Abstract
This study aimed to manage Helicobacter pylori (H. pylori) infection through a family-centered approach. It conducted a two-year follow-up on infected individuals’ family members in Yichun, Jiangxi, China, to gain comprehensive insights into the transmission dynamics, treatment adherence, and associated risk factors of H. pylori within households. A retrospective analysis was performed on the data obtained from households in Yichun City that participated in the nationwide multicenter H. pylori prevalence study in 2021, along with the corresponding subsequent follow-up data. The collected information encompassed fundamental demographic details of the families, their lifestyle patterns, and the status of H. pylori infection. Among 514 households, 222 comprised two individuals, whereas 68 constituted larger families with five or more members. All member was infected in 9.34% of households. Larger family sizes (≥ 5 individuals) and higher generational counts were closely associated with H. pylori infection (e.g., family size > 6: OR 4.46, 95%CI 1.29 to 15.46). Adult age, marital status, and household members’ infections were identified as primary risk factors (e.g., married individuals: OR 2.03, 95%CI 1.56 to 2.65). Students and previously uninfected individuals exhibited lower infection risks (e.g., tested as negative: OR 0.48, 95%CI 0.31 to 0.73). Maternal, paternal, or sibling infections were linked to increased risks of child infections (e.g., mother infected: OR 2.58 95%CI 1.37 to 4.87). Successful eradication in ≥ 2 individuals reduced the infection risk for other members (OR 0.25, 95%CI (0.07 to 0.89). H. pylori displayed noticeable clustering infection characteristics within families. This study lends support to family-based management strategies, but given suboptimal adherence to household management, there is a need to enhance education on the hazards of H. pylori before implementing screening programs.
Similar content being viewed by others
Introduction
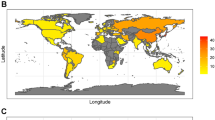
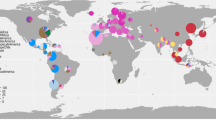
Helicobacter pylori (H. pylori) has been designated as a Class I carcinogen by the International Agency for Research on Cancer and is acknowledged as an essential, albeit not exclusive, etiological factor for gastric adenocarcinoma1,2,3,4. Empirical evidence suggests that eradication of H. pylori mitigates the risk of gastric cancer development5,6,7. In China, the overall prevalence of H. pylori infection approximates 50%8, yet there are substantial regional disparities and urban-rural differences. Despite studies indicating a decline in H. pylori infection rates over the years6, attributed to improved living standards and advancements in diagnostic techniques, it remains a prevalent communicable disease often transmitted within families9,10. In most Chinese provinces, familial prevalence of H. pylori can exceed 50%, even reaching upwards of 80%11. Most infections are acquired during early life, often in childhood or adolescence12. Studies have shown that the risk of H. pylori infection in children and adolescents is significantly associated with infection in mothers, fathers, grandparents, or siblings, underscoring the predominance of intrafamilial transmission. In most cases, unless eradicated through targeted treatment, the infection persists lifelong13.
H. pylori infection subsequently endures through most of the host’s life unless it is treated with eradication therapy14,15,16. H. pylori infection is thought to be transmitted via fecal-oral, gastro-oral, and oral-oral routes, with socioeconomic status and hygiene being significant contributors to the risk of infection17,18. The infected parent, especially the mother, is thought to play an important role in its transmission. Therefore, addressing H. pylori infection at the household level holds significant clinical and public health relevance for the prevention of associated diseases10,11,19.
Effective screening and treatment for H. pylori are essential. Current strategies encompass traditional approaches such as ‘test-and-treat’ and ‘screen-and-treat,’ as well as the Family-Based H. pylori Infection Control and Management (FBCM) strategy19. FBCM strategy addresses the infection and disease status of all family members, potentially reducing intrafamilial transmission of H. pylori. Comparative analyses indicate that FBCM and screen-and-treat strategies are more cost-effective for preventing gastric cancer than a lack of screening20. The family-based strategy can identify a greater number of infected participants with the same number of tests, compared to the widely used test-and-treat approach21. A previous large-scale, family-based epidemiological survey on H. pylori infection supports the feasibility of shifting from individual-based to family-based management strategies in clinical practice11.
This study focuses on within-family H. pylori screening. This study involves a two-year follow-up of families from Yichun City who participated in a national family-based epidemiological survey in 2021. The research further investigates factors related to intrafamilial transmission of H. pylori and the compliance with family-based H. pylori eradication treatment.
Methods
The study enrolled families who had previously participated in the national H. pylori screening in 2021, covering different communities in Yichun, Jiangxi, China. The investigation adopted a nonprobability (convenience) sampling method from each region and referred to the probability sampling for sample size calculation11. A total of 514 families, comprising 1569 individuals, were ultimately included. The collected information encompassed fundamental demographic details of the families, their lifestyle patterns, and the status of H. pylori infection. A follow-up assessment was conducted two years post-enrollment on 208 families, comprising 523 individuals, and further data was collected regarding the reinfection status and eradication therapy among the retested households. This study protocol has been approved by the Medical Ethics Committee of the First Affiliated Hospital of Nanchang University. We confirm that all methods were carried out in accordance with relevant guidelines, and all included cases were recorded in the Human Genetic Resources Center of the First Affiliated Hospital of Nanchang University. Given the retrospective nature of the study, the need for informed consent was waived by the institutional review boards.
The target population was primarily families with H. pylori-positive infections to explore intrafamilial transmission of H. pylori. Inclusion criteria: (1) past participation in the 2021 national family-based H. pylori epidemiological survey, (2) at least one family member infected with H. pylori. Exclusion criteria: (1) use of antibiotics in the past month, use of proton pump inhibitors within the last two weeks, (2) treatment for H. pylori within the past three months, (3) families deemed unsuitable for participation by the researchers. A family in which at least one member is infected with H. pylori is defined as an infected family.
Statistical analyses were conducted using the chi-square test or Fisher’s exact test to compare categorical variables that are unordered. Continuous variables were summarized as mean ± standard deviation and compared using the Student’s t-test. All variables with a p-value < 0.10 in univariate analysis were included in a multivariate logistic regression analysis to investigate risk factors associated with H. pylori infection. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. A p-value < 0.05 was considered statistically significant.
Result
Overall analysis
In 2021, the study initially registered 535 families, with 514 ultimately fulfilling the inclusion criteria for the final analysis, encompassing a total of 1,569 participants from these families (Fig. 1). The average age of the study population was 40.31 years, with a demographic composition of 738 males and 831 females, including 322 children and adolescents. H. pylori infection was detected in 520 participants, representing an infection rate of 33.14%. This rate was further stratified, with adults exhibiting a rate of 36.49% and children and adolescents at 20.19% (Fig. 2A). Notably, the age group with the highest infection rate was 26–35 years (Fig. 2D). In 2023, a subset of 208 families (comprising 523 individuals) underwent the 13 C-Urea Breath Test for H. pylori infection; the details are depicted in Fig. 1. Among these families, 277 individuals tested positive for H. pylori, while 246 tested negative. Importantly, 86 individuals from families previously negative for H. pylori seroconverted to positive in this subsequent screening round.
H. pylori infection status and risk factors
Table 1 presents the infection status within families. Among 514 families, there were 222 two-person families and only 68 families with more than five members (Fig. 2B). In the 338 infected families, 197 had one person infected with H. pylori, which is the most common scenario. There was only one household with all five members infected (Fig. 2C). The average number of infected members was 1.54, accounting for 65.75% of the total number of families. A total of 9.34% of families had all members infected. Among two-person families, 36 families had all members infected, and in families of five, one family had all members infected (Table S1). Univariate and multivariate analyses were conducted to determine factors associated with familial infection. Larger family size (≥ 5 individuals) and more generations were significantly associated with H. pylori infection in the univariate analysis (e.g., 5 family member size: OR 2.68 95%CI 1.23 to 5.83). In the multivariate regression, a family size of ≥ 5 was an independent risk factor (family member size > 6: OR 5.03, 95%CI 1.19 to 21.33), while the number of generations showed no significant statistical difference. Other factors, such as utensil disinfection practices; dishwashing methods, drinking water sources, sharing of eating utensils among family members, meal segregation; presence of pets, poultry, or livestock at home had no impact on infection risk (p > 0.05).
The personal infection status and associated risk factors for H. pylori are detailed in Table 2. Being an adult, being married, and having infected family members were identified as the primary risk factors. Students and individuals with a previous negative H. pylori status had a lower risk of infection (tested as negative: OR 0.48, 95%CI 0.31 to 0.73). A multivariate analysis showed that individual infection was significantly associated with the presence of infected family members (p < 0.01). Further analysis was conducted focusing on the infection status among children and adolescents, as well as the potential intrafamilial transmission routes, as presented in Table 3. Among the 322 children surveyed, 133 were from single-child families, while the rest had 1–3 or more siblings. The overall infection rate among these children was 20.19%. The risk of infection in children was associated with infection in their mothers, fathers, or siblings. However, only maternal and sibling infections were independent risk factors for infection (e.g., mother infected: OR 2.58, 95%CI 1.37 to 4.87).
Among the 208 households, 64 families (12.2%) exhibited new H. pylori infections, affecting 86 individuals (34.9%). Among these, 5 individuals had a delta over baseline (DOB) value ranging between 4 and 6. In 112 families where H. pylori-positive members either did not receive eradication treatment or for whom the treatment was unsuccessful, 37 families experienced new infections. Successful eradication of H. pylori in two or more infected members within a family significantly reduced the risk of infection in previously negative members (OR 0.25, 95%CI 0.07 to 0.89). Other factors, including gender, age, living space, and lifestyle, did not significantly impact intrafamilial transmission, as detailed in Table 4.
Eradication treatment and compliance analysis
Adult patients testing positive on initial screening are advised to undergo gastroscopy and H. pylori eradication therapy at a nearby hospital. Two years later, patient-related information was collected, and factors affecting compliance were further evaluated (Table 5). Of the 523 individuals, 277 were infected with H. pylori, and 178(64.3%) followed the advice to undergo eradication treatment. Further analysis of risk factors for compliance with eradication therapy showed that adults, particularly married individuals, demonstrated better treatment compliance. Gender, family, annual income, education level, and related symptoms were not significantly associated with compliance (P > 0.05). Of the 523 individuals followed up, 103 had previously undergone gastroscopy. Among the 277 individuals, 53 (19.1%) underwent gastroscopic treatment, with 31 cases (58.4%) of gastritis, 11 (20.7%) of gastric ulcers, and no cases of gastric cancer. Compliance with gastroscopy showed similar risk factors to those for treatment compliance, with married individuals, adults, and those with previous symptoms being more likely to comply with gastroscopy (e.g., having symptoms: OR 5.36, 95%CI 2.78 to 10.33). Conversely, being a student was associated with a higher risk of low compliance with both gastroscopy and eradication treatment. Gender, family, annual income, education level, were not significantly linked with compliance.
Discussion
This study investigates the intrafamilial transmission of H. pylori in Yichun City, along with an assessment of the associated risk factors. The analysis is structured to examine H. pylori transmission at various levels, including individuals, families, and children and adolescents. The results demonstrate that the presence of infected family members and multigenerational householding are the predominant risk factors for transmission within families. Moreover, children’s risk of infection is significantly associated with parental infection status. Cohabiting with H. pylori-infected members elevates the susceptibility of other household members, such as spouses and children, to the infection. While H. pylori may not infect all family members, the risk of infection is contingent upon factors such as close contact, lifestyle practices, and hygiene conditions19,22,23.
Previous studies have examined the relationship between familial H. pylori infection and a range of risk factors. A study conducted in Central China focused on family-based H. pylori infections and found that infection rates were positively correlated with the duration of marriage. Additionally, the study reported an association between educational level and H. pylori infection, with higher education being linked to lower infection rates24. However, this study did not find a statistically significant association with education level, which may relate to the smaller sample size included. A larger study encompassing 31 provinces of China, which offered greater external validity, identified that living with infected family members and residing in high-prevalence areas were independent risk factors for familial infection; families with higher levels of education and income, as well as those using serving chopsticks, had lower infection rates24. Our study corroborates the high rate of familial transmission of H. pylori and suggests that contact with infected family members is likely the main route of transmission. The findings of our research are consistent with these previous studies, further confirming the familial aggregation of H. pylori and providing a theoretical basis for the development and implementation of family-based H. pylori screening strategies.
Children often acquire H. pylori infections from their familial environment. Recent national statistics indicate that the average household size has diminished from 4.05 individuals in 1990 to 2.62 individuals in 2021, influenced by the one-child policy, resulting in most families having a single child25. In the absence of siblings, the transmission of H. pylori from parents or grandparents to the child may represent a more significant vector for bacterial dissemination. Yi-Qi Du and colleagues have identified parental H. pylori infection as an independent risk factor for the child’s acquisition of the bacterium11. Research by P Dominici et al. in 1999 has already investigated the familial clustering of H. pylori, revealing that infections tend to aggregate within families belonging to the same demographic, with children from dual-positive parents having twice the risk of infection compared to those from dual-negative households26. Furthermore, the potential for H. pylori infection in negative family members from positive households may also be associated with the number of infected individuals within the family. This study followed negative individuals over two years, finding that approximately one-third negative members seroconverted, suggesting a correlation with the number of family members infected and whether eradication was pursued. However, distinguishing between community-acquired and intrafamilial infections requires confirmation of clonal origin through H. pylori typing within the stomach27. In Japan, studies utilizing multilocus sequence typing (MLST) and analysis of random amplified polymorphic DNA (RAPD) fingerprint patterns revealed that intrafamilial transmission, particularly between mother and child and among siblings, is a predominant pathway of spread28. Conversely, a study in Peru reported opposing findings, with 70% of mother-child strains showing mismatched RAPD fingerprint patterns and non-matching diagnostic gene sequences (> 1% DNA sequence divergence); most strains from siblings or other paired family members also lacked genetic relatedness29. These discrepancies may be associated with varying levels of development across countries. Thus, the issue remains contentious and warrants further investigation through multi-center studies with large sample sizes.
Eradication of H. pylori equates to a reduction in the reservoir of infection. We observed suboptimal compliance with H. pylori eradication therapy and gastroscopy. Factors such as gender, type of residence, age, occupation, cultural background, and intrafamilial infection status may be pertinent risk determinants. The study identified marital status as correlated with compliance; married individuals demonstrated better adherence, possibly linked to a heightened sense of familial responsibility. Although studies indicate that 90% of intestinal-type gastric carcinomas are associated with H. pylori30, the progression to cancer typically requires over a decade, rendering eradication necessary but not urgent. A survey of 3,211 members of the general public and 546 physicians indicated a lack of awareness regarding the risks posed by H. pylori and preventive measures31, which may contribute to non-adherence with our study recommendations. For gastroscopy, symptomatic positive patients are more inclined to opt for this diagnostic procedure. The majority of H. pylori infections are asymptomatic, thereby affecting gastroscopy compliance. This also reflects low public awareness of the risks associated with H. pylori infection. Pre-screening education has been demonstrated to be feasible and effective in enhancing patient compliance32,33.
This study acknowledges several limitations that may influence the interpretation of the results: (1) The population primarily reflects the local residents of Yichun, which may affect the generalizability of the findings. (2) There is a relatively low level of awareness about H. pylori among the local populace, potentially impacting the community’s engagement with the study. (3) The small number of individuals who have undergone eradication treatment results in a sample size that may be insufficient to accurately assess the efficacy of the eradication regimen. However, this study also exhibits several advantages: (1) It encompasses a large sample size across the entire Yichun region, providing a comprehensive overview of the prevalence and dynamics of H. pylori infection. (2) Both univariate and multivariate analyses were conducted, which strengthens the reliability of the study’s findings by accounting for various factors that may influence infection rates. (3) The study has contributed to elevating awareness of H. pylori among the local community, which may effectively reduce intrafamilial transmission through informed preventive measures.
Conclusion
This study reflects the prevalence of H. pylori infection in families in the Yichun area of China, suggesting that intrafamilial transmission may be a primary mode of H. pylori infection locally. Family-based H. pylori infection control and related disease prevention offer a novel alternative. To better implement this strategy, pre-screening education for the population is deemed necessary.
Data availability
The data that used to support the findings of this research are available from the corresponding author.
References
Hooi, J. K. Y. et al. Global prevalence of H. pylori infection: systematic review and Meta-analysis. Gastroenterology 153 (2), 420–429 (2017).
Eslick, G. D. et al. Association of H. Pylori Infection with Gastric Carcinoma: a Meta-analysis. Am. J. Gastroenterol. 94 (9), 2373–2379 (1999).
Helicobacter, Cancer, G. & Collaborative Gastric cancer and H. Pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut 49 (3), 347–353 (2001).
Huang, J. Q. et al. Meta-analysis of the relationship between H. Pylori seropositivity and gastric cancer. Gastroenterology 114 (6), 1169–1179 (1998).
Takenaka, R. et al. H. Pylori eradication reduced the incidence of gastric cancer, especially of the intestinal type. Aliment. Pharmacol. Ther. 25 (7), 805–812 (2007).
Lee, Y. C. et al. Association between H. Pylori Eradication and Gastric Cancer incidence: a systematic review and Meta-analysis. Gastroenterology 150 (5), 1113–1124e5 (2016).
Yeh, J. M. et al. Exploring the cost-effectiveness of H. Pylori screening to prevent gastric cancer in China in anticipation of clinical trial results. Int. J. Cancer. 124 (1), 157–166 (2008).
Zamani, M. et al. Systematic review with meta-analysis: the worldwide prevalence of H. Pylori infection. Aliment. Pharmacol. Ther. 47 (7), 868–876 (2018).
Sari, Y. S. et al. H pylori: treatment for the patient only or the whole family?. World J. Gastroenterol., 14(8). (2008).
Ding, S. Z. Global whole family based-H. pylori eradication strategy to prevent its related diseases and gastric cancer. World J. Gastroenterol. 26 (10), 995–1004 (2020).
Zhou, X. Z. et al. Large-scale, national, family-based epidemiological study onH. Pyloriinfection in China: the time to change practice for related disease prevention. Gut 72 (5), 855–869 (2023).
Malaty, H. M. et al. Age at acquisition of H. Pylori infection: a follow-up study from infancy to adulthood. Lancet 359 (9310), 931–935 (2002).
Du, Y. et al. Consensus on eradication of H. Pylori and prevention and control of gastric cancer in China (2019, Shanghai). J. Gastroenterol. Hepatol. 35 (4), 624–629 (2020).
Malfertheiner, P. et al. H. Pylori infection. Nat. Reviews Disease Primers, 9(1). (2023).
Malfertheiner, P. et al. Management ofH. Pyloriinfection: the Maastricht VI/Florence consensus report. Gut 71 (9), 1724–1762 (2022).
Sugano, K. et al. Kyoto global consensus report onH. Pylorigastritis. Gut 64 (9), 1353–1367 (2015).
Asaka, M. et al. Guidelines in the management of H. Pylori infection in Japan. Helicobacter 6 (3), 177–186 (2001).
Schwarz, S. et al. Horizontal versus familial transmission of H. Pylori. PLoS Pathog. 4 (10), e1000180 (2008).
Ding, S. Z. et al. Chinese Consensus Report on Family-BasedH. pyloriInfection Control and Management ( Gut, 2022. 71(2): pp. 238–253. (2021).
Ma, J. et al. Both family-based H. Pylori infection control and management strategy and screen‐and‐treat strategy are cost‐effective for gastric cancer prevention. Helicobacter, 27(4). (2022).
Zhang, J. et al. ‘Family-based’ strategy forH. Pyloriinfection screening: an efficient alternative to ‘test and treat’ strategy. Gut, (2023).
Nahar, S. et al. Evidence of intra-familial transmission of H. Pylori by PCR-based RAPD fingerprinting in Bangladesh. Eur. J. Clin. Microbiol. Infect. Dis. 28 (7), 767–773 (2009).
Osaki, T. et al. Analysis of intra-familial transmission of H. Pylori in Japanese families. J. Med. Microbiol. 64 (1), 67–73 (2015).
Yu, X. C. et al. Family-based H. Pylori infection status and transmission pattern in central China, and its clinical implications for related disease prevention. World J. Gastroenterol. 28 (28), 3706–3719 (2022).
China, N. B. o.s.o., China statistical Yearbook 2021. China Statistical Press 2021. (2022).
Dominici, P. et al. Familial clustering of H. Pylori infection: population based study Commentary: H. Pylori—the story so far. Bmj 319 (7209), 537–541 (1999).
Osaki, T. et al. Multilocus sequence typing of DNA from faecal specimens for the analysis of intra-familial transmission of H. Pylori. J. Med. Microbiol. 62 (5), 761–765 (2013).
Yokota, S. et al. Intrafamilial, preferentially Mother-to‐child and Intraspousal, H. Pylori infection in Japan determined by Mutilocus sequence typing and Random amplified polymorphic DNA fingerprinting. Helicobacter 20 (5), 334–342 (2015).
Herrera, P. M. et al. DNA-Level diversity and relatedness of H. pylori strains in Shantytown Families in Peru and Transmission in a developing Country setting. J. Clin. Microbiol. 46 (12), 3912–3918 (2008).
Plummer, M. et al. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Global Health. 4 (9), e609–e616 (2016).
Wu, Y. et al. Awareness and attitudes regarding H. Pylori infection in Chinese physicians and public population: a national cross-sectional survey. Helicobacter, 25(4). (2020).
Walter, B. et al. Smartphone application to Reinforce Education increases High-Quality Preparation for Colorectal Cancer Screening colonoscopies in a Randomized Trial. Clin. Gastroenterol. Hepatol. 19 (2), 331–338e5 (2021).
Crankshaw, S. et al. The Durham Initiative for Stomach Health (DISH): a pilot community-based H. Pylori education and screening study. BMC Gastroenterol., 20(1). (2020).
Acknowledgements
The Key Laboratory Project of Digestive Diseases in Jiangxi Province (2024SSY06101), and Jiangxi Clinical Research Center for Gastroenterology (20223BCG74011).
Funding
This work was supported by the National Natural Science Foundation of China (82170580).
Author information
Authors and Affiliations
Contributions
Ao-fei Huang, Cong He and Jian-Wen Sheng contributed equally to this work and share first authorship. Yin Zhu and Hui-Zhen Fan designed the main idea of this study; AFH contributed to data analysis and wrote the manuscript; YZ and CH reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, Af., He, C., Sheng, JW. et al. The epidemiological study of family-based Helicobacter pylori screening and its benefits: a cross-sectional study. Sci Rep 15, 5553 (2025). https://doi.org/10.1038/s41598-025-87836-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87836-5
Keywords
This article is cited by
-
Current concepts of Helicobacter pylori infection
European Journal of Medical Research (2025)