Abstract
This descriptive study focuses on the oral health of African migrants, especially adolescents, arriving in the Canary Islands. Notably, these patients show a high prevalence of caries and oral mucosal alterations. These are influenced by multifactorial factors, such as living conditions in their country of origin, hygiene habits, and sugar-rich diets. Furthermore, it is worth noting the need for inclusive oral health policies in receiving countries and the need to develop oral health care protocols in regions with migratory flows to effectively address oral health needs and facilitate the integration of migrants. We included 104 migrant patients from different African countries, mainly from North and West Africa, and analyzed their oral health status. We found that 89.4% of the patients had dental caries, with a higher prevalence in North Africa. Moreover, 25% of patients showed oral mucosal alterations, with leukoedema being the most common condition. Regarding malocclusions, 42.6% of patients had Class I malocclusion and only 15.4% had dental crowding. Regarding intraosseous lesions, 97.1% of the patients had no lesions and most did not require dental prostheses. This study provides a detailed overview of the oral health conditions of African migrants in the Canary Islands.
Similar content being viewed by others
Calle la Juventud, s/n, 35,450 Santa María de Guía.
Canary Islands, Spain.
Introduction
The World Health Organization defines oral health as a well-being condition of the teeth, gums, and the stomatognathic system that allows us to smile, speak, and chew. Oral health represents one of the most important indicators of general well-being, quality of life, and self-confidence. The most prevalent oral diseases include dental caries, periodontitis, tooth loss, and oral cancer. Given that migrants or refugees can experience social conditions that lead to vulnerability due to their special situation of lacking access to healthcare systems, they may be more affected by these oral diseases. Dental caries, periodontal diseases, oral soft tissue lesions, and traumatic dental injuries are prevalent issues among refugees1,2,3,4.
According to the World Migration Report5, the number of international migrants has increased globally, but it has done so especially in Europe. Europe receives around 87 million international migrants, representing 61% of the world’s total international migrant population. Of the European countries, Spain is one of those with the highest percentage of migrants, given that 14.6% of the population has this condition. The Canary Islands (Spanish territory) are located near the African Coast. Thus, the political instability in Africa has an immediate impact on migration to the Canary Islands and, hence, to Europe.
In the last few years, the Canary Islands have suffered a significant migration crisis because of irregular migration, and the arrival of irregular immigrants seems to be increasing since 2006. In 2021, more than 20,000 people arrived from Africa in the Canary Islands by sea, and most were minors6. The immigration situation in the European health system poses a challenge in ensuring access to health systems for refugees or migrant people, paying special attention to the most vulnerable, like children and adolescents7.
Migrant people bear a greater social and health burden. Thus, they experience a greater risk of suffering unfavorable conditions, such as less access to essential oral services. The FDI World Dental Federation has been at the forefront of promoting oral health amongst refugees, acknowledging their unique challenges in accessing dental care. Through its Refugee Oral Health Project, the FDI has developed advocacy guides8. However, oral health is often neglected in the primary health packet for refugee populations in the host countries9.
When assuming the biopsychosocial model, a physical condition is related to social and psychological factors10. Therefore, oral health is directly related to the quality of life, emotional aspects, and the social inclusion of these migrants in the receiving countries11,12,13,14. Oral aesthetics is determined by the presence of oral diseases, which affect self-perception and can develop depressive symptoms15. Inequalities based on gender, ethnicity, or origin affect the entire population in general, they take on a special significance in childhood, as this is the stage when social gender roles or differences stemming from ethnic backgrounds are generated and incorporated16. According to Font-Ribera et al.17, in the early stage of child development, social inequalities contribute to inequalities in adult life. The Commission on Social Determinants of Health of the World Health Organization states that the child and adolescent stage is a fundamental part of the pathways and mechanisms through which social inequalities are produced and perpetuated as individuals reach adulthood18 Thus, preventing oral diseases in childhood and adolescence involves a unique opportunity to promote equity and physical and mental health. The FDI World Dental Federation further emphasized the importance of integrating oral health in all health policies at national and international levels to prevent oral disease by encouraging governments, stakeholders, and decision-makers to adopt oral health promotion as an integral part of general health policies19.
Compared to the most disadvantaged groups in host countries, studies have repeatedly demonstrated that refugees have a greater prevalence of oral diseases and face barriers to receiving oral health care9,20. Furthermore, the high demand for sophisticated restorative and cosmetic procedures has led to increased commercialism in dental practice, which has, in turn, encouraged the dental profession to disregard society’s most basic oral health care needs and violate the social contract. The right to health is a fundamental human right protected in international law by the International Covenant on Economic, Social, and Cultural Rights (ICESCR). The right to health is a social right included in Article 12.1 of the ICESCR: “The States Parties to the present Covenant recognize the right of everyone to the enjoyment of the highest attainable standard of physical and mental health”. However, major global health monitoring systems, such as the Noncommunicable Diseases (NCD) Global Monitoring Framework and the Sustainable Development Goals, do not include oral health indicators. The human rights-based approach (RBA) to health system design is advocated by the United Nations (UN) and the World Health Organization (WHO) as a means of achieving the right to health. It has a track record of improving community health in many healthcare settings17.
Indeed, the 2030 Agenda for Sustainable Development, with its 17 Sustainable Development Goals (SDGs), presents both opportunities and challenges regarding addressing the needs of migrants. The goals are interconnected and address many aspects of sustainable development, including social, economic, and environmental dimensions.
Due to the psychosocial impact of oral diseases in immigrant adolescents, this study’s main contribution includes describing and analyzing the oral health and the prevalence of oral diseases in patients who come from North and West Africa to the University Dental Clinic of the Universidad Fernando Pessoa Canarias (CDUFPC). This institution assesses the vulnerable population. The aim is to furnish data on a challenging-to-recruit cohort that is currently arriving in large numbers to the Canary Islands. Thus, relevant data related to oral health in immigrant adolescents is expected.
Method
Participants
The study included 104 patients coming from different countries in Africa. They were divided into three groups, according to the country. Thus, 62.5% of patients came from North Africa, 33.7% from West Africa, and 3.8% from Central Africa. All the patients were in an age range between 13 and 17 years, and most were men (89.4%) (Table 1). Patients were treated at CDUFPC, which cares for approximately 900 patients a year, of which 30% are at risk of social exclusion. This study’s sample was assessed from September 2022 to May 2023 and came from institutions coordinated with the clinic. All the patients were informed of the study’s objective. They participated voluntarily and gave their informed consent. Since they were minors under 18 years old, we obtained the signature of their legal representative to authorize access to their medical records and personal and clinical data. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the European Scientific Institute (ECESI) (protocol HESU 12/2021).
Procedure
Data on dental estatus was determined by radiography and visual inspection. The 28 teeth were considered, not counting the third molars, following the instructions of the DMFT-index (frequency of patients with decayed, missing, and filled teeth)21. Moreover, teeth that have been restored by trauma were not considered. Regarding filled teeth, if a tooth has a filling and caries, it is counted as decayed. A tooth with a prosthetic crown is considered filled, and teeth indicated for extraction are considered lost. Regarding malocclusions, Angle’s Classification was considered22. Crowding was recorded as the presence or absence, understanding it as dental malpositions caused by tooth misalignment, commonly due to a negative bone-dental discrepancy.
The clinical record for each patient was created and kept. In this session, the clinic coordinator recorded the visit, diagnosis, treatment, and the surgeries or interventions performed in each case. All the information was organized in a document exported to the statistical database.
Data analyses
Statistical analyses were conducted using Jamovi version 2.4.1. Absolute and relative frequencies were calculated for sociodemographic data and health variables. In age, nonparametric statistics were used to describe the data because the Shapiro-Wilk W test showed that the data deviated from the standard normal distribution.
Results
Dental status (DMFT-index)
Regarding the total sample, 89.4% of patients had decayed teeth. However, 68.3% of them did not lose teeth and 87.5% did not have filled teeth.
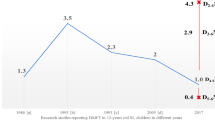
Focusing on regions, North Africa stands out with 58.7% of decayed tooth patients. Meanwhile, these only represent 3.8% in Central Africa. In West Africa, 26.9% of patients had decayed teeth. In the same way, the highest percentage of patients with missing teeth belongs to North Africa (18.3%). Meanwhile, the percentage of patients with missing teeth was 12.5% in West Africa and 1% in Central Africa. In Central Africa, no patient had filled teeth. However, 3.8% of patients in West Africa had filled teeth and 8.7% in North Africa (Table 2; Fig. 1).
Tooth crowding and malocclusions
Only 15.4% of patients in the whole sample had tooth crowding. Regarding regions, more than half of patients in North and West Africa did not have tooth crowding. These patients represented 51% and 29.8%, respectively. In Central Africa, no one had tooth crowding (Table 3; Fig. 2). Concerning malocclusions (Table 3; Fig. 3), “Class I” was the most prevalent, especially in North Africa, where 42.6% of patients had it, followed by West Africa, with 24% of patients. “Class II” and “Class III” malocclusions were below 8% in patients, considering that no one had “Class II” malocclusion in Central Africa. Undetermined malocclusions were only shown in North Africa (2.9% of patients).
Oral mucosal and intraosseous lesions
We found oral mucosal alterations in 25% of patients (Table 4). The most common condition was leukoedema with a 6.7% prevalence, followed by leukoplakia and smoker’s melanosis, both with 2.9% of prevalence and traumatic ulcer, frictional keratosis and morsicatio buccarum with 1.9%. Other mucosal alterations found were acute necrotizing ulcerative gingivitis, median rhomboid glossitis, actinic cheilitis, exfoliative cheilitis, fissured tongue, melanotic macule and fibroma. All these alterations had a prevalence of 1%. Considering the patients with oral mucosal alterations, 12.9% presented one pathology, while 2.9% had two pathologies and 1.9% had three. Focusing on regions, 20.2% of patients in North Africa had some oral mucosal lesions, 4.8% in West Africa and 0.0% in Central Africa.
Regarding intraosseous lesions (Table 4), 97.1% of patients did not have lesions. Only three patients had intraosseous lesions: two had a radicular cyst and the other had idiopathic osteosclerosis. Regarding regions, 1.9% of patients from North Africa had intraosseous lesions and 1.0% from West Africa. No Central African patients had intraosseous lesions.
Developmental alterations were also found in the sample. 16.3% of the patients presented racial melanosis, North Africa being the most prevalent region, with 8.7% of patients with developmental abnormalities. This was followed by West Africa with 6.7% and Central Africa with 1%.
Dental prosthesis
Regarding the total sample, 83.7% of patients did not need dental prostheses. Regarding regions, the percentage of patients who needed dental prostheses was 9.6% in North Africa, 5.8% in West Africa, and 1% in Central Africa (Fig. 4).
Discussion
This study aimed to describe and analyze the prevalence of oral diseases in African migrant adolescents who came to the CDUFPC in the Canary Islands. Overall, migrant patients from North, West and Central Africa were not characterized by missing or filled teeth, malocclusions, or dental prostheses. However, patients were characterized by dental caries and oral pathologies. These oral diseases may be due to the living conditions for which migrant people come. Developmental alterations were also observed in the sample. Epidemiological research highlights the burden of untreated oral disease in the World Health Organization (WHO) African Region (AFR), with about half its population suffering from oral diseases, most notably dental caries, periodontal disease and tooth loss23. This situation is complex because, in African countries, there is a pronounced shortage of health personnel specialized in oral health, highlighting the need for development action supported by capacity building to address oral health needs by practitioners.
In contrast, these countries show great potential for developing innovative care models that make greater use of human resources24. Focusing primarily on the limitation of surveillance systems of oral care systems in Africa, we could highlight the limited economic resources that are focused mainly on fighting communicable infectious diseases25.
The role played by socio-behavioral factors and oral health is universally accepted. Oral conditions are mostly a result of a lack of timely dental care due to educational and economic deficiencies, which are the product of social inequality. Thus, they result in the consequent difficulty of the population in taking care of themselves and obtaining access to health services, affecting the quality of life of individuals with these pathologies, which can lead to other organic and psychological conditions. However, treating oral diseases is costly, even in high-income countries where 5–10% of public health spending is used for dental care26,27,28.
Regarding dental status (DMFT-Index), 89.4% of patients had dental caries, which is consistent with similar studies that found a high incidence of dental caries (compared to native patients) regardless of the country of origin and gender. The etiopathogenesis of dental caries in migrant patients may be multifactorial. They pay little attention to dental hygiene, have a diet rich in cariogenic sugars and have limited access to additional preventive measures, such as fluoride supplements. All of this, combined with the lack of hygiene during the extended period of migration from their hometown to the destination country, leads to a high number of dental caries29,30,31.
Racial melanosis is not a pathology but rather a developmental alteration. It presents clinically as macular pigmented areas of varying shapes and sizes in patients from many different ethnic backgrounds. The pigmentation color can vary from light brown to nearly black, increasing with age, and the intensity of the color can be influenced by factors such as smoking, hormones, and systemic medications32,33.
The sample comprises younger individuals (13–17 years old). Regarding oral mucosal lesions, the most common entity observed was leukoedema. Hariri et al.34 examined the bilateral whitish patches in the buccal mucosa and their relation to leukoedema, highlighting that this condition is more prevalent among adults of African descent.
Entities such as frictional keratosis and morsicatio buccarum were also found to have a low prevalence. Morsicatio is a condition caused by habitual chewing of the lips (labiorum), tongue (linguarum) or buccal mucosa (buccarum). Clinically, it often produces a white lesion caused by pieces of the oral mucosa torn free from the surface. The condition is generally found among people who are stressed or psychologically impaired30 and it could perfectly occur in patients migrants. Most patients with these conditions are not even aware of their biting habit. It is important to differentiate frictional keratosis and morsicatio buccarum from pathological conditions to avoid unnecessary treatments and interventions, just as it should be observed for conditions such as leukoedema, which should not be confused with other white oral lesions such as leukoplakia.
Studies indicate that the most common type of injury in adolescents is recurrent aphthous stomatitis35,36,37,38,39. The general prevalence of this injury varies considerably as several studies record their findings cross-sectionally. In other words, the findings were recorded on the same day the patient was examined, as the data were categorized in this study. The prevalence is likely underestimated because the ulcerated lesions can occur at intervals and generally heal within two weeks, depending on the subtype. The same fact occurs with herpes simplex lesions, which are transient, and their prevalence would be underestimated in the population. Therefore, it would justify the absence of both lesions in the studied population.
The prevalence rate of oral maxillofacial pathologies in the population increases with age because of the deterioration of the individual’s health status. It could explain why only three patients had intraosseous lesions in the sample studied since it was a very young population. In a previous study, Velázquez-Cayón et al.40 presented data from a migrant population, primarily from Morocco. The oral mucosal pathologies diagnosed in the adult group (41–70 years old) included fibrous lesions, benign migratory glossitis, black hairy tongue, intraoral lesions due to Herpes Simplex Virus, gingival enlargement due to drugs, florid cemento-osseous dysplasia, and mucosal ulceration with bone sequestration.
If we focus on the skeletal relationships of the jaws, on the one hand, 42.6% of migrant patients had a Class I Angle malocclusion. Classes II and III were found in smaller proportions. Only 2.9% of the patients could not have their malocclusions assessed, primarily due to the absence of teeth. Alhammadi et al.41 analyzed the global distribution of malocclusions, determining that the Class I Angle malocclusion is the most prevalent in the African population, which is in line with the results of this study. Malocclusions may not be a primary concern in the general population based on ethnicity. However, it is important to consider the consequences of tooth loss due to caries. This occlusal imbalance can lead to serious consequences for the remaining teeth.
On the other hand, dental crowding was not a problem in the studied population either. Regarding adolescents, 85% did not have issues with dental crowding, which is in line with Mugonzibwa et al.42 who found greater crowding in Caucasian youth compared to Africans. Regarding dental prostheses, 83.7% did not have any prosthetic needs. Since patients are children and adolescents, the need for fixed prosthetics is mainly to restore severely decayed teeth. Untreated carious lesions pose a public health problem due to their impact on an individual’s quality of life and the high cost of dental care and restorative materials.
Maatouk et al.43 revealed a high morbidity of oral diseases in the Maghreb countries, dominated by dental caries and periodontal diseases requiring extensive oral care. The prevalence of dental caries exceeded 50% for temporary dentition at age 6 and 60% for permanent dentition at age 12. For periodontal disease, the prevalence was over 55% at the age of 15. Inequalities in access to oral health care between regions were noted. In the same way, Font-Ribera et al.17 studied social inequalities in child and adolescent health, with the most representative age group being from 13 to 15 years old, coinciding with our study. In general, they detected social inequalities and a consistent social gradient in dental health, with all the indicators used and across all age groups. In this regard, access to healthcare services has not shown inequalities, except for access to the dentist. It is probably due to the lack of complete coverage of dental services in the National Health System, which underscores the importance of social work carried out by the CDUFPC. At the CDUFPC, almost 80% of vulnerable patients (mostly North African migrants) treated from September 2019 to July 2022 were young people (from 15 to 20 years old), and they presented the greatest need for conservative dentistry. Considering that the Canary Islands (Spain) receive approximately more than 20,000 people each year from Africa, especially from North Africa, primary dental care services are required for migrant people in general, but especially for children and adolescents. They could integrate without additional difficulties with those they already have in society. Furthermore, the importance of the relationship between nutrition and oral health in the migrant population in general and in children and adolescents in particular must be considered. Enwonwu et al.44 highlight this relationship not only at a general level in problems of growth retardation and stunting of children but also with dental caries, periodontal diseases and oral cancer in Africa. North Africa is the main region of the patients seen, and according to recent studies, they are the ones with the worst oral health in comparison with people of other nationalities who migrate to Spain, especially women. This study subdivides the adolescent group, defining it in a range of 12 to 17 years old. Although the authors do not present the results for this age group, we can also see that caries continue to be the main oral health problem of migrants from North Africa.
Cultural and linguistic factors were shown to be the most frequent barrier (90%) to accessing care. Only 37% of the providers can access professional interpreters and cultural mediators, and 52% and 32% do not know if one or more family members are undocumented and if they are refugees/asylum seekers, respectively. Updated guidelines for the care of migrant children are only available to 35% of respondents, and 80% of them have not received specific training on the care of migrant children. In Carrasco-Sanz et al.45, 492 pediatricians completed a survey, and 87% of them worked in primary care. 63% (63%) of these pediatricians reported that the general health of migrant children is worse than that of non-immigrants. The most frequent health problem was chronic diseases. It is worth noting that in this study, 86% of the participants mentioned that the oral health of the patients was adequate. This percentage could be due to the lack of training in dentistry and pediatric dentistry of pediatric medical specialists.
WHO efforts are aimed at controlling the incidence of oral diseases, caries, and periodontal disease38 as the most prevalent to achieve the health objectives set out in the WHO Global Action Plan for Prevention and Control of NCDs 2013-20 the 2030 global agenda. In this context, studies such as the one presented here, focused on the migrant child and adolescent population from North Africa, demonstrate the need to develop policies both in the country of origin and in the receiving country to ensure this basic human right.
Observing the migratory crisis currently occurring in the Canary Islands, as part of the European territory, and taking other recent similar crises as a reference, the needs coincide. They focus on infectious diseases, such as caries and periodontal disease, and the requirement to implement measures in the receiving countries, both in public health and in increasing the private initiative to provide health care for this population.
Regarding the 2030 Agenda´s Sustainable Development Goals (SDGs), the action carried out by the CDUFPC in the treatment of vulnerable people, especially migrants, is aimed at the fulfillment of Goal 3 (Good Health and Well-being), which emphasizes the importance of ensuring healthy lives and promoting well-being for all at all ages. Within this goal, specific targets relate to ensuring access to health services, including sexual and reproductive health services, for all, regardless of their migration status. In addition, Goal 5 (Gender Equality) is fundamental for achieving sustainable development. Women migrants often face specific challenges related to their gender, including access to healthcare, education, and protection from violence. Access to oral health care is unequivocally related to achieving goals 8 (Decent Work and Economic Growth) and 10 (Reduced Inequalities). Expatriates often contribute significantly to the economies of both their host and home countries. Migrants often face discrimination and marginalization, good oral health status provides them better opportunities for employment and social integration. Particularly refugees and asylum seekers, are often vulnerable to human rights abuses, exploitation, and trafficking. Goal 16 (Peace, Justice, and Strong Institutions) targets the promotion of peaceful and inclusive societies for sustainable development, providing access to justice for all and building effective, accountable, and inclusive institutions at all levels.
By integrating the health needs of migrants into national plans, policies, and strategies across all sectors, including, as in this case, in university clinical practice, as encouraged by the 2030 Agenda, governments and institutions, such as universities, can better address the specific challenges faced by migrants and work toward achieving the SDGs more inclusively and comprehensively.
Our study has some limitations. First, data were collected retrospectively, so it was not possible to obtain a measure of the psychosocial impact of migrant patients. Furthermore, the number of patients varied according to the African regions, so they could not be adequately matched. It would be interesting to know if migrant patients from different regions of Africa present differences in oral health. Regarding the monitoring of the oral health of these patients, the main limitation was the transfer of migrant children and adolescents from the centers for migrants in Gran Canaria to different parts of the country or other European countries so that data on the follow-up of mucosal pathology or other pathologies may have been lost. However, this study shows a relevant contribution related to the need to create primary care protocols at the dental level that evaluate and treat the oral health of people at risk of social exclusion, especially in regions sensitive to migratory flow. The protocol in primary dental care could help integrate migrants in the receiving countries. Moreover, it has a lesser psychosocial impact on their quality of life and emotions.
The mobility of migrant adolescents, who are often transferred to different locations, represents another limitation, as this may have contributed to the loss of follow-up of their oral health conditions. Such dynamics imply that our results might not fully reflect the prevalence and severity of oral conditions in this population. Similarly, if we had access to the follow-up of these patients, a comparison could be made with the oral health status of local adolescents, thus also observing the impact of access to dental healthcare on this population group compared to the local population.
Despite these limitations, this study provides significant insights into the oral health of African migrant adolescents. It underscores the importance of developing primary dental care strategies that are accessible and appropriate for vulnerable populations, especially in areas with high levels of migration.
Conclusions
In analyzing the intricate nexus between migration and oral health, our study has unraveled certain patterns and challenges that are essential to address. These findings not only shed light on the specific needs of African migrant populations but also underscore broader issues within the healthcare systems of host countries. As we draw from the data, it is pivotal to understand the multifaceted dimensions of the oral health landscape for migrants. Here are our conclusions based on the evidence gathered:
-
1.
Oral Health in Migrants: migrant patients from Africa show a high prevalence of caries and oral mucosal alterations, influenced by multifactorial factors such as living conditions in their home country, hygiene habits, and diets rich in sugars.
-
2.
Need for Adaptive Protocols: there is an emphasized urgency to develop primary dental care protocols in regions with migratory flow to effectively address oral health needs and facilitate the integration of migrants.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
World Health Organization. Global oral Health Status Report: Towards Universal Health Coverage for oral Health by 2030. Executive Summary (World Health Organization, 2022). https://www.who.int/publications/i/item/9789240061569Licence: CC BY-NC-SA 3.0 IGO.
World Health Organization. Global Oral Health Status Report 2022. Geneva: World Health Organization. (2022).
World Health Organization. Global Strategy and Action plan on oral Health 2023–2030 (World Health Organization, 2023).
World Health Organization. WHO Highlights oral Health Neglect Affecting Nearly half of the World’s Population. News Release (World Health Organization, 2022).
Keboa, M. T., Hiles, N. & Macdonald, M. E. The oral health of refugees and asylum seekers: A scoping review. Globalization Health. 12 (1). https://doi.org/10.1186/s12992-016-0200-x (2016).
International Organization for Migration. World Migration Report (United Nations, 2020). https://publications.iom.int/system/files/pdf/wmr_2020.pdf
Defensor del Pueblo. La Migración en Canarias. (2021). https://www.defensordelpueblo.es/wp-content/uploads/2021/03/INFORME_Canarias.pdf
FDI World Dental Federation. Refugee oral health promotion and care project. (2021). https://www.fdiworlddental.org/refugee-oral-health-promotion-and-care-project
Kateeb, E. & Lee, H. Oral health as a refugee health right. Int. Dent. J. 73 (5), 593–594. https://doi.org/10.1016/j.identj.2023.06.013 (2023).
Gatchel, R. J. & Okifuji, A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J. Pain. 7 (11), 779–793. https://doi.org/10.1016/j.jpain.2006.08.005 (2006).
Klein, J. & Von Knesebeck, D. Inequalities in health care utilization among migrants and non-migrants in Germany: A systematic review. International J. Equity Health (Online). 17 (1). https://doi.org/10.1186/s12939-018-0876-z (2018).
Muñoz-Pino, N., Vives-Cases, C., Agudelo‐Suárez, A. A. & Ronda, E. Comparing oral Health services Use in the Spanish and immigrant Working Population. J. Immigr. Minor. Health. 20 (4), 809–815. https://doi.org/10.1007/s10903-017-0630-4 (2017).
Ribas-Perez, D. R. et al. Cross-sectional study on oral health-related quality of Life using OHIP-14 in migrants children in Melilla. Child. (Basel). 10 (7), 1168. https://doi.org/10.3390/children100711686 (2023). Spain.
Vázquez, M. L. et al. Was access to health care easy for immigrants in Spain? The perspectives of health personnel in Catalonia and Andalusia. Health Policy. 120 (4), 396–405. https://doi.org/10.1016/j.healthpol.2016.01.011 (2016).
Montes, J. L. Oral health impact in older adult life quality. Revista Dent. De Chile. 92 (3), 29–31 (2001).
Braveman, P. What is Health Equity: And how does a life-course Approach take us further toward it? Matern. Child Health J. 18 (2), 366–372. https://doi.org/10.1007/s10995-013-1226-9 (2013).
Font-Ribera, L. et al. El Estudio De las desigualdades sociales en la salud infantil y adolescente en España. Gac. Sanit. 28 (4), 316–325. https://doi.org/10.1016/j.gaceta.2013.12.009 (2014).
World Health Organization & Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. (2008). https://iris.who.int/bitstream/handle/10665/69832/WHO_IER_CSDH_08.1_eng.pdf?sequence=1
FDI World Dental Federation. Preventing Oral Diseases. (2017). https://www.fdiworlddental.org/preventing-oral-diseases
Kizi, G. et al. Oral health in migrants children in Melilla. Spain Child. (Basel). 10 (5), 888. https://doi.org/10.3390/children10050888 (2023).
World Health Organization. Oral Health Surveys: Basic Methods 5,5th, edn (Switzerland, 2013).
Angle, E. H. Classification of malocclusion. Dent. Cosmos. 41, 248–264 (1989).
Abid, A. et al. Prevalence and severity of oral diseases in the Africa and Middle East Region. Adv. Dent. Res. 27 (1), 10–17. https://doi.org/10.1177/0022034515582062 (2015).
Gallagher, J. E. et al. Oral health workforce in Africa: A scarce resource. Int. J. Environ. Res. Public Health. 20 (3), 2328. https://doi.org/10.3390/ijerph20032328 (2023).
Tchéré, M. Y., Ndiaye, C. F. & Bourgeois, D. Surveillance de la santé buccodentaire en Afrique: revue actuelle des politiques et stratégies. Revue D’épidémiologie Et De Santé Publique. 57 (6), 419–428. https://doi.org/10.1016/j.respe.2009.07.069 (2009).
Petersen, P. P. E. The world oral health report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Commun. Dent. Oral Epidemiol. 31(s1), 3–24. https://doi.org/10.1046/j.2003.com122.x (2003).
Petersen, P. E., Bourgeois, D., Ogawa, H., Estupinan-Day, S. & Ndiaye, C. The global burden of oral diseases and risks to oral health. Bull. World Health Organ. 83, 661–669 (2005).
Masood, M., Sheiham, A. & Bernabé, E. Household expenditure for Dental Care in Low and Middle Income Countries. PLOS ONE. 10 (4), e0123075. https://doi.org/10.1371/journal.pone.0123075 (2015).
Gallardo, V. P., Cencillo, C. P. & Plana, B. M. Prevalencia De La caries dental en El niño Inmigrante: Estudio comparativo con El niño autóctono. Anales Pediatría. 65, 337–341 (2006).
Hernando, C., Sabidó, M., Ronda, E., Ortiz-Barreda, G. & Casabona, J. A systematic review of longitudinal cohort studies on the health of migrant populations. Soc. Med. 9, 73–85 (2016).
Teshome, A., Muche, A. & Girma, B. Prevalence of Dental Caries and Associated factors in East Africa, 2000–2020: systematic review and Meta-analysis. Front. Public. Health. 9, 645091. https://doi.org/10.3389/fpubh.2021.645091 (2021).
Gondak, R., Silva-Jorge, D., Jorge, R., Lopes, J., Vargas, P. A. & M. A., & Oral pigmented lesions: Clinicopathologic features and review of the literature. Med. Oral Patologia Oral y Cir. Bucal. 1,17 (6), e919–e924. https://doi.org/10.4317/medoral.17679 (2012).
Rosebush, M. S., Briody, A. N. & Cordell, K. G. Black and Brown: non-neoplastic pigmentation of the oral mucosa. Head Neck Pathol. 13 (1), 47–55. https://doi.org/10.1007/s12105-018-0980-9 (2019).
Hariri, F. Bilateral whitish patches on the inner cheek: Leukoedema. In W. M. Tilakaratne & T. G. Kallarakkal (Eds.), Clinicopathological correlation of oral diseases (pp. 349–357). Springer Nature Switzerland AG. (2023). https://doi.org/10.1007/978-3-031-24408-7_30
Briody, A. & Upadhyaya, J. Clinical Pathology correlation case 1: multiple painful lesions of the tongue. Oral surgery, oral medicine. Oral Pathol. Oral Radiol. 136 (6), e177–e179. https://doi.org/10.1016/j.oooo.2023.08.004 (2023).
Amadori, F., Bardellini, E., Conti, G. M. & Majorana, A. Oral mucosal lesions in teenagers: A cross-sectional study. Ital. J. Pediatr. 43 (1). https://doi.org/10.1186/s13052-017-0367-7 (2017).
Scully, C. & Porter, S. Oral mucosal disease: Recurrent aphthous stomatitis. British Journal Of Oral & Maxillofacial Surgery/British Journal Of Oral And Maxillofacial Surgery, 46(3), 198–206. (2008). https://doi.org/10.1016/j.bjoms.2007.07.201
Furlanetto, D. L., Crighton, A. & Topping, G. Differences in methodologies of measuring the prevalence of oral mucosal lesions in children and adolescents. Int. J. Pediatr. Dent. 16 (1), 31–39. https://doi.org/10.1111/j.1365-263x.2006.00674.x (2005).
Manoj, M. A., Jain, A., Madtha, S. A. & Cherian, T. Prevalence and risk factors of recurrent aphthous stomatitis among college students at Mangalore, India. Peer J. 11, e14998. https://doi.org/10.7717/peerj.14998 (2023).
Velázquez-Cayón, R. T., Contreras-Madrid, A. I., Parra-Rojas, S. & Pérez-Jorge, D. Oral health and pathologies in migrants and Vulnerable Population and their social impact: the Good practices of the intervention model of a University Dental Clinic. International J. Environ. Res. Public. Health (Online). 20 (1), 353. https://doi.org/10.3390/ijerph20010353 (2022).
Alhammadi, M. S., Halboub, E., Fayed, M. M. S., Labib, A. & El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press. J. Orthod. 23 (6). https://doi.org/10.1590/2177-6709.23.6.40.e1-10.onl (2018). 40.e1-40.e10.
Mugonzibwa, E. et al. Spacing and crowding among African and caucasian children. Orthod. Craniofac. Res. 11 (2), 82–89. https://doi.org/10.1111/j.1601-6343.2007.00416.x (2008).
Maatouk, F. et al. La santé bucco-dentaire Au Grand Maghreb: revue systématique de la littérature. Sante Publique. 34 (2), 309–318 (2022).
Enwonwu, C. O., Phillips, R. S., Ibrahim, C. D. & Danfillo, I. S. Nutrition and oral health in Africa. Int. Dent. J. 54, 344–351. https://doi.org/10.1111/j.1875-595x.2004.tb00010.x (2004).
Carrasco-Sanz, A. et al. Migrant children’s health problems, care needs, and inequalities: European primary care paediatricians’ perspective. Child. Care Health Dev. 44 (2), 1–5. https://doi.org/10.1111/cch.12538 (2017).
Acknowledgements
The authors would like to acknowledge Fernando Pessoa Canarias University for their support.
Funding
None.
Author information
Authors and Affiliations
Contributions
E.S., R.V.C., S.P.R, J.C.S. contributed to study design and data acquisition, analysis, and interpretation, participated in drafting the article and gave their final approval of its submitted version. D.P.J. and A.CM. revised the manuscript critically and gave the approval to the submitted version critically for important intellectual content and approved the final version of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sirumal, E., Parra-Rojas, S., Cassol-Spanemberg, J. et al. Descriptive study on oral health and pathologies in vulnerable migrant adolescents from North and West Africa. Sci Rep 15, 3429 (2025). https://doi.org/10.1038/s41598-025-87972-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87972-y