Abstract
Intra-patient variability in immunosuppressive blood drug concentrations is a potential biomarker in managing organ transplant patients. However, the association between the time in therapeutic range of tacrolimus blood concentrations and its efficacy in preventing graft-versus-host disease remains unknown. In this study, we analyzed the relationship between the time in therapeutic range of tacrolimus blood concentrations and its efficacy in acute graft-versus-host disease prophylaxis in patients undergoing allogeneic hematopoietic stem cell transplantation. Eligible patients administered tacrolimus were categorized into two groups based on the grade of acute graft-versus-host disease, and propensity score matching was performed using graft-versus-host disease prophylaxis protocols and days to the disease onset to compare time in therapeutic range. In patients with tacrolimus blood concentration therapeutic range ≥ 10 ng/mL, time in therapeutic range during the first 4 weeks post-transplantation was significantly lower in the Grade II–III than in the Grade 0–I group. Among propensity score matching-extracted patients, the Grade II–III group had significantly lower time in therapeutic range during the first 2 and 4 weeks post-transplantation. Our results suggest that high time in therapeutic range early post-transplantation, particularly within 4 weeks, may avert the severity of acute graft-versus-host disease.
Similar content being viewed by others
Introduction
Hematopoietic stem cell transplantation (HSCT) is used to treat blood and hemopoietic tissue abnormalities, such as hematologic cancers. Despite its effectiveness, some patients experience graft-versus-host disease (GVHD) after allogeneic transplantation, which remains a major cause of non-relapse mortality. Effective GVHD prevention is essential for successful allogeneic HSCT outcomes. As acute GVHD is mainly mediated by effector T cells, prevention strategies have focused on suppressing T cells in the recipient1. Calcineurin inhibitors, such as tacrolimus and cyclosporine, inhibit T-cell proliferation and activation and have been used in combination with methotrexate or mycophenolate mofetil (MMF) as standard prophylaxis in human leukocyte antigen (HLA)-matched HSCT1. The introduction of post-transplantation cyclophosphamide (PTCy), combined with tacrolimus, in haploidentical transplants represented a breakthrough, enabling safe and effective HLA-mismatched transplants1.
Tacrolimus is a macrolide immunosuppressant whose immunosuppressive activity is mediated by forming a complex with FKBP12, which binds to calcineurin, inhibiting its activity2,3. Correlations between blood tacrolimus concentrations and its clinical efficacy and toxicity as a GVHD prophylactic have been reported4. However, the therapeutic range of blood tacrolimus concentrations is narrow, and tacrolimus pharmacokinetics vary widely among individuals5,6,7. Furthermore, post-HSCT, patients experience various physiological changes that affect tacrolimus pharmacokinetics8,9,10. Therefore, therapeutic drug monitoring is necessary for tacrolimus use.
Recently, intra-patient variability (IPV) in immunosuppressive drug concentrations has emerged as a potential novel biomarker for managing organ transplant patients11. IPV is a measure of the variability of immunosuppressive drug concentrations in a given patient over time, as opposed to inter-patient variability. Several approaches for assessing IPV have been proposed, the most common being the coefficient of variation of trough concentrations of immunosuppressive drugs11. Standard deviations and time in therapeutic range (TTR) have been used less frequently. Nevertheless, several recent studies have reported on the association between the TTR of tacrolimus blood concentration and the efficacy of tacrolimus in inhibiting rejection post-organ transplantation12,13,14,15,16,17. Davis et al. suggest that relying solely on the coefficient of variation to identify patients at risk for poor prognosis in renal transplant patients may lead to misclassification18. In addition, they report that the risk previously attributed to tacrolimus IPV is more likely because of low TTR rather than the coefficient of variation. In other words, the IPV that should be monitored to avoid immunologic disadvantage in patients is TTR18.
However, the association between the TTR of tacrolimus blood concentration and its efficacy in preventing GVHD in the HSCT field is yet to be reported. If a relationship exists between the TTR of tacrolimus blood concentrations and GVHD prophylaxis, it should serve as a novel indicator for controlling tacrolimus blood concentrations post-HSCT. Therefore, this study aimed to analyze the relationship between the TTR of tacrolimus blood concentrations and acute GVHD prophylaxis in allogeneic HSCT recipients to establish a new concept for managing tacrolimus blood concentrations post-HSCT in the recipients.
Results
All episodes
Patient characteristics
This study recorded 80 transplant episodes, with 69 Grade 0–I and 11 Grade II–III episodes. Grade IV GVHD was not observed at the time of initial diagnosis post-transplantation. Table 1 presents the characteristics of patients and the TTR of tacrolimus blood concentrations in each group. Sex, age, body weight, height, clinical laboratory data, GVHD prophylaxis, transplant conditions, and disease diagnosis did not significantly differ between both groups. Patients with non-malignant diseases, such as adrenoleukodystrophy, were also included in this study. Since these patients received the same conditioning regimen and GVHD prophylaxis as those with malignant diseases, their GVHD risk was considered equivalent to that of patients with malignant diseases. The GVHD-developed organs (P < 0.001) and their grades (P < 0.001) differed significantly between both groups, which was caused by GVHD grade grouping. The number of days to GVHD onset was significantly lower in the Grade II–III group than in the Grade 0-I group (P = 0.032).
TTR of tacrolimus blood concentrations
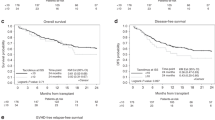
When the therapeutic range of tacrolimus blood concentrations was ≥ 10 ng/mL, TTR (TTR10) during the first 2 and 8 weeks post-transplantation did not significantly differ between the two groups (Table 1). TTR10 during the first 4 weeks post-transplantation was significantly lower in the Grade II–III group than in the Grade 0–I group (Table 1, P = 0.049). When the therapeutic range of tacrolimus blood concentrations was ≥ 12 ng/mL, TTR (TTR12) was not significantly different between the two groups at any time (Table 1). Receiver operating characteristic analysis revealed a cut-off value of 75.9% (AUC, 0.686; specificity, 0.884; sensitivity, 0.545) for TTR10 during the first 4 weeks post-transplantation, considering acute GVHD (Grade II–III) development (Fig. 1A). All episodes were again classified into two groups based on the TTR10 cut-off value, resulting in a significantly higher frequency (Fig. 1B, P = 0.003) and cumulative incidence (Fig. 2, P < 0.001) of acute GVHD (Grade II–III) development in the TTR ≤ 75.9% episode group compared with the TTR > 75.9% episode group.
Receiver operating characteristic curve (A) for determining the cut-off value of TTR10 during the first 4 weeks post-transplantation associated with acute GVHD (Grade II–III) development in all transplant episodes. Acute GVHD (Grade II–III) frequency (B) in two groups was categorized based on the TTR10 cut-off value from all transplant episodes. GVHD, graft-versus-host disease; TTR10, time in the therapeutic range at a tacrolimus concentration of ≥ 10 ng/mL.
TTR10 during the first 4 weeks post-transplantation-based comparison of cumulative incidence of acute GVHD (Grade II–III) during the observation period in all transplant episodes. Solid (n = 14) and dotted lines (n = 66) indicate the Kaplan–Meier curve of the TTR10 ≦ 75.9% and 75.9%< TTR10 groups, respectively. GVHD, graft-versus-host disease; TTR10, time in the therapeutic range at a tacrolimus concentration of ≥ 10 ng/mL.
Propensity score-matched episodes
Patient characteristics
Sixteen transplant episodes were recorded, with eight Grade 0–I and eight Grade II–III episodes. The distribution of propensity scores was very similar between the two groups (Supplementary Fig. 1). Table 2 presents patient characteristics and the TTR of tacrolimus blood concentrations in each group. No significant differences were observed in sex, age, body weight, height, clinical laboratory data, GVHD prophylaxis, transplant conditions, GVHD-developed organs, days to GVHD onset (Supplementary Fig. 2), and disease diagnosis between the groups. However, GVHD grades differed significantly between the groups (P < 0.001), which was caused by GVHD grade grouping.
TTR of tacrolimus blood concentrations
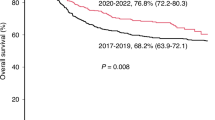
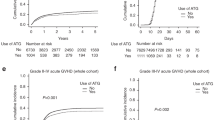
With a therapeutic range of tacrolimus blood concentrations set at ≥ 10 ng/mL, the TTR (TTR10) during the first 8 weeks post-transplantation did not significantly differ between the two groups (Table 2). TTR10 during the first 2 (P = 0.043) and 4 (P = 0.044) weeks post-transplantation was significantly lower in the Grade II–III group than in the Grade 0–I group (Table 2). When the therapeutic range of tacrolimus blood concentrations was ≥ 12 ng/mL, the TTR (TTR12) between the two groups did not significantly differ at any time (Table 2). Using receiver operating characteristic analysis, cut-off values of 83.3% (AUC, 0.789; specificity, 0.875; sensitivity, 0.750; Fig. 3A) and 89.7% (AUC, 0.805; specificity, 0.750; sensitivity, 0.875, Fig. 4A) were determined for TTR10 during the first 2 and 4 weeks post-transplantation, respectively, considering acute GVHD (Grade II–III) development. Propensity score matching (PSM) episodes were again classified into two groups based on the TTR10 cut-off value during the first 2 and 4 weeks post-transplantation, resulting in a significantly higher frequency of acute GVHD (Grade II–III) development in the TTR ≤ 83.3% (Fig. 3B, P = 0.041) and TTR ≤ 89.7% (Fig. 4B, P = 0.041) episode groups, respectively, compared with that of the episode group with a TTR greater than the cut-off value.
Receiver operating characteristic curve (A) for determining the cut-off value of TTR10 during the first 2 weeks post-transplantation associated with acute GVHD (Grade II–III) development in PSM episodes. Acute GVHD (Grade II–III) frequency (B) in two groups classified based on the TTR10 cut-off value from PSM episodes. GVHD, graft-versus-host disease; TTR10, time in the therapeutic range at a tacrolimus concentration of ≥ 10 ng/mL; PSM, propensity score matching.
Receiver operating characteristic curve (A) for determining the cut-off value of TTR10 during the first 4 weeks post-transplantation associated with acute GVHD (Grade II–III) development in PSM episodes. Acute GVHD (Grade II–III) frequency (B) in two groups classified based on the TTR10 cut-off value from PSM episodes. GVHD, graft-versus-host disease; TTR10, time in the therapeutic range at a tacrolimus concentration of ≥ 10 ng/mL; PSM, propensity score matching.
Discussion
This study showed that a high TTR can improve the prophylactic effect of tacrolimus in preventing acute GVHD after HSCT. The results provide a meaningful new concept for all healthcare professionals involved in managing tacrolimus blood concentrations in patients undergoing HSCT. This concept suggests that the rate at which target blood concentrations are achieved during a particular period determines the clinical outcome of the patient.
Traditionally, for immunosuppressive drugs whose pharmacological effects correlate with blood concentrations, target blood concentrations at a certain point or for a specific period have been considered19,20,21,22. Similarly, in GVHD prophylaxis with tacrolimus after HSCT, the target blood concentration values have been reported and used as indicators of treatment strategy efficacy in routine clinical practice. Ram et al.23 showed that a mean tacrolimus blood concentration > 10 ng/mL in the second week post-transplantation effectively prevented Grade III–IV acute GVHD. In addition, Genetskey et al.24 showed that mean tacrolimus blood concentrations < 12 ng/mL were predictive of Grade II–IV acute GVHD development, although this was limited to the first week post-transplantation. Hagen et al.25. set a target tacrolimus blood concentration of 10–15 ng/mL and reported that a tacrolimus trough value < 5 ng/dL was predictive of acute GVHD in the third or fourth week post-transplantation. They also reported that the risk of acute GVHD was lowest in patients who maintained trough levels of 10–15 ng/mL in the first 4 weeks post-transplantation25. Our results suggested that the tacrolimus blood concentration for the TTR should be ≥ 10 ng/mL, and the TTR should be maintained in the first 4 weeks post-transplantation. Our findings and those reported by Hagen et al.25. mutually supported the assessment conditions. Thus, improving the maintenance of tacrolimus blood concentrations at effective levels could further improve its efficacy in preventing acute GVHD. In contrast, TTR12 was not significantly associated with severe acute GVHD prophylaxis at any evaluation period, despite the target tacrolimus concentration during the initial induction phase being 12–15 ng/mL. In other words, we believe that a tacrolimus blood concentration of ≥ 12 ng/mL is effective but not necessarily required as a maintenance level for TTR.
PSM was employed to eliminate the bias in GVHD prophylaxis protocols between Grades 0–I and II–III groups, as well as to account for as many factors affecting GVHD development as possible. Before matching, no significant bias was observed in GVHD prophylaxis protocols; nevertheless, PTCy was selected for 40.6% of episodes in the Grade 0–I group. PTCy is a highly effective GVHD prophylactic that has been widely implemented in recent years26. After matching, the PTCy selection rate in the Grade 0–I group decreased to 12.5%. When PTCy was administered, tacrolimus was initiated 5 days post-transplantation27. This means that when PTCy was administered, the TTR evaluation period was counted after day 5 post-transplantation. Therefore, especially in the first 2 weeks post-transplantation, PTCy episodes were statistically more prone to TTR assessment variability, unlike other prophylaxis protocols. Consequently, in the all-episode analysis, the TTR assessment of the Grades 0–I and II–III groups in the first 2 weeks post-transplantation did not significantly differ. However, in the PSM episode analysis, a significant difference in TTR was observed within the first 2 weeks post-transplantation between the Grades 0–I and II–III groups. Furthermore, these results suggest that if PTCy is not selected for GVHD prophylaxis, maintaining the TTR of tacrolimus blood concentrations in the first 2 weeks post-transplantation is crucial. However, this conclusion may be speculative, as the sample size was insufficient to limit the analysis specifically to PTCy.
The inflammatory cytokine TNFα is the most frequently reported protein elevated before GVHD onset. Several reports have shown that an elevated day 7 post-HSCT/pre-HSCT ratio is a predictor of acute GVHD28,29,30. Other studies have shown that increased TNFα concentrations on day 1531 and in the first 3 weeks post-HSCT32 are predictors of subsequent GVHD. These reports suggest that maintaining a high TTR of tacrolimus blood concentrations from early post-transplantation (first 2 weeks) and suppressing T-cell activity might contribute to preventing severe acute GVHD, as observed in the present study population.
This study had some limitations regarding the assessment of TTR and its association with acute GVHD development. First, regarding TTR, we only set a lower therapeutic range limit for blood tacrolimus concentrations to evaluate the association of tacrolimus TTR with the acute GVHD-preventing effects of tacrolimus. We did not set an upper therapeutic range limit. This means that the association between TTR and adverse effect development due to tacrolimus blood concentrations in acute GVHD prophylaxis was not evaluated. Second, this study was conducted at a single center; therefore, the treatment strategy of the hospital may have influenced the trend in acute GVHD development. Third, no association analysis was performed considering HLA concordance. Fourth, after the onset of GVHD, the approach may have been to maintain high tacrolimus blood concentrations. Since the time of GVHD onset in the Grade II-III group was 15–34 days post-transplant, this approach could explain why there was no difference in TTR between the two groups during the first 8 weeks post-transplant. However, this background could not be adequately captured in the study. Fifth, our analysis, in which TTR levels were compared by dividing patients into two groups based on the presence of an event, allows for a comparison of the impact of TTR on outcomes with previous studies12,13,14,15 that evaluated the benefit of tacrolimus TTR in organ transplantation. Our analysis was further adjusted using PSM to account for the background characteristics of the patients included in the study. However, the results are dependent on the covariates selected for this study.
This study showed that maintaining a higher tacrolimus TTR in the early post-transplantation period averts severe acute GVHD development. Our data reiterates the need to control deviations in blood concentrations as much as possible and control them within the therapeutic range when using tacrolimus for acute GVHD prophylaxis after allogeneic HSCT. Early detection of deviations from this therapeutic range is required to minimize IPV in blood concentrations. Thus, effective acute GVHD prophylaxis can be enabled by increasing the frequency of blood concentration measurements when a high TTR of tacrolimus blood concentrations is required. However, the optimal frequency for measuring blood concentrations remains unclear, indicating a need for further studies.
Methods
Study design and setting
Our single-center, retrospective observational cohort study involved Japanese patients undergoing allogeneic HSCT (aged ≥ 18 years), who received tacrolimus for GVHD prophylaxis at the Department of Hematology, University of Miyazaki Hospital, between April 2018 and October 2023. Information on patient age, sex, and transplantation conditions, as well as weight, laboratory data, drug prescription history, tacrolimus blood concentrations, and acute GVHD symptoms up to 100 days post-transplantation, were collected from electronic medical records. Patients who underwent more than one transplantation during the inclusion period were also included, with each transplantation episode considered an independent study subject.
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Review Committee of the Faculty of Medicine at the University of Miyazaki, Japan (O-1546). Due to the retrospective nature of the study, the Ethics Review Committee of the Faculty of Medicine at the University of Miyazaki waived the need to obtain informed consent.
Tacrolimus dosing
Tacrolimus was typically initiated by continuous intravenous infusion at a dose of 0.02–0.03 mg/kg/day starting the day before transplantation. If PTCy was applied for GVHD prophylaxis, tacrolimus was initiated 5 days post-transplantation under the same conditions. For GVHD prophylaxis with tacrolimus and MMF, MMF was started at 30 mg/kg on post-transplant day 1. For tacrolimus and short-term methotrexate, methotrexate was administered at 10 mg/m2 on post-transplant day 1, followed by 7 mg/m2 on days 3, 6, and 11. If PTCy was used for GVHD prophylaxis, cyclophosphamide was given at 50 mg/kg on days 3 and 4 post-transplant, and MMF was initiated at 30 mg/kg on day 5. The target blood tacrolimus concentration was set at 12–15 ng/mL in the initial induction phase and changed based on the patient’s progress at the discretion of the attending physician. The attending physician determined the frequency of tacrolimus blood concentration measurements. When switching to oral administration, a rapid-release formulation (twice daily) was selected for all patients, and the timing of the change varied among patients. Blood draws for tacrolimus concentration monitoring were performed in the morning for intravenous administration and at the trough of the morning dose for oral administration. Tacrolimus blood concentrations were measured in whole blood using an ARCHITECT i1000SR system (Abbott, Tokyo, Japan).
Variables
The Rosendaal linear interpolation method was used to calculate the TTR of tacrolimus blood concentrations33. Briefly, a linear plot was drawn from the last measured blood concentration to the next measured blood concentration to assign a value for days when no blood concentration was measured. All days with measured or assigned blood concentrations were then used to calculate the TTR. In this analysis, two thresholds were established for the therapeutic range of tacrolimus blood concentration: 10 ng/mL or higher and 12 ng/mL or higher. In addition, three evaluation periods were used for TTR assessment: 2, 4, and 8 weeks post-transplantation.
The observation data for acute GVHD development included the developed organ and its grade at the time of initial diagnosis post-transplantation. Acute GVHD grading was determined based on the guidelines of the Japanese Society for Transplantation and Cellular Therapy34.
Statistical method
All transplantation episodes were classified into Grade 0–I and II–III groups based on acute GVHD grading at the time of first diagnosis post-transplantation. The groups were compared in terms of their characteristics at the time of transplantation and the TTR of tacrolimus blood concentrations. Fisher’s exact test was used for nominal variables, and the Mann–Whitney U test was used for continuous variables. For the TTR of tacrolimus blood concentrations, receiver operating characteristic analysis was used to determine the cut-off value associated with acute GVHD (Grade II–III) development. In addition, all transplantation episodes were classified into two groups based on the cut-off value of the TTR of tacrolimus blood concentration. The incidence of acute GVHD incidence (Grade II–III) and its cumulative incidence were compared. Cumulative incidence was compared using the log-rank test.
In addition, to minimize the confounding effects owing to differences in group distribution, PSM was performed at a ratio of 1:1 based on the propensity score for one episode using a logistic regression model. Covariates in the logistic regression model were selected if differences in patient characteristics existed between groups or if the variables were considered clinically important markers of the primary outcomes. The covariates in the propensity score analyses included GVHD prophylaxis and days to GVHD onset. The post-matching analysis groups were compared for characteristics and the TTR of tacrolimus blood concentrations using the same method as all episodes before matching. Furthermore, cut-off values for the TTR of tacrolimus blood concentrations associated with acute GVHD (Grade II–III) development were determined. R v.4.3.2 (R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis. P < 0.05 indicated statistical significance.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Gooptu, M. & Antin, J. H. GVHD Prophylaxis 2020. Front. Immunol. 12, 605726 (2021).
Thomson, A. W., Bonham, C. A. & Zeevi, A. Mode of action of tacrolimus (FK506): molecular and cellular mechanisms. Ther. Drug Monit. 17, 584–591 (1995).
Plosker, G. L. & Foster, R. H. Tacrolimus: A further update of its pharmacology and therapeutic use in the management of organ transplantation. Drugs 59, 323–389 (2000).
Przepiorka, D. et al. Relationship of tacrolimus whole blood levels to efficacy and safety outcomes after unrelated donor marrow transplantation. Biol. Blood Marrow Transpl. 5, 94–97 (1999).
Gao, Y. & Ma, J. Tacrolimus in adult hematopoietic stem cell transplantation. Expert Opin. Drug Metab. Toxicol. 15, 803–811 (2019).
Kuypers, D. R. J. Intrapatient variability of Tacrolimus exposure in solid organ transplantation: a novel marker for clinical outcome. Clin. Pharmacol. Ther. 107, 347–358 (2020).
Yoshikawa, N. et al. Relationship between CYP3A5 polymorphism and Tacrolimus Blood concentration changes in allogeneic hematopoietic stem cell transplant recipients during continuous infusion. Pharmaceuticals (Basel). 14, 353 (2021).
Nakashima, T. et al. Differences in kinetics of tacrolimus concentration after letermovir discontinuation by type of concomitant azole antifungal. Int. J. Hematol. 115, 158–162 (2022).
Yoshikawa, N. et al. Retrospective analysis of the correlation between tacrolimus concentrations measured in whole blood and variations of blood cell counts in patients undergoing allogeneic haematopoietic stem cell transplantation. Eur. J. Hosp. Pharm. 27, e7–e11 (2020).
Suetsugu, K. et al. Impact of CYP3A5, POR, and CYP2C19 polymorphisms on Trough Concentration to dose ratio of Tacrolimus in Allogeneic hematopoietic stem cell transplantation. Int. J. Mol. Sci. 20, 2413 (2019).
Coste, G. & Lemaitre, F. The role of Intra-patient variability of Tacrolimus drug concentrations in solid organ transplantation: a Focus on Liver, Heart, Lung and Pancreas. Pharmaceutics 14, 379 (2022).
Song, W. et al. Lower tacrolimus time in therapeutic range is associated with inferior outcomes in adult liver transplant recipients. Basic. Clin. Pharmacol. Toxicol. 132, 51–59 (2023).
Lao, Q. et al. Effect of Tacrolimus Time in Therapeutic Range on postoperative recurrence in patients undergoing liver transplantation for Liver Cancer. Ther. Drug Monit. 46, 42–48 (2024).
Nguyen, T. V. A. et al. Higher tacrolimus trough levels and time in the therapeutic range are associated with the risk of acute rejection in the first month after renal transplantation. BMC Nephrol. 24, 131 (2023).
Katada, Y. et al. Association between time in therapeutic range of tacrolimus blood concentration and acute rejection within the first three months after lung transplantation. J. Pharm. Heal care Sci. 8, 25 (2022).
Adie, S. K. et al. Tacrolimus time in therapeutic range and long-term outcomes in heart transplant recipients. Pharmacotherapy 42, 106–111 (2022).
Santeusanio, A. D., Gu, A., Weinberg, A. D., Moon, J. & Iyer, K. R. Tacrolimus time-in-therapeutic range is associated with freedom from acute rejection and graft failure following intestinal transplantation. Clin. Transpl. 35, e14291 (2021).
Davis, S. et al. Tacrolimus Intrapatient Variability, Time in Therapeutic Range, and risk of De Novo Donor-Specific antibodies. Transplantation 104, 881–887 (2020).
Brunet, M. et al. Therapeutic drug monitoring of Tacrolimus-Personalized Therapy: second Consensus Report. Ther. Drug Monit. 41, 261–307 (2019).
Hartinger, J. M., Ryšánek, P., Slanař, O. & Šíma, M. Pharmacokinetic principles of dose adjustment of mTOR inhibitors in solid organ transplanted patients. J. Clin. Pharm. Ther. 47, 1362–1367 (2022).
Jorga, A., Holt, D. W. & Johnston, A. Therapeutic drug monitoring of cyclosporine. Transplant. Proc. 36, S396–S403 (2004).
Yang, Y. et al. Population pharmacokinetics of cyclosporine A in hematopoietic stem cell transplant recipients: a systematic review. Eur. J. Pharm. Sci. 204, 106882 (2024).
Ram, R. et al. Association between calcineurin inhibitor blood concentrations and outcomes after allogeneic hematopoietic cell transplantation. Biol. Blood Marrow Transpl. 18, 414–422 (2012).
Ganetsky, A. et al. Higher tacrolimus concentrations early after transplant reduce the risk of acute GvHD in reduced-intensity allogeneic stem cell transplantation. Bone Marrow Transpl. 51, 568–572 (2016).
Hagen, P. A., Adams, W., Smith, S., Tsai, S. & Stiff, P. Low mean post-transplantation tacrolimus levels in weeks 2–3 correlate with acute graft-versus-host disease in allogeneic hematopoietic stem cell transplantation from related and unrelated donors. Bone Marrow Transpl. 54, 155–158 (2019).
Bolaños-Meade, J. et al. Post-transplantation Cyclophosphamide-based graft-versus-host Disease Prophylaxis. N Engl. J. Med. 388, 2338–2348 (2023).
Luznik, L. et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol. Blood Marrow Transpl. 14, 641–650 (2008).
Willems, E. et al. Elevations of tumor necrosis factor receptor 1 at day 7 and acute graft-versus-host disease after allogeneic hematopoietic cell transplantation with nonmyeloablative conditioning. Bone Marrow Transpl. 45, 1442–1448 (2010).
Kitko, C. L. et al. Plasma elevations of tumor necrosis factor-receptor-1 at day 7 postallogeneic transplant correlate with graft-versus-host disease severity and overall survival in pediatric patients. Biol. Blood Marrow Transpl. 14, 759–765 (2008).
Choi, S. W. et al. Change in plasma tumor necrosis factor receptor 1 levels in the first week after myeloablative allogeneic transplantation correlates with severity and incidence of GVHD and survival. Blood 112, 1539–1542 (2008).
August, K. J. et al. Biomarkers of immune activation to screen for severe, acute GVHD. Bone Marrow Transpl. 46, 601–604 (2011).
Liu, D. et al. Diarrhea during the conditioning regimen is correlated with the occurrence of severe acute graft-versus-host disease through systemic release of inflammatory cytokines. Biol. Blood Marrow Transpl. 16, 1567–1575 (2010).
Rosendaal, F. R., Cannegieter, S. C., Van Der Meer, F. J. M. & Briet, E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb. Haemost. 69, 236–239 (1993).
Guidelines of the Japanese Society for Transplantation and Cellular Therapy GVHD. 5th edition. Japanese Society for Transplantation and Cellular Therapy. (2022). https://www.jstct.or.jp/uploads/files/guideline/01_02_gvhd_ver05.1.pdf
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This research was funded by the Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science [grant number JP23K06236] and a grant for clinical research from Miyazaki University Hospital.
Author information
Authors and Affiliations
Contributions
N.Y. wrote the manuscript; N.Y. and Y.E. designed the research; N.Y., Y.E., and Y.M. performed the research; N.Y. and Y.Y. analyzed the data; K.S. and R.I. reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yoshikawa, N., Ehara, Y., Yamada, Y. et al. Time in therapeutic range of tacrolimus in allogeneic hematopoietic stem cell transplant recipients is associated with acute graft-versus-host disease prophylaxis. Sci Rep 15, 3364 (2025). https://doi.org/10.1038/s41598-025-87801-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87801-2