Abstract
To investigate the influence of early dysphagia on quality of life in patients with partial laryngectomy, and to investigate the application value of Flexible Endoscopic Evaluation of Swallowing (FEES). This study included 30 inpatients who underwent partial laryngectomy due to laryngeal cancer. In the early postoperative period, a comprehensive assessment was conducted on each patient, encompassing Videofluoroscopic Swallowing Study (VFSS), Flexible Endoscopic Evaluation of Swallowing (FEES), and MD Anderson Dysphagia Inventory (MDADI). Each patient underwent two evaluations at different time points following the surgical procedure, all conducted on the same day. The patients’ first MDADI assement score after surgery was 45.4 ± 3.6 points, and the second score was 54.7 ± 13.4 points. VFSS as the gold standard, FEES showed good sensitivity (84%) and specificity (94%) for detecting aspiration, as well as good sensitivity (78%) and moderate specificity (86%) for detecting penetration. The Kappa consistency test results showed high consistency between FEES and VFSS swallowing function evaluations (Kappa value = 0.669); evaluations of thin liquid, thick liquid, and solid bolus had high consistency (Kappa value = 0.631, 0.675, and 0.678, respectively), while evaluations of semi-liquid bolus had poor consistency (Kappa value = 0.598); evaluations of four bolus sizes all had high consistency (Kappa value = 0.658, 0.647, 0.705, 0.670). The Kappa values for evaluating patients undergoing horizontal partial laryngectomy, vertical partial laryngectomy, and supraglottic laryngectomy were 0.572, 0.604, and 0.680, respectively. This study shows that dysphagia is an important problem affecting the early quality of life of patients after partial laryngectomy, and early instrumental evaluation is also extremely important. This study also emphasizes the reliability problems in the identification of false invasion and aspiration. FEES can be used to evaluate the early swallowing function of patients after partial laryngectomy, thus guiding the timing and type of eating, and evaluating the rehabilitation effect. In addition, compared with VFSS, FEES have more advantages for the identification of penetration.
Similar content being viewed by others
Introduction
Laryngeal cancer is a common malignant tumor in otolaryngology, accounting for 11–22% of malignant tumors in the head and neck region1,2. Surgery stands as the primary treatment method for laryngeal cancer, including total laryngectomy and partial laryngectomy3. Due to the long-term need for intubation and dysphonia, total laryngectomy has seriously affected the quality of life of patients 4, while partial laryngectomy with larynx preservation has been widely used in clinic 5.Total laryngectomy results in the separation of the respiratory and digestive tracts, damage to pharyngeal muscles, and narrowing of the neopharynx, often leading to dysphagia. Partial laryngectomy results in damage to and destruction of partial anatomical structures, nerves, and muscle functions in the larynx, often manifesting as aspiration, coughing, and residual pharynx, with aspiration posing a particular risk of aspiration pneumonia and life-threatening complications6,7,8.Therefore, detecting aspiration assumes paramount importance. Videofluoroscopic swallowing study (VFSS) and flexible endoscopic evaluation of swallowing (FEES) are considered the gold standards for diagnosing swallowing disorders9. VFSS has been the traditional gold standard with a long history of clinical application10. FEES can be easily performed at the bedside, suitable for daily monitoring, and minimizes patient exposure to radiation11. However, there is limited research on FEES in patients after partial laryngectomy.
Although the preservation of the larynx can greatly improve the quality of life of patients after partial laryngectomy, due to abnormal swallowing function for a long time after partial laryngectomy, patients often feel anxious, which affects social interaction and seriously affects the patient. Quality of life, even affecting further treatment of patients12.
The purpose of this study is to simultaneously conduct FEES and VFSS in early-stage patients after partial laryngectomy and assess patients using the MD Anderson Dysphagia Inventory (MDADI) to evaluate the application value of FEES and understand the impact of early-stage dysphagia after partial laryngectomy on patients.
Materials and methods
Inclusion criteria and exclusion criteria
Patients who underwent partial laryngectomy at the Department of Otolaryngology-Head and Neck Surgery of the First Hospital of Shanxi Medical University from August 2022 to October 2023. Inclusion criteria were as follows: (1) Patients diagnosed with laryngeal cancer for the first time and underwent partial laryngectomy at our hospital; (2) No complaints of swallowing disorders before surgery; (3) No swallowing rehabilitation performed after surgery. Exclusion criteria were as follows: (1) Presence of other diseases causing swallowing disorders (such as neurological diseases, neuromuscular junction diseases, muscular diseases, and other structural diseases of the oropharynx); (2) Severe malnutrition; (3) Severe surgical site infection postoperatively; (4) Poor compliance. This study was conducted in accordance with the Helsink i Declaration and approved by the Ethics Committee of the First Hospital of Shanxi Medical University (No.KYLL-2023-191). Informed consent was obtained from all patients.
Equipment
Japanese Olympus ENF-VH2 electronic nasopharyngoscope (equipped with OTV-S190 endoscopic high-definition imaging system) and gastrointestinal endoscopy with power above 500mmA and digital imaging system.
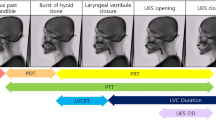
Grouping and assessment time
Group A (partial vertical laryngectomy) are assessed at 7–10 days and 25–30 days postoperatively. Group B (partial horizontal laryngectomy) are evaluated at 15–20 days and 25–30 days postoperatively. In Group C (Supra-cricoid partial laryngectomy), patients who undergo cricohyoidoepiglottopexy (CHEP) are assessed 10–15 days and 25–30 days postoperatively, while those who undergo cricohyoidopexy (CHP) are assessed at 25–30 days postoperatively and 40–45 days postoperatively. The questionnaires for FEES, VFSS, and MDADI are completed on the same day.
Pre-assessment test—banana puree swallowing test
Before undergoing VFSS and FEES, patients undergo a banana puree swallowing test13. Sitting upright with the head and neck slightly forward, a stainless steel blunt-ended long-handled spoon with a capacity of 10 ml is used to vertically scoop banana puree, ensuring uniform density without lumps or chunks. After filling the spoon, the patient is fed, and the banana puree is gently pressed towards the back of the tongue at the anterior 1/3 of the tongue. The patients are then instructed to close their lips immediately and swallow after each feeding, making an “ah” sound. Three spoonfuls are fed consecutively, with each spoonful containing approximately 7–10 ml. The assessment criteria are as follows: (1) Negative: the banana puree is smoothly swallowed for all three spoonfuls, and an “ah” sound is made after each swallow without any significant change in voice. (2) Positive: coughing or throat clearing occurs after swallowing the banana puree; the “ah” sound after swallowing the banana puree is more muffled or hoarse than before. The presence of any one symptom is considered positive. FEES and VFSS is conducted for negative patients.
Swallowing bolus
In accordance with Chinese dietary habits and the food grading standards in the Chinese Expert Consensus on Nutritional Management of Swallowing Disorders (2019 Edition), the types of boluses in this study, including Bolus 2 (thick liquid), Bolus 3 (pudding-like), and Bolus 4 (solid), all pass the spoon tilt test14. Bolus 1 (thin liquid) remains unchanged as water or Iohexol solution (50 ml:12 g), all pass the IDDSI Flow test15.
VFSS Swallowing Bolus: Divided into four types: Bolus 1 (thin liquid): Iohexol solution (50 ml:12 g); Bolus 2 (thick liquid): 75 ml Iohexol solution plus 2.5 g Ourdiet Swallow thickener(xanthan gum and little modified starch); Bolus 3 (pudding-like): 50 ml Iohexol solution plus 2.5 g Ourdiet Swallow thickener; Bolus 4 (solid): 50 ml Iohexol solution plus 5 g Ourdiet Swallow thickener.
FEES Swallowing Bolus: Divided into four types: Bolus 1 (thin liquid): water; Bolus 2 (thick liquid): 75 ml water plus 2.5 g Ourdiet Swallow thickener; Bolus 3 (pudding-like): 50 ml water plus 2.5 g Ourdiet Swallow thickener; Bolus 4 (solid): 50 ml water plus 5 g Ourdiet Swallow thickener. A small amount of edible green pigment is added to all 4 types of boluses.
Videofluoroscopic swallowing study (VFSS)
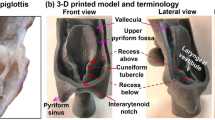
According to the requirements of the Videofluoroscopic Swallowing Study, the patients assume a right lateral position. Starting from the most viscous to the least viscous (from bolus 4 to bolus1), the patients sequentially ingest food boluses of different dose (5 ml, 10 ml, 15 ml, 20 ml). Before each ingestion, the patients rinse their mouths or swallows multiple times to clear residual material. Two experienced dysphagia physicians observe the procedure onsite and repeatedly review the recorded videos to identify any occurrences of aspiration or penetration. (Aspiration refers to the entry of a bolus into the airway below the vocal folds, while penetration refers to the entry of a bolus into the laryngeal cavity above the vocal folds. In post-laryngectomy patients, changes in laryngeal anatomy necessitated redefinition of terms, with the “vocal cords” referring to the postoperative neoglottis and “laryngeal vestibule” to the postoperative neopharynx vestibule.) Consensus was reached through collaborative discussion. For patients who experience aspiration, techniques such as back patting, coughing, or induced coughing (applying pressure above the trachea) are used to expel the aspirated material (including bolus 1, 2, 3 and 4). After each ingestion, the patients are instructed to assume anterior and posterior positions to check for signs of aspiration into the lungs. If significant aspiration occurs, the examination is halted. For suspected accidental invasion and aspiration, the swallowing test can be repeated for many times to obtain a true reflection of the patient’s real swallowing function16.
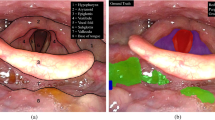
Flexible endoscopic evaluation of swallowing (FEES)
The patient was seated on the right side as an electronic laryngoscope is inserted through the nasal passage to the oropharynx. Similar to VFSS, the patient ingests food boluses (from bolus 4 to bolus1) of different dose (5 ml, 10 ml, 15 ml, 20 ml), rinsing their mouth, swallowing multiple times, or using suction to clear residual material before each ingestion. Following bolus ingestion, the laryngoscope is further advanced to observe the presence of residue in the pharynx and hypopharynx. Two experienced dysphagia physicians observe the procedure onsite and review the recorded videos to identify aspiration or penetration, reaching a consensus agreement. Similar aspiration management techniques are employed for patients who aspirate during FEES. The examination is halted if significant aspiration is observed. For suspected accidental invasion and aspiration, the swallowing test can be repeated for many times to obtain a true reflection of the patient’s real swallowing function. Figures 1 and 2 show the penetration and aspiration under FEES.
MD anderson dysphagia inventory (MDADI)
The MDADI is a self-assessment inventory developed by the MD Anderson Cancer Center in 2001, consisting of 20 items across four dimensions: overall (1 item), functional (5 items), emotional (7 items), and physiology (8 items). It is specifically designed to measure the impact of dysphagia on the quality of life of head and neck cancer patients, with lower scores indicating a greater negative impact on quality of life17. A Chinese version of the MDADI, translated and validated by Zou et al. in18, is used in conjunction with FEES and VFSS to assess the severity of dysphagia-related quality of life issues. Patients were also given twice post-operatively, each time MDADI was given on the same day as VFSS and FEES.
Power size
The power size analysis using PASS 2023 program showed that α was set to 0.05 and κ0 was set to 0.4. Except for the power size of Bolus 1 in Table 6 and Group B in Table 8, which are 0.65 and 0.73 respectively, the other sample sizes in this study are sufficient to achieve 80% power in the Kappa test.
Statistical analysis
Swallowing Function Assessment Results: Data from swallowing function assessments are analyzed using SPSS 26.0 software, with qualitative data described using numbers. The consistency between FEES and VFSS is evaluated using the Kappa test. Differences with a p-value of less than 0.05 are considered statistically significant. Sensitivity, specificity, and validity of FEES and VFSS in detecting aspiration and penetration events are calculated using each other as the gold standard (Table 1). Scores from the MDADI are described using means and standard deviations.
Taking FEES as an example, VFSS is used as the gold standard, and the sensitivity, specificity and validity of FEES detecting aspiration is calculated.
Results
Patients
There were 9 cases of horizontal partial laryngectomy, 9 cases of vertical partial laryngectomy, and 12 cases of Supra-cricoid Partial Laryngectomy (SCPL). There were 24 male and 6 female patients, with age range from 47 to 76 years and a median age of 56 years. 13 cases underwent unilateral neck lymph node dissection, while 12 cases underwent bilateral neck lymph node dissection.
MD Anderson dysphagia inventory (MDADI)
Thirty patients completed the MDADI twice postoperatively, resulting in a total of 60 assessments. According to the study by Zhang, the critical threshold for screening swallowing disorders in head and neck cancer patients with MDADI is 69 points19. In the first postoperative MDADI assessment, all patients scored < 69 points. In the second evaluation, three patients who underwent vertical partial laryngectomy scored > 69 points on MDADI,while the rest scored < 69 points, indicating the presence of swallowing disorders (Table 2). In the first assessment, the total average score of the Emotional dimension (7 items) was 1.9, Functional domain (5 items) was 2.6, and Physical domain (8 items) was 2.2. In the second assessment, the total average scores for the emotional, functional, and physiological dimensions were 2.3, 3.4, and 2.4, respectively. Scores in all three domains were relatively low, with the Emotional dimension scores beings the lowest (Table 3). Compared to the first postoperative assessment, patients who underwent vertical partial laryngectomy showed a significant increase in average scores in all dimensions in the second assessment.
Assessment of the reliability of FEES and VFSS
Using VFSS and FEES as gold standards respectively, the reliability indicators of FEES and VFSS were calculated, including sensitivity, specificity, and validity (Table 4). FEES showed good sensitivity (84%) and specificity (94%) for detecting aspiration. Similarly, VFSS also demonstrated good sensitivity (89%) and specificity (92%) for detecting aspiration. In comparison to VFSS, which had a sensitivity of 42% for detecting penetration, FEES exhibited a higher sensitivity of 78% for detecting penetration, indicating its advantage in detecting penetration.
Consistency evaluation of FEES and VFSS
Consistency tests were conducted on the overall swallowing function assessments of 30 patients using FEES and VFSS, yielding a Kappa value of 0.669 (Table 5), indicating a high level of consistency between the two. Consistency tests were also performed on boluses 1, 2, 3, and 4 separately, with Kappa values of 0.598, 0.631, 0.675, and 0.678 respectively (Table 6). It can be observed that there is a high level of consistency between the two for boluses 2, 3, and 4. However, for food item 1, there is only moderate consistency between them. Consistency tests on bolus doses of 5 ml, 10 ml, 15 ml, and 20 ml yielded Kappa values of 0.658, 0.647, 0.705, and 0.670 respectively (Table 7). It can be seen that for these four bolus volumes, there is a high level of consistency between the two, without significant differences. Consistency tests were conducted separately on patients who underwent horizontal partial laryngectomy, vertical partial laryngectomy, and supracricoid laryngectomy, yielding Kappa values of 0.572, 0.604, and 0.680 respectively (Table 8). It can be observed that there is moderate consistency between the two in patients undergoing horizontal and vertical partial laryngectomy. In patients undergoing supracricoid laryngectomy, there is a high level of consistency between the two.
Discussion
The purpose of performing partial laryngectomy on patients with laryngeal cancer is to ensure safety margins while preserving and reconstructing laryngeal function20. Swallowing function is a crucial aspect of laryngeal function. However, after partial laryngectomy, where the trachea and pharynx remain connected, there is a high risk of aspiration and penetration, leading to significant psychological and physiological impacts on patients12. Many patients may avoid eating or swallowing, affecting their social interactions and leading to feelings of inferiority, ultimately severely impacting their quality of life. Therefore, the assessment and rehabilitation of swallowing disorders in patients after partial laryngectomy deserve attention. A thorough evaluation of swallowing function can guide patients’ eating habits more effectively and provide better monitoring of rehabilitation progress. Swallowing disorders are not only common complications after partial laryngectomy but may also be exacerbated by postoperative radiotherapy21,22. Hence, it is important to explore standardized assessment methods and early intervention for swallowing function in patients after laryngeal surgery.
Currently, research on swallowing characteristics and bolus types used in relevant studies is limited, with few swallowing instances and inconsistent bolus preparation methods, often using solid foods. In this study, four types of bolus with varying consistencies were prepared using thickening agents and water during FEES, all meeting the food standards outlined in the "Chinese Expert Consensus on Dietary Nutrition Management of Swallowing Disorders (2019 Edition)" and aligning more closely with Chinese dietary habits. These boluses were prepared in 5 ml, 10 ml, 15 ml, and 20 ml volumes to reflect typical portion sizes. In cases where assessment was challenging, multiple repeated trials were conducted during FEES to better reflect patients’ daily eating conditions. In this study, we used a mixture of xanthan gum and little modified starch as thickening agents. It dissolves easily in both cold and hot water. It is user-friendly, stable, acid-resistant, alkali-resistant, enzyme-resistant, heat-resistant, and salt-resistant, maintaining bolus viscosity stability upon contact with saliva23,24,25. Moreover, FEES does not require contrast agents for imaging, thereby avoiding discomfort and allergic reactions associated with contrast agents26,27.
Both FEES and VFSS are considered gold standards for diagnosing swallowing disorders. However, determining the appropriate method for assessing swallowing function in patients after partial laryngectomy poses challenges. Currently, there is research on VFSS and FEES in patients after supraglottic laryngectomy, with limited exploration into other types of partial laryngectomy28. Some studies have indicated that FEES is superior to VFSS in detecting pharyngeal residue, penetration, and even aspiration29,30,31,32. In this study, FEES demonstrated higher sensitivity and specificity in detecting aspiration and penetration, surpassing VFSS in detecting penetration. The direct visualization during FEES using a flexible endoscope enables clearer and more sensitive detection of pharyngeal residue and penetration compared to X-ray fluoroscopy. Small amounts of material may be difficult to identify on VFSS, leading to underestimation of penetration in patients after partial laryngectomy, often categorized as normal. Studies have shown that only 7% of aspirations occur during the swallowing process33. A large-scale study on mixed-diagnosis patients reported that over 90% of aspirations occur before or after swallowing34. Evidence of aspiration is observed when swallowed bolus is expelled from the airway after swallowing. Most aspirations in patients with head and neck cancer occur after swallowing, as residues enter the pre-epiglottic space when the airway opens. If the swallowed bolus enters the lower airway from the pre-epiglottic space or leaves residue below the vocal cords after swallowing, it is considered evidence of aspiration. The consistency test of the four boluses yielded Kappa values of 0.678, 0.675, 0.631, and 0.598, indicating better agreement between the two assessments for thicker foods. Water, being thinner, flows quickly through the airway, leaving minimal traces, making detection more challenging, consistent with previous studies28,35,36. In patients after partial laryngectomy, FEES allows for direct and clear observation of the relationship between the pharynx and laryngeal structures during swallowing, providing valuable information for postoperative patients. Therefore, for early-stage patients after partial laryngectomy, FEES can to some extent replace the traditional gold standard VFSS, offering an objective assessment of swallowing function for early postoperative rehabilitation and feeding.
After vertical partial laryngectomy, patients typically experience relatively ideal recovery of swallowing function, with early resumption of eating and relatively early restoration of water intake function. However, horizontal partial laryngectomy and supracricoid partial laryngectomy notably affect patients’ swallowing function. While patients can eat postoperatively, they may experience occasional strain during swallowing, leading to the consumption of small amounts of viscous foods. Among these procedures, patients who undergo supracricoid laryngectomy exhibit the most significant recovery of swallowing function, although eating challenges may persist between 25 and 30 days postoperatively. Therefore, the impact of partial laryngectomy on swallowing function in the early postoperative period is considerable. Recovery of swallowing function in most patients after partial laryngectomy takes a longer time, primarily relying on self-exercise or natural recovery of neurological and muscular function37. Studies have indicated a slow recovery of swallowing function in patients after partial laryngectomy, with 11.9% still experiencing swallowing abnormalities up to 48 weeks postoperatively. In some cases, there may be no significant improvement in swallowing function and associated quality of life in the second year postoperatively compared to the first year12.
The results of the Anderson Dysphagia Inventory assessment show lower scores in emotional, functional, and physiological dimensions, underscoring the multifaceted impact of dysphagia on patients. This impact transcends mere physiological impairment, extending into the realms of psychological and social functioning, with the psychological ramifications being particularly salient. Research suggests that patients grappling with laryngeal cancer are prone to developing feelings of helplessness, hopelessness, anxiety, and depression, which not only negatively affect their quality of life but may also interfere with their treatment and recovery38. Within the context of this study, select patients exhibited aversion towards swallowing or reluctance to engage in swallowing activities due to overwhelming postoperative psychological distress, resulting in poorer recovery of swallowing function compared to counterparts undergoing analogous procedures. Research conducted by Zhu et al. suggests that a combined regimen of swallowing exercises and nutritional interventions holds promise in ameliorating swallowing difficulties, nutritional status, and overall quality of life among post-laryngectomy and post-radiotherapy patients39. Consequently, timely and appropriate psychological interventions alongside tailored swallowing rehabilitation programs emerge as imperative components of comprehensive patient care. Moreover, studies indicate that communication dynamics between patients can serve as a conduit for addressing swallowing-related challenges encountered by individuals undergoing partial or total partial laryngectomy40,41. And postoperative health and safety education for patients with laryngeal cancer is also necessary42.
However, this study has certain limitations. The consistency of FEES and VFSS in this cohort needs further confirmation with larger samples, especially the Bolus 1 group. Other types of partial laryngectomy procedures should be included in future studies. Due to the severe impairment of swallowing function in patients undergoing supracricoid partial laryngectomy, the follow-up time for recovery of swallowing function needs to be extended further. This study excluded severely malnourished patients and those with poor postoperative compliance (including those allowed to swallow independently but unwilling to do so). The specific relationship between these nutritional and psychological factors and the recovery of swallowing function requires further detailed investigation.
Conclusion and outlook
This study shows that dysphagia is an important problem affecting the early quality of life of patients after partial laryngectomy, including emotional, functional, physiological and other aspects, so early instrumental evaluation is extremely important. This study also emphasizes the reliability problems in the identification of false invasion and aspiration. FEES can be used to evaluate the early swallowing function of patients after partial laryngectomy, thus guiding the timing and type of eating, and evaluating the rehabilitation effect. In addition, compared with VFSS, FEES have more advantages for the identification of penetration.
Due to the anatomical changes associated with partial laryngectomy and the insufficient attention paid by clinicians to the rehabilitation of postoperative patients with swallowing disorders, the evaluation and intervention areas of swallowing disorders are still greatly underexplored in this population. FEES are helpful in evaluating all aspects of swallowing after partial laryngectomy, but further research is needed to optimize their use in this patient cohort. It is likely to become increasingly important to identify symptoms of swallowing disorders using reliable assessment tools to enable the development of appropriate interventions for patients with partial laryngectomy.
Data availability
Data supporting the findings of this study are available within the paper. Any further data are available from the corresponding author upon request.
References
Li, H. et al. Incidence and mortality of laryngeal cancer in Zhejiang cancer registry, 2000–2011. Cancer Res.. Ther. 11(Suppl 2), 155–160. https://doi.org/10.4103/0973-1482.168177 (2015).
Zhang, S. S., Xia, Q. M., Zheng, R. S. & Chen, W. Q. Laryngeal cancer incidence and mortality in China, 2010. Cancer Res Ther. 11(Suppl 2), C143–C148 (2015).
Laccourreye, O. et al. Otorhinolaryngologists’ personal treatment preferences (total laryngectomy or laryngeal preservation) when faced with advanced stage laryngealcancer. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 131, 339–343 (2014).
Wulff, N. B. et al. Health-related quality of life, dysphagia, voice problems, depression, and anxiety after total laryngectomy. Laryngoscope. 132(5), 980–988 (2022).
Nakayama, M. et al. Functional organ preservation for laryngeal cancer: Past, present and future. Jpn. J. Clin. Oncol. 42, 155–160 (2012).
Tomeh, C. & Holsinger, F. C. Laryngeal cancer. Curr. Opin. Otolaryngol. Head Neck Surg. 22, 147–153 (2014).
Alicandri-Ciufelli, M. et al. Voice and swallowing after partial laryngectomy: Factors influencing outcome. Head Neck. 35, 214–219 (2013).
Lips, M. et al. Supracricoid laryngectomy and dysphagia: A systematic literature review. Laryngoscope. 125, 2143–2156 (2015).
Langmore, S. E. History of fiberoptic endoscopic evaluation of swallowing for evaluation and management of pharyngeal dysphagia: Changes over the years. Dysphagia. 32(1), 27–38 (2017).
Costa, M. M. Videofluoroscopy: The gold standard exam for studying swallowing and its dysfunction. Arq. Gastroenterol. 47(4), 327–328 (2010).
Javorszky, S. M., Reiter, R. & Iglseder, B. Validation of a geriatric bedside swallowing screen (GEBS): Protocol of a prospective cohort study. JMIR Res. Protoc. 12, e46252 (2023).
Yang, H. et al. Investigation of swallowing function and swallowing-related quality of life after partial laryngectomy in Chinese patients with laryngeal carcinoma. Health Qual. Life Outcomes. 17(1), 132 (2019).
Gong, X. L. et al. Feasibility study of banana paste swallowing test in food intake assessment of stroke patients with dysphagia. Chin. J. Phys. Med. Rehabil. 40(10), 745–746 (2018).
Chinese consensus Group of experts on Dietary Nutrition Management of dysphagia. Chinese expert consensus on dietary nutrition management of dysphagia (version 2019). Chin. J. Phys. Med. Rehabil. 41(12), 881–888 (2019).
Cichero, J. A. et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: The IDDSI framework. Dysphagia. 32(2), 293–314 (2017).
Baijens, L. W. et al. FEES protocol derived estimates of sensi-tivity: Aspiration in dysphagic patients. Dysphagia. 29(5), 583–590 (2014).
Chen, A. Y. et al. The development and validation of a dysphagia-specific quality-of-life questionnaire for patientswith head and neck cancer: The M.D. Anderson dysphagia inventory. Arch. Otolaryngol. Head Neck Surg. 127(7), 870–876 (2001).
Zou, M. et al. Reliability and validity of the Chinese version of Anderson dysphagia scale. Chin. J. Nurs. 48(11), 1003–1007 (2013).
Zhang, L. J. Best cut-off point and value of evaluation and diagnosis for M.D. Anderson Dysphagia Inventory by ROC. J. Nurs. Admin. 18(11), 766–769 (2018).
Ahn, S. H. et al. Guidelines for the surgical management of laryngeal cancer: Korean society of thyroid-head and neck surgery. Clin. Exp. Otorhinolaryngol. 10(1), 1–43 (2017).
Brook, I. Early side effects of radiation treatment for head and neck cancer. Cancer Radiother. 25(5), 507–513 (2021).
Brook, I. Late side effects of radiation treatment for head and neck cancer. Radiat. Oncol. J. 38(2), 84–92 (2020).
Vilardell, N. et al. A comparative study between modified starch and xanthan gum thickeners in post-stroke oropharyngeal dysphagia. Dysphagia. 31(2), 169–179 (2016).
Nsengiyumva, E. M. & Alexandridis, P. Xanthan gum in aqueous solutions: Fundamentals and applications. Int. J. Biol. Macromol. 216, 583–604 (2022).
Popa Nita, S., Murith, M., Chisholm, H. & Engmann, J. Matching the rheological properties of video fluoroscopic contrast agents and thickened liquid prescriptions. Dysphagia 28, 245–252 (2013).
Pasternak, J. J. & Williamson, E. E. Clinical pharmacology, uses, and adverse reactions of iodinated contrast agents: a primer for the non-radiologist. Mayo Clin. Proc. 87(4), 390–402 (2012).
Juchem, B. C. & Almeida, M. A. Risk for adverse reaction to iodinated contrast media: A validation study. Rev. Gaucha Enferm. 38(2), e68449 (2017).
Zhong, Z. et al. A preliminary study on the assessment of swallowing function after supracricoid partial laryngectomy. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 50(2), 95–100 (2015).
Fattori, B. et al. Interjudge and intrajudge reliabilities in fiberoptic endoscopic evaluation of swallowing (Fees) using the penetration-aspiration scale: A replication study. Dysphagia. 17(4), 308–315 (2002).
Park, W. Y. et al. Adding endoscopist-directed flexible endoscopic evaluation of swallowing to the videofluoroscopic swallowing study increased the detection rates of penetration, aspiration, and pharyngeal residue. Gut Liver 9(5), 623 (2015).
Adachi, K., Umezaki, T. & Kikuchi, Y. Videoendoscopy worsens swallowing function: A videofluoroscopic study: A randomized controlled trial. Eur. Arch. Oto-Rhino-Lar-yngol. 274, 3729 (2017).
Maniaci, A. et al. Post-cere-brovascular stroke and early dysphagia assessment: A systematic review. Acta Biomed. 93(4), e2022263 (2022).
Yoon, J. A. et al. Correlations between aspiration and pharyngeal residue Scale scores for fiberoptic endoscopic evaluation and videofluoroscopy. Yonsei Med. J. 60(12), 1181 (2019).
Colodny, N. Interjudge and intrajudge reliabilities in fiberopticendoscopic evaluation of swallowing (Fees) using the penetra-tion-aspiration scale: A replication study. Dysphagia. 17(4), 308–315 (2002).
Fattori, B. et al. Comparison between videofluoroscopy, fiberoptic endoscopy and scintigraphy fordiagnosis of oro-pharyngeal dysphagia. Acta Otorhinolaryngol. Ital. 36(5), 395–402 (2016).
Park, W. Y. et al. Adding endoscopist-directed flexible endoscopic evaluation of swallowing to the video fluoroscopic swallowing study increased the detection rates of penetration, aspiration, and pharyngeal residue. Gut Liver 9(5), 623 (2015).
Philippe, Y. F. et al. Partial laryngectomy as salvage surgery after radiotherapy: oncological and functional outcomes and impact on quality of life: A retrospective study of 20 cases. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 131(1), 15–19 (2014).
Johansson, M., Rydén, A. & Finizia, C. Mental adjustment to cancer and its relation to anxiety, depression, HRQL and survival in patients with laryngeal cancer: A longitudinal study. BMC Cancer 11, 283 (2011).
Zhu, X. et al. Effect of swallowing training combined with nutritional intervention on the nutritional status and quality of life of laryngeal cancer patients with dysphagia after operation and radiotherapy. J. Oral Rehabil. 49(7), 729–733 (2022).
Zheng, Y. et al. The influence of the “patient-to-patient model” on swallowing problems in patients with supraglottic laryngeal cancer. ORL J. Otorhinolaryngol .Relat. Spec. 76(3), 171–177 (2014).
Tian, L. et al. Effect of the patient-to-patient communication model on dysphagia caused by total laryngectomy. J. Laryngol. Otol. 131(3), 253–258 (2017).
Han, J. et al. Effects of health education intervention on negative emotion and quality of life of patients with laryngeal cancer after postoperative radiotherapy. Cancer Radiother. 22(1), 1–8 (2018).
Funding
This study was funded by Ph.D. start-up Fund of Shanxi Medical University in Shanxi Province (03201628).
Author information
Authors and Affiliations
Contributions
Mrs. Lina Jia and Mr. Chenxu Yan contributed equally to this manuscript. Mrs. Lina Jia and Mr. Chenxu Yan did data collectionand wrote the main manuscript text. Mrs. Run Liu, Mr. Pengfei He and Miss. Fei Yang prepared Figs. 1–2 and did data collection. Mr. Hui Huangfu, Mrs. Sen Zhang and Mrs. Ailing Liu conducted the research.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of the First Hospital of Shanxi Medical University (No.KYLL-2023-191). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jia, L., Yan, C., Liu, R. et al. Early application value of flexible laryngoscope swallowing function assessment in patients after partial laryngectomy. Sci Rep 15, 6040 (2025). https://doi.org/10.1038/s41598-025-86799-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-86799-x