Abstract
The best treatment method for reverse obliquity intertrochanteric fractures (ROIFs) is still under debate. Our team designed the modified proximal femoral nail (MPFN) specially for treating such fractures. The objective of this research was to introduce the MPFN device and compare the biomechanical properties with Proximal Femoral Nail Antirotation (PFNA) and InterTAN nail via finite element modelling. An AO/OTA 31-A3.1 ROIF model was established via Mimics software. Three implants were depicted and assembled on the ROIF models. The axial, bending, and torsion loads were simulated to test stress and displacement of three fixation models. Compared to the PFNA and InterTAN models, the MPFN model had more dispersed stress distribution under axial loads of 2,100 N. The MPFN showed lower von Mises stress on bones compared with that of PFNA and InterTAN in axial loads. In term of maximum displacement, the MPFN had a 12.6% reduction compared to the PFNA model in axial load case. In bending and torsion loads, the MPFN model also demonstrated better biomechanical properties than the PFNA and InterTAN models. The modified proximal femoral nail presented the best biomechanical performance, followed by the InterTAN nail, and the PFNA for fixing reverse obliquity intertrochanteric fractures. The MPFN has the potential to be a promising device for patients with ROIFs.
Similar content being viewed by others
Introduction
Based on the AO/OTA classification guidelines, reverse obliquity intertrochanteric fractures (ROIFs) are classified as the type of AO/OTA 31-A31. The main fracture line of ROIFs usually passes from the proximal-medial to the distal-lateral1. This is different from that of AO/OTA 31-A1 and A2. The proportion of AO/OTA 31-A3 fractures has reached to 5.3-23.5% of all femoral intertrochanteric fractures2,3. Nowadays, to reduce long-term immobilization and the associated complications, surgical treatment is recommended for most of ROIFs. Yet, the fixation failure rate of ROIFs remains high4,5. Therefore, how to improve the treatment effects of ROIFs has been a hot issue faced by orthopedic scholars.
Several extramedullary implants were used in fixing ROIFs initially, comprising the dynamic hip screw (DHS), the sliding hip screw, the proximal femoral anatomic plate, etc1,6,7,8. However, patients using the above fixation devices suffered lots of complications6,7,8. Moreover, the surgical trauma is relatively large when using extramedullary implants to fix ROIFs, such as the long incision and excessive blood loss. In view of this, scholars have tended to use intramedullary nails to treat such fractures and have achieved good clinical effects9,10. Intramedullary fixation has some advantages, including the short level arm, the central and minimally invasive fixation, and early weight-bearing. The common intramedullary implants for fixing ROIFs contain PFNA, Gamma3 nail and InterTAN. Notably, the neck screws of these intramedullary nails are approximately parallel to the main fracture line of ROIFs. This anatomical characteristic of ROIFs makes it significantly different from other types of intertrochanteric fractures. It also generates different biomechanical mechanisms. The proximal fracture fragment of ROIFs is prone to sliding downward and outward. The distal fragment has the trend for medial migration while the neck screw is prone to cutting out. The region between the implant junction and the main fracture line forms a stress concentration area. The fixation failure resulting from these factors is not uncommon in ROIF patients11. Other scholars used cables to resist this sliding tendency in ROIFs12,13. Yet, the insertion of cables brings additional soft tissue damage and prolongs operation time. Hence, there is no specially designed intramedullary implants for the treatment of ROIFs currently.
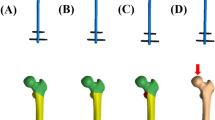
Based on these factors, our team proposed the modified proximal femoral nail (MPFN, Fig. 1A) to treat patients with ROIFs. Two screws are interlocked at the proximal part of the MPFN, including the neck screw and the subtrochanteric screw. The subtrochanteric screw passes through the tail of the neck screw and then the main nail, and is fixed below the lesser trochanter. The interlocking design aims to resist the sliding of the fracture fragment and disperse the local stress. Our team made biomechanical comparisons among the three fixation models (PFNA, InterTAN, and MPFN) for fixing ROIFs via finite element modelling. Finite element analysis (FEA) is a virtual technique which combines computer simulation and digitization. The mechanical properties of new implants could be evaluated via setting boundary conditions and loading loads14. Compared with clinical trials and cadaveric experiments, finite element technique possesses several advantages, including low cost, allowing repeated tests, etc. In this research, an AO/OTA 31-A3.1 ROIF model was established via finite element modelling. Three fixation models were evaluated in axial, bending, and torsion load cases. Our team assumed that the MPFN had the best biomechanical properties among the three fixation models in simulating loads.
Materials and methods
Construction of the AO/OTA 31-A3.1 ROIF model
Written informed consents were achieved from the volunteers, and all methods were conducted in accordance with relevant guidelines and regulations. The experimental protocols have been approved by the ethics committee of Xi’an Honghui Hospital. Twenty sets of intact femoral CT scans were gotten via a blinded and randomized trial. The mean values of CT data were obtained. Then, an intact three-dimensional (3D) femur model was established according to the above data via Mimics software (Materialize Company, Leuven, Belgium). These data were imported into the Studio software (3D system Inc., Rock Hill, SC, USA). The surface of the femur model was smoothed and polished. Based on the values of Hounsfield Unit (HU), cortex and cancellous bones were identified14. The boundary value was assumed to be 70015. On the basis of the AO/OTA classification, an osteotomy plane was performed which was set as 60 degrees relative to the sagittal plane above the lesser trochanter. Thus, an AO/OTA 31-A3.1 ROIF model was established15,16.
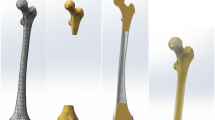
Construction of three implant models
The computer-aided design (CAD) software was used to depict 3D models of three implants (PFNA, InterTAN, and MPFN). Then, these implant models were assembled on the ROIF models. The anteroposterior (AP) and lateral images of the MPFN device are displayed graphically in Fig. 1A. The dimensions of the MPFN are illustrated as follows. The length of the main nail is 240 mm. The diameters for the proximal and distal parts of the main nail are designed as 17 mm and 10 mm, respectively. The diameters of the neck screw, the subtrochanteric screw, and two distal locking screws are designed as 10 mm, 5 mm, and 5 mm. The neck screw is located at the center of the femoral neck and head. The subtrochanteric screw is located below the lesser trochanter which interlocks with the main nail and the neck screw. The included angle between the subtrochanteric screw and the neck screw is at a right angle while between the main nail and the neck screw is 130 degrees, respectively.
Mesh convergence test and model validation
The tetrahedral element mesh was used during finite element setting. A convergence test was conducted to evaluate the reliability of these models referring to similar studies17. The maximum von Mises stress on bones was used for analyzing mesh convergence. The maximum stress on femur models were compared to five mesh sizes, including 3 mm, 2.5 mm, 2 mm, 1.5 mm, and 1 mm. The results indicated that the values of maximum stress on bones at the 1.5 mm mesh was approximate to those of the 1 mm and 2 mm meshes, and the difference was within 5%. Therefore, the mesh size of this study was defined as 1.5 mm. With maximum Degree of Freedom, field variables, including displacement and strain energy, were also in the range of 5% for both types of elements and there was no maximum stress point. The values of mesh convergence were within 5%, demonstrating the reliability of these models.
To perform model validation, our finite element model of the intact femur was compared to previous experimental data18. The vertical loads of 2,100 N were loaded onto the femoral head to evaluate axial stiffness. The values of axial stiffness from our finite element computation were 0.52 kN/mm which were within the interval (0.76 ± 0.26 kN/mm) of cadaveric experiments18. The results demonstrated that our finite element models were well validated.
Finite element settings of boundary conditions and loads
Material properties of bones and implants were set as homogeneous, isotropic, and linear elastic referring to previous literature14. Elements and nodes were 534,775 and 840,042 for the PFNA fixation model, 552,155 and 872,985 for the InterTAN while 537,984 and 847,212 for the MPFN, respectively. Titanium alloy was endowed with the three implants. The Young’s modulus was assumed to be 16,800 MPa, 840 MPa, and 110,000 MPa for cortex, cancellous bones, and Titanium alloy14. Poisson’s ratio was supposed to be 0.3 for cortex and Titanium alloy while 0.2 for cancellous bones, respectively19.
Frictional contacts were defined between different sections of these fixation models and the frictional coefficient was assumed to be 0.415. Boundary settings for axial, bending, and torsion loads are shown graphically in Fig. 1B. With regard to axial loads, the femoral condyle was properly fixed to inhibit extra movement of the whole configuration. In order to simulate axial compression, axial loads of 2,100 N were applied vertically to the femoral head. Under bending boundary conditions, the mid and distal femur was fixed at the same time. 175 N-loads acted laterally onto the femoral head to simulate bending force14. As to torsion load case, a torque force of 15 Nm loaded along the femoral neck axis to simulate rotation14.
Evaluation parameters and percent difference (PD)
Maximum stress on implants and bones, maximum displacement of models and fracture surface were tested via FEA under axial, bending, and torsion loads. Since the PFNA device has become one of the most widely applied implants in fixing intertrochanteric fractures, and has obtained relatively good therapeutic effects, it was defined as the control group during data analyzing. The percent difference was calculated through the following formula: PD =(P1 − Pa)/ P1 × 100%. Pa denotes the values of the InterTAN or MPFN models while P1 denotes the value of the PFNA model.
Results
Maximum stress on implants under three simulating loads
The nephograms of maximum stress on implants under axial, bending, and torsion loads are presented in Fig. 2. The von Mises stress concentration area was the junction between the neck screw and the main nail for the PFNA and InterTAN models. It was concentrated on the junction between the subtrochanteric screw, the neck screw and the main nail for the MPFN model. Under axial loads of 2,100 N, the maximum stress on implants was 241.34 MPa, 259.13 MPa, and 214.55 MPa for the PFNA, InterTAN, and MPFN models, respectively. This value was 64.83 MPa, 58.49 MPa, and 53.98 MPa for these models under bending loads. Besides, it was 53.53 MPa, 59.30 MPa, and 48.04 MPa under torsion loads of 15 Nm for the three fixation models, respectively. The values of maximum stress on implants for the MPFN models were less than those of the PFNA and InterTAN models in three simulating loads. Compared to the PFNA, the reduction of PD for the MPFN was 11.1%, 16.7%, and 10.2% in axial, bending, and torsion load cases, respectively.
Maximum stress on bones under three simulating loads
The nephograms of maximum stress on femurs under axial, bending, and torsion loads are exhibited in Fig. 3. The maximum stress on femurs was 174.92 MPa, 125.72 MPa, and 123.94 MPa for the PFNA, InterTAN, and MPFN models in axial load case, respectively. It was 60.20 MPa, 56.35 MPa, and 51.04 MPa for the three fixation models in bending load case. In addition, this index was 61.19 MPa, 27.64 MPa, and 34.46 MPa in torsion load case, respectively. The values of maximum stress on femurs for the MPFN models was less than those of the PFNA and InterTAN models in axial and bending tests. It was also lower for the MPFN model than that of the PFNA model in torsion test. Notably, compared to the PFNA, the PD reduction of this index for the MPFN was 29.1%, 15.2%, and 43.7% under axial, bending, and torsion load conditions, respectively.
Maximum displacement under three simulating loads
The nephograms of maximum displacement under three simulating loads are presented in Fig. 4. In axial load experiments, the maximum displacement was 19.35 mm, 18.58 mm, and 16.91 mm for the PFNA, InterTAN, and MPFN models, respectively. This parameter was 0.49 mm, 0.50 mm, and 0.43 mm in bending load experiments while 3.12 mm, 3.37 mm, and 2.55 mm in torsion load conditions. The values of maximum displacement for the MPFN models were smaller than those of the PFNA and InterTAN models in three load cases. The PD reduction of maximum displacement for the MPFN model was 12.6% in axial load case, 10.9% in bending load case, and 18.1% in torsion load case, compared to the PFNA model.
Maximum displacement of fracture surface (MDFS) under three simulating loads
The nephograms of MDFS in axial, bending and torsion loads are exhibited in Fig. 5. The MDFS was 13.51 mm, 13.82 mm, and 12.25 mm for the PFNA, InterTAN, and MPFN models in axial load case, respectively. It was 0.10 mm, 0.07 mm, and 0.07 mm in bending load case for the three fixation models. In addition, this index was 2.15 mm, 2.32 mm, and 1.78 mm in torsion load case, respectively. The values of MDFS for the MPFN models were smaller than those of the PFNA and InterTAN models in three load tests. Specially, compared to the PFNA, the PD reduction of this index for the MPFN was 9.3%, 33.4%, and 17.0% under axial, bending, and torsion load conditions, respectively.
Discussion
From an overall trend perspective, findings showed that maximum stress of the MPFN models was lower than those of the PFNA and InterTAN models, and maximum displacement was smaller for the MPFN models than those of the PFNA and InterTAN models under axial, bending, and torsion loads. Our results indicated that the MPFN had biomechanical advantages compared to PFNA and InterTAN for the management of ROIFs. The MPFN might be a good strategy for the treatment of ROIF patients.
Intramedullary fixation is recommended by most scholars for the treatment of unstable femoral trochanteric fractures20,21. This central fixation method typically allows patients with ROIFs to perform partial or complete weight-bearing early on, thereby reducing the incidence of bed-rest related complications22. Previous literature have demonstrated that stress applying to the femoral head surface could be as high as two to three times of one’s weight in walking23. Hence, the axial loads of 2,100 N were simulated via finite element method in this study. The unique design of the MPFN may be the reason for its superior axial stiffness compared to PFNA and InterTAN. The interlocking between the neck screw and the subtrochanteric screw restricts the sliding of the proximal fracture fragment in ROIFs. Simultaneously, the subtrochanteric screw disperses the stress at the junction between the main nail and the neck screw. These factors make the MPFN less prone to implant failure compared to PFNA and InterTAN.
Currently, there is few literature focusing on the antirotation of implants in patients with ROIFs. Based on our data, compared to the PFNA and InterTAN models, the MPFN model showed better antirotation performance in fixing ROIFs. The improvement of the MPFN’s antirotation may be due to its subtle structure. A small triangular and rigid structure is formed between the main nail, the neck screw, and the subtrochanteric screw. In addition, a big triangular stable structure is shaped between the neck screw, the subtrochanteric screw, and the medial wall of the proximal femur. This conforms to the principle of triangular stable structure proposed by Zhang et al.24. Proximal Femur Bionic Nail (PFBN) is a new type of implant designed based on triangular stability theory for fixing intertrochanteric fractures. Biomechanical studies have shown that compared to PFNA and InterTAN, the PFBN had better mechanical properties in fixing AO/OTA 31-A1.3 and 31-A3 fractures25,26. The two neck screws of PFBN are located at the proximal fragment above the main fracture line of ROIFs, so this design may not provide good antirotation for ROIFs. The neck screw and the subtrochanteric screw of the MPFN device are located on both sides of the fracture line of ROIFs. These two screws are locked in a right angle, ensuring good resistance to rotation. As shown in our results, this interlocking structure of the MPFN also provided better anti-compression and anti-bending properties, compared to the PFNA and InterTAN devices.
Several scholars emphasized the importance of medial support for intertrochanteric fractures27,28,29. Chen et al.’s study indicated that the reduction loss incidence after surgery due to comminuted medial wall was approximately 20% in patients with trochanteric fractures27. Song et al.’s study demonstrated that the comminuted medial wall was a relatively reliable parameter to predict implant failure after intramedullary fixation for femoral intertrochanteric fractures29. Nie et al. conducted biomechanical experiments and demonstrated that the medial wall of proximal femur was more important than the lateral wall for patients with trochanteric fractures28. A medial support nail-II (MSN-II) with the triangular stability structure was developed for the treatment of ROIFs16. Nie et al.’s research showed that compared with PFNA-II, the MSN-II exhibited better mechanical stability for fixing ROIFs under increasing axial loads via finite element analysis16. Although the MSN-II consists of two neck screws, the two screws are almost parallel to the fracture line of ROIFs. This limits its overall antisliding capacity. The design of the MPFN enables it to provide good medial support through the subtrochanteric screw and effectively resist sliding via the right angle locking structure.
This study has some limitations. Ligaments, muscles, and tendons were not considered during finite element modelling. This is a common phenomenon in similar studies on the biomechanical properties of new orthopedic implants17,30. Notably, the interaction between new implants and bones was the focus of this study. Therefore, ignoring the influence of soft tissues was reasonable to some extent. What’s more, the force applying to the femoral head is complex in reality, but we simplified it into axial compression, bending, and torsion loads. In further study, we will try to simulate the loads during walking and motion. Besides, we assigned the femur model as a homogeneous material property. The femur of patients is actually a heterogeneous structure. Yet, the current digital simulation technique is still unable to fully simulate heterogeneous materials via finite element modelling. Finally, cadaveric experiments and clinical studies will be conducted to further validate our current conclusions.
Conclusion
The modified proximal femoral nail presented the best biomechanical performance, followed by the InterTAN nail, and the PFNA for fixing reverse obliquity intertrochanteric fractures. The MPFN has the potential to be a promising device for patients with ROIFs.
Data availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
References
Haidukewych, G. J., Israel, T. A. & Berry, D. J. Reverse obliquity fractures of the intertrochanteric region of the femur. J. Bone Joint Surg. Am. 83, 643–650 (2001).
Makki, D., Matar, H. E., Jacob, N., Lipscombe, S. & Gudena, R. Comparison of the reconstruction trochanteric antigrade nail (TAN) with the proximal femoral nail antirotation (PFNA) in the management of reverse oblique intertrochanteric hip fractures. Injury 46, 2389–2393 (2015).
Park, S. Y., Yang, K. H., Yoo, J. H., Yoon, H. K. & Park, H. W. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J. Trauma. 65, 852–857 (2008).
de Bruijn, K., den Hartog, D., Tuinebreijer, W. & Roukema, G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J. Bone Joint Surg. Am. 94, 1266–1272 (2012).
Hsueh, K. K. et al. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int. Orthop. 34, 1273–1276 (2010).
Larsson, S., Friberg, S. & Hansson, L. I. Trochanteric fractures. Mobility, complications, and mortality in 607 cases treated with the sliding-screw technique. Clin. Orthop. Relat. Res. 260, 232–241 (1990).
Nuber, S., Schönweiss, T. & Rüter, A. Stabilisation of unstable trochanteric femoral fractures. Dynamic hip screw (DHS) with trochanteric stabilisation plate vs. proximal femur nail (PFN). Unfallchirurg 106 (1), 39–47 (2003).
Zha, G. C., Chen, Z. L., Qi, X. B. & Sun, J. Y. Treatment of pertrochanteric fractures with a proximal femur locking compression plate. Injury 42 (11), 1294–1299 (2011).
Lu, G. L., Li, S. J. & Li, W. X. Biomechanical study of extramedullary and intramedullary fixation in the treatment of unstable intertrochanteric reversed-tilt fractures of the femur. Ann. Transl Med. 10(4), (2022).
Şensöz, E., Ergun, S., Kayaalp, M. E. & Eceviz, E. The comparison of dynamic condylar screw plate to proximal femoral nail in reverse oblique and transverse intertrochanteric fractures: a retrospective study on 61 patients. Cureus 15(3), (2023).
Chou, D. T., Taylor, A. M., Boulton, C. & Moran, C. G. Reverse oblique intertrochanteric femoral fractures treated with the intramedullary hip screw (IMHS). Injury 43(6), (2012).
Afsari, A. et al. Clamp-assisted reduction of high subtrochanteric fractures of the femur. J. Bone Joint Surg. Am. 91, 1913–1918 (2009).
Robinson, C. M., Houshian, S. & Khan, L. A. Trochanteric-entry long cephalomedullary nailing of subtrochanteric fractures caused by low energy trauma. J. Bone Joint Surg. Am. 87, 2217–2226 (2005).
Bai, H. et al. Biomechanical evaluation of three implants for treating unstable femoral intertrochanteric fractures: finite element analysis in axial, bending and torsion loads. Front. Bioeng. Biotechnol. 11, 1279067 (2023).
Eberle, S., Gerber, C., Von Oldenburg, G., Hogle, F. & Augat, P. A biomechanical evaluation of orthopaedic implants for hip fractures by finite element analysis and in-vitro tests. Proc. Inst. Mech. Eng. H. 224, 1141–1152 (2010).
Nie, S. B. et al. Medial support nail and proximal femoral nail antirotation in the treatment of reverse obliquity inter-trochanteric fractures (Arbeitsgemeinschaft fur Osteosynthesfrogen/Orthopedic Trauma Association 31-A3.1): a finite-element analysis. Chin. Med. J. (Engl) 133(22), (2020).
Ding, K. et al. Proximal femoral bionic nail-a novel internal fixation system for the treatment of femoral neck fractures: a finite element analysis. Front. Bioeng. Biotechnol. 11, (2023).
Papini, M., Zdero, R., Schemitsch, E. H. & Zalzal, P. The biomechanics of human femurs in axial and torsional loading: comparison of finite element analysis, human cadaveric femurs, and synthetic femurs. J. Biomech. Eng. 129 (1), 12–19 (2007).
Li, J., Zhao, X., Hu, X., Tao, C. & Ji, R. A theoretical analysis and finite element simulation of fixator-bone system stiffness on healing progression. J. Appl. Biomater. Funct. Mater. 16, 115–125 (2018).
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D. & Kellam, J. F. Fracture and dislocation classification compendium-2018. J. Orthop. Trauma. 32, S1–S10 (2018).
D’Arrigo, C. et al. Intertrochanteric fractures: comparison between two different locking nails. Int. Orthop. 36, 2545–2551 (2012).
Zehir, S., Zehir, R., Zehir, S., Azboy, I. & Haykir, N. Proximal femoral nail antirotation against dynamic hip screw for unstable trochanteric fractures; a prospective randomized comparison. Eur. J. Trauma. Emerg. Surg. 41, 393–400 (2015).
Bergmann, G. et al. Hip contact forces and gait patterns from routine activities. J. Biomech. 34, 859–871 (2001).
Zhang, Y., Chen, W. & Zhang, Q. A triangular-supported intramedullary nail for femoral neck and intertrochanteric fractures. Patent CN201524132U, (2010).
Wang, Y. et al. Finite element analysis of proximal femur bionic nail (PFBN) compared with proximal femoral nail antirotation and InterTan in treatment of intertrochanteric fractures. Orthop. Surg. 14(9), (2022).
Yang, Y. J. et al. Comparative study of a novel proximal femoral bionic nail and three conventional cephalomedullary nails for reverse obliquity intertrochanteric fractures: a finite element analysis. Front. Bioeng. Biotechnol. 12 (0), 1393154 (2024).
Chen, S. Y. et al. A new fluoroscopic view for evaluation of anteromedial cortex reduction quality during cephalomedullary nailing for intertrochanteric femur fractures: the 30 oblique tangential projection. BMC Musculoskelet. Disord. 21 (1), 719 (2020).
Nie, B., Chen, X., Li, J., Wu, D. & Liu, Q. The medial femoral wall can play a more important role in unstable intertrochanteric fractures compared with lateral femoral wall: a biomechanical study. J. Orthop. Surg. Res. 12, 197 (2017).
Song, H., Chang, S. M., Hu, S. J., Du, S. C. & Xiong, W. F. Calcar fracture gapping: a reliable predictor of anteromedial cortical support failure after cephalomedullary nailing for pertrochanteric femur fractures. BMC Musculoskelet. Disord. 23 (1), 175 (2022).
Ren, W. et al. The study of biomechanics and clinical anatomy on a novel plate designed for posterolateral tibial plateau fractures anterolateral approach. Front. Bioeng. Biotechnol. 10, (2022).
Funding
This study was supported by the Bureau project of Xi’an Health Commission (2024ms08). The funding source has no role in study design, conduction, data collection or statistical analysis.
Author information
Authors and Affiliations
Contributions
K.Z. designed the study. Q. H., Q. W, L. L., L. S., T. M., K. Z. and Z. L. searched relevant clinical data, analyzed and interpreted the data. Q. W. wrote the manuscript. H. Q. and K. Z. contributed most in the revision of this manuscript. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate/consent to publish
All patients or their family members have signed the informed consent before surgery and provided the consent to publish and report individual clinical data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Q., Sun, L., Liu, L. et al. Biomechanical evaluation of the modified proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures. Sci Rep 15, 3261 (2025). https://doi.org/10.1038/s41598-025-87951-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87951-3