Abstract
The purpose of this study was to compare preoperative anxiety and intraoperative pain between the first and second cataract surgeries in patients who underwent immediate sequential bilateral cataract surgery (ISBCS). This retrospective study was conducted between June 20, 2023, and September 20, 2023, at Korea University Guro Hospital. A total of 170 cataract surgeries was included, and 130 eyes underwent ISBCS. Clinical records, including patients’ intraoperative pain score (visual analog scale [VAS] for pain, 1–10 points) and patients’ preoperative anxiety score (VAS for anxiety (VASA), 1–10 points), were investigated. Also, correlations between clinical factors and pain scores were analyzed. The pain score did not significantly differ between the first and second surgeries in ISBCS patients (2.51 ± 1.16 vs. 2.43 ± 1.36 points) (P = 0.692). However, the anxiety score recorded before the second eye surgery was significantly lower compared to that recorded before the first eye surgery. (3.32 ± 1.68 vs. 2.31 ± 1.29 points) (P < 0.001). Among the clinical factors, only the anxiety score was significantly correlated with the pain score (P = 0.013). We suggest ISBCS may serve as a beneficial strategy for a better surgery experience, reducing patients’ anxiety during surgery.
Similar content being viewed by others
Introduction
These days, topical anesthesia is a highly preferred method among many cataract surgeons1. Compared to retrobulbar block, which was frequently administered in the past, it is cost- and time efficient2. Most importantly, topical anesthesia is not an invasive procedure, decreasing the risk of optic nerve damage and supporting quicker visual recovery1,3. However, the ability to move the eye is maintained. As a result, patient cooperation has become essential for successful surgery.
Several studies have demonstrated that patient cooperation correlates with the pain experienced4,5. In cases where the patient complains of high anxiety or is anticipated to have low cooperation level, modification of the anesthesia method could be considered5,6,7,8.
Numerous studies have compared anxiety and pain levels in sequential cataract surgery. Ługowska et al. reported patients experienced greater anxiety before their first-cataract surgery than before their second-cataract surgery9.
From the perspective of pain comparison, some studies have reported an increase in pain during the second surgery compared to the first surgery6,10, whereas others suggested that no correlation exists between the pain level and the sequence of surgeries11,12,13 (Table 1). However, in these studies, there were intervals of several days or several weeks between the sequential surgeries6,10,11,12,14. As far as we know, no study has investigated patients undergoing immediate sequential bilateral cataract surgery (ISBCS). We believed that if cataract surgeries were performed consecutively, there would be no difference in the pain scores. Therefore, In this study, we aimed to compare anxiety levels and pain scores in ISBCS patients. We also analyzed the correlations between the pain score and clinical factors.
Methods
This retrospective study was conducted at the Department of Ophthalmology at Korea University Guro Hospital. All subjects provided written informed consent. This study was approved by the Institutional Review Board of the Korea University Guro Hospital and adhered to the Declaration of Helsinki. We retrospectively investigated the medical records of 217 patients who underwent cataract surgery performed by a single surgeon (J.S.S.) between June 20, 2023, and September 20, 2023, at Korea University Guro Hospital.
Patient selection
The ISBCS group included patients who underwent cataract surgeries on both eyes back-to-back on the same day. On the other hand, the unilateral cataract surgery group included patients requiring cataract surgery on 1 eye or patients who underwent bilateral surgery with an interval of more than 1 week between the procedures.
We also further divided unilateral cataract patients into subgroups based on performance of cataract surgery on the other eye. If they had undergone surgery on the other eye, the patients were categorized into the unilateral second surgery group; if they had not undergone cataract surgery on the other eye, they were categorized into the unilateral first surgery group.
Patients with glaucoma, retinal disorder or corneal opacity were excluded. Patients were also excluded if they had high myopia with an axial length > 26 mm, which carries a risk of lens–iris diaphragm retropulsion syndrome.
15Eyes with white cataract, trauma cataract, phacodonesis, or other conditions requiring additional surgical procedures were excluded. Eyes with intraoperative complications like posterior capsule rupture were also excluded. Finally, we excluded patients who were unable to cooperate with investigations, such as those with Alzheimer’s disease or neurological disorders.
Measurements
Clinical records, including preoperative anxiety score (visual analog scale [VAS] for anxiety [VASA], 1–10 points), intraoperative pain score (VAS for pain, 1–10 points), sex, age (y), laterality of the eye, cataract nucleus grading (Lens Opacities Classification System (LOCS) III), cataract cortex grading (LOCS III), intraocular lens (IOL) diopters (D), surgery time (s), and ultrasound energy consumption during phacoemulsification (cumulative dispersed energy [CDE], units) were investigated.
Each patient’s anxiety score and pain score were measured at the operation room immediately preceding and immediately following each surgery.
Before starting the surgical draping, patients were asked their anxiety level using the VASA, which was scored from 0 points for no anxiety to 10 points for overwhelming terror. After the surgical procedure, the pain score was investigated using the VAS for pain. Likewise, this score ranged from 0 points for no pain to 10 points for unbearable pain. With ISBCS patients, before starting surgical draping for the second procedure, patients were asked about their anxiety level once more. After the second surgery, they were asked for their pain score for the second cataract surgery.
Cataract nucleus grade and cataract cortex grade were evaluated using the LOCS III, with grading ranging from 1 to 6 and 1–5, respectively.
The measurement of surgery time commenced with the initiation of corneal paracentesis and was concluded upon completion of stromal hydration.
CDE, which was measured with a phacoemulsification device (Infiniti Vision System; Alcon Laboratories, Inc., Geneva, Switzerland), was used to evaluate ultrasound energy consumption during phacoemulsification.
Surgical methods
All surgeries were performed by a single highly experienced surgeon (J.S.S.) using the same procedures under topical anesthesia of 0.5% proparacaine hydrochloride (Alcaine; Alcon Laboratories Inc., Geneva, Switzerland). During all procedures, corneal irrigation was performed with 4% lidocaine to minimize patient pain. The eyelids were washed with a povidone–iodine solution. Then, a sterile drape was applied, and the speculum was placed. After making a 2.20-mm clear corneal incision, forceps were used to create a continuous curvilinear capsulorrhexis, followed by hydrodissection. Phacoemulsification was performed via a stop and chop technique, and coaxial irrigation and aspiration were completed to remove the lens cortex. Thereafter, the folded IOL was inserted into the capsular bag through the corneal incision, which was sealed using stromal hydration.
In cases of ISBCS, each surgery was conducted as an independent procedure, ensuring complete separation of the two operations. After the first surgery, the surgical team changed gowns, gloves, and plastic surgical drapes. Subsequently, the second surgery was performed using identical procedures to those used in the initial procedure.
Additional sets of sanitized surgical equipment should be prepared for the second surgery so that the risk of bilateral endophthalmitis could be reduced. Additionally, to prevent incorrect switching of the IOLs, before starting each surgery the surgeon and assistant checked the patient’s data and IOL information.
Statistical analysis
The anxiety score and pain score were compared using the Wilcoxon singed-rank test. The clinical data, including age, nucleus grading (LOCS III), cortex grading (LOCS III), intraocular lens (IOL) diopters (D), surgery time (s), and CDE (units), were compared between the two groups using Student’s t test. Pearson’s chi-square test was used to compare the distribution of sex and laterality between the two groups. The Mann–Whitney U test was used to compare the anxiety score or pain score between ISBCS patients and those undergoing unilateral cataract surgery. Spearman’s correlation analysis was performed to analyze the correlations between clinical factors and pain scores. Then, we conducted a partial Spearman analysis on factors that exhibited significant correlations in the Spearman analysis.
Statistical analysis was performed using IBM SPSS for Windows version 21.0 (IBM Corporation, Armonk, NY, USA) and SAS 9.4 (SAS Institute, Cary, NC, USA).
P < 0.05 was considered statistically significant. Meanwhile, when the P-value was 0.05–0.1, it was described as borderline significant.
Results
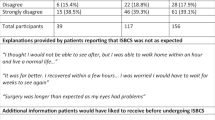
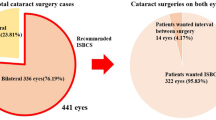
Among the 170 cases, 130 (76.47%) eyes underwent ISBCS and 40 eyes underwent unilateral cataract surgery. Among the unilateral cataract surgery patients, 13 (7.65%) had previously experienced cataract surgery on the other eye, while 27 (15.89%) had not undergone previous cataract surgery (Fig. 1).
Distribution of cataract surgery patients. A total of 170 eyes was included in the investigation, and 130 (76.47%) underwent ISBCS. Sixty eyes underwent unilateral cataract surgery; among which 13 patients (7.65%) had undergone cataract surgery on the other eye and 27 (15.89%) had no previous cataract surgery. Abbreviation: ISBCS, Immediate sequential bilateral cataract surgery.
There was no difference in the distribution of clinical factors between the first and second ISBCS surgeries, including nucleus grade (LOCS III), cortex grade (LOCS III), surgery time (s), and CDE (units) (P = 0.367, P = 0.713, P = 0.579, and P = 0.931, respectively) (Table 2). Patient anxiety scores were 3.32 ± 1.68 points before the first ISBCS surgery and 2.31 ± 1.29 points before the second ISBCS surgery, and the difference was statistically significant (P < 0.001). The pain score was also lower during the second ISBCS surgery, but the difference in scores between the first and second procedures was not significant (2.51 ± 1.16 vs. 2.43 ± 1.36, P = 0.692) (Fig. 2).
Comparison of anxiety and pain scores between the first and second ISBCS surgeries. The anxiety score was 3.32 ± 1.68 points before the first surgery and 2.31 ± 1.29 points before the second surgery, with a significant difference (P < 0.001). Separately, the pain score was 2.51 ± 1.16 points during the first surgery and 2.43 ± 1.36 points during the second surgery, with no significant difference (P = 0.692). Abbreviation: ISBCS, Immediate sequential bilateral cataract surgery. *P < 0.05 (Wilcoxon signed-rank test).
When we compared anxiety and pain scores from the first ISBCS surgery and the first unilateral surgery, they did not statistically differ (3.32 ± 1.68 vs. 2.78 ± 1.53 points, P = 0.124) (2.51 ± 1.16 vs. 2.33 ± 1.66 points, P = 0.219). Also, there was no statistical difference in either score between the second ISBCS surgery and the second unilateral surgery (2.31 ± 1.29 vs. 2.62 ± 1.61 points, P = 0.556) (2.43 ± 1.36 vs. 2.62 points, P = 0.789) (Fig. 3).
Comparison of anxiety and pain scores between ISBCS and unilateral cataract surgery patients. The anxiety and pain scores were not different between the first ISBCS and unilateral surgery. (3.32 ± 1.68 vs. 2.78 ± 1.53 points, P = 0.124) (2.51 ± 1.16 vs. 2.33 ± 1.66 points, P = 0.219). There were also no significant differences in anxiety and pain scores between the second ISBCS and unilateral surgeries (2.31 ± 1.29 vs. 2.62 ± 1.61 points, P = 0.556) (2.43 ± 1.36 vs. 2.62 points, P = 0.789) (Fig. 3). Abbreviation: ISBCS, Immediate sequential bilateral cataract surgery. Mann–Whitney U test.
By sex, the pain score was 2.13 ± 0.84 points in male patients and 2.53 ± 1.42 points in female patients, without a significant difference (P = 0.535). The pain score was also not significantly different between the right and left eyes (2.39 ± 1.19 vs. 2.45 ± 1.41 points, P = 0.833).
We analyzed the correlations between clinical factors and pain scores in 170 patients. In the Spearman correlation analysis, age (y), nucleus grade (LOCS III), surgery time, and CDE (units) showed significant correlations with the pain score (P = 0.042, P = 0.015, P = 0.042, and P = 0.011, respectively). The anxiety score showed a borderline significant correlation with the pain score (P = 0.054) (Table 3).
We conducted a Spearman partial correlation analysis involving only the factors that showed a correlation with the pain score. According to this Spearman partial correlation analysis, the anxiety score alone showed a significant correlation with the pain score (P = 0.012) (Table 4).
Discussion
During the coronavirus disease 2019 pandemic, interest in ISBCS increased16 because it requires less face-to-face contact and fewer visits, ultimately reducing societal costs and making it economically efficient17,18,19,20. Patients prefer ISBCS due to the reduced number of visits and the rapid recovery of eyesight21. In South Korea, 96% of patients in one study agreed to undergo ISBCS if they were indicated for cataract surgeries on both eyes19. Furthermore, many previous studies reported that there was no difference in postoperative complications between ISBCS and delayed sequential bilateral cataract surgery17,18,19. We also believe that ISBCS can contribute to patient satisfaction, enhancing the overall surgical experience.
In this study, ISBCS patients reported significantly decreased anxiety scores before the second surgery. This result is consistent with findings of previous studies that investigated sequential surgeries5,22,23. Fagerström et al. suggested that, after a positive experience during the first cataract surgery, patients feared the second surgery less23. Likewise, we believe that reduced patient anxiety was attributed to their experience during the first surgery, which involved less pain than expected and provided a sense of accomplishment upon completing the first surgery successfully. Several studies have demonstrated that increased anxiety is associated with more severe pain in cataract surgery4,5. Reducing anxiety might be attributed to patients’ positive experiences with cataract surgery as well as less intraoperative pain. In this study, we focused on patients without co-existing diseases. However, further studies investigating the relationship between such factors and anxiety would also be helpful.
On the other hand, many studies have documented an increase in pain during the second surgery6,7,24,25. One of these studies even demonstrated that patients reported more pain and exhibited less cooperation in the second surgery, suggesting that additional sedation could be considered in some second surgery cases7.
Ursea et al. suggested several mechanisms that might explain the increase in pain during the second surgery6. First, the previous surgery can physiologically cause sympathetic irritation, which could intensify pain stimuli during the second surgery. Second, the use of analgesic medications during the first surgery could lead to drug tolerance during the second surgery6. Third, due to psychological mechanisms, patients may perceive pain from the second experience to be more severe.
The initial two hypotheses are difficult to consider in earnest because unilateral cataract surgery does not usually cause inflammation in the other eye26.
Sympathetic ophthalmia is usually caused by severe trauma, including eyeball rupture or laceration, and rarely occurs after cataract surgery27. Additionally, the use of only a few drops of procaine or lidocaine seems to have a low possibility of inducing anesthesia tolerance in the opposite eye7.
The psychological factor is considered the most reasonable explanation. Patients tend to perceive the amount of pain as minimal if it is less than expected6,28. After the first procedure, on the other hand, patient expectation for ocular pain has decreased and they may perceive the pain to be greater than actual. Furthermore, although the duration of recall bias related to pain in cataract surgery is not precisely known, due to the intervals between the surgeries, we believe there could be a recollection error regarding the pain experienced. Similarly, Ang et al. reported that 40% of patients are more frightened after the second surgery because they could not remember the visual sensation experienced during cataract extraction29.
However, in our study, the pain score was even lower during the second procedure, though the difference was not significant.
It is possible that ISBCS patients might have overestimated the pain score of the first surgery. When a questionnaire regarding surgical pain is administered by the surgeon, patients might report a higher pain score, anticipating that the surgeon would pay more attention to the upcoming second surgery or provide additional anesthesia for better pain management.
However more importantly, we suggest that, as the interval between the ISBCS first and second surgeries is short, ISBCS patients have a relatively vivid memory of the previous surgery as the time gap between the two surgeries is not sufficient to induce recollection error. Additionally, because we investigated the perceived pain immediately after the operation, the patient might have provided a more accurate report regarding their perceived pain.
Surgeons often encounter patients who have undergone previous cataract surgery in the other eye complaining of more pronounced pain in the second surgery compared to the first. ISBCS appears to offer a solution to alleviate such concerns. We also believe that ISBCS patients who experience reduced anxiety and no change in pain would show better cooperation during the second surgery. However, as this study did not directly evaluate patient cooperation, more studies are necessary.
According to the analysis of the correlation between pain and clinical factors, preoperative anxiety was the only factor correlated with pain perception.
Although ISBCS accounted for the largest proportion of the total patients, the correlation is consistent with prior studies with intervals between sequential surgeries6,30. There has been controversy about the presence of sex-based differences in pain scores. In this study, there was no difference in pain based on sex, which was consistent with the findings of Gupta et al. and Kelly et al.31,32,33.
This study has several limitations. We did not perform a sample size calculation for statistical significance. Conducting a sample size calculation or increasing the sample size in future studies could yield more persuasive results.
We believe that the current results are associated with recall bias. Previous studies have reported that the duration of recall bias may vary depending on the type of surgery or the location of pain34,35. However, research on cataract surgery pain has not been conducted. Therefore, further research on the duration of recall bias related to cataract surgery pain should be conducted. This would be beneficial for scheduling surgeries.In conclusion, ISBCS patients reported significantly lower anxiety scores before the second cataract surgery, while their pain scores were not different between the sequential surgeries. In addition, preoperative anxiety had a positive correlation with the pain score. ISBCS may serve as a beneficial strategy for patients who expect to experience increased pain during the second surgery.
Data availability
The raw data for this study are available upon reasonable request from the corresponding author.
References
Assam, J. H., Bernhisel, A. & Lin, A. Intraoperative and postoperative pain in cataract surgery. Surv. Ophthalmol. 63 (1), 75–85 (2018).
Jacobi, P. C., Dietlein, T. S. & Jacobi, F. K. A comparative study of topical vs retrobulbar anesthesia in complicated cataract surgery. Arch. Ophthalmol. 118 (8), 1037–1043 (2000).
Zhao, L. Q. et al. Topical anesthesia versus regional anesthesia for cataract surgery: a meta-analysis of randomized controlled trials. Ophthalmology 119 (4), 659–667 (2012).
Aslan, L. et al. The pain experience and cooperation of patients in consecutive cataract surgery. Eur. J. Ophthalmol. 23 (3), 339–343 (2013).
Omulecki, W., Laudanska-Olszewska, I. & Synder, A. Factors affecting patient cooperation and level of pain perception during phacoemulsification in topical and intracameral anesthesia. Eur. J. Ophthalmol. 19 (6), 977–983 (2009).
Ursea, R. et al. Pain perception in sequential cataract surgery: comparison of first and second procedures. J. Cataract Refract. Surg. 37 (6), 1009–1014 (2011).
Akkaya, S., Ozkurt, Y. B., Aksoy, S. & Kokcen, H. K. Differences in pain experience and cooperation between consecutive surgeries in patients undergoing phacoemulsification. Int. Ophthalmol. 37 (3), 545–552 (2017).
Liu, P. et al. Factors affecting pain in patients undergoing bilateral cataract surgery. Int. Ophthalmol. 40 (2), 297–303 (2020).
Lugowska, D., Konopinska, J., Mariak, Z. & Obuchowska, I. Comparison of subjective preoperative experiences of patients before first- or Second-Eye Cataract surgeries. Clin. Ophthalmol. 14, 2883–2889 (2020).
Adatia, F. A. et al. Documenting the subjective patient experience of first versus second cataract surgery. J. Cataract Refract. Surg. 41 (1), 116–121 (2015).
Bardocci, A. et al. Pain during second eye cataract surgery under topical anesthesia: an intraindividual study. Graefes Arch. Clin. Exp. Ophthalmol. 249 (10), 1511–1514 (2011).
Sharma, N. S. et al. Patient perceptions of second eye clear corneal cataract surgery using assisted topical anaesthesia. Eye (Lond). 22 (4), 547–550 (2008).
Hari-Kovacs, A., Lovas, P., Facsko, A. & Crate, I. D. Is second eye phacoemulsification really more painful? Wien Klin. Wochenschr. 124 (15–16), 516–519 (2012).
Obuchowska, I. & Konopinska, J. Fear and anxiety Associated with cataract surgery under local anesthesia in adults: a systematic review. Psychol. Res. Behav. Manag. 14, 781–793 (2021).
Wilbrandt, H. R. & Wilbrandt, T. H. Pathogenesis and management of the lens-iris diaphragm retropulsion syndrome during phacoemulsification. J. Cataract Refract. Surg. 20 (1), 48–53 (1994).
Bhalla, J. S., Zakai, M. U. & Mehtani, A. Immediate sequential bilateral cataract surgery and its relevance in COVID-19 era. Indian J. Ophthalmol. 69 (6), 1587–1591 (2021).
Lundstrom, M., Albrecht, S., Nilsson, M. & Astrom, B. Benefit to patients of bilateral same-day cataract extraction: randomized clinical study. J. Cataract Refract. Surg. 32 (5), 826–830 (2006).
Arshinoff, S. A. Same-day cataract surgery should be the standard of care for patients with bilateral visually significant cataract. Surv. Ophthalmol. 57 (6), 574–579 (2012).
Hong, S. et al. Comparisons of outcomes and complications of immediate sequential bilateral cataract surgery and unilateral cataract surgery in a tertiary hospital in South Korea. Sci. Rep. 12 (1), 22382 (2022).
Dmuchowska, D. A., Obuchowska, I. & Konopinska, J. Immediate versus delayed sequential bilateral cataract surgery. Lancet 401 (10392), 1907–1909 (2023).
Obuchowska, I., Micun, Z., Mlynarczyk. M, et al. Pros and cons of Immediate Sequential bilateral cataract surgery from a patient perspective: a Survey. Int. J. Environ. Res. Public. Health 20(2), (2023).
Pager, C. K. Randomised controlled trial of preoperative information to improve satisfaction with cataract surgery. Br. J. Ophthalmol. 89 (1), 10–13 (2005).
Fagerstrom, R. Fear of a cataract operation in aged persons. Psychol. Rep. 72 (3 Pt 2), 1339–1346 (1993).
Tan, C. S. et al. Analgesic effect of supplemental intracameral lidocaine during phacoemulsification under topical anaesthesia: a randomised controlled trial. Br. J. Ophthalmol. 95 (6), 837–841 (2011).
Jiang, L. et al. Perceived Pain during cataract surgery with topical anesthesia: a comparison between First-Eye and Second-Eye surgery. J. Ophthalmol. 2015, 383456 (2015).
El Rami, H., Fadlallah, A., Fahd, D. & Fahed, S. Patient-perceived pain during laser in situ keratomileusis: comparison of fellow eyes. J. Cataract Refract. Surg. 38 (3), 453–457 (2012).
Bondok, M. S. et al. Incidence of sympathetic ophthalmia after intraocular surgery: a systematic review and Meta-analysis. Ophthalmology 131 (7), 836–844 (2024).
Pud, D., Golan, Y. & Pesta, R. Hand dominancy–a feature affecting sensitivity to pain. Neurosci. Lett. 467 (3), 237–240 (2009).
Ang, C. L. et al. Patients’ expectation and experience of visual sensations during phacoemulsification under topical anaesthesia. Eye (Lond). 21 (9), 1162–1167 (2007).
Socea, S. D. et al. Preoperative anxiety levels and Pain during cataract surgery. Curr. Eye Res. 45 (4), 471–476 (2020).
Gupta, S. K., Kumar, A. & Agarwal, S. Cataract surgery under topical anesthesia: gender-based study of pain experience. Oman J. Ophthalmol. 3 (3), 140–144 (2010).
Johnston, R. L. et al. Topical versus peribulbar anesthesia, without sedation, for clear corneal phacoemulsification. J. Cataract Refract. Surg. 24 (3), 407–410 (1998).
Kelly, A. M. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad. Emerg. Med. 5 (11), 1086–1090 (1998).
Zwaans, W. A. R. et al. Recall bias in pain scores evaluating abdominal wall and groin pain surgery. Hernia 27 (1), 41–54 (2023).
Middel, B. et al. Recall bias did not affect perceived magnitude of change in health-related functional status. J. Clin. Epidemiol. 59 (5), 503–511 (2006).
Acknowledgements
This research was supported by the Korea Environment Industry & Technology Institute (KEITI) through the Core Technology Development Project for Environmental Diseases Prevention and Management funded by the Korean Ministry of Environment (MOE) (2022003310001). The funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
JSS was involved in the conception and design of the study. SJH was involved in data collection and the literature research. SJH was involved in the interpretation and critical revision of the article. JSS, HMS, SJH, DHK, EYS, and WJK were involved in the data analysis and drafting of the manuscript. SJH, HMS, DHK, EYS, WJK, and JSS were involved in the final approval of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hong, S., Shin, H., Kim, W. et al. Analysis of anxiety and pain in patients undergoing immediate sequential bilateral cataract surgery or unilateral cataract surgery. Sci Rep 15, 3971 (2025). https://doi.org/10.1038/s41598-025-87359-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87359-z