Drinking is a common unhealthy behaviour among youth smokers aged 25 or below. However, the effects of drinking on smoking cessation outcomes are not well understood. This study aimed to explore the impact of drinking on smoking cessation outcomes among Hong Kong Chinese youth smokers who received smoking cessation counselling. This study adopted a cross-sectional design at the Youth Quitline, which is the only government-funded hotline providing telephone smoking cessation counselling to Hong Kong smokers aged 25 or younger. Of the 142 participants at the six-month follow-up, 75 were in the drinking group and 67 in the non-drinking group. Multiple logistic regression analyses were performed to identify any significant differences in self-reported quit rates, smoking reduction by at least 50%, quit attempts, and biochemically validated quit rates between the drinking and non-drinking groups. The results showed a significant difference in self-reported quit rate between the two groups at 6-month, but no significant difference in smoking reduction by at least 50%, quit attempts, and biochemically validated quit rate. Alcohol drinking and male were identified as significant factors decreasing self-reported quit rate at 6 months. The study revealed that drinking could decrease quit rates among young smokers who received counselling, but not their smoking reduction or quit attempts. Given the negative impact of drinking on smoking abstinence and the increased popularity of drinking among the youth, assessment of alcohol use and brief advice on smoking are recommended to be an integral part of smoking cessation counselling for youth smokers.
Similar content being viewed by others
Introduction
Smoking is the most preventable cause of mortality and morbidities1. According to World Health Organizations (WHO), one in two smokers are killed by smoking-related diseases, such as lung cancer, chronic obstructive pulmonary disease, heart disease, stroke and asthma2. Recent evidence also indicated that two in every three smokers who smoked at very young ages died in diseases attributable to smoking3. Smoking is considered to be a paediatric pandemic4. Previous studies in the West have showed that approximately 30% of college students are current smokers5,6. A recent survey conducted by Centers for Disease Control and Prevention (2022) also revealed that 13.4% of high school students were current users of tobacco products in 20217. When compared to the statistics from western countries, the problem of youth smoking appears to be a less serious problem in Hong Kong, with the prevalence of 1.2% among secondary 1 to 6 students in 20218. However, the prevalence of ever smokers among Hong Kong secondary 1 to 6 students in 2021 was 7.4%, reflecting that there were still a significant amount of youth experimenting with smoking8. The average age when youth aged between 12 and 25 years first experiment with nicotine products was 14.5 years9. The most common type of nicotine products used in Hong Kong youth are conventional cigarettes, e-cigarettes and heated tobacco products10. Smokers who start smoking in adolescence are likely to continue this habit in adulthood11, resulting in chronic diseases that bring tremendous cost to the healthcare system12. Hence, providing assistance for youth smokers to quit smoking is of paramount importance to tackle this serious public health issue.
Apart from smoking, drinking is another unhealthy behaviour which usually co-occur in smokers, especially among the youth13. When compared with non-smokers, smokers are three time more likely to drink excessively14. Drinking itself is known to be associated with many chronic diseases, including high blood pressure, multiple types of cancer, particularly gastro-oesophageal cancer and liver cancer, liver cirrhosis, impaired memory and cognition and poor psychological conditions, such as increased anxiety and depressive symptoms15,16,17. Excessive alcohol use can result in numerous consequences, such as impaired cognitive function, disrupted sleep, delayed puberty, increased risk of accidents and poor academic performance in youth18. Indeed, co-occurrence of smoking and drinking can lead to multiplicative health risks, resulting a deadly consequences19. As indicated by World Health Organization, 8.5 million people are killed by both smoking and drinking annually20. The multiplicative health risks associated with both smoking and drinking are similarly observed in youth. In a cohort study of 5873 individuals, adolescents who reported concurrent use of cigarettes and alcohol were found to have high rates of deviant behaviours and violent, and had a higher likelihood to develop substance use problems than those who reported drinking but without a smoking habit21.
Despite the aforementioned multiplicative health risks, drinking can also bring detrimental impact on the smoking cessation process22, especially when the alcohol consumption level is moderate to high23. In a smoking cessation study of 1504 smokers with the mean age of 44.7 years, drinking was found to reduce the cessation rate in binge drinkers, while the difficulty in smoking cessation for non-frequent drinkers was more related to tobacco dependence24. In a population study of 2115 adults, heavy drinkers were found to be less likely to quit smoking. Even they attempted to quit, they were less likely to succeed in smoking cessation than non-heavy drinkers which included lifetime abstainers, quitters, and light and moderate drinkers22. Besides, from a convenience sample of data from 923 adults in a smoking cessation program, moderate drinkers were found to have the same likelihood as heavy drinkers to continue smoking after receiving smoking cessation advice from a website23. Consequently, these studies suggested a potential dose-response relationship between alcohol consumption and smoking outcomes in adults. The relationship between alcohol drinking and smoking has also been explored in adolescents and young adults. In a secondary data analysis of 775 adolescents who participated in a study examining the effectiveness of a text messaging-based intervention, a lower alcohol assumption was found to predict smoking abstinence25. Similar findings were also found in a US national survey of 74,836 adolescents and young adults. Particularly, past-year smokers were shown to drink in higher quantities than never-smokers. Besides, in a cross-sectional survey of a representative sample of 1321 secondary school students, drinkers were three times more likely than non-drinkers, while smokers were two times more likely than non-smokers to drink26.
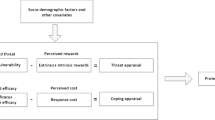
There are some hypotheses addressing the negative impact of drinking on smoking cessation. For example, it is postulated that tobacco and alcohol are often used in conjunction, and hence they are associated with each other based on classical conditioning in which the use of one substance can trigger the use of another substance (i.e., smoking triggers drinking, or vice versa)27. Another postulation is that drinking can impair people’s cognition and thus reduce their self-control to restrain them to engage in smoking, precipitating lapse and relapse27. One more postulation is about self-medication in which both alcohol and nicotine are suggested to have anxiety reducing and antidepressant effects. Hence, people tend to smoke and drink together to achieve a greater effect to control anxiety and depression28. However, these three hypotheses have not yet been tested in previous studies with adults and youth.
Despite ample evidence have indicated the association between smoking and drinking in adults and adolescents, they did not specifically examine the impact of drinking on various smoking cessation outcomes, including self-reported and biochemically validated quit rates as well as smoking reduction and quit attempts. Likewise, previous literature has indicated that the association between smoking and drinking is more prominent among younger adolescents than in other age group25,26, which may be because adolescents are more likely to be co-users than other age groups29. Thus, it limited the generalizability of existing findings in adults to youth smokers. To address the gap in existing literature, we aimed to explore the impact of drinking on smoking cessation outcomes including self-reported and biochemically validated quit rates, smoking reduction by at least 50% and quit attempts among Hong Kong Chinese youth smokers who received smoking cessation counselling.
Methods
Study design and setting
A cross-sectional design was adopted in the Youth Quitline, which is the only government-funded hotline to provide telephone smoking cessation counselling for youth smokers aged 25 or below in Hong Kong. Telephone counselling on smoking cessation was given at baseline, 1-week, 1-, 3-, 6-, 9-, and 12-month follow-ups.
Sample size calculation
The sample size was calculated based on the following formula, n = (Zα/2+Zβ)2· (P0(1–P0) + P1(1– P1))/(P0–P1)2, where n is the minimum sample size, Zα/2 is the Z-value for the desired significance level (1.96 for α = 0.05), Zβ is the Z-value for the desired power (1.28 for 90% power), P0 and P1 are the proportions of successful smoking cessation in the non-drinking and drinking groups, respectively30. According to a previous European study of smoking cessation among adolescents, 62.4% of the non-drinkers successfully quit smoking while 32.7% of the drinkers successfully quit smoking31. We thus adopted 0.624 for P0 and 0.327 for P1 in this study. The minimum sample size for this study was 110, with 55 participants in each group.
Subjects
A caller would be eligible for the Quitline service if (i) he or she was an ethnic Chinese male or female; (ii) he or she was age 25 or below; (iii) he or she smoked at least one cigarette (including all types of tobacco products available on the market, such as shisha and electronic cigarettes) in the past 30 days, which is the definition of current smokers adopted by the Hong Kong government32 and various smoking-related studies33,34; (iv) he or she could communicate in Cantonese; and (v) he or she had verbally consented to join the Quitline service. However, callers would not be eligible for the service if they were (i) physically or mentally unable to communicate or (ii) participating in existing smoking cessation programs.
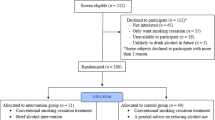
During 1st December 2020 to 28th February 2022, the Youth Quitline received a total of 5,255 calls. 91.4% (n = 4,802/5,255) was proactive call, followed by incoming call, 7.7% (n = 404/5,255) and 0.9% (n = 49/5,255) referred calls. 94.5% (n = 4,967/5,255) of the calls were relevant to smoking cessation. The remaining was irrelevant calls which included wrong numbers, promotion, sought help other than smoking cessation, asking for interview, system checking and tricks. Of these relevant calls, 99.4% (n = 4,937/4,967) were from smokers and 0.6% (n = 30/4,967) were from their family members, friends, and helping professionals. Among the smokers, 46.7% (n = 2,306/4,937) were eligible for the Quitline service, and 27.7% (n = 638/2306) agreed to join the service. Of those who have joined the service, 37.6% (n = 240/638) have received telephone counselling at 6 months and completed the corresponding questionnaire. Hence, they were included in the study.
According to the study’s purpose, the included participants were classified into two groups, namely non-drinking group and drinking group, based on their self-reported drinking status at 6-month follow-up. The reason of choosing this time point was that the participants might change their drinking behaviours between the period from baseline to 6-month follow-up. For example, participants who were drinkers might quit drinking after baseline which in turns increased the likelihood to quit smoking at 6-month follow-up, while those who did not drink alcohol at baseline might subsequently drink alcohol and reduced the likelihood in quitting smoking at 6 months. Using the drinking status at baseline might not be the best to reflect the participants’ drinking status, which in turns affected the estimation of the association between smoking cessation outcomes and alcohol drinking. Hence, instead of using the drinking status at baseline for group classification, the drinking status reported at 6 months was used. Also, abstinence measured at 6 months is the Russell standard for evaluation in smoking cessation studies35. There is no consensus on a specific timepoint that should be used for evaluation on drinking behaviours. However, in one of our systematic review and meta-analysis of psychological interventions on alcohol use disorder in adolescents and young adults, 6-month follow-up is the most commonly used timepoint for evaluation36.
Participants were classified into drinking group if they reported to consume one or more alcoholic drink on ≥ 1 days per month37, and vice versa. In this study, 75 participants were classified into the drinking group, while 67 were in the non-drinking group.
Smoking cessation intervention
The peer counsellors provided telephone-based smoking cessation counselling to the participants38. The intervention was based on the ‘5 A’ approach which has been widely advocated by World Health Organization in the field39. In particular, the counsellors1 Asked about tobacco use2, Advised the participants to quit3, Assessed their willingness to quit4, Assisted in their quitting attempt and5 Arranged for follow-up.
At baseline, the peer counsellors evaluated the amount of nicotine dependence, past quit attempts, stage of readiness to quit, and level of self-efficacy to quit smoking among the participants. The stage of readiness to quit was defined according to the Transtheoretical model40. In the model, behavioural change can be divided into five different stages, including precontemplation stage, contemplation stage, preparation stage, and action and maintenance stages. When applying this model into the smoking context, pre-contemplation refers to people who are not intend to quit smoking within the next six months; contemplation refers to people who intend to quit smoking within the next six months; preparation refers to people who intend to quit smoking within the next 30 days and make at least one quit attempt in previous year; action refers to people who are now quitting smoking and maintenance refers to people who quit smoking for more than six months40. Using a risk communication strategy, the peer counsellors then described the health implications of active and passive smoking as well as the benefits of quitting. The counsellors also assisted youth smokers in identifying unhealthy lifestyle characteristics, such as excessive drinking and lack of physical exercise. For youth smokers who engaged in unhealthy activities (e.g., drinking) to manage stress, the counsellors would first correct their misunderstanding and educate them on effective stress management strategies. The counsellors would emphasize the need of regular exercise to preserve good health and reduce stress. Based on the information gathered over the telephone, the counsellors created tailored cessation plans for each participant before the conclusion of the baseline counselling session. The cessation plan contained a quit date, a short-term objective, such as a decrease in the amount of cigarettes smoked for individuals who did not want to quit immediately, counselling for dealing with withdrawal symptoms using the Wisconsin Smoking Withdrawal Scale41, and adopting a healthy lifestyle, and a quit date. However, the content might vary from person to person after taking into account the smokers’ stage of readiness to quit, their nicotine dependency and facilitators and barriers in quitting. Importantly, engaging peer counsellors is intended to improve the individuals’ self-efficacy to stop smoking by boosting their perceived competence in dealing with high-risk circumstances, hence decreasing the likelihood of relapse38,42. Particularly, the peer counsellors could serve as a role model and share how they refused smoking temptations in their daily lives38,42. The evidence shows that this strategy is beneficial in assisting smokers to quit38.
There were six telephone follow-ups (1 week, 1, 3, 6, 9 and 12 months) to monitor on smoking cessation after the first counselling session. During these follow-up calls, the peer counsellors evaluated the severity of the participants’ withdrawal symptoms, provided them with tools for preventing relapse, and assisted them in establishing and maintaining a smoke-free lifestyle.
Multiple strategies were used to safeguard the intervention quality. Firstly, all peer counsellors were Year 3 nursing students who possessed basic counselling skills and medical knowledge to communicate with smokers. Secondly, they must complete a 2-day training organized by the research team and passed both written and oral assessments before serving as peer counsellors in the Quitline. Thirdly, all telephone counselling was audio-recorded and reviewed by a registered nurse with 5 years of experience in smoking cessation counselling. Fourthly, peer counsellors were required to complete a self-evaluation form after each counselling38. The effectiveness of the Youth Quitline was evaluated retrospectively on 1684 youth smokers who received telephone counselling between August 2005 and August 2015. The quit rate at 6-month follow-up was 23.6%; 16.9% of the smokers reduced their cigarette consumption by 50% or more at 6 months. This supported the use of peer counsellors and the effectiveness of our training35.
Outcomes
The primary outcomes of this study were the self-reported quit rates (7-day point prevalence) at 6-month follow-up. Biochemically validated quit rate could be a more accurate measure than self-reported quit rate which is subjected to social desirability bias43. However, this study was conducted in the pandemic which made biochemical validation to be very difficult due to social distancing measure. Also, the SRNT Subcommittee on Biochemical Verification conducted a meta-analysis and found that, using a complete-case approach, only 12.9% of outcome comparisons showed that treatment outcome was affected by biochemical verification43. This supported the accuracy of self-reported quit rate despite the social desirability bias. The secondary outcomes included (1) biochemically validated quit rate at 6 months; (2) rates of smoking reduction by at least 50% at 6 months; (3) rates of having a quit attempt at 6 months. These measures were chosen as secondary outcomes because previous literature indicated that they are closely related to self-reported quit rate44,45, and are good indicators to reflect the quitting behaviour44,45.
Data collection
This project was approved by the Institutional Review Board of the Hong Kong Polytechnic University (Reference number: HSEARS2020111800). Verbal consent was obtained from the participants. Data collection was done at baseline, 1 week, 1, 3, and 6, 9 and 12 months. Since we adopted the Russell standard for evaluation, only the data obtained at baseline and at 6 month was used in data analysis35. Data collected at other timepoints were used by counsellors to develop and adjust the cessation plan with participants. Before providing the smoking cessation counselling intervention via telephone, our peer counsellors assessed the smoking profile of the participants using a structured questionnaire which was developed by the research team. The questionnaire covered 6 areas, including1 smoking history2, readiness to quit by stages of change3, self-efficacy in quitting4, nicotine dependency by Fagerström Test5, lifestyle behaviours, and6 demographics38. The nicotine dependency measured by the Fagerström Test has a good construct reliability coefficient (0.74)46, and the readiness to quit by stages of change has moderate test-retest reliability (0.57) and good predictive validity for smoking behavior change47. All smokers were invited to self-report their frequency and amount of alcohol drinking in the past 30 days. In addition, they were also invited to indicate what kind of alcoholic drinks, e.g., beer and wine have been consumed. Concerning self-efficacy of quitting smoking, it is defined as a smoker’s confidence towards his/her own ability to refrain from smoking when facing external and/or internal stimuli48. This can be assessed in terms of their perceived importance, confidence, and difficulty towards quitting smoking38. For lifestyle behaviors, we only assessed the frequency of physical activities. The participants who reported no smoking in the past 7 days at 6- month follow-up were invited for biochemical validation which contained a carbon monoxide (CO) breathing test and a salivary cotinine test. For the breathing test, each participant was instructed to take a deep breath in and hold for 10–15 s, and then blow out into a mouthpiece of a Smokerlyzer to empty the lungs once the beep countdown was completed. Concerning the salivary test, it was done by an iScreen OFD Cotinine Saliva Test Device. Each participant was asked to insert the sponge of the device into the mouth and soak the sponge with oral fluid by swabbing the inside of the mouth and tongue. The participant can take out the sponge after three minutes, or until the sponge was saturated. The sponge was then put into the screening device, with the colour line shown to indicate the result. Their abstinence was confirmed by saliva cotinine level ≤ 10ng/ml and a carbon monoxide level in expired air ≤ 4 parts per million (p.p.m.)49,50.
Data analysis
The Statistical Package for Social Science (SPSS: Version 26; SPSS Inc., Chicago, IL, USA) for Windows was employed to analyse the data. Descriptive statistics were used to report the baseline and 6-month characteristics of the participants, as well as the primary and secondary outcomes, including self-reported and biochemically validated quit rates, rates of smoking reduction by 50%, and rates of having a quit attempt. The primary and secondary were all measured as binary outcomes, i.e., yes or no. Lifestyle factors at baseline and 6 months were also reported by descriptive statistics. Chi-square tests were used to examine any statistically significant difference in 6-month characteristics between drinking and non-drinking groups. Prior to conducting the analysis, we verified that the assumptions of the Chi-square test were met, ensuring that the expected value of cells was 5 or greater in at least 80% of the cells. In cases where these assumptions were not met, Fisher’s Exact Test was used as an alternative. Age, sex, marital status, employment, educational level, frequency of physical activities, total counselling points, nicotine dependency, previous quit attempts, and intention to quit were covariates. Univariate logistic regression was first used to determine the relationship between covariates and smoking cessation outcomes. Drinkers or not and covariates with a p value ≤ 0.15 in the univariate analysis were entered into the multivariate logistic regression analysis to determine any statistically significant difference in the primary outcome51, i.e. self-reported quit rate at 6-month follow-up, and in the secondary outcomes, including smoking reduction ≥ and 50%, quit attempts at 6 months between drinking and non-drinking groups, after controlling the covariates that were significant in univariate analysis. We chose a p-value threshold of 0.15 for including covariates in multivariate regression models to balance inclusivity and exclusivity51. This widely recommended threshold helps maintain a parsimonious model, reducing the risk of overfitting51. The Hosmer-Lemeshow test was used to assess how well the logistic regression model fits the observed data52. A high p-value (typically > 0.05) from the Hosmer-Lemeshow test suggests that the model fits the data well, meaning there is no significant difference between observed and expected frequencies52. However, multiple logistic regression was not performed on biochemically validated quit rate at 6 months because only 8.5% (n = 12) of our participants were biochemically verified to quit smoking. Hence, we failed to achieve the minimal number of observations for the logistic regression. The principle of intention-to-treat was adopted. Participants who were lost to follow-up, did not complete biochemical validations, or withdrew from the study were considered as having no change in smoking (i.e. no quitting or reduction).
Results
Table 1 presents the demographic characteristics and the smoking characteristics of our participants. Participants were between 12 and 25 years, with a mean age of 20.70 [Standard Deviation (SD) = 2.96]. Of them, 76.1% (n = 108) were male, 97.9% (n = 139) were either single or divorced, 57.0% (n = 81) were full-time students, and 48.6% (n = 69) were at the bachelor level or above. The mean total received counselling points were 4.93 (SD = 0.31). Among the participants, 67 were in non-drinking group and 75 were in drinking group according to their drinking status at 6 month. Regarding the drinking group, 84.0% (n = 63) reported 1–5 glasses of beer/wine per week. Comparability statistics showed that the drinking group and non-drinking group were similar in terms of the aforementioned demographic characteristics. Of the participants, 46.5% (n = 66) started to smoke at the age of 15–18, 54.9% (n = 78) smoked for 1–3 years, 73.2% (n = 104) smoked more than 20 cigarettes per day, 68.3% (n = 97) had mild nicotine dependency by Fagerström test, 67.7% (n = 84) made 1–3 times of quit attempts before joining the Quitline service, 66.2% (n = 94) intended to quit, and 37.3% (n = 53) are at the preparation stage to quit smoking. The participants in drinking group and those in non-drinking group were comparable in terms of these smoking characteristics at baseline.
Table 2 shows the comparison of different smoking cessation outcomes between the drinking group and non-drinking group at 6 months. The results of chi-square tests showed that the drinking group had a statistically significantly higher self-reported quit rate than the non-drinking group at 6-month follow-up (x2 = 6.793, p = 0.009). However, no significant difference was observed between the two groups in terms of smoking reduction by at least 50%, quit attempts as well as biochemically validated quit rate at 6 months.
Table 3 shows the results of multivariate logistic regression analysis on cessation outcomes at 6-month follow-up. In the univariate analysis of self-reported quit, sex, educational level, frequency of physical activities, nicotine dependency were covariates with p value < 0.15. After controlling for these covariates, drinking was found to be statistically significantly factors predicting self-reported quit rate at 6 months in the multivariate model (Adjusted odds ratio = 3.791, 95% CI = 1.438–9.994%). The Hosmer-Lemeshow test indicated a good fit (χ2 = 12.147, p = 0.145), suggesting that the logistic regression model of self-reported quit adequately fits the data.
In the univariate analysis of smoking reduction, covariates including sex, frequency of physical activities, nicotine dependency, previous quit attempts showed p value < 0.15. After adjusting for these covariates in the multivariate model, drinking was found not to be statistically significantly factor predicting smoking reduction at 6 months (Adjusted odds ratio = 2.186, 95% CI = 0.883–5.410%). The Hosmer-Lemeshow test demonstrated a good fit for the model, with χ2 = 4.162 and p = 0.842.
In the univariate analysis of quit attempt ≥ 24 h, covariates including frequency of physical activities, previous quit attempts demonstrated p value below 0.15. Subsequent adjustments for these covariates in the multivariate model revealed that drinking was not a statistically significant factor in predicting quit attempts at 6 months (Adjusted odds ratio = 0.851, 95% CI = 0.308–2.353%). The logistic regression model was assessed using the Hosmer-Lemeshow test, which showed a good fit (χ2 = 4.017, p = 0.674).
Discussion
Ample evidence shows that drinking is associated with smoking13,22. However, little is known about how drinking may impact on different cessation outcomes in the context of youth. This study addressed the gap in existing literature by examining the impact of drinking on various cessation outcomes, including self-reported and biochemically validated quit rates, smoking reduction and quit attempts among Hong Kong Chinese youth smokers who had received smoking cessation counselling.
Our statistical analysis revealed that the drinking and non-drinking groups were not statistically different in terms of smoking reduction and quit attempts at 6-month follow-up. However, in the multivariate logistic regression, the two groups were different in self-reported quit rate, with the non-drinking group reporting 1.7 times more likely than the drinking group to achieve abstinence at 6 months. These results implied that drinking may not pose a negative impact on people’s quit attempts and their reduction of cigarette consumption, but precipitate smoking lapse and relapse throughout the quitting process, eventually lowering people’s chance of success in achieving abstinence. While there may not be a conclusive mechanism to explain the association between smoking and drinking, there are potential mechanisms that have been explored. Our results appear to support an existing postulation that alcohol can lower people inhibition of smoking thus creating an inducing environment for smoking lapse and relapse53,54. Likewise, classic conditioning of associating smoking with drinking can also be a reason to increase the chance of smoking lapse and relapse55,56.
One thing warranting our attention is that drinking was able to significantly reduce the self-reported quit rate at 6 months among youth smokers despite the consumption of alcohol was at a low level. This is supported by the fact that a majority of our smokers who were drinkers reported that they have only drunk 1–5 glasses of beer and/or wine per week. This finding was inconsistent with available evidence on adult smokers from the West22,24 that only moderate and heavy drinking bought a detrimental impact on smoking cessation, but not mild drinking. A possible explanation is that all our participants were youth smokers aged 25 or below, with lower daily cigarette consumption and nicotine dependency when compared to adult smokers57, and thus a low level of alcohol consumption could bring a significant impact on their smoking cessation process. While for adult smokers, their quitting process is more dependent on nicotine addiction due to their longer smoking history and higher daily cigarette consumption58. Hence, the impact of drinking on smoking cessation will only be apparent if the alcohol consumption is moderate and high23. Our finding also concurs with the World Health Organization’s conclusions based on a recent report published in the Lancet which found no safe level of alcohol consumption59. The report included 694 data sources of individuals and population-level alcohol consumption, along with 592 prospective and retrospective studies on the risk of alcohol use59. Based on the analysis, alcohol was found to be the seventh leading risk factor for mortality and disability-adjusted life years in 2016, contributing to 2.2% and 6.8% of age-standardized death in females and males, respectively59. For the population aged 15–19 years, the leading causes of death attributed to alcohol use included tuberculosis, road injuries and self-harm59. For the population group aged 50 or older, cancer was the most leading cause of death attributed to alcohol use59. Previous literature which supported a persistent protective effect for some low or moderate levels of alcohol consumption on all-cause mortality were subjected to several limitations, including small sample sizes, inadequate control for confounders, and non-optimal choices of a reference category for calculating relative risks59. This report addressed these limitations by including multiple data sources and calculating the weighted attributable risk, and found that alcohol use, regardless of amount, leads to health loss across populations59. Given the negative impact of drinking on smoking cessation among youth smokers and the increased popularity of drinking during COVID-19 pandemic, they should always be advised to completely stop drinking during their quitting process. Also, assessment of alcohol use and brief advice on drinking should be incorporated in the smoking cessation counselling to increase their quit rate. One potential challenge for implementation is that smokers may not understand and even be aware of the impact of drinking on smoking cessation; and hence cannot see the relevancy of these assessment and advice, especially when the smokers are receiving telephone counselling from a smoking cessation hotline. To overcome this challenge, counsellors have to clearly inform the smokers the impact of drinking on smoking cessation, i.e., reduced chance of success and smoking relapse, when the smokers are engaged to develop a quit plan, enhancing their understanding of the relevancy. Another challenge for implementation is that including the assessment and advice on drinking can lengthen the counselling, reducing the acceptability of smokers. In view of this issue, we consider the application of a very brief intervention for drinking developed from evidence-based practices. One of the options can be FRAME which is acronym standing for Feedback, Responsibility, Advice, Menu of options, Empathy and Self-efficacy. This brief intervention has been widely tested in different populations for drinking behaviours60,61, and was found to be very effective to promote abstinence in alcohol use60,61. Importantly, this intervention is brief which can be completed within ten minutes. This improves the feasibility of integrating this intervention into the current smoking cessation counselling with high acceptability from smokers in the hotline.
Despite a higher self-reported quit rate was observed in participants who were non-drinkers at 6-month follow-up, there was no statistically significantly different in biochemically validated quit rate between the drinking and non-drinking groups at 6 month in the logistic regression. A possible reason is that not many participants have joined the biochemical validation, resulting in a type II error. This is particularly true when our data was collected during COVID-19 pandemic, and hence the infection risk associated with biochemical validation might hinder participants’ motivation to join biochemical validation. This is supported by the fact that the participation rate of biochemical validation has been greatly improved to 18.5% post-pandemic when compared to only 8.2% in pandemic.
Participants who reported that the higher frequencies of physical activities reported the higher likelihood of quit attempts and self-reported quit rate. These findings align with the growing body of literature suggesting a positive correlation between physical activity and successful cessation outcomes62,63. The mechanisms underlying this relationship could include the role of physical activity in reducing withdrawal symptoms, improving mood, and providing a healthy distraction from cravings62,63.
Our study further stratified participants based on the frequency of physical activity, revealing that low, moderate and high frequencies of activity were associated with higher success rates in quitting. This suggests that the benefits of physical activity in smoking cessation are not limited to high-intensity exercises but can also be achieved through more accessible moderate or low-frequency activities. These findings highlight the potential benefits of engaging in regular physical activity as part of a smoking cessation strategy. The flexibility in the frequencies of physical activities that can aid in quitting smoking is particularly relevant for younger populations, who may have varying levels of access to resources and different preferences for physical activity.
For participants with mild nicotine dependency (scores 0–3), they were significantly more likely to report having quit smoking compared to those with severe dependency. This result suggests that lower levels of nicotine dependency may facilitate successful quitting, likely due to less intense withdrawal symptoms and cravings64, making the cessation process more manageable. This finding highlights the importance of assessing nicotine dependency levels when designing smoking cessation interventions. Tailored strategies that address the specific needs and challenges of individuals with varying levels of dependency could enhance the effectiveness of cessation programs. For those with severe dependency, more intensive support, such as pharmacotherapy or behavioral counselling, may be necessary to increase the likelihood of successful quitting.
Participants with a history of attempting to quit smoking were significantly more likely to reduce their cigarette consumption compared to those who have never tried. This suggests that previous quit attempts may be a critical factor in motivating individuals to cut down on smoking. Those who have tried to quit before may have a stronger intrinsic motivation to change their habits. Despite the smokers are unable to quit smoking, the experience of quit attempt can reinforce their commitment to reduce smoking which is a crucial step toward eventual cessation. These findings highlight the importance of encouraging smokers to make quit attempts, even if they are not immediately successful. Each attempt can build valuable motivation for future efforts to reduce or quit smoking. Smoking cessation programs should emphasize the benefits of persistence and provide support for individuals to learn from past attempts.
Strengths and limitations
The major strength of this study lies in the originality of the research question. For the limitations, the first was that this study was conducted on the data obtained from a smoking cessation hotline. Hence, our participants were more motivated to quit smoking which in turns limited the generalizability of our findings to those community smokers who are less motivated to quit. To address this limitation, future studies are recommended to include community smokers. The second was that although some of our smoking participants were also drinker, we did not know whether they engaged these two behaviours at the same time and venue, or at different time and venue. Thus, the hypothesis that drinking is a situational factor predisposing lapse and relapse couldn’t be fully confirmed. Ecological instantaneous assessment involves repeated, real-time assessments of phenomena based on mobile technology is a possible option to overcome this limitation65. Thirdly, we did not use any validated measures for alcohol use, e.g., AUDIT, CAGE and NIAAA to assess the participants’ drinking behavior. This is because the subject recruitment was done in the hotline for smoking cessation in which these validated measures for alcohol use were not incorporated. We understand that this might affect the reliability and validity in categorizing the participants, despite the international standard was used in the classification66. Additionally, there was a possibility of underreporting of drinking data via a self-reported mean due to social desirability bias. To address this limitation, future studies should consider using both validated self-reported and objective alcohol consumption measurements to capture drinking behaviours. Fourthly, drinking amounts among the drinking group greatly varied, affecting the precision of the estimates. Fifthly, different threshold choices for p-value in univariate analysis might influence which covariates are included in the multivariate models and, consequently, the results. It is suggested that future studies should explore the sensitivity of the findings to the threshold selection. Sixthly, self-reported quit rate might be subjected to social desirability bias, affecting the accuracy of the results.
Conclusion
Drinking and smoking are unhealthy behaviours that usually co-occur. This study bridged the gap in existing literature by showing that drinking could reduce quit rate for young smokers who had received smoking cessation counselling, but not their smoking reduction and quit attempts. These results appeared to support the hypothesis that drinking creates an environment inducing smoking lapse and relapse. Given the negative impact of drinking on smoking abstinence and the increased popularity of drinking among the youth in COVID-19 pandemic, assessment of alcohol use and brief advice on smoking are recommended to be an integral part of smoking cessation counselling for youth smokers who are likely to engage in these two unhealthy behaviours. To enhance the perceived relevancy of the assessment and brief advice on drinking for smokers, counsellors have to take the lead to clearly inform them the impact of drinking on smoking cessation, i.e., reduced chance of success and smoking relapse, when the smokers are engaged to develop a quit plan. Another challenge for implementation is the time issue for additional assessment and intervention, a well-known and effective brief approach, i.e., FRAME can be adopted. The FRAME can be usually completed within 10 min, thus improving the feasibility of integrating it into the current smoking cessation counselling with high acceptability from smokers.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Chan, K. H. et al. Tobacco smoking and risks of more than 470 diseases in China: a prospective cohort study. Lancet Public. Health. 7(12), e1014–e26 (2022).
WHO. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package (World Health Organization, 2008).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13(1), 1–10 (2015).
Lando, H. A. et al. Tobacco is a global paediatric concern. SciELO Public. Health 2–A (2010).
Abuse, S. Results from the 2005 national survey on drug use and health: national findings. http://www.oas.samhsa.gov/nsduh/2k5nsduh/2k5Results.pdf (2006).
Lenk, K. et al. Cigarette use among young adults: comparisons between 2-year college students, 4-year college students, and those not in college. J. Am. Coll. Health. 60(4), 303–308 (2012).
Gentzke, A. S. et al. Tobacco product use and associated factors among middle and high school students—national youth tobacco survey, United States, 2021. MMWR Surveill. Summar. 71(5), 1 (2022).
Wong, A. H. L. Moving Hong Kong towards a tobacco-free generation: rebutting counter arguments. Lancet Reg. Health West. Pac. 45, 101064 (2024).
Villanti, A. C. et al. Flavored tobacco product use in youth and adults: findings from the first wave of the PATH study (2013–2014). Am. J. Prev. Med. 53(2), 139–151 (2017).
Wang, L. et al. Use patterns of cigarettes and alternative tobacco products and socioeconomic correlates in Hong Kong secondary school students. Sci. Rep. 11(1), 17253 (2021).
Lydon, D. M., Wilson, S. J., Child, A. & Geier, C. F. Adolescent brain maturation and smoking: what we know and where we’re headed. Neurosci. Biobehav. Rev. 45, 323–342 (2014).
Hu, T. et al. Childhood/adolescent smoking and adult smoking and cessation: the international childhood cardiovascular cohort (i3C) consortium. J. Am. Heart Assoc. 9(7), e014381 (2020).
Nakaseko, E., Kotera, S. & Nakazawa, M. Factors Associated with Smoking and drinking among early adolescents in Vanuatu: a cross-sectional study of adolescents and their parents. Int. J. Environ. Res. Public. Health 17, 22 (2020).
Szinay, D., Tombor, I., Garnett, C., Boyt, N. & West, R. Associations between self-esteem and smoking and excessive alcohol consumption in the UK: a cross-sectional study using the BBC UK Lab database. Addict. Behav. Rep. 10, 100229 (2019).
Dumitrescu, R. G. Alcohol-induced epigenetic changes in cancer. Cancer Epigenet. Precision Med. 2018, 157–172 (2018).
Iranpour, A. & Nakhaee, N. A review of alcohol-related Harms: a recent update. Addict. Health 11(2), 129–137 (2019).
Anker, J. J. & Kushner, M. G. Co-occurring alcohol use disorder and anxiety: bridging psychiatric, psychological, and neurobiological perspectives. Alcohol Res. Curr. Rev. 40, 1 (2019).
Lees, B., Meredith, L. R., Kirkland, A. E., Bryant, B. E. & Squeglia, L. M. Effect of alcohol use on the adolescent brain and behavior. Pharmacol. Biochem. Behav. 192, 172906 (2020).
Hurley, L. L., Taylor, R. E. & Tizabi, Y. Positive and negative effects of alcohol and nicotine and their interactions: a mechanistic review. Neurotox. Res. 21(1), 57–69 (2012).
WHO. Global Status Report on Alcohol and Health 2018 (World Health Organization, 2019).
Orlando, M., Tucker, J. S., Ellickson, P. L. & Klein, D. J. Concurrent use of alcohol and cigarettes from adolescence to young adulthood: an examination of developmental trajectories and outcomes. Subst. Use Misuse 40(8), 1051–1069 (2005).
Zimmerman, R. S., Warheit, G. J., Ulbrich, P. M. & Auth, J. B. The relationship between alcohol use and attempts and success at smoking cessation. Addict. Behav. 15(3), 197–207 (1990).
Lynch, K. L., Twesten, J. E., Stern, A. & Augustson, E. M. Level of alcohol consumption and successful smoking cessation. Nicotine Tob. Res. 21(8), 1058–1064 (2019).
Cook, J. W. et al. Relations of alcohol consumption with smoking cessation milestones and tobacco dependence. J. Consult. Clin. Psychol. 80(6), 1075 (2012).
Haug, S., Schaub, M. P. & Schmid, H. Predictors of adolescent smoking cessation and smoking reduction. Patient Educ. Couns. 95(3), 378–383 (2014).
Faeh, D., Viswanathan, B., Chiolero, A., Warren, W. & Bovet, P. Clustering of smoking, alcohol drinking and cannabis use in adolescents in a rapidly developing country. BMC Public. Health 6, 1–8 (2006).
Lisha, N. E., Carmody, T. P., Humfleet, G. L. & Delucchi, K. L. Reciprocal effects of alcohol and nicotine in smoking cessation treatment studies. Addict. Behav. 39(3), 637–643 (2014).
Little, H. J. Behavioral mechanisms underlying the link between smoking and drinking. Alcohol Res. Health 24(4), 215 (2000).
Ho, K. Y. et al. Exploratory study on the relationship between smoking and other risk behaviours among young smokers. J. Clin. Nurs. 27(13–14), 2859–2867 (2018).
Fleiss, J. L., Levin, B. & Paik, M. C. Statistical Methods for Rates and Proportions (Wiley, 2013).
Mertens, A. E. J. et al. Smoking cessation among adolescents in Europe: the role of school policy and programmes. Drug Alcohol Depend. 227, 108945 (2021).
Wong, A. H. Moving Hong Kong towards a tobacco-free generation: rebutting counter arguments. Lancet Reg. Health–Western Pac. 45, 859 (2024).
Jiang, N., Ho, S. Y., Wang, M. P., Leung, L. T. & Lam, T. H. Exclusive and concurrent use of cigarettes and alternative tobacco products among Hong Kong adolescents. Tob. Prev. Cessat. 4, 19 (2018).
Ho, K. Y. et al. An integrated smoking cessation and alcohol intervention among Hong Kong Chinese young people: study protocol for a feasibility randomized controlled trial. PLoS One 18(8), e0289633 (2023).
Li, W. H. C. et al. An evaluation of the Youth Quitline Service Young Hong Kong Smokers. J. Adolesc. Health. 60(5), 584–591 (2017).
Belay, G. M. et al. Psychosocial treatment options for adolescents and young adults with alcohol use disorder: systematic review and meta-analysis. Front. Public. Health 12, 1371497 (2024).
Esser, M. B. Current and binge drinking among high school students—United States, 1991–2015. MMWR Morbid. Mortal. Wkly. Rep. 2017, 66 (2017).
Ho, K. et al. Utilization of the Youth Quitline as an opportunity for an undergraduate nursing students to deliver smoking cessation counseling as their clinical placement: an implementation of a service-learning model. Nurse Educ. Today. 112, 105330 (2022).
WHO. Toolkit for Delivering the 5A’s and 5R’s Brief Tobacco Interventions to TB Patients in Primary care (WHO [Internet], 2014).
Fidanci, I., Ozturk, O. & Unal, M. Transtheoretic model in smoking cessation. J. Exp. Clin. Med. 34(1), 9–13 (2017).
Smith, S. S. et al. Revision of the Wisconsin Smoking Withdrawal Scale: development of brief and long forms. Psychol. Assess. 33(3), 255–266 (2021).
Dickerson, F. B. et al. The use of peer mentors to enhance a smoking cessation intervention for persons with serious mental illnesses. Psychiatr. Rehabil. J. 39(1), 5–13 (2016).
SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine Tob. Res. 4(2), 149–159 (2002).
Cheung, Y. T. D. et al. Physicians’ very brief (30-sec) intervention for smoking cessation on 13 671 smokers in China: a pragmatic randomized controlled trial. Addiction 116(5), 1172–1185 (2021).
Hartmann-Boyce, J. et al. Behavioural interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst. Rev. 1(1), Cd013229 (2021).
Huang, C-L., Lin, H-H. & Wang, H-H. The psychometric properties of the Chinese version of the Fagerstrom test for nicotine dependence. Addict. Behav. 31(12), 2324–2327 (2006).
Miskimins, K., Kaufmann, A. & Haaga, D. A. Comparative analysis of alternate measures of readiness to quit smoking: stages of change and the contemplation ladder. Subst. Abuse Rehabil. 2023, 167–171 (2023).
Al Thani, M. et al. Factors associated with baseline smoking self-efficacy among male Qatari residents enrolled in a quit smoking study. PLoS One. 17(1), e0263306 (2022).
Li, W. H. C. et al. Effectiveness of a brief self-determination theory-based smoking Cessation intervention for smokers at Emergency Departments in Hong Kong: a Randomized Clinical Trial. JAMA Intern. Med. 180(2), 206–214 (2020).
Ho, K. Y. et al. Comparison of two approaches in achieving smoking abstinence among patients in an outpatient clinic: a phase 2 randomized controlled trial. Patient Educ. Couns. 101(5), 885–893 (2018).
Hosmer, D. W. Jr, Lemeshow, S. & Sturdivant, R. X. Applied Logistic Regression (Wiley, 2013).
Fagerland, M. W. & Hosmer, D. W. Tests for goodness of fit in ordinal logistic regression models. J. Stat. Comput. Simul. 86(17), 3398–3418 (2016).
Shiffman, S. Relapse following smoking cessation: a situational analysis. J. Consult. Clin. Psychol. 50(1), 71 (1982).
Shiffman, S., Paty, J. A., Kassel, J. D., Gnys, M. & Zettler-Segal, M. Smoking behavior and smoking history of tobacco chippers. Exp. Clin. Psychopharmacol. 2(2), 126 (1994).
Abrams, D. B. et al. Smoking and treatment outcome for alcoholics: effects on coping skills, urge to drink, and drinking rates. Behav. Ther. 23(2), 283–297 (1992).
Niaura, R. S. et al. Relevance of cue reactivity to understanding alcohol and smoking relapse. J. Abnorm. Psychol. 97(2), 133 (1988).
Hammond, D. Smoking behaviour among young adults: beyond youth prevention. Tob. Control 14(3), 181–185 (2005).
Schoberberger, R., Böhm, G. & Schroeder, Y. Heavy dependent nicotine smokers–newfound lifestyle appreciation after quitting successfully. Experiences from inpatient smoking cessation therapy. Public. Health 129(5), 539–544 (2015).
Burton, R. & Sheron, N. No level of alcohol consumption improves health. Lancet 392(10152), 987–988 (2018).
Mattoo, S. K., Prasad, S. & Ghosh, A. Brief intervention in substance use disorders. Indian J. Psychiatry 60(Suppl 4), S466–s72 (2018).
Rodgers, C. Brief interventions for alcohol and other drug use. Aust Prescr. 41(4), 117–121 (2018).
Blank, M. D. et al. Physical activity and quit motivation moderators of adolescent smoking reduction. Am. J. Health Behav. 41(4), 419–427 (2017).
Taylor, A. H. et al. Motivational support intervention to reduce smoking and increase physical activity in smokers not ready to quit: the TARS RCT. Health Technol. Assess. 27(4), 1–277 (2023).
Lin, H., Chen, M., Yun, Q., Zhang, L. & Chang, C. Tobacco dependence affects determinants related to quitting intention and behaviour. Sci. Rep. 11(1), 20202 (2021).
Ram, N., Brinberg, M., Pincus, A. L. & Conroy, D. E. The questionable ecological validity of ecological momentary assessment: considerations for design and analysis. Res. Hum. Dev. 14(3), 253–270 (2017).
Nicholson, H. L. & Ford, J. A. Correlates of prescription opioid misuse among black adults: findings from the 2015 National Survey on Drug Use and Health. Drug Alcohol Depend. 186, 264–267 (2018).
Acknowledgements
We thank the participants for spending their time in this study.
Funding
This study was funded by the Department of Health, HKSAR, Ref.: LM (4) to DH TACO/7-10/5PT.5.
Author information
Authors and Affiliations
Contributions
HKY carried out the whole conception and design. HKY and LWK accounted for the drafting of the paper. LQ, MT, FNY, and GB were responsible for the analysis and interpretation of the data. Also, WST and MYW conducted revising it critically for intellectual content. All authors approved all aspects of the final work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of The Hong Kong Polytechnic University, with approval number HSEARS20201118001, which strictly adhere to the Declaration of Helsinki (https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/). The informed consent of all participants was verbally obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ho, K.Y., Lam, K.K.W., Liu, Q. et al. The impact of drinking on smoking cessation outcomes among Hong Kong Chinese youth smokers. Sci Rep 15, 3161 (2025). https://doi.org/10.1038/s41598-025-87391-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87391-z