), except mandibular canines (p < 0.05). The 1TN1 configuration predominated across all age groups for these teeth, with varying proportions. Additionally, the 1TN1–2−1, 2TN B1 L1, and 2TN 1B1 L1 configurations were noted.
Mandibular premolars
Table 8 presents the distribution of root and canal anatomy in mandibular premolars based on gender. In mandibular first premolars, the 1TN1 configuration was highly prevalent in both males (90.08%) and females (92.85%), with minimal occurrences of supplemental configurations such as 1TN1–2−1 and 1TN1–2. Similarly, in mandibular second premolars, the 1TN1 configuration was predominant in both males (95.75%) and females (94.50%), with additional configurations like 1TN1–2−1, and 1TN1–2, present in very low frequencies. Additional configurations such as 1TN1–2−3−2, 2TN B1 L1, 2TN 1B1 L1, 2TN 1M1/D1–2−1, and 2TN M1/D1 were observed across both genders, with no statistically significant differences found in the distribution of root canal configurations between males and females for mandibular premolars (p > 0.05).
Table 9 details the distribution of root and canal morphology in mandibular premolars across different age groups. In mandibular first premolars, the 1TN1 configuration was the most prevalent across all age groups, notably 40.9% in the 30–40 age group, with supplemental configurations like 1TN1–2−1 and 1TN1–2 appearing less frequently. Similarly, in mandibular second premolars, the 1TN1 configuration dominated across all age groups, particularly 43.6% in the 30–40 age group, with other configurations such as 1TN1–2 and 2TN B1/L1 present in low numbers. However, no statistically significant differences were found in the distribution of root canal configurations among different age groups for both mandibular first and second premolars (p > 0.05). Additional configurations such as 1TN1–2−3−2, 2TN B1 L1, 2TN 1B1 L1, 2TN 1M/1D1–2−1, and 2TN M1/D1 were observed across all age groups (Figs. 7, 8 and 9).
CBCT images showing root and canal anatomy in mandibular premolars. (a) Single-rooted mandibular first premolars with code 1TN1. (b) Single-rooted mandibular first premolars with code 1TN1–2−1. (c) Single-rooted mandibular first premolars with code 1TN1–2. (d) Single-rooted mandibular second premolars with code 1TN1. (e) Single-rooted mandibular second premolars with code 1TN1–2−1.
Discussion
A comprehensive understanding of root anatomy and canal morphology serves as a cornerstone for achieving successful root canal treatment outcomes32. Variability in root canal morphology across different population groups underscores the importance of conducting thorough investigations to elucidate regional differences. The CBCT has emerged as a valuable tool for precisely delineating intricate root canal systems, providing detailed three-dimensional images that facilitate comprehensive assessments9.
Assessing root canal morphology using CBCT has several advantages. Three-dimensional scans enable accurate root canal system visualization, which can uncover subtle anatomical changes that two-dimensional imaging misses33. This thorough picture helps identify multiple canals, unique root forms, and accessory canals, which are essential for endodontic treatment planning. CBCT imaging can also detect root canal proximity to essential anatomical structures, preventing procedure challenges34. However, CBCT has limitations. Though relatively low, the greater radiation dose compared to standard radiography requires careful consideration, especially in younger patients and repeated exposures35. CBCT imaging is expensive and not often available in clinical settings36. Image abnormalities from patient mobility or metal restorations can also affect CBCT scan quality and interpretation37. CBCT provides comprehensive and accurate diagnostic information, which typically outweighs its shortcomings, especially in complicated cases38.
The classification method employed in this study, as proposed by Ahmed et al.24, offers a detailed and nuanced approach to describing root and canal morphology. This system provides greater specificity compared to traditional classifications. For example, Ahmed’s system differentiates between single- and double-rooted teeth with more precision and accounts for various canal configurations, including those with multiple roots and complex canal systems24. This level of detail is particularly valuable in clinical practice, as it aids in the accurate diagnosis and treatment planning of complex cases.
The findings of this study revealed a predominantly single-rooted morphology in maxillary incisors and canine teeth, consistent with observations reported in various global populations such as Brazilian11, Turkish39, and Indian40 cohorts. These consistencies underscore the universality of single-rooted maxillary incisors and canines across diverse ethnic groups. However, it is noteworthy that isolated instances of double-rooted maxillary anterior teeth have been documented in the literature (as observed in this study in a maxillary lateral incisor), aligning with the singular occurrence identified in this study. Such anomalies, although rare, have been documented in previous case reports41 suggesting the occasional presence of atypical root configurations in maxillary incisors and canines, which is similar to the tooth identified in this study. This study demonstrates a prevalent occurrence of code 1TN1, representing a single root canal configuration, predominantly observed across the root canals of maxillary anterior teeth. This finding resonates with similar patterns identified in earlier research9,12,39. However, the investigation reveals intriguing variations in the root canal morphology of mandibular incisors compared to their maxillary counterparts.
The role of gender in shaping the diversity of root canal anatomy remains a subject of debate, with studies presenting conflicting findings. For instance, research conducted on the Chinese population highlighted notable gender-based disparities in root canal anatomy42. This suggests a potential gender-related influence on root canal morphology, albeit with relatively modest variations observed between male and female subjects. Conversely, findings from another study conducted among Turkish individuals did not reveal any significant gender-based differences in root canal anatomy43. These results closely parallel the observations made in the present study, indicating a consistent pattern across diverse populations. Thus, while some investigations suggest a potential gender-related influence on root canal morphology, others indicate a lack of significant gender-based disparities, underscoring the need for further research to elucidate this complex relationship44,45. The study findings show that the most common root canal configuration of maxillary anterior teeth in both males and females was 1TN1, with no significant differences between genders. This finding aligns with other studies, such as those by Hasanreisoglu et al.46 and Mashyakhy et al.47, which also identified 1TN1 as the predominant configuration in maxillary anterior teeth, suggesting consistency in root canal anatomy irrespective of gender. The absence of significant gender differences in root canal configurations across maxillary anterior tooth types (p > 0.05) supports the notion that anatomical variations are more likely influenced by age and individual biological factors rather than gender48.
The present study findings demonstrate non-significant differences in the distribution of root canal configurations across various age groups. Similar findings were observed in a study by Albannay49. Predominantly, the 1TN1 configuration was observed for maxillary central and lateral incisors, and canines aligning with previous studies14,50,51,52. This suggests that the 1TN1 configuration may represent a stable and common anatomical feature across different populations and age groups, despite morphological age changes in the shape and size of the canal space.
This study revealed that approximately 80% of maxillary first premolars exhibited two roots. Interestingly, similar findings have been reported in studies conducted on Turkish16 and German populations19, where approximately two-thirds of maxillary first premolars were found to be double-rooted. In contrast, a higher prevalence of single-rooted morphology in maxillary first premolars was observed in studies involving Chinese53 and Brazilian54 populations. These discrepancies in results among studies could be attributed to variations in population demographics and sample sizes. Regarding maxillary second premolars, approximately 87% of the samples in this study exhibited a single root, consistent with findings from previous studies18,55,56,57 reporting more than 80% prevalence of single-rooted maxillary second premolars. Additionally, the occurrence of three roots 3TN MB1 DB1 P1 and 3TN 1(MB1 DB1) P1 (1.37%) in maxillary first premolars was rare in this investigation, aligning with findings from another study58. However, higher percentages of three-rooted maxillary first premolars have been reported in other studies17,19. Similarly, the scarcity of three-rooted maxillary second premolars observed in this study is consistent with findings from previous investigations16,59.
The findings from this study indicate that 2TN B1 P1 canal configuration was the most prevalent in maxillary first premolars, which is consistent with numerous previous studies18,19,20,25. Similarly, the predominance of a single canal configuration was observed in maxillary second premolars, aligning with findings reported in other studies15,18,20,56. Interestingly, when classified according to Ahmed et al., the 2TN B1 P1 code emerged as the most common for maxillary first premolars, while codes 1TN1 and 1TN1–2−1 were predominant for maxillary second premolars. This classification offers a more precise representation of root and canal morphology compared to Vertucci’s system, particularly in distinguishing between single- and double-rooted teeth. Moreover, it addresses the limitation in Vertucci’s classification by differentiating between single- and double-rooted teeth with a type IV canal configuration. Additionally, while Vertucci’s classification lumps all three-canalled maxillary premolars into type VIII without considering the number of roots, our study describes the three-canalled morphology in various presentations involving both double and three roots. This nuanced approach provides a clearer understanding of the root and canal anatomy variations in maxillary premolars.
This study examined the distribution of root and canal morphology in mandibular anterior teeth by gender. The 1TN1 configuration was the predominant pattern for both mandibular central and lateral incisors in males (75.68% and 76.35%) and females (75.0% and 83.20%), respectively with previous studies10,60,61. Specifically, males exhibited a higher prevalence of the 1TN1 configuration compared to females, accompanied by lower proportions of supplemental configurations. These observations align with previous studies that have reported gender-based disparities in root canal anatomy, particularly in mandibular incisors62,63. However, similar to our findings, no significant differences were found in the mandibular central incisor and lateral incisors, suggesting a comparable distribution of root canal configurations between genders. This lack of gender-based variation in mandibular incisors and lateral incisors is consistent with some previous studies47,64, while other studies have reported conflicting results65,66. The discrepancies among studies may stem from differences in sample size, demographic characteristics of the study populations, and methodological variations in assessing root canal morphology. This suggests a nuanced landscape of root canal configurations in mandibular incisors, potentially influenced by anatomical intricacies and regional differences. Results showed that the most prevalent root canal morphology observed in mandibular canines was 1TN1, aligning with observations reported in earlier literature13,60,67,68. These findings collectively shed light on the variations of root canal morphology across different tooth types, underscoring the importance of detailed anatomical assessments for effective endodontic treatment strategies. Minimal occurrences of supplemental configurations (e.g., 2TN B1 L1 and 2TN 1B1 L1) were noted with seven samples (1.79%) demonstrating the presence of two roots. This finding contrasts with the lower prevalence rates reported in studies conducted in Iran60 and Malaysia9 but aligns more closely with findings from a study in China69. Such discrepancies underscore the inherent variability in root anatomy even within specific tooth types across different geographic regions, highlighting the need for region-specific investigations to discern population-specific trends accurately.
The current study findings showed no significant differences in mandibular anteriors among different age groups. The 1TN1 configuration was predominant across all age groups, consistent with prior studies70,71, which also identified 1TN1 as the most common canal morphology in mandibular anterior teeth. The observed variations in root canal configurations of mandibular anteriors among different age groups could be attributed to several factors, including developmental changes and physiological adaptations of the teeth over time1. Younger age groups may exhibit simpler canal systems, while older individuals could present with more complex morphologies due to secondary dentine deposition and other age-related changes72, which has been observed in the current study in which the age groups between 10 and 40 years showed more complex canal configurations compared to those above 40 years.
The findings from this study reveal that the 1TN1 configuration is the predominant root and canal anatomy in mandibular premolars for both genders. In mandibular first premolars, 90.08% of males and 92.85% of females exhibited the 1TN1 configuration, while in mandibular second premolars, it was observed in 95.75% of males and 94.50% of females. These high percentages highlight the prevalence of the 1TN1 configuration in mandibular premolars, aligning with previous studies51,52, which also reported the 1TN1 configuration as the most common in mandibular premolars. The minimal occurrences of supplemental configurations, such as 1TN1–2−1 and 1TN1–2, suggest that while anatomical variations exist, they are relatively rare in mandibular premolars. These findings are crucial for endodontic practitioners as they indicate that the majority of mandibular premolars are likely to have a straightforward canal system, simplifying the procedures of cleaning, shaping, and obturation. Additionally, the study observed other configurations such as 1TN1–2−3−2, 2TN B1 L1, 2TN 1B1 L1, 2TN 1M1/D1–2−1, and 2TN M1/D1, though these were present in very low frequencies across both genders. The lack of statistically significant differences (p > 0.05) in the distribution of these configurations between males and females suggests that gender does not significantly influence the root canal morphology of mandibular premolars73. This consistency between genders further reinforces the predictability of the 1TN1 configuration in clinical practice.
Across all age groups, the 1TN1 configuration was the most prevalent in both mandibular first and second premolars. The presence of supplemental configurations such as 1TN1–2−1 and 1TN1–2 in mandibular first premolars, and configurations such as 1TN1–2 and 2TN B1/L1 in mandibular second premolars, albeit in lower frequencies, suggests some degree of anatomical complexity that varies with age. Despite these observations, the study found no statistically significant differences in the distribution of root canal configurations among the different age groups for both mandibular first and second premolars (p > 0.05). This lack of significant variation suggests that the root canal morphology in mandibular premolars remains relatively stable across different ages, which is important for endodontic treatment planning. However, additional configurations such as 1TN1–2−3−2, 2TN B1 L1, 2TN 1B 1 L1, 2TN1M1/D1–2−1, and 2TNM1/D1 were also observed across all age groups, indicating some degree of anatomical variability. These findings highlight the need for careful radiographic assessment and individualized treatment strategies in endodontic practice74. Understanding that the predominant 1TN1 configuration remains consistent, and can aid clinicians in anticipating the common root canal morphology, while also being prepared for less frequent, more complex configurations. This comprehensive understanding of root canal anatomy can enhance the success of endodontic procedures and improve patient outcomes.
Clinical implications
The predominant 1TN1 configuration in maxillary and mandibular anterior teeth suggests relatively straightforward treatments, but the presence of more complex canal systems necessitates careful preoperative planning. Clinicians should be prepared for variations such as multiple roots or complex canal configurations, especially in maxillary premolars, which may need to employ advanced techniques such as CBCT for accurate mapping of complex anatomies. These anatomical variations also have clinical implications in terms of instrumentation and treatment outcomes. For example, variations in root canal morphology, such as the presence of extra roots or canals may influence the choice of instruments and techniques, such as using troughing between canal orifices, using lesser tapered instruments in teeth with extra roots because of the reduced root dentine thickness and warm compaction techniques in complex canal configurations52. Recognizing these variations can help endodontists minimize the risk of treatment failure, particularly in cases that may require retreatment or surgical intervention75. This study emphasizes the value of personalized treatment plans that account for anatomical diversity, ensuring higher success rates and improved long-term outcomes for patients in Saudi Arabia.
Limitations
The sample size and demographic characteristics of the participants may limit the generalizability of our findings to broader subpopulations in Saudi Arabia. Additionally, variations in CBCT imaging parameters, such as resolution and voxel size, may influence the quality and clarity of the images, which could impact the accuracy of the morphological assessments. Potential artifacts, such as those caused by patient movement or metallic restorations, could also affect image interpretation. These limitations should be considered when interpreting the results, and future studies with larger, more diverse samples and standardized imaging protocols would help to further validate the findings.
Conclusions
This study identified a wide range of root and canal anatomical variations in anterior and premolar teeth within a Saudi subpopulation. Our findings revealed that while age influenced the complexity of root canal systems in mandibular incisors, no significant association between gender and canal complexity was observed. The Ahmed et al. classification system offered a detailed analysis of these complex variations, providing a clear understanding of the root canal morphology in this population.
Given these findings, future research should focus on exploring the clinical impact of these anatomical variations on treatment outcomes, such as the success rates of root canal therapies and long-term prognoses. Additionally, further studies should investigate how these variations influence specific endodontic procedures, including canal instrumentation and root canal filling techniques. Expanding research to include diverse populations will help refine treatment approaches and provide more comprehensive insights into the role of genetic, environmental, and demographic factors in shaping root canal morphology.
Data availability
The data set used in the current study will be made available at the reasonable request to the corresponding authors.
References
Vertucci, F. J. Root canal morphology and its relationship to endodontic procedures. Endod. Top. 10 (1), 3–29 (2005).
Essam, O. et al. The endodontic complexity assessment tool (E-CAT): a digital form for assessing root canal treatment case difficulty. Int. Endod. J. 54 (7), 1189–1199 (2021).
Bueno, M. R. et al. Root canal shape of human permanent teeth determined by new cone-beam computed tomographic software. J. Endod. 46 (11), 1662–1674 (2020).
Ahmed, H. et al. Application of a new system for classifying root canal morphology in undergraduate teaching and clinical practice: a national survey in Malaysia. Int. Endod. J. 53 (6), 871–879 (2020).
Peikoff, M. & Trott, J. An endodontic failure caused by an unusual anatomical anomaly. J. Endod. 3 (9), 356–359 (1977).
Karobari, M. I. et al. Micro computed tomography (Micro-CT) characterization of root and root canal morphology of mandibular first premolars: a systematic review and meta-analysis. BMC Oral Health 24 (1), 1 (2024).
Razumova, S. et al. Evaluation of cross-sectional root canal shape and presentation of new classification of its changes using cone-beam computed tomography scanning. Appl. Sci. 10 (13), 4495 (2020).
Weng, X. L. et al. Root canal morphology of permanent maxillary teeth in the Han nationality in Chinese Guanzhong area: a new modified root canal staining technique. J. Endod. 35 (5), 651–656 (2009).
Karobari, M. I. et al. Root and canal morphology of the anterior permanent dentition in Malaysian population using two classification systems: a CBCT clinical study. Aust. Endod. J. 47 (2), 202–216 (2021).
Rankine-Wilson et al. The bifurcated root canal in lower anterior teeth. J. Am. Dent. Assoc. 70 (5), 1162–1165 (1965).
Nogueira Leal et al. Evaluation of root canal configuration of maxillary and mandibular anterior teeth using cone beam computed tomography: an in-vivo study. Quintessence Int. 47, 1 (2016).
Cleghorn, B. et al. Anomalous mandibular premolars: a mandibular first premolar with three roots and a mandibular second premolar with a C-shaped canal system. Int. Endod. J. 41 (11), 1005–1014 (2008).
Zhengyan, Y. et al. Cone-beam computed tomography study of the root and canal morphology of mandibular permanent anterior teeth in a Chongqing population. Ther. Clin. Risk Manag. 1, 19–25 (2015).
Iqbal, A. et al. Evaluation of root canal morphology in permanent maxillary and mandibular anterior teeth in Saudi subpopulation using two classification systems: a CBCT study. BMC Oral Health 22 (1), 171 (2022).
Vertucci, F. et al. Root canal morphology of the human maxillary second premolar. Oral Surg. Oral Med. Oral Pathol. 38 (3), 456–464 (1974).
Kartal, N. et al. Root canal morphology of maxillary premolars. J. Endod. 24 (6), 417–419 (1998).
Ahmed, H. M. A. et al. Accessory roots and root canals in maxillary premolar teeth: a review of a critical endodontic challenge. ENDO Endod. Pract. Today 6 (1), 7–18 (2012).
Abella, F. et al. Cone-beam computed tomography analysis of the root canal morphology of maxillary first and second premolars in a Spanish population. J. Endod. 41 (8), 1241–1247 (2015).
Bürklein, S. et al. Evaluation of the root canal anatomy of maxillary and mandibular premolars in a selected German population using cone-beam computed tomographic data. J. Endod. 43 (9), 1448–1452 (2017).
Martins, J. N. R. et al. Root and root canal morphology of the permanent dentition in a caucasian population: a cone-beam computed tomography study. Int. Endod J. 50 (11), 1013–1026 (2017).
Yu, X. et al. Cone-beam computed tomography study of root and canal morphology of mandibular premolars in a western Chinese population. BMC Med. Imaging 12, 18 (2012).
Wolf, T. G. et al. Root canal morphology of the mandibular second premolar: a systematic review and meta-analysis. BMC Oral Health 21 (1), 309 (2021).
Arayasantiparb, R. & Banomyong, D. Prevalence and morphology of multiple roots, root canals and C-shaped canals in mandibular premolars from cone-beam computed tomography images in a Thai population. J. Dent. Sci. 16 (1), 201–207 (2021).
Ahmed, H. M. A. et al. A new system for classifying root and root canal morphology. Int. Endod. J. 50 (8), 761–770 (2017).
Saber, S. et al. Root and canal morphology of maxillary premolar teeth in an Egyptian subpopulation using two classification systems: a cone beam computed tomography study. Int. Endod. J. 52 (3), 267–278 (2019).
Fayad, M. I. & Johnson, B. R. Utilization of cone beam computed tomography in endodontic diagnosis. 3D Imaging in Endodontics: A New Era in Diagnosis and Treatment 57–82 (2023).
Kaur, K. et al. Exploring technological progress in three-dimensional imaging for root canal treatments: a systematic review. Int. Dent. J. 1, 1 (2024).
Patel, S. et al. Cone beam computed tomography (CBCT) in endodontics. Dent. Update 37 (6), 373–379 (2010).
Estrela, C. et al. Common operative procedural errors and clinical factors associated with root canal treatment. Braz. Dent. J. 28 (2), 179–190 (2017).
General Statistics Authority. The Population Development of Al-Kharj. (2022).
Ahmed & Dummer A new system for classifying tooth, root and canal anomalies. Int. Endod. J. 51 (4), 389–404 (2018).
Dilip Katakam, M. et al. Exploring the depths: a comparative study of material properties and sealing efficacy among commonly used root canal sealers in endodontics. J. Pharm. Negat. Results 1, 6664–6669 (2022).
Mohamad, B. Impact of Cone Beam Computed Tomography on Treatment Planning in Endodontics (2017).
Kolarkodi, S. H. The importance of cone-beam computed tomography in endodontic therapy: a review. Saudi Dent. J. 35 (7), 780–784 (2023).
Jacobs, R. Dental cone beam CT and its justified use in oral health care. J. Belg. Soc. Radiol. 94, 5 (2011).
Sukovic, P. Cone beam computed tomography in craniofacial imaging. Orthod. Craniofac. Res. 6, 31–36 (2003).
Wanderley, V. A. et al. Dentomaxillofacial CBCT: clinical challenges for indication-oriented imaging. In Seminars in Musculoskeletal Radiology (Thieme Medical, 2020).
Reia, V. C. B. et al. Diagnostic accuracy of CBCT compared to panoramic radiography in predicting IAN exposure: A systematic review and meta-analysis. Clin. Oral Investig. 25, 4721–4733 (2021).
Altunsoy, M. et al. A cone-beam computed tomography study of the root canal morphology of anterior teeth in a Turkish population. Eur. J. Dent. 8 (03), 302–306 (2014).
Amardeep, N. S. et al. Root canal morphology of permanent maxillary and mandibular canines in Indian population using cone beam computed tomography. Anat. Res. Int. 2014, 1 (2014).
Ahmed, H. & Hashem, A. Accessory roots and root canals in human anterior teeth: a review and clinical considerations. Int. Endod. J. 49 (8), 724–736 (2016).
Liu, J. et al. CBCT study of root and canal morphology of permanent mandibular incisors in a Chinese population. Acta Odontol. Scand. 72 (1), 26–30 (2014).
Geduk, G. et al. Cone-beam computed tomography study of root canal morphology of permanent mandibular incisors in a Turkish sub-population. J. Oral Maxillofacial Radiol. 3 (1), 7–10 (2015).
Syed, G. A. et al. CBCT evaluation of root canal morphology of maxillary first premolar in Saudi subpopulation. J. Pharm. Bioallied Sci. 16 (Suppl 2), S1619–S1622 (2024).
Pawar, A. et al. An In-Vivo cone-beam computed tomography analysis of root and canal morphology of maxillary first permanent molars in an Indian population. Indian J. Dent. Res. 32 (1), 104–109 (2021).
Hasanreisoglu, U. et al. An analysis of maxillary anterior teeth: facial and dental proportions. J. Prosthet. Dent. 94 (6), 530–538 (2005).
Mashyakhy et al. Root and root canal morphology differences between genders: A comprehensive in-vivo CBCT study in a Saudi population. Acta Stomatol. Croatica 53 (3), 231–246 (2019).
Almonaitiene, R. et al. Factors influencing permanent teeth eruption. Part one–general factors. Stomatologija 12 (3), 67–72 (2010).
Albannay, B. Evaluation of Root and Canal Morphology of Mandibular Permanent Anterior Teeth in Emirati Subpopulation: A Cone-Beam Computed Tomography Study (2021).
Karobari, M. I. et al. Evaluation of root and canal morphology of mandibular premolar amongst Saudi subpopulation using the new system of classification: A CBCT study. BMC Oral Health 23 (1), 291 (2023).
Mustafa, M. et al. Assessment of the root and canal morphology in the permanent dentition of Saudi Arabian population using cone beam computed and micro-computed tomography—A systematic review. BMC Oral Health 24 (1), 343 (2024).
Ahmed, H. M. et al. Tooth, root, and canal anatomy. Endodontic Adv. Evid.-Based Clin. Guidel. 1, 1–50 (2022).
Walker, R. T. Root form and canal anatomy of maxillary first premolars in a southern Chinese population. Dent. Traumatol. 3 (3), 130–134 (1987).
Pécora, J. D. et al. Root form and canal anatomy of maxillary first premolars. Braz. Dent. J. 2 (2), 87–94 (1992).
Neelakantan, P. et al. Root and canal morphology of Indian maxillary premolars by a modified root canal staining technique. Odontology 99, 18–21 (2011).
Yang, L. et al. Use of cone-beam computed tomography to evaluate root canal morphology and locate root canal orifices of maxillary second premolars in a Chinese subpopulation. J. Endod. 40 (5), 630–634 (2014).
Candeiro, G. T. et al. Vertucci’s root canal configuration of 14,413 mandibular anterior teeth in a Brazilian population: a prevalence study using cone-beam computed tomography. J. Endod. 47 (3), 404–408 (2021).
Awawdeh, L. et al. Root form and canal morphology of Jordanian maxillary first premolars. J. Endod. 34 (8), 956–961 (2008).
Al-Ghananeem, M. M. et al. The number of roots and canals in the maxillary second premolars in a group of Jordanian population. Int. J. Dent. 2014, 1 (2014).
Haghanifar, S. et al. Morphologic assessment of mandibular anterior teeth root canal using CBCT. Acta Med. Acad. 46, 2 (2017).
Shemesh, A. et al. Root canal morphology evaluation of central and lateral mandibular incisors using cone-beam computed tomography in an Israeli population. J. Endod. 44 (1), 51–55 (2018).
Baxter, S. et al. Cone-beam-computed-tomography of the symmetry of root canal anatomy in mandibular incisors. J. Oral Sci. 62 (2), 180–183 (2020).
Ghabbani, H. M. et al. Assessment of root canal morphology of mandibular incisors using cone-beam computed tomography among residents of Al-Madinah Al-Munawara Region, Saudi Arabia. Eur. J. Gen. Dent. 9 (01), 40–44 (2020).
Tome, W. et al. Demonstration of a sex difference in the predictability of widths of unerupted permanent canines and premolars in a Japanese population. Angle Orthod. 81 (6), 938–944 (2011).
Martins, J. N. et al. Gender influence on the number of roots and root canal system configuration in human permanent teeth of a Portuguese subpopulation. Quintessence Int. 49 (2), 103–111 (2018).
Sert, S. & Bayirli, G. S. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J. Endod. 30 (6), 391–398 (2004).
Kayaoglu, G. et al. Root and canal symmetry in the mandibular anterior teeth of patients attending a dental clinic: CBCT study. Braz. Oral Res. 29, 1–7 (2015).
Aminsobhani, M. et al. Evaluation of the root and canal morphology of mandibular permanent anterior teeth in an Iranian population by cone-beam computed tomography. J. Dent. (Tehran) 10 (4), 358–366 (2013).
Gu, Y. et al. Detection of root variations of permanent teeth in a northwestern Chinese population by cone-beam computed tomography. Chin. J. Conserv. Dent. 21, 499–505 (2011).
Llena, C. et al. Cone-beam computed tomography analysis of root and canal morphology of mandibular premolars in a Spanish population. Imaging Sci. Dent. 44 (3), 221 (2014).
Buchanan, G. D. et al. Root and canal morphology of the permanent anterior dentition in a black South African population using cone-beam computed tomography and two classification systems. J. Oral Sci. 64 (3), 218–223 (2022).
Peiris, H. et al. Root canal morphology of mandibular permanent molars at different ages. Int. Endod. J. 41 (10), 828–835 (2008).
Alenezi, D. J. et al. Root and canal morphology of mandibular premolar teeth in a Kuwaiti subpopulation: A CBCT clinical study. Eur. Endod. J. 5 (3), 248 (2020).
Rahimi, S. et al. Root canal configuration of mandibular first and second premolars in an Iranian population. J. Dent. Res. Dent. Clin. Dent. Prospects 1 (2), 59–64 (2007).
Gulabivala, K. & Ng, Y. L. Factors that affect the outcomes of root canal treatment and retreatment—A reframing of the principles. Int. Endod. J. 56, 82–115 (2023).
Acknowledgements
The authors extend their appreciation to Prince Sattam bin Abdulaziz University for funding this research work through the project number (PSAU/2024/03/30714).
Author information
Authors and Affiliations
Contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted according to the guidelines of the Declaration of Helsinki and the current study obtained independent approval from the Institutional Review Board of Prince Sattam bin Abdulaziz University, Al-Kharj, with the reference number PSAU2020024. The CBCT images were sourced from the College of Dentistry, Prince Sattam Bin Abdulaziz University, Al Kharj, Saudi Arabia. These images were initially captured for various purposes unrelated to this study, such as for assessing traumatic injuries and conducting surgical procedures. The informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mustafa, M., Karobari, M.I., Al-Maqtari, A.A.A. et al. Investigating root and canal morphology of anterior and premolar teeth using CBCT with a novel coding classification system in Saudi subpopulation. Sci Rep 15, 4392 (2025). https://doi.org/10.1038/s41598-025-86277-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-86277-4