Abstract
The start of rehabilitation directly affects the effectiveness of treatment. This is a quantitative, exploratory, analytical, and cross-sectional study, with 618 Brazilian adults with spinal cord injury (SCI). Participants were predominantly male (68.90%), with a mean age of 38.04 years (SD = 9.85), with higher education (49.50%), receiving social security benefits (63.60%), and with a monthly income of up to 3 minimum wages (55.10%). The main cause of SCI was traffic accident (40.80%) and 58.70% of the participants had paraplegia. Moreover, 19.40% had not undergone any rehabilitation and the mean time to start rehabilitation after SCI was 17.68 months (SD = 38.80). Participants with the highest level of education were 4.30 times more likely to undergo rehabilitation. The results suggest that those who were more educated and with higher income also had greater access to rehabilitation programs and sought these programs earlier. In contrast, those with less resources had fewer opportunities for rehabilitation. The optimization of referral systems in the health care network, outreach programs, and a greater supply of rehabilitation centers can increase access to rehabilitation among people with SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) of traumatic or non-traumatic etiology is one of the most disabling and life-changing conditions that can affect humans. This condition causes physical, psychological, and social alterations1 and can be classified as paraplegia or quadriplegia, according to the level of the lesion2.
People with SCI invariably need rehabilitation to develop and/or recover functionality and reach the highest possible level of autonomy, social inclusion and participation3. Therefore, rehabilitation should be initiated as early as possible to minimize the functional, psychological, individual, and family-related impacts and improve the quality of life of the rehabilitated person2,4,5,6. Any delay to the start of rehabilitation negatively interferes with the effectiveness of treatment, leading to a further deterioration of the irreversible damage related to injury, and hinders the individual’s reentry into the job market7.
Therapeutic path, also referred to as therapeutic itinerary in Portuguese, is a term used to describe all the activities undertaken by people who seek treatment for a disease or seek assistance at health care services and it is always based on multiple perspectives8. The social anthropological literature uses therapeutic path to define this process9. The paths taken by individuals seeking therapeutic care do not necessarily coincide with the pathways predetermined by modern medicine or health services. The chosen path may include several subjective, individual, and collective constructs related to the process of illness and forms of treatment, further influenced by social and cultural factors, personal experiences, and the available health care services8,9,10.
For this study, therapeutic paths provided a framework against which to evaluate the effectiveness of health service networks and the guarantee of access to these services. Moreover, this framework was adopted to detect the need for educational and outreach health care programs, professional training, and the appropriateness and adaptation of service flow9. Studies on the therapeutic paths of people with disabilities (PWD) aimed at rehabilitation help identify the difficulties faced during the journey in search of health care11. They also promote the qualification of rehabilitation services in the current health care system and its service network11,12. Therefore, in this study, the priority was identification of the therapeutic path undertaken by patients with SCI in the different health care subsystems.
The main purpose was to find answers to relevant questions regarding access of people with SCI to rehabilitation services and the time elapsed from SCI onset to first exposure to rehabilitation services. Moreover, the aim of this study was to identify whether participants had access to rehabilitation and to evaluate their therapeutic path by analyzing the time elapsed between SCI and rehabilitation services (path time) while taking into account income, sex, education, and other factors.
Method
This is a quantitative study, with an exploratory, analytical, and cross-sectional design. The research project was approved by the Research Ethics Committee of the Ribeirão Preto School of Nursing at the University of São Paulo of the proponent institution, in accordance with Resolution 466/12, of the National Council for Ethics in Research of the Brazilian Ministry of Health, which addresses ethics in research with human beings, filed under protocol No. CAAE: 07814219.6.0000.5393.
Data were collected nationwide via internet. In Brazil there is no database on people with SCI as in other countries. The online questionnaire was widely disseminated by researchers from the Neurorehab research group on social media (Facebook®, Instragram®, Whatsapp® Groups, blogs and websites), with disclosures directed to groups with the research’s target audience of people interested in participating in research on spinal cord injury by the organization in general. Furthermore, the invitation via the online form was published on the profiles of the University and the research group. All participants in the present study confirmed acceptance and clarification in the informed consent form. The sample consisted of Brazilian adults with SCI with internet access. Volunteers from all over Brazil who enrolled between February and August 2018, were considered for the study. Participants who did not fully complete the online form and/or declared they were under 18 were excluded from the study for not meeting the eligibility criteria. A non-probabilistic sample was composed of the individuals who fulfilled the eligibility criteria. Participants who did not fully fill out the online questionnaire and/or reported a date of birth under 18 years of age were excluded from the study as they did not meet the eligibility criteria. The online form was initiated by 966 people, of which 618 completed it and met the eligibility criteria.
An online questionnaire developed using the SurveyMonkey® platform, validated in a previous study, was used for registration and data collection. This form consisted of 22 questions to describe the profile of participants with SCI (traumatic and non-traumatic) and their therapeutic path. The profiles followed the format adopted by the International Spinal Cord Society datasets (ISCoS)11 to enable future international comparative studies. The online questionnaire, available at https://pt.surveymonkey.com/r/JG2SKK2, was widely publicized on social media using posts directed at groups with the target audience of research and digital influencers who post content related to PWD.
Data collected was transferred directly to the software Statistical Package for the Social Sciences, version 22.0, and R, version 3.3.0.
For descriptive statistical data analysis, absolute and relative frequencies were estimated, while measures of central tendency and variability were calculated as well. To determinate the association of categorical variables income, education level, and level of injury were associated with rehabilitation (yes/no), the Fisher’s exact test was used. The Mann–Whitney test was used to evaluate the significance between the variables therapeutic path time (numerical variable) and sex (dichotomous categorical variable). The Kruskal Wallis test was used to compare origin (categorical variable) with path time (numerical variable). The associations between the variables’ origin and rehabilitation (yes/no) were determined using Pearson’s Chi-Square test. Lastly, the odds ratios (OR) were calculated using contingency tables. A significance level of 0.05 (95%) was considered.
Results
The sample consisted of 618 participants with SCI, of which 426 (68.90%) were male and 192 (31.10%) were female (Table 1). The age of participants ranged from 18 to 70 years old, with a mean of 38.04 years old (± 9.85). The mean age at the time of SCI was 28.14 years old (± 10.24). The mean time of SCI was 9.3 years (± 7.90). Regarding the region of origin, 387 (62.60%) participants were from the Southeast, 105 (17.00%) from the South, 65 (10.50%) from the Northeast, 47 (7.60%) from the Center-West, and 17 (2.30%) from the North of Brazil.
The category of non-traumatic injuries (113, 18.30%) included congenital injuries (spina bifida/myelomeningocele), infections, and neoplasms. The category of traumatic injuries (499, 80.70%) included injuries from traffic accidents, firearm and knife injuries, falls, and diving in shallow water. Six participants (1.00%) reported causes that were not classified, such as loss of movement without apparent cause. Regarding the type of SCI, 386 (62.50%) had paraplegia and 232 (37.50%) had quadriplegia.
In terms of treatment in rehabilitation centers, 80.60% (498) reported that they were undergoing treatment. However, 19.40% (120) had not yet undergone any treatment in rehabilitation centers (Fig. 1).
Regarding rehabilitation and income reported by the participants, the results revealed an association between income and whether or not they underwent rehabilitation after SCI (p ≥ 0.008, Fisher’s exact test).
The results also showed an association between education level and rehabilitation (p ≥ 0.001, Fisher’s exact test), which highlights that participants with higher education levels are more likely to undergo rehabilitation after SCI in a specialized center in neuropsychomotor rehabilitation. Moreover, participants with SCI and a higher level of education (higher education or graduate studies) were 4.3 times more likely to undergo rehabilitation than those with only high school or elementary/middle school diplomas.
According to the test, no association was found between rehabilitation and neurological level of impairment related to SCI (p ≥ 0.116, Fisher’s exact test) and with region of origin (p ≥ 0.533, Pearson’s Chi-square test).
Regarding the therapeutic path time, the time from trauma (SCI) and onset of disorder to the start of rehabilitation ranged from 0 to 316 months, with a mean of 17.68 months (± 38.80). Of these participants, 50.00% started rehabilitation on average seven months after SCI. Furthermore, 11.80% (73) of the participants were able to start rehabilitation up to one month after SCI. Regarding their characteristics, they showed a higher level of education and monthly salary income.
No statistically significant differences were observed between path time and sex (p ≥ 0.690, Mann–Whitney test), region of origin (p ≥ 0.358, Kruskal–Wallis test), and type of SCI (paraplegia or quadriplegia) (p ≥ 0.139, Kruskal–Wallis test). Education level and income were associated with path time (p ≥ 0.001, Kruskal–Wallis test).
The means and medians in Table 2 showed that the higher the education level, the shorter the time elapsed from the start of rehabilitation, that is, the shorter the therapeutic path (p ≥ 0.001, Kruskal Wallis test).
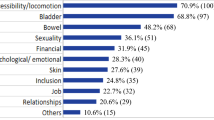
Regarding the rehabilitation centers/services, the SARAH network was the most widely used service (Fig. 2). It should be noted that specialized rehabilitation services offer services like Orthopedics, Developmental Pediatrics, Neurological Rehabilitation, Neurosurgery, Reconstructive Plastic Surgery, Neurorehabilitation in Spinal Cord Injury, Post COVID Rehabilitation, post-discharge follow-up, guidance and support groups. It should be noted that the participants could indicate more than one option since some attend more than one rehabilitation center.
Discussion
Regarding the regional distribution of the participants in this study, a representative sample of 618 people with SCI was obtained from all regions in Brazil. The predominance of males and young people with a mean age of 38 years corroborates the finding of other national and international studies13,14. The main cause of SCI was the occurrence of trauma (traffic accidents, firearm and knife injuries, falls, and diving in shallow water), which can be associated with an increase in urban violence in Brazil. In contrast, in developed countries, the main cause of SCI is falls, which is associated with an aging population11.
The evaluation of education level category showed that most of the participants had higher education, considered above the average education level of the Brazilian population. This result can be related to greater access to the Internet and information among people with higher education, which may have increased their awareness of the research. In addition, most of the participants was from the southeast region of Brazil, with the highest rates of education level and greater access to the Internet according to the National Household Sample Survey (PNAD)15.
In the 2017 continuous PNAD survey, of the 17.7 million people interviewed who did not have Internet access, 28.70% reported financial reasons and 22.00% stated they did not know how to use the Internet15.
In this study, most of the participants were able to undergo rehabilitation, even if after the optimal time, in an average of 17.6 months between SCI and the start of rehabilitation. Associated with this delay in starting rehabilitation, a considerable number (19.40%) has not even managed to visit a rehabilitation center to start treatment. In Brazil, most people with spinal cord injuries go home and receive care from public services. The time from start of rehabilitation found in this study was similar to the time reported in a study from the city of São Paulo11,16. In developed countries, patients continuously proceed with their therapeutic paths until rehabilitation, without any interruption of treatment. An Italian study showed that patients who were treated early (up to 30 days after SCI) had better functional recovery than those who took longer to start rehabilitation (SCIVOLETTO; MORGANTI; MOLINARI, 2005). Notably, several scholars emphasize the importance of early rehabilitation to minimize functional, psychological, individual, and family-related impacts and improve quality of life for the rehabilitated persons2,4,5,6,7
The findings of these studies regarding “lack of access” to rehabilitation services and the long therapeutic path time are serious and disturbing both for people with SCI and their families and for physical therapists. According to Article 26 of Decree No. 6949 of 2009 Rights of Persons with Disabilities and their Optional Protocol, countries should expand rehabilitation services and based on multidisciplinary assessments of the needs of individuals, initiate rehabilitation as early as possible, including access to devices and assistance technologies17. Although not evaluated in this study, the mood and emotions of young people with SCI when they first lose their mobility, virility, work capacity, and, consequently, their autonomy should be considered when planning for early rehabilitation treatment. Additionally, the sooner people with SCI start rehabilitation, the greater their chances of preventing and treating complications related to SCI. Moreover, they can actively return to society, including work-related activities, reestablish themselves financially, and become less dependent on social security, as well as improve their quality of life and that of their families11.
Regarding the right to rehabilitation, based on the assumptions established by Brazilian laws, Law No. 8080 of September 1990, Chapter II, Article 7, individuals must receive comprehensive care with equal rights and access to health care information18. In addition to the specialized centers, primary care networks should monitor and provide resources to assist people with SCI, thus ensuring easy access. In this regard, easy access includes care close to home for PWD and the provision of self-care training, which minimizes possible complications associated with SCI. Thus, the referral of people with SCI from emergency care to arrival at the rehabilitation center and return to the health services of their community of origin must be integrated and function as a network. It should be noted that both the hospital network and primary care can and should refer these patients to centers of greater technological complexity19. However, in reality, this network and the referral system of people with SCI to rehabilitation centers do not always work effectively.
Another relevant finding about the timing of receiving rehabilitation services and time revealed a significant association between timing of rehabilitation and education level and income. In this regard, participants with SCI and a higher level of education (higher education or graduate studies) were 4.3 times more likely to undergo rehabilitation than those with only elementary/middle or high school diplomas. The data also suggested that participants with higher incomes were more likely to be able to undergo rehabilitation after SCI. This type of association has already been identified in another Brazilian study, where participants with a higher level of education tended to seek health services more frequently because they identified the importance of health care. Also in this study, participants with higher income sought more preventive health care, while people with lower income had higher hospital admission rates. This finding suggests that people with lower incomes are more likely to seek emergency care than preventive care11,20.
The results suggest that people with SCI with higher education levels and income had more access and sought rehabilitation centers earlier. In this regard, optimized referral systems in the health care network and increased provision and outreach actions of available public rehabilitation centers would bridge this socioeconomic gap and increase access to rehabilitation by people with SCI. Furthermore, respecting the eligibility criteria for acceptance in specialized neuropsychomotor rehabilitation centers such as medical referral and diagnosis, characteristics such as level of injury, time since trauma (or not trauma) and other clinical characteristics of the person with SCI, are facilitators for faster initiation and acceptance to specialized rehabilitation services. Notably, the most widely used specialized rehabilitation centers, regardless of income and education level, were the public rehabilitation centers11.
In particular, the most widely used rehabilitation centers were those of the SARAH (46.50%) and Lucy Montoro (20.80%) networks. The SARAH network, where most of the participants sought rehabilitation, provides high quality care and nationwide coverage, with nine rehabilitation centers in the cities of Brasília, Salvador, São Luís, Belo Horizonte, Fortaleza, Rio de Janeiro, Macapá, and Belém21. The Lucy Montoro network, the second most widely sought service, has units in the capital and in the cities of the interior of the state of São Paulo, thus covering the Southeast region of Brazil, which is also the region of origin of most of the study participants13. Everyone has the right to the Unified Health System (SUS), however a small part of the population has private care, as shown in Fig. 2 of this study. The distribution of specialized centers is not homogeneous throughout Brazil. Most specialized services are found in large cities. Rehabilitation centers in Brazil are mostly distributed in specific national regions, which may cause delays and lack of access to those who do not reside in these regions. Additionally, despite the Brazilian health system being unified, there is difficulty in connecting the hospital system with rehabilitation centers, making it a challenge for the patient.
In Brazil, the protocols of care and referral to rehabilitation centers are not widely standardized, thus causing further delays to the start of rehabilitation of people with SCI. In reality, there is a shortage of rehabilitation programs in relation to the number of patients. Moreover, in the initial stage of treatment, health workers in Brazil are not appropriately trained to refer patients with SCI as soon as possible to a specialized rehabilitation center.
Study limitations
The study provides an overview of people with SCI in Brazil. One limitation of this study was online data collection, which excludes all people with SCI who do not have Internet access. However, 74.90% of the Brazilian population reportedly has Internet access and online data collection facilitates the participation of wheelchair users22. The present study was carried out by only volunteers registered on the surveymonkey platform, limiting the general panorama of people with spinal cord injuries in Brazil. Furthermore, the veracity of the information collected, as it was self-declared by the participants, could not be proven with other means of information from the participant.
The questionnaire was self-answered (by the participant himself) and the researchers did not have access to the electronic medical records, limiting access to some important variables for analysis.
Studies on therapeutic paths are relatively recent. The way people live and their life context result in a wide variety of therapeutic paths in societies9,16. Although not addressed in the present study, the influence of the social network may facilitate the use of various forms of care and its conformation may modify the therapeutic path. Previous studies have highlighted the importance of a consistent and positive network of family, neighbors, friends, and health care workers9,16,22.
Final considerations
It is emphasized that the present study is pioneering in Brazil, and was possible identified important aspects of the therapeutic path of people with spinal cord injury (SCI), such as the long time elapsed from onset to the start of rehabilitation. Almost 20.00% of the participants reported they had not yet undergone rehabilitation after SCI. The results suggest that people with SCI with higher education levels and income had greater access and sought rehabilitation centers earlier. In this regard, optimized referral systems in the health care network and increased provision and outreach actions of available public rehabilitation centers could bridge this socioeconomic gap and increase access to rehabilitation by people with SCI.
Data availability
Data Availability The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
VanDiemen, T. et al. Associations between self-efficacy and secondary health conditions in people living with spinal cord injury: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 98(12), 2566–3257 (2017).
Cardol, M. et al. Beyond disability: Perceived participation in people with a chronic disabling condition. Clin. Rehabil. 16, 27–35 (2002).
Cordeiro, A. et al. Portuguese language translation of the lower urinary tract Data Set for patients with spinal cord injury. Texto e Contex. J. 27, e5390016 (2018).
Scivoletto, G., Morganti, B. & Molinari, M. Early versus delayed inpatient spinal cord injury rehabilitation: An Italian study. Arch. Phys. Med. Rehabil. 86, 512–516 (2015).
Cheng, et al. Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home?. J. Neurotrauma 34, 2867–2876. https://doi.org/10.1089/neu.2016.4930 (2017).
– Andrade, L. T. de, Favoretto, N. B., Souza, D. R. P. de, Gimenes, F. R. E. & Faleiros, F. Diagnósticos, resultados e intervenções de enfermagem para indivíduos com lesão medular. In: PRONANDA: Programa de Atualização em Diagnósticos de Enfermagem, ciclo 6. Porto Alegre: ArtmedPanamericana (2018).
Phillips, V. L., Hunsaker, A. E. & Florence, C. S. Return to work and productive activities following a spinal cord injury: The role of income and insurance. Int. Spin. Cord Soc. 50, 623–626 (2012).
Alves, P. C. Itinerário terapêutico e os nexus de significados da doença. Revista de Ciências Sociais 42, 29–43 (2015).
Cabral, A. L. L. V., Martinez-Hemáez, A., Andrade, E. I. G. & Cherchiglia, M. L. Itinerários terapêuticos: o estado da arte da produção científica no Brasil. Ciência&SaúdeColetiva 16(11), 4433–4442 (2011).
Younes, S., Rizzotto, M. L. F. & Araújo, A. C. F. Therapeutic itinerary of patients with obesity treated in high-complexity services of a University Hospital. Saúde Debate, Rio de Janeiro 41(115), 1046–1060 (2017).
Faleiros, F. et al. Surveying people with spinal cord injuries in Brazil to ascertain research priorities. Sci. Rep. 13, 654. https://doi.org/10.1038/s41598-022-26733-7 (2023).
Siqueira, S. M. C., Jesus, V. S. & Camargo, C. L. The therapeutic itinerary in urgente/emergency pediatric situations in a maroon community. Ciência & Saúde Coletiva 21(1), 179–189 (2016).
Vasconcelos, E. C. L. & Riberto, M. Caracterização clínica e das situações de fratura de coluna vertebral no município de Ribeirão Preto, propostas para um programa de prevenção do trauma raquimedular. Coluna/Columna 10, 40–43 (2011).
Silva, G. A. D. et al. Functional assessment of people with spinal cord injury: Use of the functional independence measure—FIM. Texto & Contexto—Enfermagem 21, 929–936 (2012).
IBGE–Instituto Brasileiro de Geografia e Estatística. PNAD Contínua TIC 2017: Internet chega a três em cada quatro domicílios do país. Estatísticas Sociais, 2018. https://agenciadenoticias.ibge.gov.br/agencia-sala-de-imprensa/2013-agencia-de-noticias/releases/23445-pnad-continua-tic-2017-internet-chega-a-tres-em-cada-quatro-domicilios-do-pais.
Souza, et al. Identification of occupational roles in adapted sport athletes. Cadernos Brasileiros de Terapia Ocupacional 29, e2131 (2021).
Brasília. Convenção sobre os Direitos das Pessoas com Deficiência: Protocolo Facultativo à Convenção sobre os Direitos das Pessoas com Deficiência: Decreto Legislativo nº 186, de 09 de julho de 2008: Decreto nº 6.949, de 25 de agosto de 2009. Secretaria de Direitos Humanos, 4ª Ed. Pp: 54–55 (2010). https://www.pessoacomdeficiencia.gov.br/app/sites/default/files/publicacoes/convencaopessoascomdeficiencia.pdf.
Brasil. Lei n.8080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes, e dá outras providências. Diário Oficial da União, Brasília, DF (1990).
Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Diretrizes de Atenção à Pessoa com Lesão Medular/Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Ações Programáticas Estratégicas e Departamento de Atenção Especializada. 2. Ed, Brasília: Ministério da Saúde, 1–11 (2015).
Cambota, J. N, Rocha, F. F. Determinantes das desigualdades na utilização de serviços de Saúde: Análise para o Brasil e regiões. Pesquisa e Planejamento Econômico 45(2) (2015).
REDE SARAH. Conheça a Rede SARAH de hospitais de reabilitação. http://www.sarah.br/a-rede-sarah/
Corbo, et al. Use of the virtual environment as a strategy for disseminating information during the COVID-19 pandemic. Creat. Nurs. https://doi.org/10.1177/10784535231195482 (2023).
Author information
Authors and Affiliations
Contributions
Conceptualization, Greve, Tate and Faleiros; Methodology, Tate, Faleiros, Rabeh and Greve; Validation, Faleiros, Tate and Rabeh; Formal Analysis, Faleiros, Rabeh, Greve, Henriques, Tholl and Machado; Investigation, Faleiros and Tate; Resources, Corbo, Faleiros, Tholl and Machado; Data Curation, Faleiros and Tate; Writing—Original Draft preparation, Corbo, Machado, Faleiros and Rabeh editing—Review and editing, Corbo and Faleiros; visualization, Faleiros; supervision, Faleiros and Tate; Project administration, Faleiros; Acquisition of financing, Faleiros and Tate.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Faleiros, F., Corbo, L.N., Greve, J.M.D. et al. Therapeutic path of Brazilians with spinal cord injury until rehabilitation. Sci Rep 15, 9342 (2025). https://doi.org/10.1038/s41598-025-87022-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87022-7