Abstract
The current stem cell tissue engineering always requires in vitro cell culture. To solve this problem, the bone mesenchymal stem cells (MSCs) screen-enrich-combine circulating system (SECCS) was created to rapidly enrich stem cells and combined with β-tricalcium phosphate (β-TCP) to immediately produce bioactive MSCs/β-TCP composites. 37 patients who underwent transforaminal lumbar interbody fusion (TLIF) surgery were included in this study and randomly divided into two groups. One group uses laminal bone grafts (LBG) for intervertebral fusion, and another group uses MSCs/β-TCP composites. The new technique could quickly and selectively enrich stem cells from the bone marrow and simultaneously implant them into the intervertebral space during operation. The cells eluted from the β-tricalcium phosphate were confirmed to be stem cells based on their characteristics. Higher early fusion rates, similar intervertebral height decreases, and functional improvement tendencies were observed in the SECCS group when compared to the LBG group. The bioactive scaffold prepared by SECCS showed better osteogenic efficiency at the early stage of intervertebral fusion compared to autologous LBG, which provided a new bone scaffold substitute for autologous bone.
Similar content being viewed by others
Lumbar spinal stenosis, disc herniation, spondylolisthesis, and other degenerative lumbar spine illnesses are prevalent orthopedic conditions that can cause severe pain and impairment. These complications not only negatively impact quality of life but also impose a great economic burden on the family and society1.
Lumbar interbody fusion is a common and effective treatment for lumbar degenerative disease2,3. Increasing the interbody fusion rate is the most important goal of surgery. Fusion failure may lead to a series of complications, such as lumbar instability, pseudarthrosis formation, pedicle screw and rod breakage, and even cage retropulsion4,5. Although many factors contribute to poor fusion, the choice of bone graft material is critical. The most commonly used bone graft for intervertebral fusion is the decompressed lamina bone. Despite the disadvantage that it contains too much cortical and sclerotic bone, the decompressed laminal bone demonstrates a satisfactory fusion rate6. However, in cases of infection or vertebral tumors, the laminal bone is not suitable for implantation. In addition, with the development and progress of minimally invasive technology, some new approaches have been developed, such as anterior lumbar interbody fusion (ALIF), oblique lumbar interbody fusion (OLIF), minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF), and endoscopic translaminar lumbar interbody fusion7,8,9,10. No autogenous bone transplant is available for these surgical approaches; hence, the iliac bone is always harvested. However, bone harvesting might cause discomfort, local hematoma, infection, nerve injury, and increased surgery time11. As a compromise, researchers are currently seeking a substitute scaffold for autologous bone grafts. An ideal bone graft material should have bone conduction, bone induction, and bone formation properties12. Recently, biomaterials and tissue engineering technologies have been rapidly developed. The use of new stem cell composite biomaterials to promote bone fusion has become a research hotspot and is gradually progressing towards clinical application. Quarto et al. found that expanding mesenchymal stem cells (MSCs) in vitro and combining them with porous hydroxyapatite particles could successfully repair large, long bone (7 cm) defects13. It demonstrates the powerful effects of stem cell therapy.
Stem cell-based tissue engineering technology has excellent application prospects for bone repair, according to laboratory and animal trials. However, clinical translation is subject to many restrictions, such as in vitro culture-related contamination, ethical concerns, and additional time cost14.
To overcome these difficulties, we developed a novel system called the bone marrow MSCs screen-enrich-combine circulating system (SECCS). MSCs from bone marrow can be quickly enriched and combined with porous β-tricalcium phosphate (β-TCP) to create bioactive composites without in vitro cell amplification. This method has successfully treated bone nonunions and deformities since 200415,16,17. However, we have not applied this technique to lumbar spine interbody fusion, and the role of the SECCS in promoting interbody fusion has not been reported. Therefore, we designed a randomized controlled clinical study to use the SECCS to efficiently combine MSCs with β-TCP for lumbar intervertebral fusion. We then observed the clinical outcome compared with a traditional decompressed laminal bone graft (LBG). This research approach is expected to provide a new alternative method of bone grafting for lumbar interbody fusion. This article follows the CONSORT reporting checklist.
Materials and methods
Study participants
The study was approved by the Translational Medicine Ethics Committee (Approval Number: 2016-179-T123). All methods were performed in accordance with the Declaration of Helsinki and informed consent was obtained from all participants and/or their legal guardians. The study was registered for CHICTR (https://www.chictr.org.cn/index.html) on 06/03/2017, and the registration number was ChiCTR-INR-17,010,805. From June 2019 to December 2021, patients who were diagnosed with degenerative lumbar diseases and were ready for the transforaminal lumbar interbody fusion (TLIF) procedure were recruited into this study. The inclusion criteria for patients were as follows: (1) aged from 18 to 65 years, regardless of whether patients were male or female; (2) diagnosed with degenerative lumbar diseases; (3) did not participate in another clinical study within three months; and (4) voluntarily participated and provided signed informed consent. The exclusion criteria were as follows: (1) fracture; (2) tumor; (3) infection; (4) severe osteoporosis; (5) revision surgery; (6) mental illness; (7) metabolic or immune dysfunction; (8) drug abuse; (9) severe primary diseases of vital organs; (10) allergy; (11) pregnancy and breastfeeding; or (12) poor compliance. After the patients signed the informed consent form, they were randomly divided into two groups according to a computer-generated random number table. One group used laminal bone grafts (LBG) produced after spinal canal decompression for intervertebral fusion, and another group received MSCs/β-TCP composites prepared by the SECCS for intervertebral fusion. Eventually, 37 patients were enrolled in the study, of whom 19 received LBG treatment and 18 received SECCS treatment (Fig. 1). The detailed data of patients included in the two groups is demonstrated in Table 1.
Preparation of MSCs/β-TCP paticles
After general anesthesia, the patient was placed in a supine position, and a 16-gauge bevel medullo-puncture needle was used to puncture the anterior superior iliac spine. Approximately 80 mL of bone marrow was collected before surgery (Fig. 2A). The SECCS system mainly consists of the following parts: (1) a detachable columnar double-layer filter box, which is used for loading the porous biomaterial and hemofiltration; (2) a sealed pipeline for fluid circulation; and (3) a peristaltic pump that exerts a force to drive the continuous circulation of the bone marrow (Fig. 2B–D). When the procedure was started, 3 ~ 6 g β-TCP particles (Bio-Lu Bioceramic, Shanghai Bio-Lu Biomaterials Co., Ltd., China) with mechanical strength > 2 Mpa, porosity > 40%, a diameter of 1–3.5 mm, and a mean pore size of 500 ± 200 μm were placed in the inner box. The inner and outer filter boxes were then screwed together. Approximately 60 mL of bone marrow was injected into the pipeline, and the power pump was started to circulate the bone marrow in the pipeline and filter it through the porous β-TCP (Fig. 2E-F). After 6 min (60 r/min, 50 HZ), the MSC-enriched β-TCP (MSCs/β-TCP composites) particles were manufactured and ready for implantation. In addition, 5 mL of bone marrow before and after enrichment was collected for cell culture and testing.
Major component parts of the SECCS. (A) Bone marrow was aspired from iliac bone. (B) The box was assembled for placement of TCP. (C) The parts of the box were separated. (D) The box was linked to three-way switch. (E) Bone marrow was injected into the assembled circulation pipeline from the three-way switch. (F) Bone marrow was circulated in the pipeline using a peristaltic pump.
Surgical procedure
After the collection of bone marrow blood, the patient was placed in a prone position, and sterile drapes were placed on the surgical field after disinfection. TLIF was performed as previously reported18. In particular, decompressed laminal bone was used as the bone graft in front of the intervertebral space and in the fusion cage (PEEK: Polyether ether ketone, Capstone, Medtronic Sofamor Danek USA, Inc.) for patients in the LBG group. On the other hand, MSC/β-TCP composites were used as the bone graft in front of the intervertebral space and in the cage for fusion in the SECCS group. For patients undergoing two-level surgery, the same bone graft material was used for each level. In addition, bilateral pedicle screws and rods (CDHORIZON Spinal System, Medtronic Sofamor Danek USA, Inc.) were used for fixation. All surgeries were performed by the same chief surgeon and the same team of doctors.
Enrichment efficiency evaluation
5 ml of bone marrow before and after enrichment was collected for detection and cultivation. First, a cell counting machine (Beckman Coulter, USA) detected the viability of nuclear cells. Then, a blood cell analyzer was used to look at the bone marrow before and after enrichment to see how the basic parts of the bone marrow, such as leukocytes, erythrocytes, hemoglobins, and platelets, had changed. Besides, bone marrow were cultured with ɑ Minimum Essential Medium (ɑ-MEM, Sigma, USA) with 10% fetal bovine serum (FBS; HyClone). Every two days, the medium was changed. After 10 to 14 days, it was switched out for osteogenic induction solution (ɑ-MEM + 50 µM sodium ascorbate [Sigma] + 10 mM glycerophosphate [Sigma, USA] + 100 nM Mdexamethasone [Sigma, USA]), and the cells were cultured for another 10 to 14 days. Next, the cell colonies were fixed with 4% paraformaldehyde and stained with alkaline phosphatase (ALP: NBT/BCIP; Beyotime, Shanghai, China). The number of ALP-positive colony-forming units (CFUs/ALP+) with a diameter of more than 2 mm was counted and identified as MSC colonies. The reduced number of CFUs/ALP + colonies after enrichment compared to pre-enrichment represents the number of MSCs implanted in each patient. Enrichment efficiency was formulated as (PreCFUs/ALP+ – PostCFUs/ALP+)/PreCFUs/ALP+ × 100%.
Scanning electron microscope (SEM) observation and differentiation induction
Some MSC/β-TCP granules were collected and respectively cultured with ɑ-MEM for 2 h and 21 days before SEM observation, and the cells eluted from MSC/β-TCP granules were collected and cultuered for osteogenic, adipogenic, and chondrogenic differentiation, and undergo corresponding Alizarin Red staining, Oil Red O staining, and Alcian Blue staining respectively as previously reported15.
Flow cytometry
The MSC/β-TCP composite granules that remained after surgery were collected for detective, and the MSCs were eluted by Tripsin-EDTA (Gibco, America). The cells were resuspended and cultured in MEM for 14 days. Then the adherent cells were digested and labeled with CD44, CD73, CD90, CD105, CD34, CD11b, CD19, CD45, and HLA-DR antibodies (BD Biosciences, USA) to identify MSC markers by flow cytometry (RRID: AB_2869404, Becton, Dickinson and Company, USA).
Patient follow-up
All patients were routinely followed up within one week, three months (± 7 days), six months (± 15 days), and one year after surgery. The intervertebral fusion rate was evaluated using X-ray and computed tomography (CT) scans. According to dynamic X-ray radiographs, with the angle between the vertebral bodies less than 5°, continuous trabecular bone formation in the segment analyzed by CT is recognized as fusion. Fusion failure is determined to have occurred when the cage is loosened and shifted, there is a translucent band > 2 mm on the cage surface, and the angle between the vertebral bodies is > 5° on the dynamic radiographs19,20 (supplement 1). Intervertebral height collapse can also reflect the fusion quality; as such, we observed the change in intervertebral height, which was calculated as follows: (anterior disc height + posterior disc height)/2. Functional improvement was evaluated using the Japanese Orthopaedic Association (JOA) and Oswestry Disability Index (ODI) scores. The images were blindly evaluated by two senior orthopedic surgeons and one radiologist, and the unanimously judged result of two or three doctors was confirmed to be the approved result.
Statistical analysis
SPSS 22.0 statistical software (IBM Corp., America) was used for data management and statistical analysis. The measurement data are expressed as‾X ± S, and the count data are expressed as rate (%). The normal distribution was evaluated by the Shapiro-Wilk test. Two sample t-test or paired t-test was used to compare normally distributed variables. Chi-squared test was used to compare the proportion. P < 0.05 was considered to indicate a statistically significant difference.
Results
A total of 37 patients in both groups were followed up for one year without any complications or other adverse events. 18 patients in the SECCS group had no complications such as hematoma or infection at the puncture site, and there were no complaints of pain or any other discomfort after surgery.
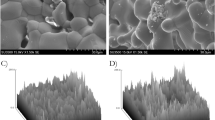
The SECCS can successfully enrich MSCs from bone marrow
To confirm that the cells adhered to β-TCP were indeed MSCs, the cells eluted from TCP particles were collected for stem cell identification. In fact, after SECCS processing, the white TCP particles became red, indicating that cells from bone marrow adhered to TCP, especially red blood cells (Fig. 3A-B). In order to confirm that the MSCs adhered to TCP particles and maintained their proliferation capacity, we cultured the TCP particles for 21 days and found the particles were all ALP-positive, suggesting that the MSCs were successfully grown on TCP particles (Fig. 3C). After SECCS filtration, the number of ALP-positive CFUs was significantly reduced (Fig. 3D-E), indicating a lot of MSCs were captured by TCP and implanted into patients. By scanning the TCP immediately after enrichment, we confirmed that MSCs and many erythrocytes were captured, and at this time, the cells had not spread completely. However, after being cultured for 21 days, erythrocytes disappeared while MSCs had spread completely and demonstrated fibroblast-like morphology (Fig. 3F–G). In addition, cells eluted from β-TCP particles were successfully induced for osteogenic, adipogenic, and chondrogenic differentiation (Fig. 3H–J). Flow cytometry showed that the cells were negative for Lin (including CD34, CD11b, CD19, CD45, and HLA-DR) and positive for CD44 (99.99%), CD73 (100%), CD90 (97.9%), and CD105 (91.3%) (Fig. 4A–E). These results demonstrate that the SECCS can successfully enrich MSCs from the bone marrow.
Identification of stem cells. (A) β-TCP particles before preparation by the SECCS. (B) β-TCP particles after preparation by the SECCS. (C) ALP staining for β-TCP after preparation by the SECCS. (D-E) Colony-forming units from bone marrow pre- and post- enrichment. (F) Scanning electron microscope images of cells adhered to β-TCP immediately after preparation by the SECCS. (G) Scanning electron microscope images of cells adhered to β-TCP after preparation by the SECCS and cultured for 3 weeks. (H-J) Alizarin Red, Oil Red O, and Alcian blue staining of cells eluted from β-TCP.
The SECCS demonstrated selective enrichment for MSCs
To evaluate the enrichment efficiency of MSCs by the SECCS, pre- and post-enriched bone marrow was collected. First, we observed that cell viability was not reduced immediately after enrichment (Fig. 5A). And then we found that platelets showed significant enrichment (26.8 ± 18.2%), while other components, including erythrocytes, leukocytes, and hemoglobins, were not significantly reduced after enrichment (Fig. 5B-E). Importantly, we observed a significant decrease in cell colonies after enrichment; there were 182.3 ± 23.4 CFUs/mL formed before enrichment and 30.4 ± 11.0 CFUs/mL formed after enrichment, of which the enrichment efficiency was 83.6 ± 4.3% (Fig. 5F).
Evaluation for the enrichment efficiency of SECCS. (A) Cell viability pre- and post-enrichment. (B-E) Changes in the different components of bone marrow pre- and post-enrichment. (F) Numbers of Colony-forming units pre- and post-enrichment. The pre- and post-numbers are 18 each. **Indicated P < 0.01, ****Indicated P < 0.0001.
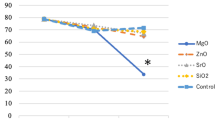
The SECCS possesses a similar clinical effect to autologous bone grafts
Follow-up was conducted for 19 patients (25 lumbar segments) in the LBG group and 18 patients (26 lumbar segments) in the SECCS group. We found that the intervertebral height was all reduced after TLIF compared to pre-operation, and the height continuously decreased with time; however, a similar downward trend was observed in both groups (Fig. 6A). Furthermore, even though the two groups acquired the same fusion rate at 12 months for 100% fusion, while at an early stage, cases in the SECCS group showed a higher fusion rate than the LBG group (Table 2). In addition, the JOA score represented surgical improvement rate, and the ODI score represented low back pain intensity; both showed a similar increasing or decreasing trend between the two groups, respectively (Fig. 6B-C). A typical case of a patient who received SECCS treatment is shown in Fig. 7A–G, which indicates satisfactory intervertebral fusion after 3, 6, and 12 months of follow-up.
A typical case of a patient (Female, 56 years old, diagnosed with lumbar disc herniation and lumbar spinal stenosis) who received SECCS treatment at the L4/5 level. (A) The sagittal MRI of lumber spine before surgery. (B) The transverse MRI of L4/5 before surgery. (C) Cage filled with bioactive MSC/β-TCP. (D) Postoperative cross-sectional CT showed that the fusion cage was placed transversely in the L4/5 intervertebral space. (E-G) Three-, six-, and twelve-month follow-up of the L4/5 intervertebral fusion by sagittal CT scan.
Discussion
In this study, the SECCS circulates bone marrow blood in a sealed conduit, and we found no effect on cell viability. The MSC enrichment rate can reach over 80% in 6 min, and they sustain proliferative viability and osteogenic differentiation in vitro. In TLIF surgery, the ß-TCP-loaded MSCs showed higher bone formation capacity at the early stage of intervertebral fusion, and they also caused similar decreases in intervertebral height and functional improvement compared to autologous bone grafts.
In 1995, Crane et al. proposed the concept of bone tissue engineering, which uses natural or synthetic materials as a scaffold for cell transplantation21. BMSCs have strong osteogenic differentiation ability, and are often seeded on scaffolds to be implanted in bone defects. Good results have been achieved in both experimental and clinical settings22, however, they are rarely used for spinal fusion. Due to the minimal number of MSCs in bone marrow and the majority of cells being unwanted, selecting and enriching cells is the main goal of stem cell therapy. The most common method to obtain these cells is to separate MSCs and amplify them in vitro. In Zheng’s mouse L4/L5 interbody fusion model, bone marrow MSCs were seeded on a collagen sponge scaffold and grown in osteoblast induction medium for three weeks to create a cell-scaffold complex that was implanted in the intervertebral space. After 12 weeks, bone marrow MSCs could induce osseous fusion in the lumbar vertebrae23. Lu24employed New Zealand rabbits with L3–L6 intervertebral discs removed to cultivate bone marrow MSCs on porous tantalum implants for intervertebral body fusion to compare with autologous bone transplantation. Radiographic fusion index scores at 12 months post-op were similar for autograft and tantalum groups. In another study, Li25 removed the rat tail vertebral disc and created a spinal intervertebral fusion model. This study loaded bone marrow MSCs onto polycaprolactone and nano-hydroxyapatite porous scaffolds treated with a sinusoidal electromagnetic field (EMF). The results revealed that the scaffold loaded with MSCs was successfully stimulated by EMF, which accelerates intervertebral fusion. Although all of these studies eventually revealed a satisfactory interbody fusion ratio, but they all required in vitro MSC culture, which demands extra time, stringent culture conditions, and secondary implantation, and they were performed only on animals.
Ofluoglu26filled β-TCP in the cage for anterior cervical fusion and achieved good clinical and radiological results, demonstrating the feasibility of using β-TCP in the intervertebral space of humans. However, due to the lack of bioactivity of β-TCP27, this method of bone grafting has not been widely recognized in clinical practice. Lechner28 mixed β-TCP and bone marrow aspirate as a bone graft substitute in anterior lumbar interbody and achieved a good fusion rate, but did not mention the mechanisms of action of bone marrow and bone marrow mesenchymal stem cells.
Our SECCS system is just designed to avoid the restrictions by not requiring in vitro cell cultivation, and this study is the first to use stem cells and biomaterials for TLIF. The β-TCP utilized in this study is a synthetic bioceramic with the formula Ca3(PO4)2. Chemically identical to inorganic bone components, it has good compressive strength and biocompatibility29. The porous nature of β-TCP provides a wider surface area for collecting bone marrow MSCs during blood circulation. In fact, the combination of TCP with MSCs not only provides osteogenic cells but also provides cytokines and growth factors that promote bone production, enabling quick and robust bone creation30. However, there have been no reports of using β-TCP solely as a bone graft material for lumbar interbody fusion in humans. A failure of fusion could lead to serious clinical consequences; therefore, due to safety considerations, we did not include it in the control group.
Previous research demonstrated saturation of MSC enrichment after five cycles of circulation in 10 min15. To accelerate MSC/β-TCP particle production for implantation, we improved circulation speed to 6 min with a peristaltic pump at 60 rounds per minute. Unexpectedly, we observed that platelets, like MSCs, are prone to adhering to β-TCP, with an enrichment rate of about 26%. Recent studies showed that platelet-rich plasma (PRP) can promote tissue repair, wound healing, and bone repair through the abundant cytokines released by platelets31,32. As for lumbar interbody fusion, multiple studies have demonstrated its positive effects33,34. Moreover, PRP can also enhance the biological properties of mesenchymal stem cells35. Since the enrichment rate of platelets from bone marrow is not as high as that of MSCs, the extent to which it promotes fusion in this study remains unclear. In summary, the enrichment of mesenchymal stem cells and platelets can facilitate lumbar interbody fusion.
This study has several limitations. First of all, this research is monocentric and prospective, and it’s possible that surgeons’ performance bias influenced the results. Secondly, due to a limited number of cases, we were unable to conduct a stratified analysis based on gender, age, region, and disease type. As a result, a more accurate understanding of the effectiveness of the proposed method among patients with different conditions could not be obtained. Additionally, the quantitative evaluation of stem cells is indeed challenging, and at present, we are unable to determine the exact number of stem cells implanted into the body. Subsequent research will focus on this aspect. Lastly, the follow-up time in this study is relatively short; although no recurrences were observed 12 months postoperatively, an extended follow-up is imperative to ascertain long-term efficacy.
It is our hope that the bone graft prepared by the SECCS can provide a substitute for autologous bone grafts in intervertebral fusion. However, it must be noted that this study did not simply target typical TLIF surgery. As the SECCS’s quality for intervertebral fusion is good, it may be more suitable for diseases such as vertebral tumors, infections, or osteoporosis, where laminal bone cannot be used as a bone graft. When anterior, lateral, or endoscopic surgery is chosen and the laminal bone is unavailable, the SECCS may also be useful.
Conclusions
This study shows that the new SECCS method, which involves making bioactive MSC/β-TCP scaffold very quickly, is easy to use, safe, and effective for lumbar intervertebral fusion. As such, this method could avoid complications caused by iliac bone harvest. Because of its similar bone regeneration efficiency to autologous bone grafts, the SECCS technique has broad prospects for clinical application, especially as a replacement for autologous bone.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Martin, B. I. et al. Trends in lumbar Fusion Procedure Rates and Associated Hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa. 1976). 44, 369–376. https://doi.org/10.1097/BRS.0000000000002822 (2019).
Aoki, Y. et al. Changes in lumbar lordosis and predicted minimum 5-year surgical outcomes after short-segment transforaminal lumbar interbody fusion. Sci. Rep. 12, 14353. https://doi.org/10.1038/s41598-022-18679-7 (2022).
Takaoka, H. et al. Comparison between intervertebral oblique lumbar interbody fusion and transforaminal lumbar interbody fusion: a multicenter study. Sci. Rep. 11, 16673. https://doi.org/10.1038/s41598-021-95774-1 (2021).
Kovac, V. Failure of lumbar disc surgery: management by fusion or arthroplasty? Int. Orthop. 43, 981–986. https://doi.org/10.1007/s00264-018-4228-9 (2019).
Li, N. et al. Risk factors for cage retropulsion after transforaminal lumbar interbody fusion in older patients. Ann. Transl Med. 8, 1660. https://doi.org/10.21037/atm-20-7416 (2020).
Han, S. et al. Comparison of Fusion rate between demineralized bone matrix versus autograft in lumbar Fusion: Meta-Analysis. J. Korean Neurosurg. Soc. 63, 673–680. https://doi.org/10.3340/jkns.2019.0185 (2020).
Sun, D. et al. OLIF versus ALIF: which is the better surgical approach for degenerative lumbar disease? A systematic review. Eur. Spine J. 32, 689–699. https://doi.org/10.1007/s00586-022-07516-0 (2023).
Ao, S. et al. Comparison of preliminary clinical outcomes between percutaneous endoscopic and minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative diseases in a tertiary hospital: is percutaneous endoscopic procedure superior to MIS-TLIF? A prospective cohort study. Int. J. Surg. 76, 136–143. https://doi.org/10.1016/j.ijsu.2020.02.043 (2020).
Sousa, J. M., Ribeiro, H., Silva, J. L., Nogueira, P. & Consciencia, J. G. Clinical outcomes, complications and fusion rates in endoscopic assisted intraforaminal lumbar interbody fusion (iLIF) versus minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): systematic review and meta-analysis. Sci. Rep. 12, 2101. https://doi.org/10.1038/s41598-022-05988-0 (2022).
Liu, L. et al. Comparison between OLIF and MISTLIF in degenerative lumbar stenosis: an age-, sex-, and segment-matched cohort study. Sci. Rep. 13, 13188. https://doi.org/10.1038/s41598-023-40533-7 (2023).
Shin, S. R. & Tornetta, P. 3 Donor Site Morbidity after Anterior Iliac Bone Graft Harvesting. J. Orthop. Trauma. 30, 340–343. https://doi.org/10.1097/BOT.0000000000000551 (2016).
Hasan, A. et al. Advances in osteobiologic materials for bone substitutes. J. Tissue Eng. Regen Med. 12, 1448–1468. https://doi.org/10.1002/term.2677 (2018).
Quarto, R. et al. Repair of large bone defects with the use of autologous bone marrow stromal cells. N Engl. J. Med. 344, 385–386. https://doi.org/10.1056/NEJM200102013440516 (2001).
Peric Kacarevic, Z. et al. An introduction to bone tissue engineering. Int. J. Artif. Organs. 43, 69–86. https://doi.org/10.1177/0391398819876286 (2020).
Wang, X. et al. Bone mesenchymal stem cell-enriched beta-tricalcium phosphate Scaffold processed by the screen-enrich-combine circulating System promotes regeneration of Diaphyseal Bone Non-union. Cell. Transpl. 28, 212–223. https://doi.org/10.1177/0963689718818096 (2019).
Chu, W. et al. Mesenchymal stem cells and porous beta-tricalcium phosphate composites prepared through stem cell screen-enrich-combine(-biomaterials) circulating system for the repair of critical size bone defects in goat tibia. Stem Cell. Res. Ther. 9, 157. https://doi.org/10.1186/s13287-018-0906-1 (2018).
Gan, Y. et al. The clinical use of enriched bone marrow stem cells combined with porous beta-tricalcium phosphate in posterior spinal fusion. Biomaterials 29, 3973–3982. https://doi.org/10.1016/j.biomaterials.2008.06.026 (2008).
Ge, D. H. et al. Comparative Analysis of Two Transforaminal Lumbar Interbody Fusion Techniques: Open TLIF Versus Wiltse MIS TLIF. Spine (Phila Pa 1976) 44, E555-E560 (2019). https://doi.org/10.1097/BRS.0000000000002903
Gruskay, J. A., Webb, M. L. & Grauer, J. N. Methods of evaluating lumbar and cervical fusion. Spine J. 14, 531–539. https://doi.org/10.1016/j.spinee.2013.07.459 (2014).
Park, Y., Ha, J. W., Lee, Y. T. & Sung, N. Y. The effect of a radiographic solid fusion on clinical outcomes after minimally invasive transforaminal lumbar interbody fusion. Spine J. 11, 205–212. https://doi.org/10.1016/j.spinee.2011.01.023 (2011).
Crane, G. M., Ishaug, S. L. & Mikos, A. G. Bone tissue engineering. Nat. Med. 1, 1322–1324. https://doi.org/10.1038/nm1295-1322 (1995).
Gjerde, C. et al. Cell therapy induced regeneration of severely atrophied mandibular bone in a clinical trial. Stem Cell. Res. Ther. 9, 213. https://doi.org/10.1186/s13287-018-0951-9 (2018).
Zheng, W. D., Ming, J. J. & Chang, W. L. The impact of collagen sponge composite bone marrow mesenchymal stem cells (BMSCs) in inducing interbody fusion. Eur. Rev. Med. Pharmacol. Sci. 22, 5822–5827. https://doi.org/10.26355/eurrev_201809_15908 (2018).
Lu, M. et al. Application of a novel porous tantalum implant in rabbit anterior lumbar spine fusion model: in vitro and in vivo experiments. Chin. Med. J. (Engl). 132, 51–62. https://doi.org/10.1097/CM9.0000000000000030 (2019).
Li, W. et al. Low-frequency electromagnetic fields combined with tissue engineering techniques accelerate intervertebral fusion. Stem Cell. Res. Ther. 12, 143. https://doi.org/10.1186/s13287-021-02207-x (2021).
Ofluoglu, A. E., Erdogan, U., Aydogan, M., Cevik, O. M. & Ofluoglu, O. Anterior cervical fusion with interbody cage containing beta-tricalcium phosphate: clinical and radiological results. Acta Orthop. Traumatol. Turc. 51, 197–200. https://doi.org/10.1016/j.aott.2017.03.001 (2017).
Bezerra Melo, M. C. et al. Enhanced mechanical strength and bioactivity of 3D-printed beta-TCP scaffolds coated with bioactive glasses. J. Mech. Behav. Biomed. Mater. 163, 106850. https://doi.org/10.1016/j.jmbbm.2024.106850 (2024).
Lechner, R., Putzer, D., Liebensteiner, M., Bach, C. & Thaler, M. Fusion rate and clinical outcome in anterior lumbar interbody fusion with beta-tricalcium phosphate and bone marrow aspirate as a bone graft substitute. A prospective clinical study in fifty patients. Int. Orthop. 41, 333–339. https://doi.org/10.1007/s00264-016-3297-x (2017).
Tian, Y. et al. beta-tricalcium phosphate composite ceramics with high compressive strength, enhanced osteogenesis and inhibited osteoclastic activities. Colloids Surf. B Biointerfaces. 167, 318–327. https://doi.org/10.1016/j.colsurfb.2018.04.028 (2018).
Gao, P. et al. Beta-tricalcium phosphate granules improve osteogenesis in vitro and establish innovative osteo-regenerators for bone tissue engineering in vivo. Sci. Rep. 6, 23367. https://doi.org/10.1038/srep23367 (2016).
Farmani, A. R. et al. Application of platelet Rich Fibrin in tissue Engineering: focus on bone regeneration. Platelets 32, 183–188. https://doi.org/10.1080/09537104.2020.1869710 (2021).
Al-Maawi, S. et al. Biologization of pcl-mesh using platelet Rich Fibrin (Prf) enhances its regenerative potential in Vitro. Int. J. Mol. Sci. 22 https://doi.org/10.3390/ijms22042159 (2021).
Imagama, S. et al. Efficacy of early Fusion with local bone graft and platelet-rich plasma in lumbar spinal Fusion surgery followed over 10 years. Global Spine J. 7, 749–755. https://doi.org/10.1177/2192568217696690 (2017).
Kubota, G. et al. Efficacy of platelet-rich plasma for Bone Fusion in Transforaminal lumbar Interbody Fusion. Asian Spine J. 12, 112–118. https://doi.org/10.4184/asj.2018.12.1.112 (2018).
Dai, P. et al. Multiomics analysis of platelet-rich plasma promoting biological performance of mesenchymal stem cells. BMC Genom. 25, 564. https://doi.org/10.1186/s12864-024-10329-8 (2024).
Acknowledgements
This work was supported by the Emerging Advanced Technology Joint Research Project (Grant No.SHDC12016110); the National Natural Science Foundation of China (Grant No.81871790, 81972136); the National Key R&D Program of China (Grant No.2017YFB1104104); and the Shanghai Leading Talents Program in 2020 (Grant No.110).
Author information
Authors and Affiliations
Contributions
B.D. and X.W. wrote the main manuscript text and prepared figures and tables.C.Z. and J.Z. conception and design of the work.All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ding, B., Wang, X., Zhao, C. et al. Rapid preparation of bioactive composites for transforaminal lumbar interbody fusion. Sci Rep 15, 4715 (2025). https://doi.org/10.1038/s41598-025-86776-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86776-4